(4) Psychopharmacology and Neurotransmitter Functions
1/88
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
89 Terms
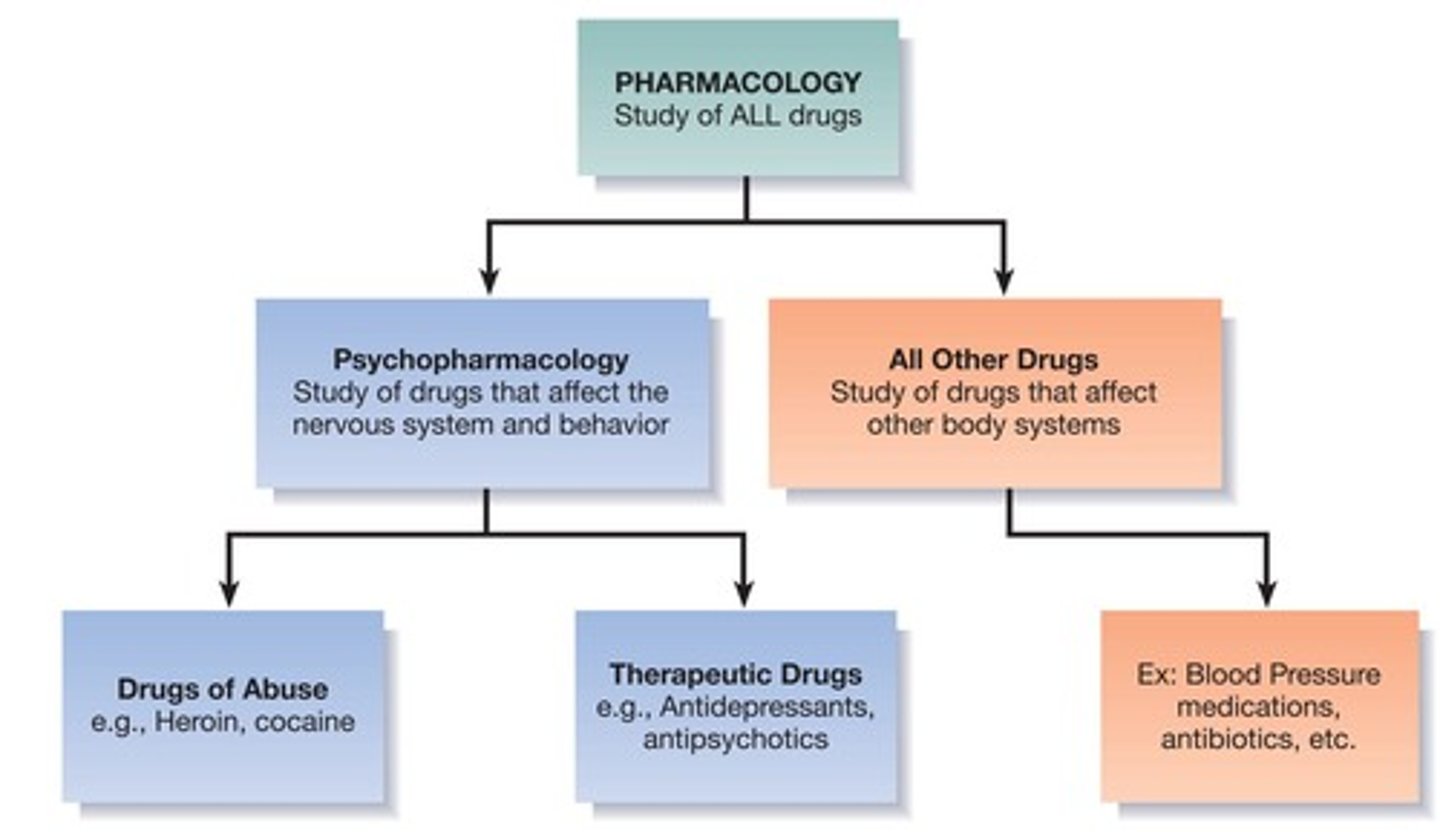
Psychopharmacology
The study of the effects of drugs on the nervous system and behavior
Drug
An exogenous chemical not necessary for normal cellular functioning that significantly alters the functions of certain cells of the body when taken in relatively low doses
Psychoactive Drug
A drug that has effects on conscious states and/or behavior
Goals of Psychopharmacology
To understand behavioral effects of drugs in the nervous system (e.g., site of reward effects, etc.), to develop novel therapeutics (e.g., to treat Alzheimer's), to understand the nervous system (as a research tool)
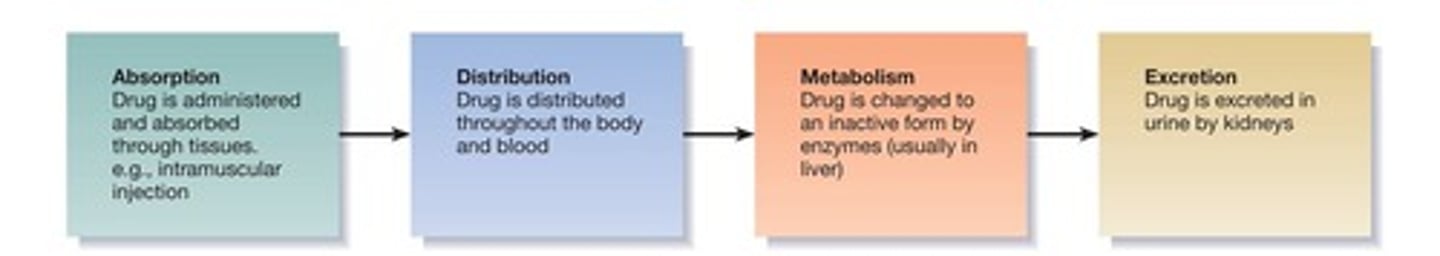
Pharmacokinetics
How drugs move through the body (kinetics = movement)
Route of Administration
Affects speed of absorption (e.g., fastest is intravenous injection) and blood levels
Absorption
Routes of Administration include intravenous injection, intraperitoneal injection, intramuscular injection, subcutaneous injection, intracerebral administration, intracerebroventricular (ICV) administration, oral administration, sublingual administration, inhalation, topical administration
Distribution
Most psychoactive drugs exert effects on cells of the CNS and must pass through the Blood Brain Barrier
Best Drug Molecule Characteristics
Best if drug molecules are lipid soluble, small, and neutral
Metabolism and Excretion
Most drugs are metabolized and deactivated by enzymes in the brain and liver, and all drugs are eventually excreted, mostly by kidneys
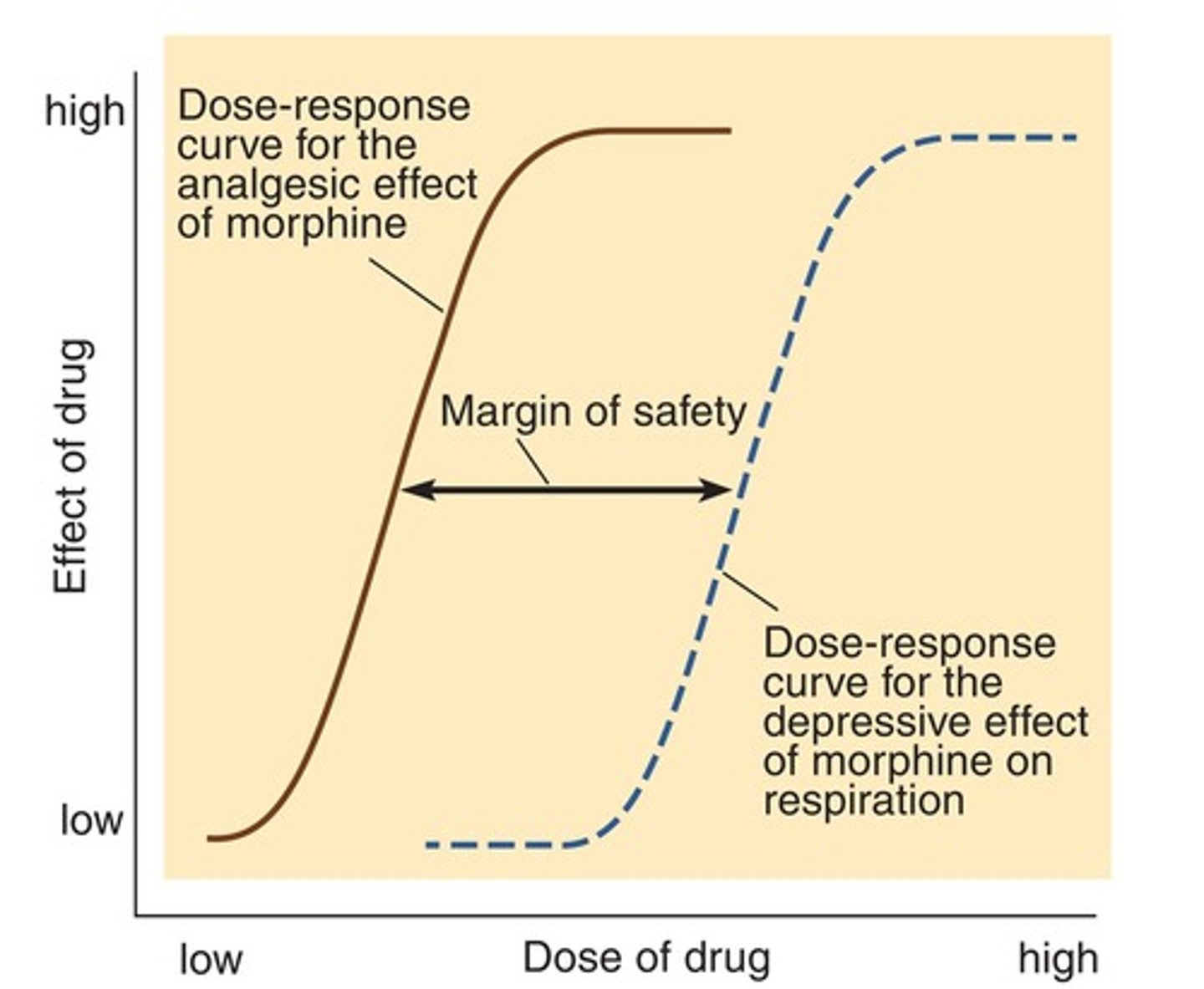
Describing Drug Effects
A given drug can have more than one effect (e.g., morphine blocks pain and suppresses respiration) and drugs can produce same effects through different mechanisms (analgesia from morphine is not same as aspirin)
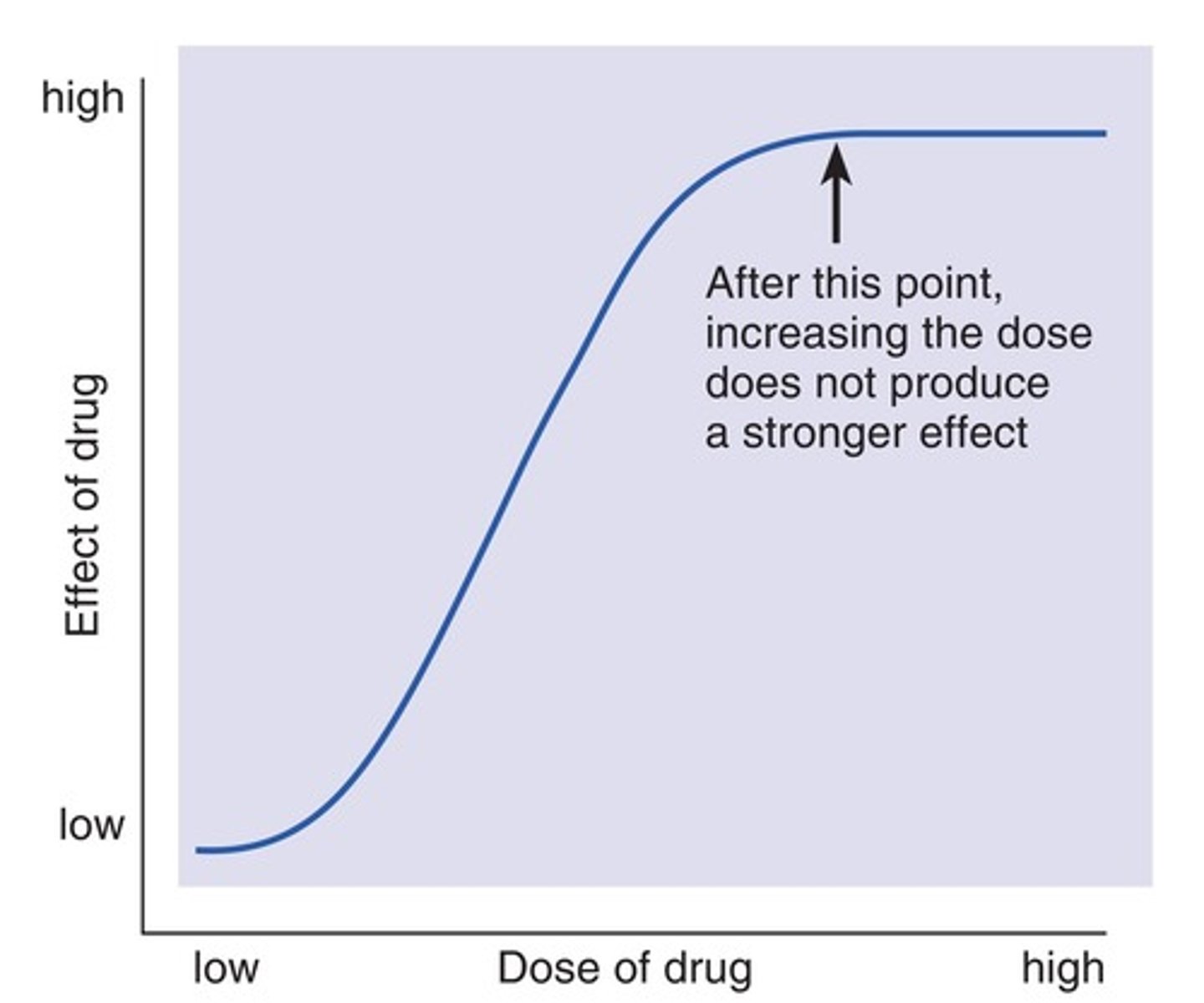
Dose-Response Curves
Effects vary with dose
Blood Brain Barrier
A selective barrier that prevents certain substances from entering the brain
Intravenous Injection
The fastest route of drug administration
Enzymes in Drug Metabolism
Enzymes sometimes transform molecules into active versions (e.g., benzodiazepines)
Classes of Neurotransmitters
Include Amino Acids (glutamate, GABA), Acetylcholine, Monoamines, Peptides, and Lipids
Actions on Receptors
Refers to how drugs interact with neurotransmitter receptors to produce effects
Deactivation and Re-uptake of Neurotransmitters
Processes that terminate the action of neurotransmitters in the synaptic cleft
Sites of Drug Actions
Locations in the body where drugs exert their effects
Intracerebroventricular (ICV) Administration
A method of drug administration directly into the brain's ventricular system
Margin of Safety
Difference between therapeutic dose and dose that produces toxicity (like respiratory suppression).
Tolerance
Decrease in drug effectiveness requiring higher doses for the same effect.
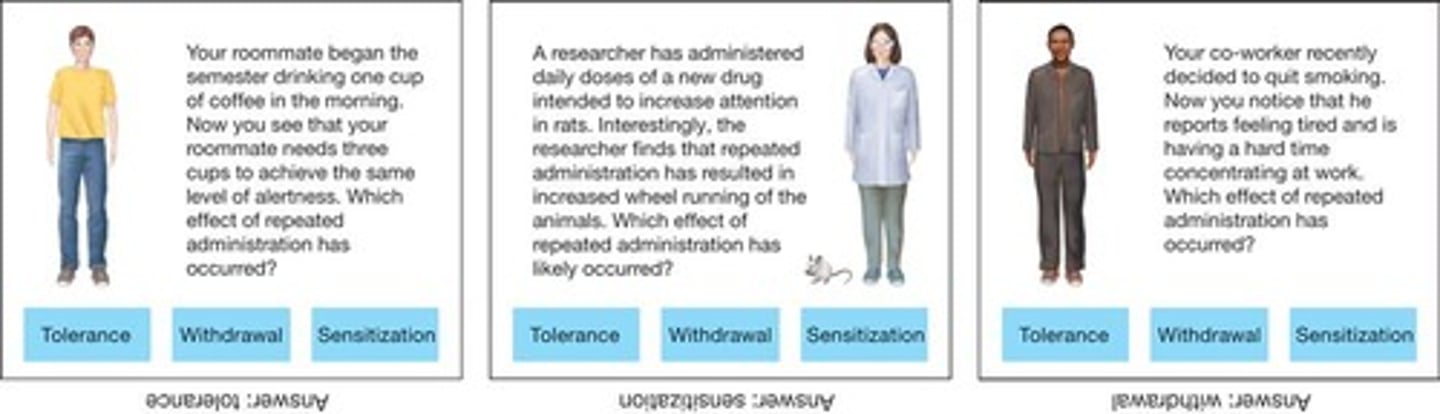
Sensitization
Drug becomes more effective.
Withdrawal symptoms
Symptoms that occur if an individual stops taking the drug, usually opposite to drug effects, indicating physical dependence.
Pharmacodynamics
Study of how drugs work at their target site, specifically the exact mechanism of action.
Agonist
Facilitates the action of a neurotransmitter.
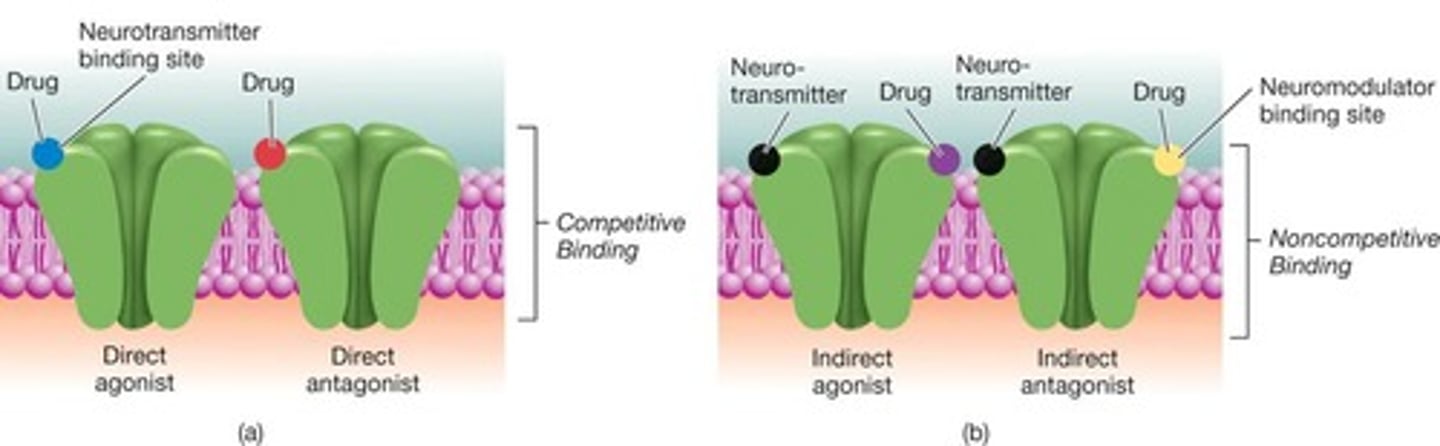
Antagonist
Blocks or decreases the action of a neurotransmitter.
Production of neurotransmitters
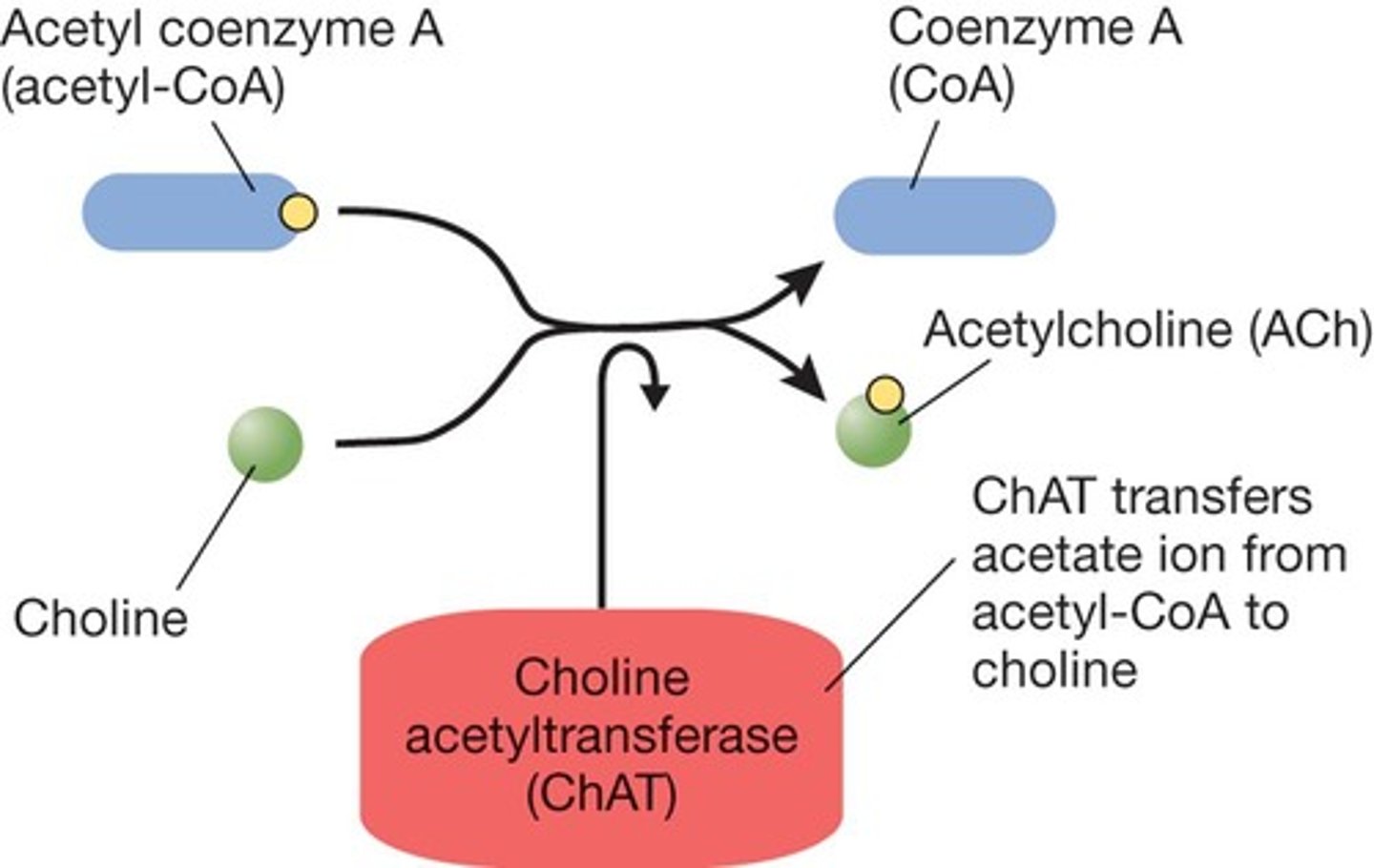
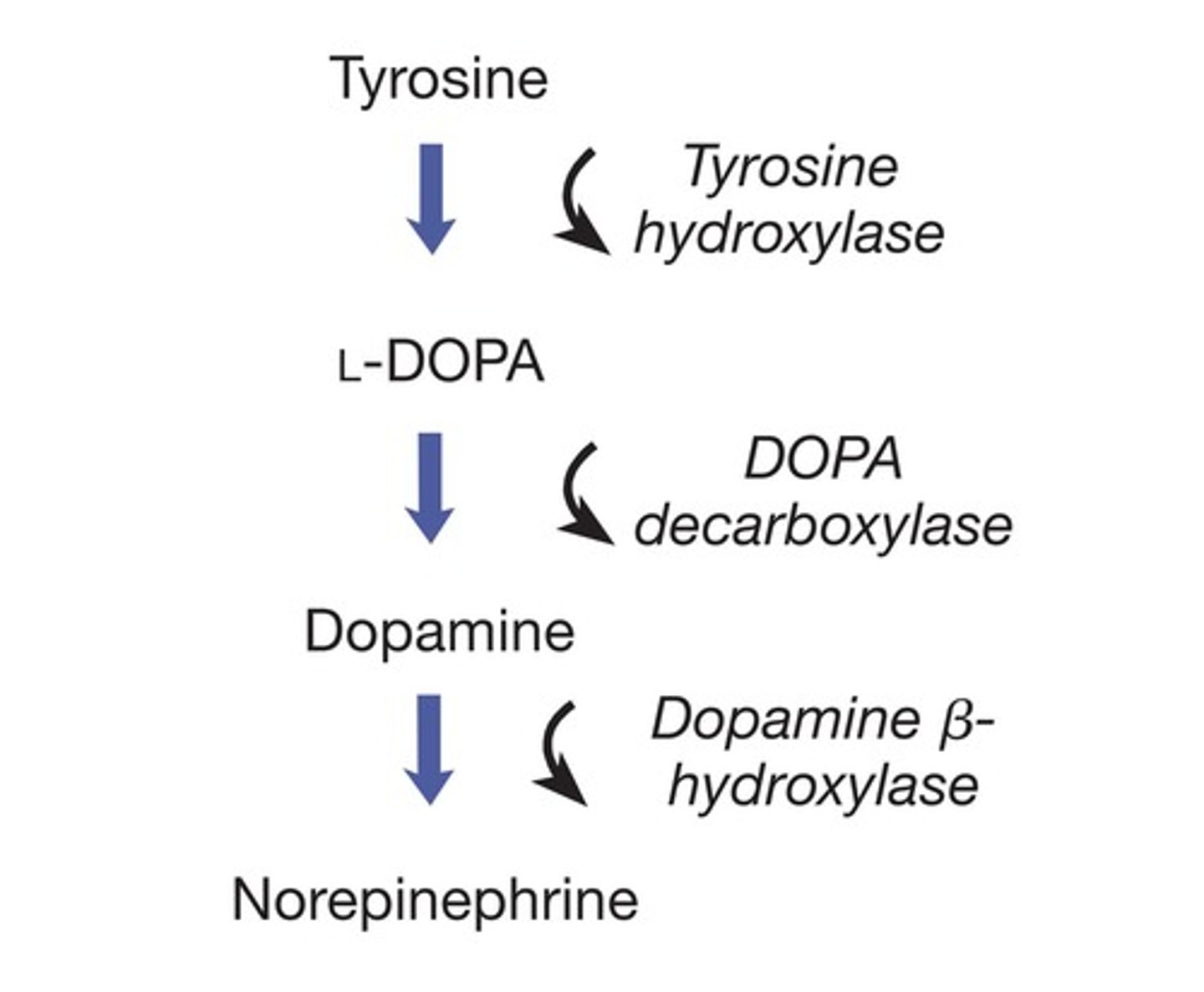
L-DOPA is a precursor for dopamine (agonist).
Storage of neurotransmitters
Reserpine prevents storage of monoamines (antagonist).
Release of neurotransmitters
Botulinum toxin blocks release of acetylcholine (antagonist).
Direct Agonist
Mimics the action of the neurotransmitter when it occupies the receptor of the neurotransmitter (e.g., nicotine and acetylcholine).
Competitive Antagonist
Competes for the same binding site as the neurotransmitter but blocks the action of the neurotransmitter (e.g., chlorpromazine blocks dopamine receptors).
Indirect Agonist
Facilitates the action of the neurotransmitter without binding to the exact receptor, often seen when drug binds to receptor complex and increases the action of the neurotransmitter (e.g., Valium and GABA).
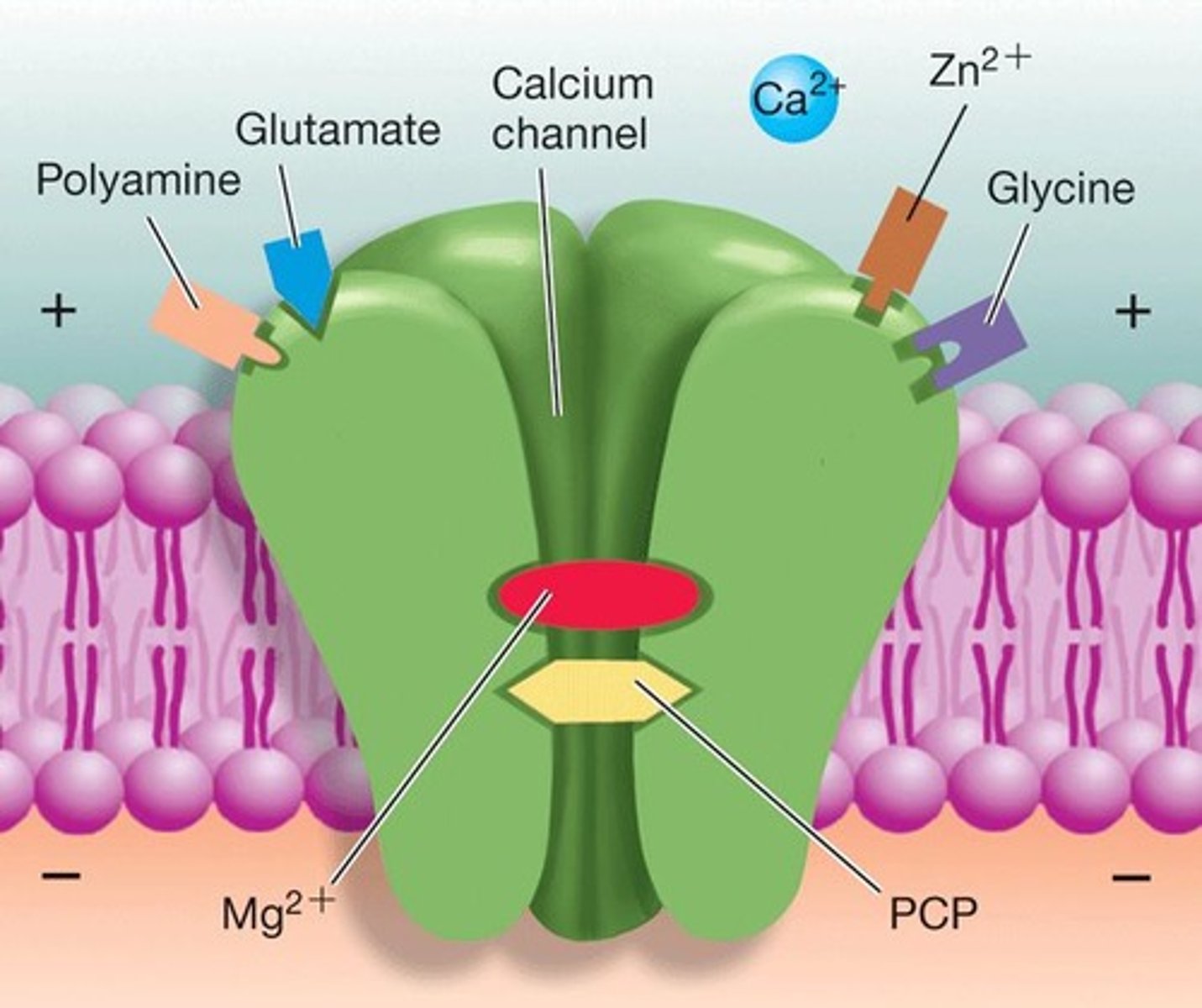
Non-competitive Antagonist
Blocks action of a neurotransmitter by binding to a different site (e.g., PCP and ion channel coupled to NMDA receptor).
Pre-synaptic auto-receptor
A receptor that, when bound by a drug, can decrease neurotransmitter release.
Post-synaptic receptor
A receptor that, when stimulated by a drug at higher doses, can increase neurotransmitter action.
Apomorphine
An agonist for dopamine receptors that at low doses binds to pre-synaptic autoreceptors and decreases dopamine release (antagonist effect) and at higher doses stimulates post-synaptic receptors (agonist effect).
Classes of Neurotransmitters
Includes Amino Acids (glutamate, GABA), Acetylcholine, Monoamines, Peptides, and Lipids.
Deactivation
The process by which neurotransmitters are broken down or removed from the synaptic cleft.
Re-uptake
The process by which neurotransmitters are reabsorbed by the presynaptic neuron after transmitting a signal.
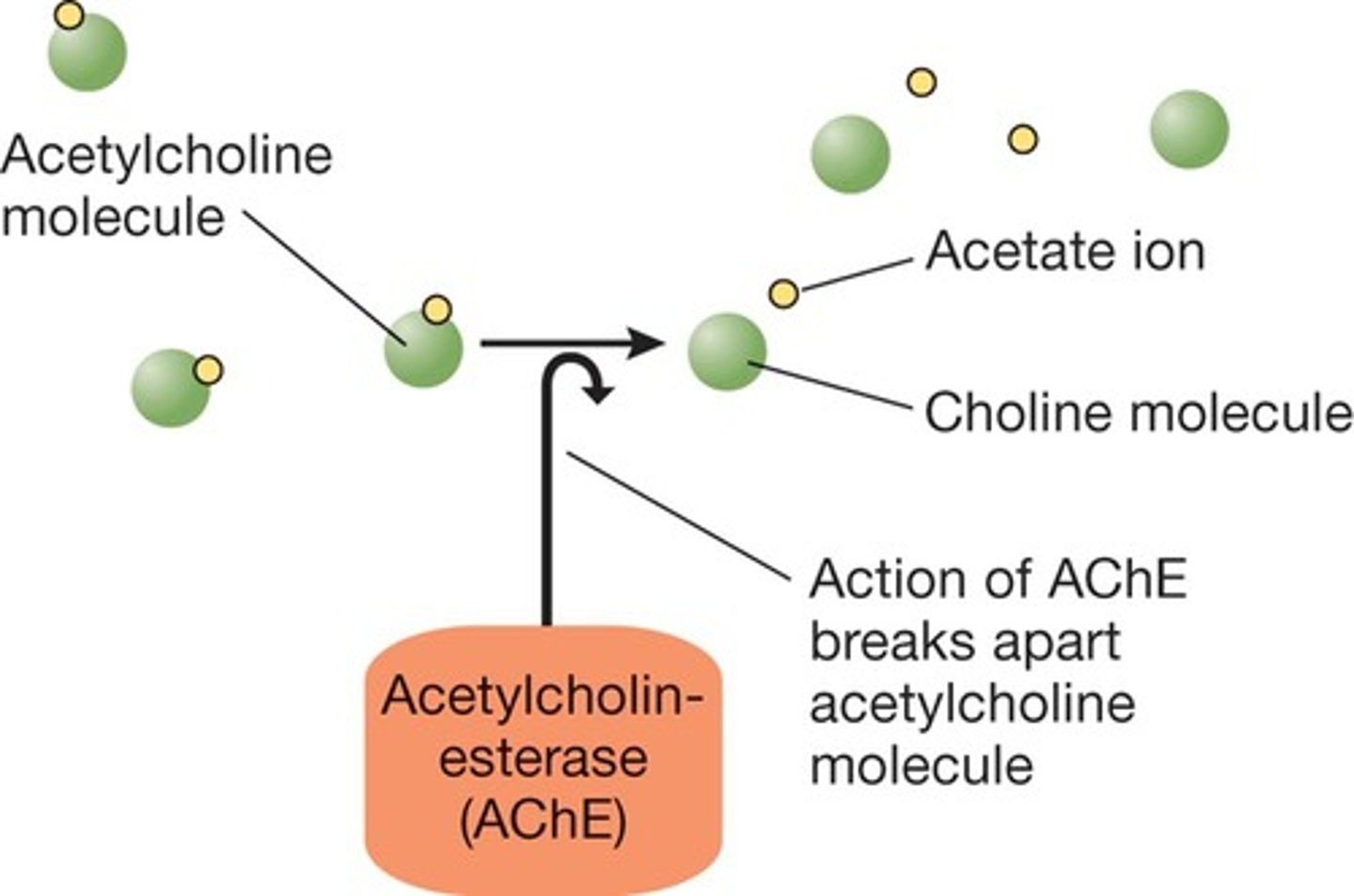
Acetylcholinesterase
An enzyme that breaks down acetylcholine in the synaptic cleft.
Fluoxetine (Prozac)
A drug that blocks the re-uptake of serotonin, leading to increased serotonin neurotransmission.
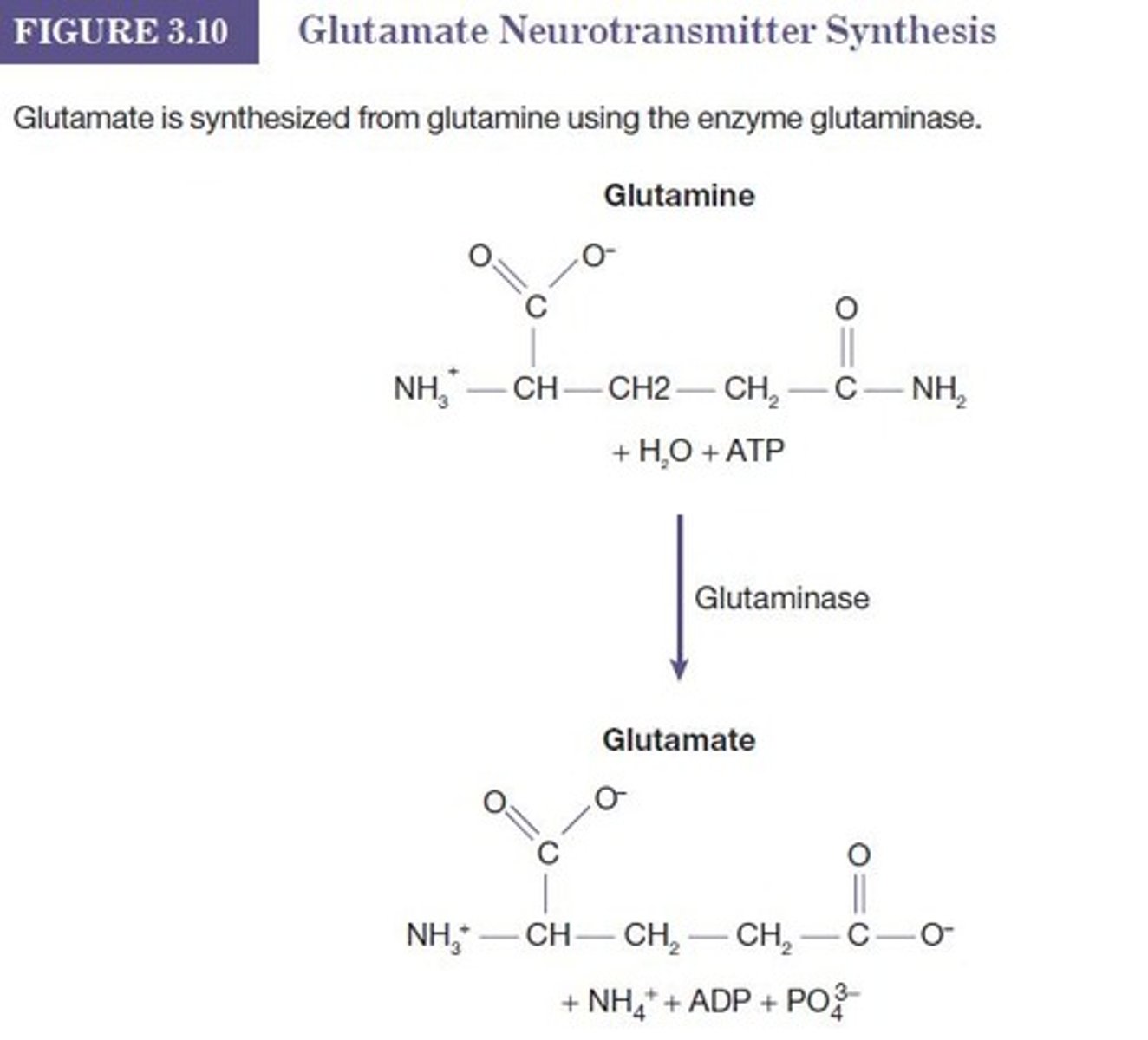
Glutamate
The main excitatory neurotransmitter in the brain and spinal cord, released by all sensory neurons except pain.
GABA
Gamma-aminobutyric acid, an inhibitory neurotransmitter in the brain.
Glycine
An inhibitory neurotransmitter found in the spinal cord and lower brain stem.
NMDA Receptor
A complex receptor that is both chemical and voltage gated, involving Ca++ and Na+ channels.
EPSPs
Excitatory post-synaptic potentials caused by the activation of excitatory neurotransmitter receptors.
Glutamate Receptors
Three ionotropic receptors (NMDA, AMPA, Kainate) and one metabotropic receptor that respond to glutamate.
Glutamine Synthetase
An enzyme that converts glutamate into glutamine.
Astrocytes
Glial cells that play an important role in regulating glutamate neurotransmission and have glutamate transporters.
Neurotoxic
A term describing substances that are harmful or damaging to nerve cells.
Ionotropic Receptors
Receptors that are coupled to ion channels and mediate fast synaptic transmission.
Metabotropic Receptors
Receptors that are linked to signaling pathways and mediate slower, longer-lasting effects.
Excitatory Neurotransmitters
Neurotransmitters that increase the likelihood of a neuron firing an action potential.
Inhibitory Neurotransmitters
Neurotransmitters that decrease the likelihood of a neuron firing an action potential.
Presynaptic Neuron
The neuron that releases neurotransmitters into the synaptic cleft.
Synaptic Cleft
The space between the presynaptic and postsynaptic neurons where neurotransmitters are released.
Vesicles
Small membrane-bound sacs that store neurotransmitters in the presynaptic neuron.
Glutamate
Termination: Astrocytes are swell...
GABA
Main inhibitory neurotransmitter in brain; inhibitory influence keeps brain stable; Seizures may be result of lacking or poorly functioning GABA-secreting neurons or receptors; Drugs such as barbiturates, alcohol, and benzodiazepines produce their effects by enhancing GABA neurotransmission.
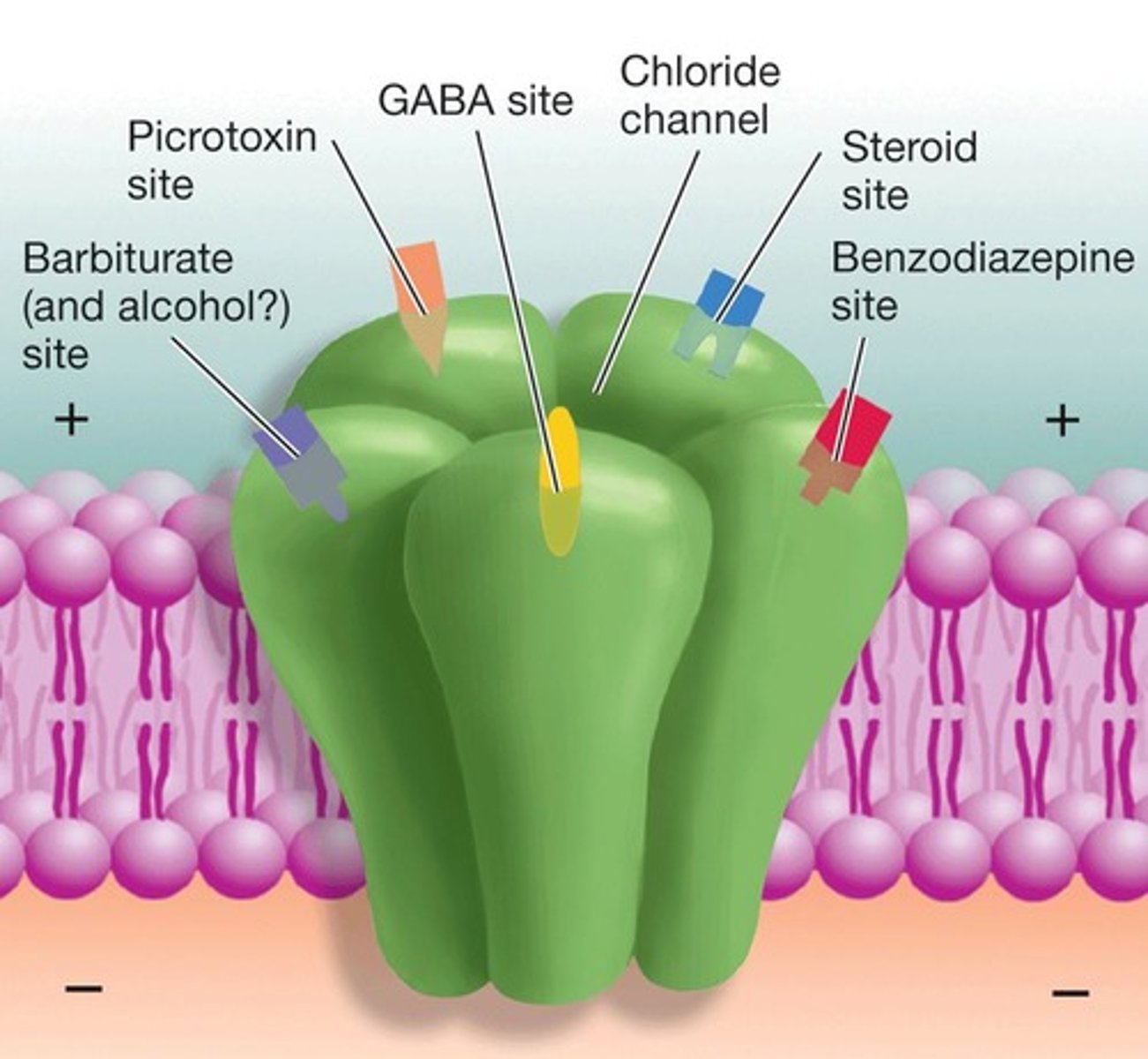
GABAA
Ionotropic, Cl- channel; hyperpolarizations; Multiple binding sites on surface for drugs: benzodiazepines, alcohol, barbiturates.
GABAB
Metabotropic; Also inhibitory.
GABA Transporters
Termination: GABA transporters; GABA aminotransferase.
Acetylcholine
Earliest known neurotransmitter; Neuromuscular junctions (PNS); Also in brain (CNS); Important for learning and memory.
Acetylcholine Pathways
Dorsolateral pons (REM sleep); Basal forebrain or nucleus basalis (facilitate learning); Medial septum (memory formation).
Nicotinic Receptor
Ionotropic ACh receptor is stimulated by nicotine.
Muscarinic Receptor
Metabotropic ACh receptor is stimulated by muscarine (found in the mushroom Amanita muscaria).
Acetylcholinesterase (AChE)
Deactivated by the enzyme acetylcholinesterase (AChE), present in the postsynaptic membrane; AChE inhibitors used to treat myasthenia gravis (neostigmine); memory loss associated with early stages of Alzheimer's donepezil (Aricept).
Monoamines
So named, due to a single amine group (NH2) in chemical structure; Very important psychological functions (target of many psychoactive drugs); Include: Dopamine (reinforcement, movement), Norepinephrine (attention, vigilance), Serotonin (mood, sleep), Histamine (wakefulness).
Catecholamines
Synthesized from tyrosine (Amino Acid); Series of steps (converting enzymes); Stored in vesicles; Note: L-DOPA used to treat Parkinson's; Termination: Enzymes: MAO (monoamine oxidase) & COMT; Re-uptake transporters.
Dopamine
Three main pathways.
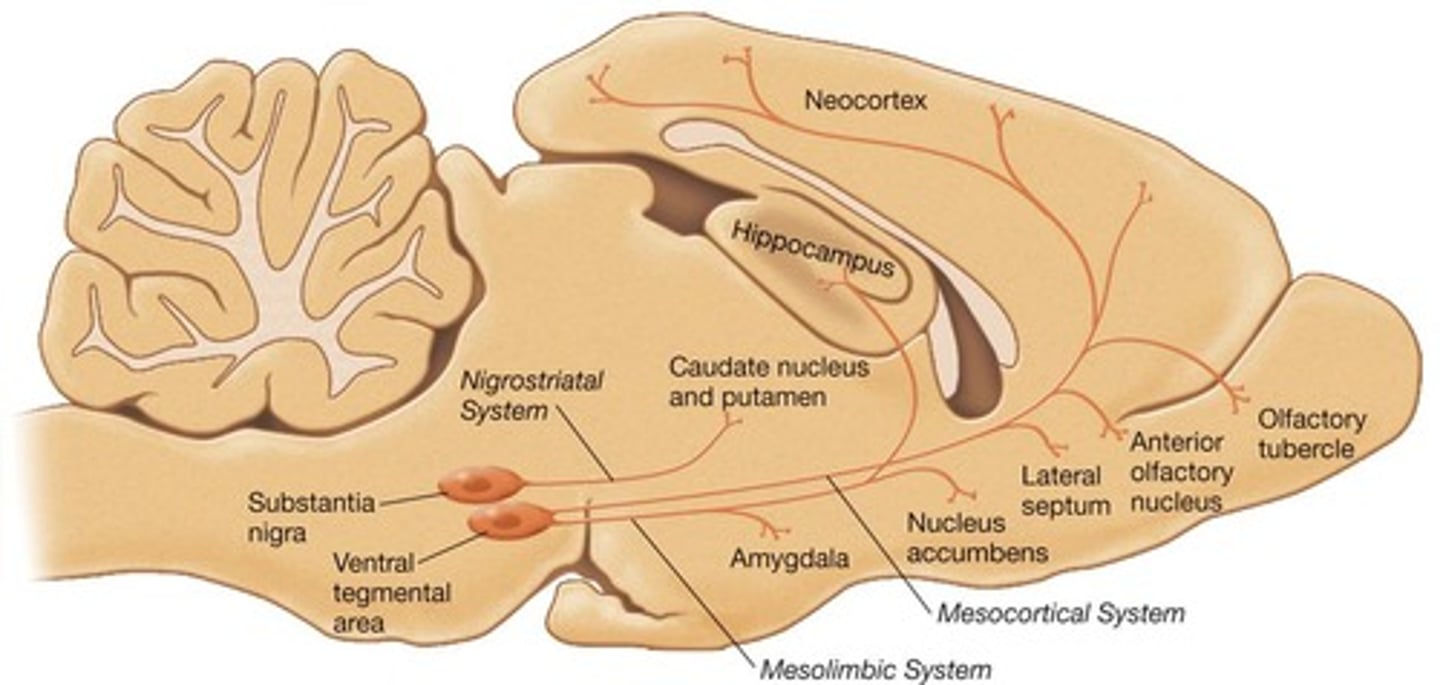
Dopamine Receptors
Five metabotropic receptors: D1, D2, D3, D4, and D5; D1 and D5 are excitatory (increase cyclic AMP); Effects depend on location of receptors; For example, D2 receptors are found on pre-synaptic membranes (auto-receptors) but also on post-synaptic membranes; Note: Post-synaptic D2 receptors in mesocortical pathway implicated in schizophrenia (anti-psychotics like chlorpromazine block D2 receptors).
Dopamine Re-uptake
Note: Stimulant drugs like cocaine, amphetamines, block dopamine re-uptake transporters; In fact, amphetamine and methamphetamine cause transporter to run in reverse which further increases DA in synapses!
Norepinephrine
Found in Brain and PNS (sympathetic NS). Most (nearly all) brain areas receive NE from pathways originating in pons. Locus coeruleus is the major source. NE leads to increased vigilance: attentiveness to environmental stimuli.
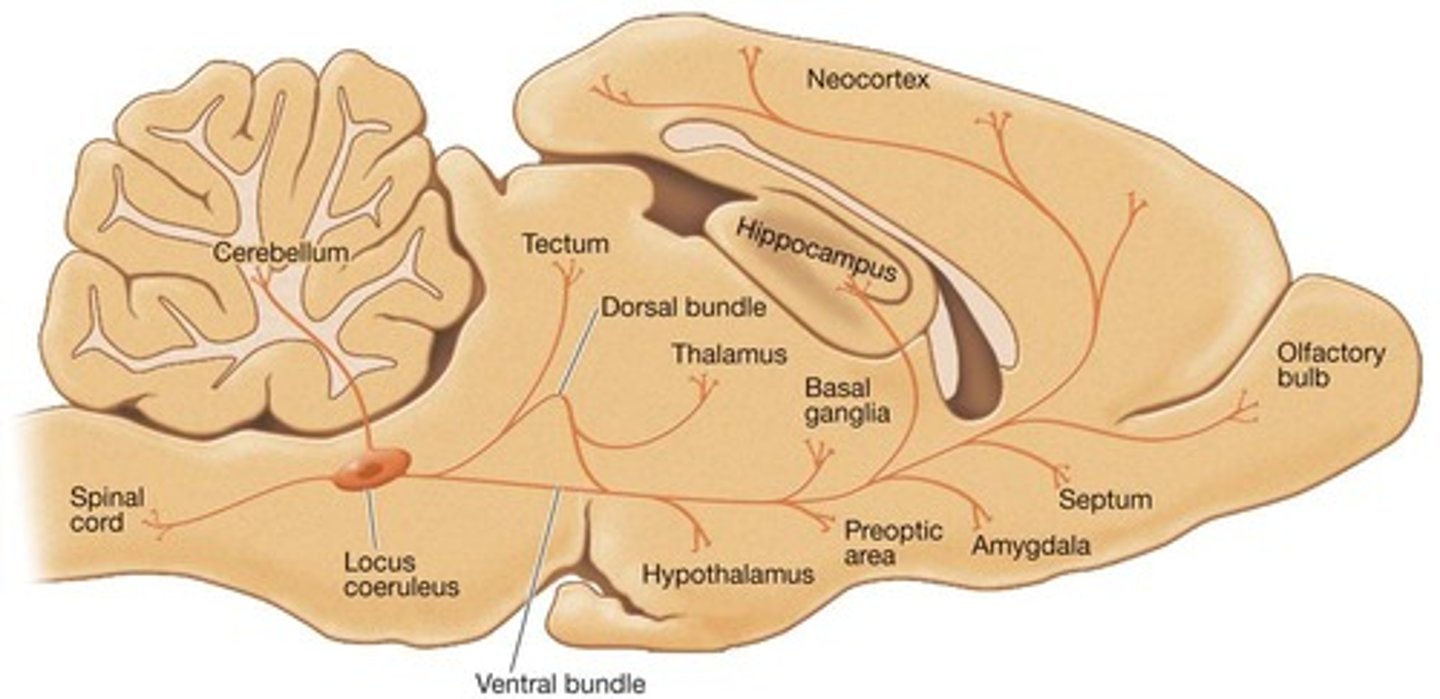
Norepinephrine Release
NE released from varicosities (swellings) along axons.
Norepinephrine Receptors
All metabotropic. Two families: α and β. α1 (excitatory), α2 (pre-synaptic auto-receptors), β1, β2 (excitatory).
Norepinephrine Termination
Catabolic enzymes (MAO or COMT) and re-uptake.
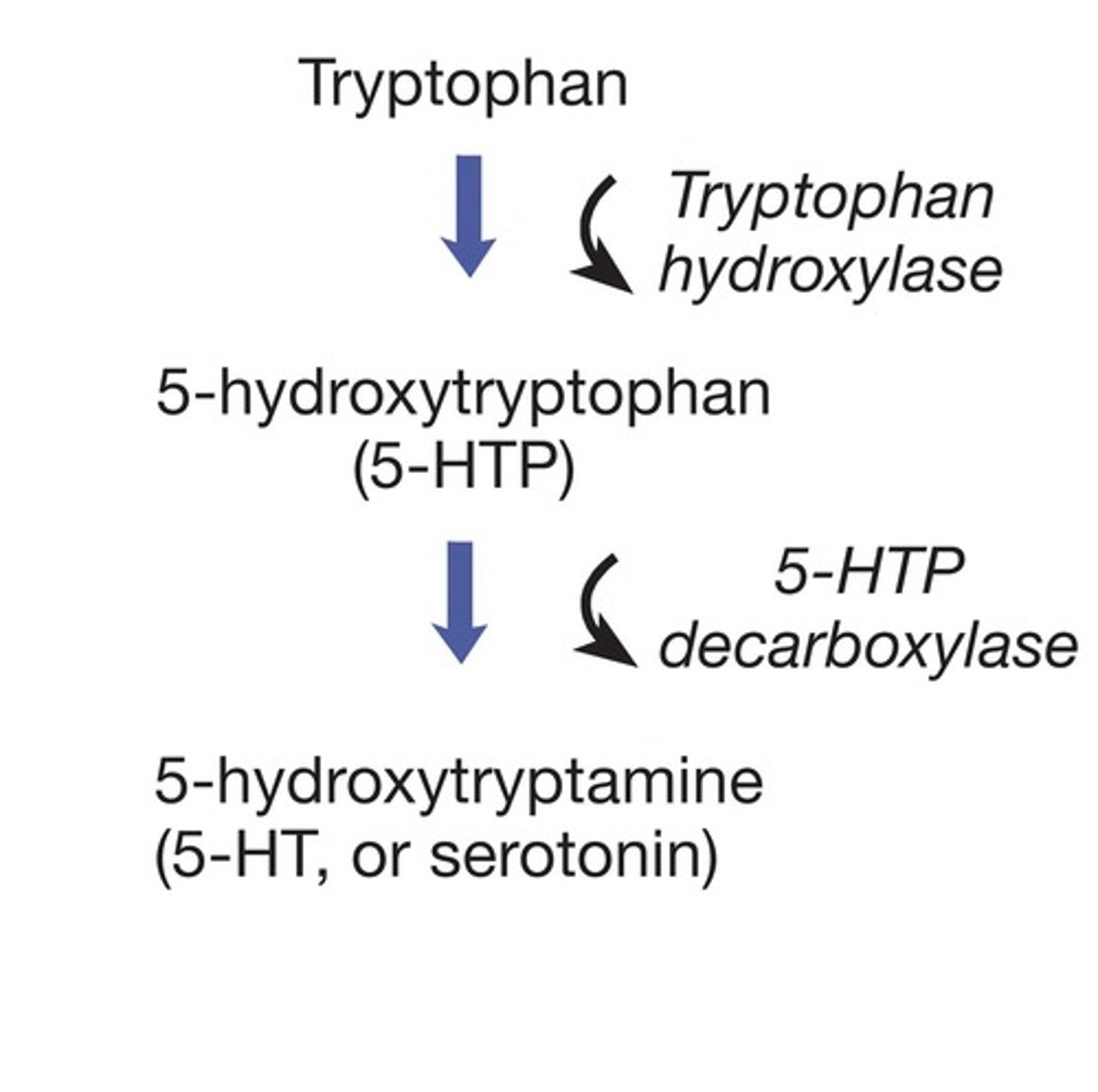
Serotonin
Synthesis: from tryptophan (AA). Plays role in regulation of mood; control of eating, sleep, and arousal; and pain regulation. Also involved in dreaming. Major source is raphe nuclei of the midbrain, pons, and medulla.
Serotonin Release
Released from varicosities, like norepinephrine.
Serotonin Receptors
At least 7 types: 5-HT1, 5HT2, etc. Most are excitatory. 5-HT1A serves as an inhibitory auto-receptor on somas and dendrites (remote from synapse).
Serotonin Termination
Monoamine oxidase (MAO) and re-uptake: serotonin transporters on pre-synaptic neurons. (SSRI antidepressants like Prozac block reuptake). MDMA (ecstasy) causes transporter to run in reverse (like METH and DA).
Histamine
Found in only one place in the brain: the tuberomammillary nucleus, located in the posterior hypothalamus. Plays important role in wakefulness. Drugs that block histamines (antihistamines) cause drowsiness.
Histamine Production
Produced from the amino acid precursor histidine by the action of the enzyme histidine decarboxylase. Stored in vesicles and released following an action potential.
Histamine Receptors
CNS contains H1, H2, H3, and H4 receptors. Antihistamines act as antagonists at histamine receptors.
Peptides
Peptides are two or more amino acids linked by peptide bonds. Produced (cleaved) from larger precursor molecules into smaller peptides. Produced in soma, transported to nerve terminals. Often co-released with another neurotransmitter. The best known are endogenous opioids (enkephalins). High concentrations in periaqueductal gray (midbrain).
Peptide Receptors
At least 3 opioids receptors (mu, delta, kappa). Produce analgesia (reduce pain). Inhibits defensive behaviors (fight and flight). Rewarding/euphoric effects: Site of action of morphine, heroin, oxycodone, fentanyl, etc. Naloxone is a competitive opioid receptor antagonist used to reverse opioid drug overdose.
Lipids
Lipid neurotransmitters appear to be synthesized on demand, produced or released as needed. Not stored in synaptic vesicles. Best known are endocannabinoids (anandamide). Involved in pain regulation, appetite (munchies). Act as retrograde signals, released by post-synaptic neurons back onto pre-synaptic neurons.
Lipid Receptors
Two types of cannabinoid receptors, CB1 and CB2. CB1 receptors located on pre-synaptic nerve terminals and decrease activity of the pre-synaptic neuron.
THC Effects
THC exerts analgesic effects by stimulating CB1. Acetaminophen also acts on these receptors (in periphery).