Touch, Temp, Pain
1/45
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
46 Terms
3 categories of somatosensorial
Exteroception
Interoception
Proprioception
Define the 3 categories of somatosension
Exteroception
Interoception
Properioception
Exteroception: (sensation from the skin in contact with the external world)
Interoception: (information sensation from internal organs provides information about internal functions digestion, etc)
Proprioception: (sensory receptors in the muscles and tendons to convey body position and movements)
Sensory system integrates all of these to
What do the three categories of somatosensory do?
They are integrated especially in the parietal cortex giving you an idea of what the organism is doing/feeling
Receptors responsible for touch
Subpain threshold stimulation → low threshold mechanoreceptors
Called low threshold because they require a low amount of sensation (not rising to the level of pain)
Axon coming in → dendritic tree which is modified by other cells (determines what is going to be sent to it)
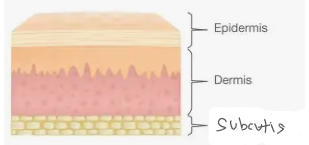
What are the 4 layers of skin called
Glabrous skin
Epidermis (outermost)
Dermis
Subcutis
What is the glabrous
Hairless skin
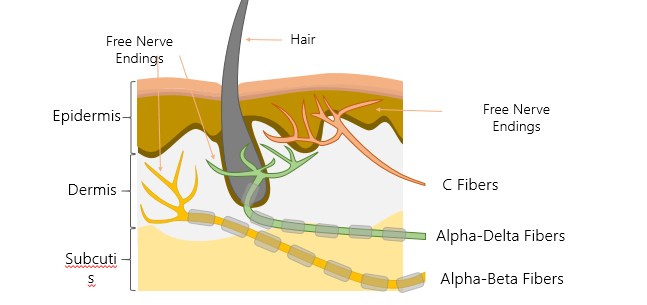
Free nerve endings
any skin area responding to pain and temp.
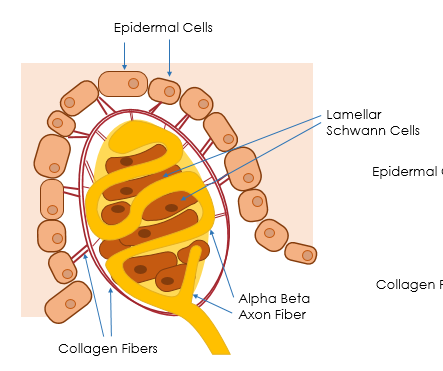
Anatomy if the Meissner corpuscle - what causes the feeling of touch here
The end of a nerve (dendritic branches) that can be modified by other cells
Lamellar Schwann cells - sandwiched in, additional cells separate them - modifies the activation
Collagen fibers connect them to the epidermal cells in the skin, so when you press on the skin, you will move the epidermal cells, causing a physical distortion of the receptor, triggering an action potential
A-beta fiber: Picks up this signal, converts it into an action potential, and rapidly conducts the signal to the spinal cord and brain.
4 different kinds of low threshold receptors innervating the skin
Merkel Disk → Found in glabrous and hairy skin, slowly adapting (type 1), responds to continuous pressure and low frequency vibration (slow changes)
Ruffini Endings → Found in glabrous and hairy skin, slowly adapting (type 2), responsive to continuous pressure and skin stretch
Meissner Corpuscles → Found in only glabrous skin, rapidly adapting (type 1), responsive to changes in pressure at a greater frequency
Pacinian Corpuscles → Found in glabrous and hairy skin, rapidly adapting (type 2),respond to the highest frequencies (vibrations)
All ab fibers
Response properties of each receptor
Merkel Disk → ////////////// (firing all along and not adapting to the pressure - why its a slow adapting receptor)
Ruffini Endings → /////// //
Meissner Corpuscles → // // (as soon as the skin is touched it fires and then adapts to the pressure and stops firing making it rapidly adapting and when you remove the pressure it fires again)
Pacinian Corpuscles → // //
Not equally destributes across your body
What are the threshold receptors connected by
Alpha Beta fibers which are myelinated and can communicate quite quickly (convey 20-100 meters per second)
Why do we respond to vibrations
you run your finger across things and textures = depressions and pressions = vibrations
We wouldn’t be able to understand texture (smooth vs bumpy) → high texture = high vibrations
This is also why we can detect sound depressing out skin
The ability to discriminate different kinds of touch depends on
How densely packed the reseptor’s are and how they are distributed through the body
How do we observe a region’s sensitivity to a point of touch, given a part of the body
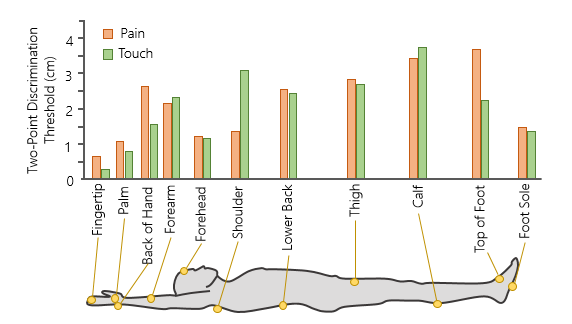
Simultaneous two-point discrimination test → looking for the discrimination threshold
On a bunch of trials, you do a single touch (25%) of the time
75% of the time you take two sharp objects and touch them to the skin at the same time - vary the distance between the two so that you can observe when they feel a difference
Discrimination threshold
The distance between two stimuli at which people are just able to tell they are being touched by two stimuli rather than one stimulus.
Not an exact point
where is two-point discrimination the longest/shortest
Longest in the calf, shoulder, thigh
Shortest in the fingertips, palm, back of hand *even here, receptors are not evenly distributed
depends on how many receptors there are
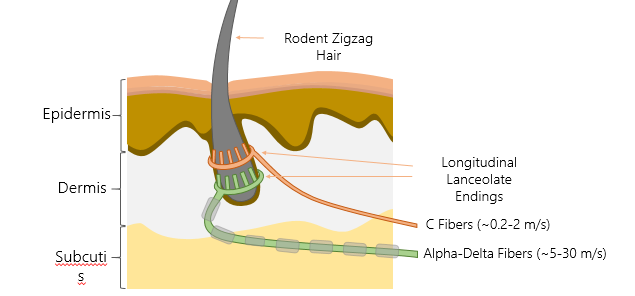
LTMR responsive to hair movement
Zigzag hairs are enervated by two different types of fibers: Alpha-Delta Fibers, which are mylenated and conduct action potentials at roughly 5 to 30 meters per second; and C-fibers, which are unmylenated, conducting the electrical signal at roughly 0.2 to 2 meters per second.
C fibers: non-myelinated (2m per second) move slowly
Alpha-Delta fibers: Myelinated (5-30 m/s) move Medium
Schwan cells surround
These are modifying the endings - helping the detection of fibers
How do hairs assist touch - why do we have mechanoreceptors surrounding the hairs
Allows you to sense things beyond the skin (movement of air)
Part of pleasurable touch is being registered by these hairs (at least one unmyelinated slowly conducting LTMO has endings localized strictly for pleasure)
Why we like when someone strokes your hair - you're feeling the deflection of hair and its sending sensory information
High threshold mechanoreceptors
Sensitive to more intense stimulation felt as pain - stimulation of free nerve endings not modified by other cells
connected to axons that are unmylinated (c-fibres) = dull, long main
As well as two fibers that are myelinated (alpha-delta and alpha-beta fibres) = sharp
2 - point determination in pain
Follows the same results of touch (you can take more pain in calf bc its less responsive to touch)
Shoulder is more sensitive to pain then to touch
Back of the hand has a small reversal
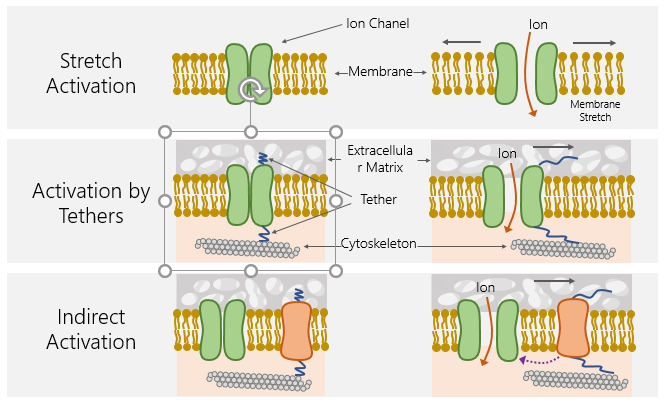
How do you take a deflection of the epidermis and transmit them into an action potential: stretch, tethers, indirect
Stretch activation: when stretch occurs the membrane pulls apart and physically opens the ion channel allowing ions to flow in and allowing for an action potential to be made
Activation by tehthers: part of ion channel attached to extracellular matrix by tether which is attached to cytoskeleton, when extracellular matrix moves it pulld the tether opens ion channel
Indirect Activation: other protien connected by tethers and when thoes tethers get pulled, they can release a messenger like a g protein that opens the ion channel indirectly
ALL ARE MECHANICAL
What does polymodal mean
polymodal receptor = a sensor in the body that can detect multiple kinds of input, not just one.
How is heat transduced
receptors sensitive to heat have a particular configuration and when you apply heat, you change this configuration of the ion channel - Changing the shape of the protein by heat
Transient reseptor potential vanilloid 1 (TRPV1) ion channel + heat
Ion channel opens, positive ions flow in
depolarization —> atp
What happens to TRPV1 when capsaicin is introduced?
Introduction of a hot food
Capsasin binds to ion channels and then your brain codes as a temperature change because its attaching to the came channel
This will open ion channels and depolarize the cell triggering the same responses as heat
These then become called polymodal ions because they not only respond to heat but also respond to chemicals (ligand gated)

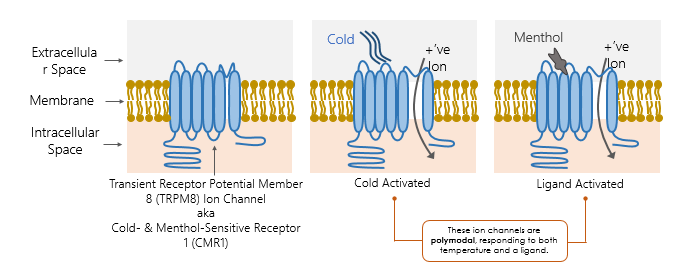
What happens in the case of the cold
Transient Receptor Potential Member 8 (TRPM8) Ion Channel aka Cold- & Menthol-Sensitive Receptor 1 (CMR1) → same name
Can be depolarized by the intoduction of cold or even menthol (ligand gated)
Also polymodal
what temps are the different TRP ion channels responsive at
TRPM8 → most responsive at 10
TRPV1 → Most responsive at 50
TRPV2 → Most responsive at 58
This info tells us if something is hot or cold
How does info flow from receptors into the cns
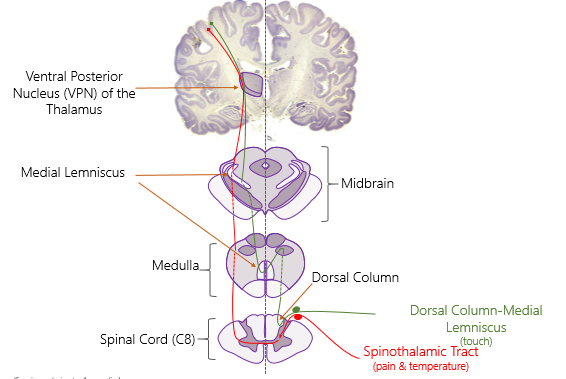
Touch info is transferred separately from pain and temperature - two major pathways:
In the spinal nerve → dorsal root carrying sensory info → synapse formed in the spinal cord and info moves up the spinal cord into brainstem and the brain
Seperation happens:
Pain and temp (high threshold) will cross sides travelling controlateral to the Spinothalamic Tract
Touch (low threshold mechanoreceptors) going up the Dorsal-column medial-lemniscus on the ipsoladeral side of the spinal cord (same side the signal is coming from)
Once it gets to the modella touch will cross and everything is now controlateral
Mild pain vs intense pain neurotransmitters
Mild pain releases glutamate
Stronger pain releases glutamate and neuropeptides, substance P and CGRP.
What would happen if you sliced above C8
You would have touch and pain coming info in but touch info is staying on the same side and is trying to travel up but youve vut the signal - not getting any touch info from that side
But the pain info has crossed over at the side that you didn’t cut
You will loose touch info from the cut side but you don’t loose pain info from that side
Shows that info travels on different sides of the spinal cord
What is the dermatome
a part of skin serviced by a single spinal nerve
Damage to that spinal nerve would equal loss of sensation in that part of the skin
What are the different sections of the spine (5)
Cranial → head
Cervical → collarbone, neck and arms/fingers
Thoracic → mid section, underarm
Lumbar → hips down
Sacral → tailbone/groin + outside of the foot
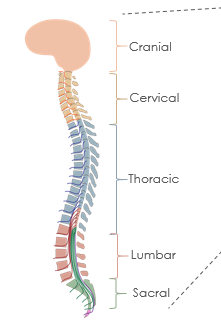
Groups of spinal nerves
Cranial nerves
Cervical nerves (8 pairs)
first thoracic vertebra +thoracic nerves (12 pairs)
lumbar nerves (5 pairs)
sacral nerves (5 pairs)
coccygeal nerves (1 pair).
Where is the trigeminal nerve
Cranial spine
Within the brain, what is the pathway for touch
From C8 → medulla (touch crosses over) → to midbrain through medial lemniscus → to the ventral posterior (only one part) nucleus in the thalamus → primary somatosensory cortex (parital lobe)
When we get to the somatosensory what happens
It gets divided into sections of specialization
S1: codes for texture of objects, and pain
S2: codes for size and shape of objects
3B: size, shape, and texture as well as pain
3A: movement of joints, tendons and muscles as well as some types of pain

Numb sense
when the primary sensory cortex (s1) is inactive, some people correctly “guess” the location of a touch while insisting that they did not consciously feel it.
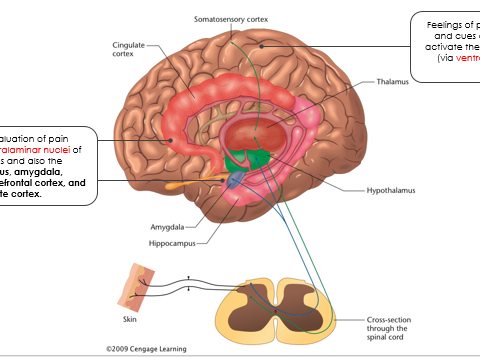
How does pain trigger an emotional response
Emotional evaluation of pain: intralaminar nuclei of the thalamus and also the hypothalamus, amygdala, hippocampus, prefrontal cortex, and cingulate cortex (giving you an innate emotional relay)
The idea of the pain is what makes it bad (like going to the gym we are ok)
Some therapies adress this and rething the pain
Feelings of pain, memories, and cues associated with pain: somatosensory cortex (ventral posterior nuclei)
Does experiencing pain make you getter at handling pain
The more you are exposed to pain, the more sensitive to pain you will be
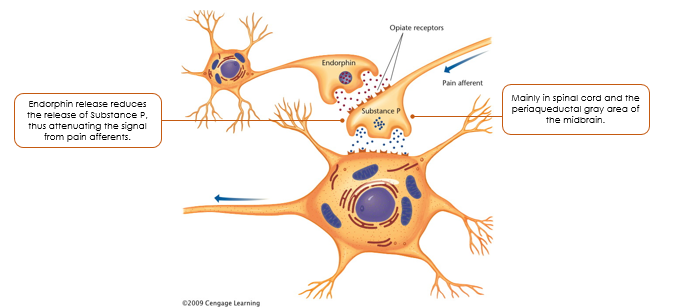
Periaqueductal gray area
the area of the brainstem that is rich in endorphin synapses.
Relieving pain with opiates
morphine:
The signal for pain comes in afferently → Pain cells in the periaquiductal grey area of the midbrain releases a neurotransmitter called substance P signaling pain and giving you that experince
We also have these cells that release endorphins which attach to the same receptors as morphine, the brain produces several types to relieve different types of pain → reduces the release of substance P
Other ways to relieve pain
A placebo (a drug or other procedure with no pharmacological effect) can reduce pain responses in the brain and in the spinal cord
even though the chemical itself is not having any effect the psychological belife triggers system like medicine = physilogical effect
Cannabinoids (in marijuana) block pain in the periphery of the body (as well as the CNS) - Capsaicin can also help release pain.
Neural inhibitors
Problem with using neural inhibitors as pain relive
Can inhibit different parts of your brain (mess with speech)
Gate theory
the idea that stimulation of certain axons can close the “gates” for pain messages.
Spinal cord neurons that can receive messages from pain receptors also receive input from other inputs that can close the gates for the pain messages
Nav1.7
The “pain signal starter.”
The 7th type of voltage-gated sodium channel, important for axons conveying pain and olfactory sensations; psychologists are developing drugs to block Nav1.7 for chronic pain.
Nocebo effect
opposite of placebo, the unpleasant reaction to a drug is increased by the nervous system.
Itch sensation
2 typessomething mechanical (crawling on skin) and tissue damage (histamines dilating blood vessels producing the itching sensation).
Inhibitory relationship between pain and itch; decreasing itch increases pain and decreasing pain increases itch.