Regulation of potassium balance
1/23
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
24 Terms
What foods are high in potassium?
pinto beans
tomato paste
raisins
baked potato
steak
Internal vs external potassium balance
Internal: (quick process) Controls distribution of potassium between ECF and ICF
External (slow process): Regulates renal potassium excretion to balance potassium intake
Factors that shift potassium into cells
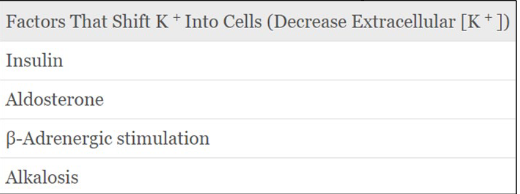
Factors that shift potassium outside of cells
How does insulin cause potassium to move into cells
increased plasma [K+] depolarises β pancreatic cells→ release insulin → stimulates K+ uptake by muscle cells and liver via an increase in Na- K-ATPase
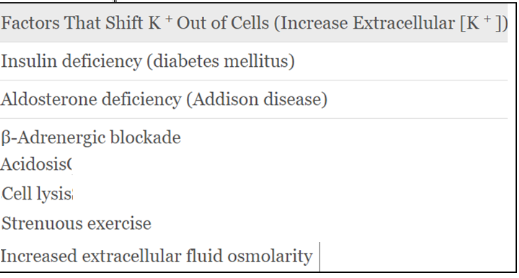
How does acidosis and alkalosis affect potassium levels?
Acidosis: shift of H + into cells → reciprocal K+ shift out of cells → Hyperkalaemia
low pH blocks Na+ - H+and Na/HCO3- → more H+ in cell → inhibits Na+/K+ pump and Na-K-Cl transporter
Alkalosis: shift of H + out of cells → reciprocal K+ shift in to cells → Hypokalaemia
How does a high plasma osmolarity affect potassium?
1. Water moves from cells into ECF (because of the osmotic gradient)
2. Cell shrinks
3. Increased [K+ ] in ICF
4. K+ leaves down concentration gradient
What other factors can cause hyperkalaemia?
cell lysis
strenuous exercise: K+ is released from skeletal muscle into ECF
In what ways do we regulate external potassium balance?
-ve feedback regulation: Reactive dependent from k+ conc
food-forward regulation: reactive independent from K+ conc
Predicative: follows circadian rhythm so kaliuresis is higher in the day
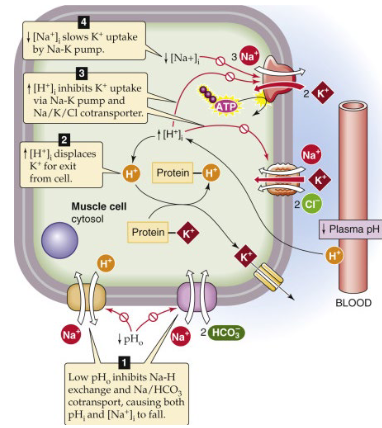
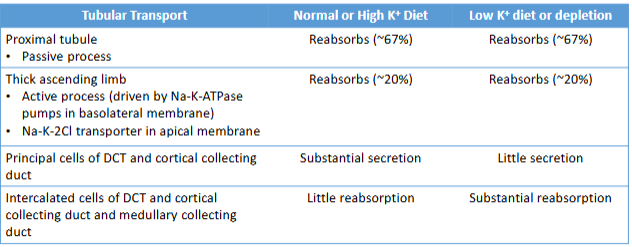
Where is potassium usuaully reabsorbed and secreted in the nephron?
reabsorbed: mostly PCT + loop of Henle
secreted: distal tubule + cortical collecting duct (unless K+ is low then it can reabsorb)
How is potassium secreted in the principal cells of the collecting duct?
Na + is reabsorbed through ENaC
Stimulates basolateral Na + /K+ - ATPase → K+ actively pumped into the cell
from the peritubular fluid
K+ (passively) secreted at the apical membrane by K+ /Cl - cotransporters and K+ channels (ROMK)
What peritubular factors affect principal cell potassium secretion?
High Plasma [K+ ]:
Directly stimulates Na-K-ATPase
↑permeability of apical K+ channels
stimulates aldosterone secretion
Aldosterone:
↑ Na-K-ATPase
↑ ENaC in apical membrane
↑ K+ channels
Acid base balance
Acidosis:↓ K+ secretion: inhibits Na-K-ATPase, ↓ K+ channel
permeabilityAlkalosis: ↑ K+ secretion: stimulates Na-K-ATPase, ↑ K+
channel permeability+ channels
What luminar factors affect principal cell potassium secretion?
Flow of distal tubular fluid:
Increased flow rate increases K+ secretion
Decreased flow rate reduces K+ secretion
[Na+ ] delivery to distal tubule:
Increased [Na + ] delivery to distal tubule → increases K+ secretion
Decreased [Na + ] delivery to distal tubule → decreases K+ secretion
How does potassium get absorbed in the intercalated cells?
** alpha- intercelated cells
K+ actively absorbed from the duct lumen through an apical H + -K+ -ATPase (** if a lot of K+ is reabsorbed there is an increase in H+ secretion → alkalosis)
K+ exit from intercalated cells into the blood is mediated by a K+ channel
Why would you get pseudohyperkalaemia?
artefactual increase in serum K+ caused by the release of K+ during venepuncture (haemolysis)
What might lead to redistribution of potassium from ICF to ECF
Acidosis (inhibits Na +/H+ exchange)
Diabetic ketoacidosis (inhibits Na +/K+-ATPase; increases plasma osmolality)
Drugs: Beta blockers, digoxin (inhibit Na +/K+- ATPase)
What can cause impaired renal potassium excretion?
Acute or chronic renal failure
Tubular disease
Lack of aldosterone (Addison’s disease)
ACE inhibitors/ ARBs
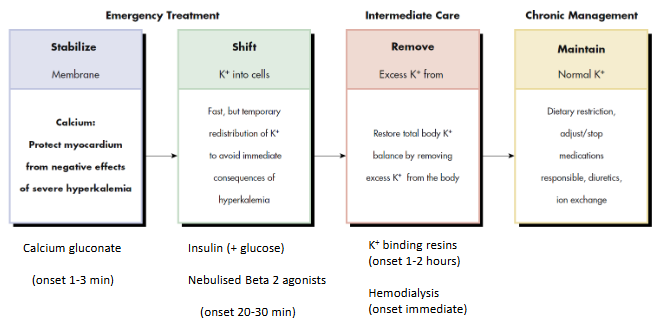
How do you manage hyperkalaemia?
Causes of hypokalaemia?
Decreased intake: Alcoholism; anorexia
Increased loss:
Extra-renal loss: GI – diarrhoea/vomiting
Renal loss
• Diuretic drugs
• Osmotic diuresis
• High aldosterone levels
• Hypomagnesemia
• Renal potassium transport defects
Symptoms of hypokalaemia
Heart: altered excitability → arrhythmias
Gastrointestinal: neuromuscular dysfunction →constipation, paralytic ileus
Skeletal muscle: neuromuscular dysfunction → muscle cramps, weakness
Renal: dysfunction of collecting duct cells → unresponsive to ADH →
nephrogenic diabetes insipidus
Treatment of hypokalaemia
identify underlying cause
potassium replacement: oral/ IV (if severe ,2.5mmol/l)