Midterms Equine
1/78
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
79 Terms
•____are parasitic, spore-producing organisms.
•They obtain their nourishment by absorbing food from the hosts on which they grow.
•Many species of fungus exist in the environment, but only some cause infections.
• The primary source of most infections is ____
• Fungal infections can be acquired by inhalation, ingestion, or through the skin (for example, through a cut or wound).
•Some fungal infections can cause disease in otherwise
•healthy animals, while others require a host that is _____ (by, for example, such stresses as poor nutrition, viral infections, or cancer) to establish infection.
•Prolonged use of _____appears to increase the likelihood of some fungal infections
•. The infection itself may be localized or may affect the entire body _______
Fungi
soil.
incapacitated or immunocompromised
antimicrobial drugs or immunosuppressive agents
(systemic or generalized
Classification of fungal dermatological infections based on location
1._______-
o confined to the stratum corneum and does not affect hairs
o little or no tissue reaction or inflammation
o facultative pathogens or commensals rather than primary pathogens
o secondary seborrheic changes resulting in excessive scales and flakes on the skin
o little immunological or cellular response
oEx. ______
Superficial mycoses
Malassezia spp.
2. ______
o all keratinized tissues including hair, horn and skin
o causes significant destruction of keratinized tissue with immunological response from host
3. ___________
o involve subcutaneous tissues in addition to dermal/epidermal involvement
o some localized, others spread insidiously to contiguous tissues and via lymphatic vessels
o difficulties with diagnosis and treatment
o with ______, most are chronic and progressive
o more serious but geographically restricted
o rare or very rare in horses
Cutaneous mycoses
Subcutaneous/deep mycoses
seroconversion
_____
Characteristics
o very common cutaneous mycosis caused by ______
o worldwide in distribution
o spores highly resistant, repeated infections occur in stables/yards
o requires epidermal damage to gain entry and remain in follicles of hair shafts
o site of infection areas of superficial skin trauma (tack and harness contact points)
trichophytosis
Trichophyton spp.
Clinical Signs of ______
1.Early clinical signs are erect hairs, local swelling/edema wild mild exudate
2.Complete shedding of hairs, lesions easily and completely epilated leaving silvery exposed epidermis
3.Abrasions of rider’s boots and girths common sites of infection
Diagnosis
1.Clinical signs
2.Differential diagnosis with other fungal diseases with similar symptoms
3.Biopsy
Treatment
1.Isolation of infected horse
2.Hygiene and sanitation to prevent spread between horses and humans
3. _________ (not for pregnant mares)
4. Use of fungicidal disinfectants such as sprays and washes for tacks and harness
Control
1.Vaccination in some countries
2.Early recognition and isolation of infected horses
3.Stable and personal hygiene best ways to prevent spread
4.Individualized tack, harness and rugs
5.Use of gloves
trichophytosis
Topical antifungal washes and oral griseofulvin
_________
Characteristics
o less common than Trichophyton spp. Infections
o isolated lesions more common than extensive coalescing areas
o pathogenesis same as trichophytosis
o common species _____
o spores and active mycelia survive for____ in beddings, wooden poles and tacks/blankets and harness
Clinical Signs
1. First as small expanding areas of localized edema resembling urticaria
2. Early lesions with exudate and mildly pruritic; horse rubs affected areas but does not bite
3. _____resented because not all hairs are affected
Diagnosis
1. Clinical signs
2. Cultures and microscopy of stained smears and hairs
3. Secondary urticarial-like plaques
4. Differentiate from Pemphigus foliaceus, sarcoid and insect bite reactions
microsporosis
M. equinum, M. canis, M. gypseum
months
Plucking of hairs
Treatment of microsporosis
1.Local topical washes with fungicide: _____; clip off hair around defined lesions
2.Environmental disinfection
3. _____ strong inhibitor of Microsporum spp.
o Prognosis excellent, most resolved spontaneously within_____
o To prevent spread to other horses and humans, treatment should be instituted
natamycin, enilconazole or miconazole
Sunshine
6-12 weeks
___________
is a fungal infection caused by several ________
•It is primarily a respiratory infection that may become generalized.
• is found worldwide and in almost all domestic animals as well as in many wild animals; however, the susceptibility to fungal infections varies among species.
•The most common form in horses is fungal disease affecting the_____
•The 2 guttural pouches are sacs formed by the auditory tube, which connects the middle ear with the back of the throat.
• Infection usually occurs only in ____ guttural pouch. The infected guttural pouch becomes thickened, and bleeding into the tissue may occur.
•___________or swallowing are common signs.
• Other signs include holding the head extended or low, head-shaking, swelling of the head, neurologic signs, and nasal discharge.
• Topical and oral antifungal agents have been reported to be effective in cases of Aspergillus infection.
• The outlook is guarded; horses may survive but not recover completely, particularly if the nerves are damaged.
Aspergillosis
(Guttural Pouch Mycosis)Aspergillus species.
guttural pouch.
1
Nosebleed and difficulty in breathing
is a localized fungal disease affecting the mucous membranes and the skin.
•It is distributed worldwide in a variety of animals and is most commonly caused by species of the yeast-like fungus, _______
•Superficial infections limited to the mucous membranes of the intestinal tract have been described in foals.
•Widespread candidiasis has also been described in foals undergoing prolonged antibiotic or corticosteroid treatment.
• Infections are rare in horses. However, Candida species have been considered a cause of arthritis in horses
•Signs are variable and nonspecific and may be associated more with the primary or predisposing conditions than with the candidiasis itself.
•An ointment or topical application may be useful in the treatment of oral or skin candidiasis.
•Your veterinarian may also recommend different drugs given by mouth or through the vein to successfully resolve arthritis induced by________ infection in a horse or to treat generalized candidiasis in foals.
Candidiasis
Candida albicans.
Candida fumata
is a dustborne, noncontagious infection caused by the fungus ___________
• Infections are limited to dry, desert-like regions of the southwestern United States and to similar areas of Mexico and Central and South America.
•Inhalation of fungal spores (often carried on dust particles) is the only established mode of infection.
•Epidemics may occur when ____ periods are followed by drought, resulting in dust storms.
•The disease varies from infections with few or no signs to progressive, disseminated, and fatal forms.
•In horses, the most common signs include loss of weight, coughing, fever, musculoskeletal pain, and abscesses of the skin.
•Placental infections leading to abortion and inflammation of bone have been described in horses.
•A diagnosis is confirmed by identifying the fungus in body tissues.
• may resolve without treatment, but if chronic respiratory signs or multisystemic disease are present, longterm antifungal treatment is needed.
•At the present time there is no known prevention other than decreasing your horse’s exposure to the desert soil and dust as much as possible in areas where the fungus is known to exist.
Coccidioidomycosis (Valley Fever)
Coccidioides immitis.
rainy
is a systemic fungal disease.
• The causal fungus,_______, exists in the environment and in tissues in a yeast form.
•The fungus is found worldwide in soil and bird manure, especially in pigeon droppings.
•Transmission is by inhalation of spores or contamination of wounds. Cryptococcosis is uncommon in horses.
•The disease in horses is, almost invariably, a respiratory ailment with obstructive growths in the nasal cavities.
•Diagnosis is based on microscopic examination of exudates
or samples from masses.
•The yeasts have a distinctive appearance. Treatment for may include ____ to remove lesions in the nasal cavity. Various antifungal drugs can be used for the treatment of cryptococcosis.
Cryptococcosis
Cryptococcus neoformans
surgery
is a disease that affects the skin, lymph vessels, and lymph nodes of the limbs and neck of horses.
• It is caused by the fungus _____
•Infection seems to be limited to horses, donkeys, and occasionally mules.
• Epizootic lymphangitis occurs in Asian and Mediterranean areas but is unknown in the United States.
• Infection probably is acquired by wound infection or transmission by bloodsucking insects such as mosquitoes.
•The disease most typically involves the skin and associated lymph vessels and nodes.
•Occasionally there is involvement of the respiratory tract.
•Some horses develop small, inconspicuous lesions that heal spontaneously.
•More typically, nodules develop under the skin. These increase in size and undergo cycles of granulation and partial healing followed by renewed eruption. The surrounding tissues become hard, painful, and swollen.
•Lesions may be seen on the skin of the face, around and in the eyes and nose, and on the forelegs, thorax, neck, and occasionally the inside of the rear legs.
•Other internal organs may be involved.
•Diagnosis can be confirmed by microscopic examination of discharges from the infected area or biopsy specimens because the yeast forms have a distinctive appearance.
•No completely satisfactory treatment is known.
• ________ combined with antifungal drugs may be tried.
•In most areas of the world, however, this is a reportable disease; treatment of animals is not permitted, and destruction of affected horses is usually mandatory
•Strict hygienic precautions are essential to prevent spread of epizootic lymphangitis.
•Great care should be taken to prevent spread on grooming or harness equipment
•Contaminated bedding should be burned. The organism may persist in the environment for many months
Epizootic Lymphangitis
Histoplasma farciminosum.
Surgical removal of lesions
is a disease caused by ______, which is not a true fungus but a water mold.
•It occurs in some tropical and subtropical areas of the world and is seen in warmer sections of the US. In the US, the disease most often is seen in fall and winter months.
•____ are the most commonly affected animals, followed by dogs and, rarely, cats and people
•Infections in horses are most commonly restricted to the skin and the tissues just inside the skin.
•There may be large, circular nodules or areas of swelling that can become open, draining sores These lesions are
•usually on the lower legs, abdomen, and chest but may occur anywhere on the body. The lesions are usually intensely itchy, and horses may mutilate the wounds if not closely monitored.
•Skin lesions often contain firm, yellowish masses of dead tissue known as ____
•Following the initial infection, the organism may spread to distant areas through the lymph system. The lymph nodes, bones, or lungs may be involved.
•Horses rarely develop gastrointestinal disease similar to that occurring in dogs.
• Horses with ______- may have signs of gastrointestinal obstruction, weight loss, poor appetite,
•diarrhea, and acute abdominal pain. In other horses, gastrointestinal disease may be unaccompanied by signs of generalized illness.
•A diagnosis may be based on the appearance of the distinctive lesions and confirmed by identification of the organism in infected tissues.
•Surgical removal of lesions, antifungal treatment, treatment directed at the immune system, or a combination of these may be recommended to treat affected horses.
•The outlook is guarded, but timely recognition and treatment may lead to a more successful outcome. Other factors that influence the outlook include the size and location of lesions and the length of infection.
Pythiosis
Pythium insidiosum
Horses
“kunkers.”
gastrointestinal pythiosis
is a general term for an infection by any of a number of fungi of the family Dematiaceae.
• This type of fungal infection is uncommon in horses.
•The fungi known to cause phaeohyphomycosis have been recovered from decaying vegetative matter and soil all over the world.
•Infection may result when the fungus enters the body at the site of an injury.
•In most cases, the infection is confined to the skin and tissues beneath the skin.
•The most common signs include nodules in the skin, upper respiratory signs, and masses that form in the lining of the nasal passages and on the legs and chest.
•The nodules may ulcerate and have draining tracts. The condition is diagnosed by microscopic examination of discharge from a mass or biopsy.
•Surgical removal of the lesion can be a cure.
•Treatment with antifungal drugs may be considered in cases when surgery is not possible.
•Antifungal treatment is long term (6-12 months), expensive, and has variable results.
Phaeohyphomycosis
is a chronic infection, primarily of the lining of the nasal passages and occasionally of the skin.
•It is caused by the fungus ________ and is rarely fatal.
•Uncommon in North America, it is seen most often in India, Africa, and South America.
•This disease is not considered transmissible.
•Infection of the nasal mucosa is characterized by polyp-like growths that may be soft, pink, crumbly, and lobular with roughened surfaces. The growths may become large enough to obstruct or close off the nasal passages
•The skin lesions may be single or multiple, attached at a base or have a stem-like connection. Signs of infection include nasal discharge and sneezing.
•Surgical removal of the lesions is considered to be the standard treatment, but recurrence is common.
Rhinosporidiosis
Rhinosporidium seeberi
is a sporadic chronic disease caused by ________
•The organism is found around the world in soil, vegetation, and timber.
•In the United States, Sporothrix schenckii is most commonly found in coastal regions and river valleys.
• Infection usually results when the organism enters the body through skin wounds via contact with plants or soil or penetrating foreign objects such as a sharp branch.
•Transmission of the disease from animals to humans can occur.
•The infection may remain localized to the site of entry (involving only the skin) or it may spread to nearby lymph nodes.
•Both of these forms occur in horses.
•Small, firm nodules develop at the site where infection enters the body. Although generalized illness is not seen initially, chronic illness may result in fever, listlessness, and depression. Rarely, infection will spread through the bloodstream or tissue from the initial site of inoculation to the bone, lungs, liver, spleen, testes, gastrointestinal tract, or central nervous system.
•To diagnose sporotrichosis in horses, it may be necessary to take samples of infected tissues, culture them, or examine them with a microscope to find yeasts with a typical appearance.
•Longterm treatment with antifungal drugs (continued 3 to 4 weeks beyond apparent cure) is usually recommended.
•Alternatively, a solution of _________, administered by mouth, has been used with some success; treatment is continued 30 days beyond apparent cure.
•During treatment, the horse should be monitored for signs of iodide toxicity.
•Because sporotrichosis can be passed from your horse to you, strict hygiene must be observed when handling animals with suspected or diagnosed sporotrichosis.
Sporotrichosis
Sporothrix schenckii.
potassium iodide
•Species specific
•Three subfamilies: alpha, beta (none in horses), gamma
•9 documented strains, but only ___ affect domestic horses
•Only ___________commonly cause diseases in horses
Equine Herpes Virus
5
EHV1, EHV3 and EHV4
_________
a.Rhinopneumonitis (respiratory form)
b.Abortion
c.Birth of weak foals
d.Peracute vasculitis – lungs; fatal in adults
e.Neurological
1.EHV-1 (a) - Subtype 1 of EHV1
•__________ is common throughout the world and most important viral cause of abortion in horses
•Can be sudden and deadly
•High temperature
•_______ respiratory disease
•May see all 5 of the syndromes at once
•Horses of all ages are affected
•Mares_________pregnant most susceptible
•_________ first identified in the 1940s
EHV-1
“Fulminating”
3-9 months
Abortion storm virus
Mode of Transmission
•Horse to horse by direct contact, nasal secretion, reproductive discharge, placenta or aborted fetus
•Short-distance airborne spread also possible
Clinical Signs
•Viral incubation for__________
1.Fever (__________)
2.Malaise, depression, anorexia
3.Congestion and serous discharge from the nostrils
4.Swollen lymph nodes
5.Mild incoordination to severe ataxia, paresis and paralysis
6.Loss of bladder tone, tail tone, skin sensation in hind limbs
EHV1
2-10 days
38.8 to 41.6’C for 1-7 days
Diagnosis of EHV1
1.Fluorescent antibody, PCR
2.Virus isolation from fetal tissues
3.Differential diagnosis with ______and other resp dss
EI, EVA
Treatment of EHV1
1.Supportive nursing
2._____to control malaise and fever; will encourage eating
3.Fluid therapy if dehydrated
4.Antibiotics to prevent secondary bacterial infection (especially if respiratory disease); _______ 30mg/kg,PO, bid
5._____ to reduce nerve inflammation
•If horse remains standing, prognosis is _____
NSAIDs
Valacyclovir
Corticosteroids
good
Prevention of EHV1
1.Vaccination at ______month of gestation
2.Prevent exposure to other horses attending shows or other equine events
5, 7 and 9
2._____
•Venereal disease
•________
•Rare but important
•Doesn’t cause death
•Self-limiting
•Characteristic lesions on genitalia of stallions and mares
EHV-3
Equine Coital Exanthema
3.____
•Subtype 2 of EHV1
•Respiratory infection only (“Rhino”); ________
•Non-fatal, rarely results in abortion
•Severe, widespread outbreaks in young horses; foals → 3 years old in training
•Not a problem in older horses (develop immunity)
EHV-4
rhinopharyngitis and rhinotracheitis
4._____
•Gamma family
•“Ubiquitous” but rarely causes disease
•Found in nearly 100% of healthy foals
•Can cause problems in the following diseases:
1.EHV2 - _________ in young foals; may act as a forerunner that leads to Rhodococcal infection (through immune suppression)
2.EHV5–_____________; in middle-aged horses
EHV-2 and EHV-5
Herpetic keratoconjunctivitis
equine multinodular pulmonary fibrosis (EMPF)
•Has emerged as a pathogen (EMPF)
Clinical Signs
1.Tachycardia, tachypnea, increased inspiratory effort and poor body condition
2.Wheezing and crackling, maybe mistaken as _____
•Associated with lymphoproliferative diseases and lymphoma
EHV5
heaves
Diagnosis of EHV5
1. CBC – ________
2.Thoracic radiographs
3.Virus-specific PCR test on pulmonary secretions or percutaneous lung biopsy sample
•Prognosis for survival is approx. ___
neutrophilic leukocytosis with or without hyperfibrinogenemia and anemia
50%
Treatment of EHV5
1.___30 mg/kg, PO, tid and/or _____10ng/kg, IV in 1L of isotonic crystalloid fluid as infusion over 1 hour, bid for 2 days
2.____ – 5 to 10mg/kg, PO, 1-2 times daily; for 2ndary bacterial infection and anti-inflammatory properties
3. _____ – 0.08-0.1 mg/kg IV very 24-48 hours; reduction of pulmonary cytokines and inflammatory mediators; cause immunosuppression and enhance viral replication
Valacyclovir
acyclovir
Doxycycline
Corticosteroid
Diagnosis of EHV
•PCR and isolation of virus from nasopharygeal swabs and blood samples during early stage of infection
Treatment
• Anti-inflammatory drugs
•IV fluid
•Antibiotics for secondary bacterial infection
Prevention
•Vaccination
Control
•Biosecurity practices
•Arthropod-borne viruses that cause central nervous system dysfunction and moderate to high mortality
•Caused by alphaviruses of the family Togaviridae
•Endemic in North, South and Central America
•Western (WEE) - 20-50% fatal
•Eastern (EEE) - 50-90% fatal
•Venezuelan (VEE) - 50-75% fatal
•Highland J virus, Everglades virus
•Semliki Forest virus – East and West Africa
•Japanese encephalitis virus (JEE/Flavivirus) – Asia, India, Russia, Western Pacific – 35-45%
•Madariaga (MADV/Flavivirus) in South America and Caribbean
•WNV (Flavivirus) in Africa, Middle East, Europe, NSC Americas, Australia
Equine Arboviral Encephalomyelitis
Transmission of
1. ____
•Transmitted by mosquitoes; not horse-horse or horse-human; dead-end hosts
•Life cycle of alphaviruses between birds/rodents and mosquitoes
•Sylvatic cycle between passerine birds and _____
EEE
Culiseta melanura
Transmission
2.MADV principal vector belong to ____
3.WEE transmitted by ____
4.VEE in jungle or swampy areas; two life cycles, the ____ cycle “paddling”
a.Enzootic – mosquito (____) serves as primary vector for bird/rodent-mosquito life cycle; sylvatic rodents spiny and cotton rats
b.Epizootic – mutation to subtype I (A, B, C and possibly E) with change in mammalian pathogenesis
b.and several bridge vectors; horse infection becomes predominant feature in maintenance of epizootic ___
•All encephalitides caused by ____ transmitted by mosquito, Culex spp usually the most efficient
5. ____ – widest geographic distribution of all flaviviruses
Culex (Melanoconion) spp
C. tarsalis, Dermacentor andersoni
enzootic and epizootic
ci
VEE
Flaviviruses
WNV
Equine Encephalomyelitis
Clinical Signs:
•Neurologic signs occur____ days after infection
1.Quiet and depressed
2.Ataxia, wandering, impaired vision, reduced reflexes, circling, inability to swallow, drooling, fever
3.Paralysis usually followed by death ____days after onset of signs
9-11
2-3
Diagnosis of Equine Encephalomyelitis
1.Clinical assessment
2.CSF examination – in EEE with neutrophilic pleocytosis (count > 50%)
3.IgM capture ELISA – 85-90%; neutralizing antibodies gold standard (
____)
4.PCR – midbrain and brain stem
Treatment:
1.Supportive nursing care
2.Management of pain and inflammation
3. For WNV, _____1.1mg/kg, IV, bid to prevent muscle tremors and fasciculations
IgG
flunixin meglumine
Prevention of Equine encephalomyelitis
1. Core annual vaccination one month prior to mosquito season; formalin-inactivated whole viral vaccines
•Mares vaccinated ____ month before foaling
•With colostrum, foals vaccinated at ____ months plus 2 additional vaccinations 30 and 90 days after
•Zoonotic risks
1
5-6
•Highly contagious respiratory disease caused by Orthomyxovirus Influenza virus A/equine 2
•Subtyupes H7N7 and H3N8; ____spreads rapidly and cause severe clinical diases
•Horses ___ years most susceptible
•Endemic in many countries except New Zealand and Iceland
•Rarely fatal except in donkeys, zebras and debilitated horses
Equine Influenza
H3N8
1-5
Transmission of ____
•Incubation period < 48 hrs
•Morbidity 60-90%
•Mortality <1%
•Outbreak due to close contact
•Transmission by direct contact via nasal secretion or droplet infection
Clinical Signs
1.High fever up to 41.1’C
2.Harsh, dry cough
3.Loss of appetite
4.Depression
5.Watery nasal discharge
•Signs last <3 days; recovery in 2-3 weeks
•Virus replicates in respiratory epithelial cells resulting in destruction of tracheal and bronchial epithelium and cilia
Equine Influenza
Treatment of Equine Influenza
1.Fresh air, rest for 1-3 weeks
•Avoid dust
2.NSAIDs for fever above 40’C
3.Antibiotics to control secondary infection
Prevention:
1. Vaccination
•Most vaccines are effective against multiple strains
2.Hygienic practices
3. Isolation of newly acquired horses
Equine Infectious Anemia
•_____, Coggins disease; non-contagious, infectious disease
•Caused by an RNA Lentivirus, Retroviridae
•____ are the only known natural host
•No treatment available to eliminate EIA from an infected horse
•Horses surviving EIA can
relapse and/or pass it on to
other horses
•Lifetime Quarantine
•Euthanasia
Transmission
•Blood from infected animal is source of infection
1.Mechanical transmission by Tabanus sp and Stomoxys calcitrans
2.Vertical transmission – in utero/colostrum feeding
3.Venereal transmission via semen
4.Iatrogenic – blood contaminated products
Mode of Transmission
•Blood from infected horses
•Blood-sucking flies, mosquitoes
•Needles
•Surgical instruments
•Dental floats
•Bridle Bits
“Swamp Fever”
Horses
_____
Clinical Signs
•Incubation period ____ days
1.Sudden onset of high fever of 40º - 42.2º C
2.Severe depression
3.Depressed appetite
4.Weight Loss
5.Weakness/incoordination
6.Jaundice
7.Ventral edema
8.Rapid destruction of red blood cells
EIA
15-45
Types of infection of EIA
1.____ – 1 to 3 days characterized by fever, depression and thrombocytopenia
2.____ - most common
•Similar symptoms to acute, but not as severe
•Death not as common
3. ____:
•Horses are unthrifty and lack stamina
•May have acute or subacute attacks
Acute
Subacute form
Chronic EIA
EIA - Diagnosis
1. _____
•Dr. Leroy Coggins of Cornell University
•Only 10 cc of blood is needed for the test
•Results can be available in 24 to 48 hours
•Most require a negative Coggins test for transporting horses, racing, breeding
•Most shows require negative Coggins test for participants
•Required negative Coggins for sales
2. ____
v
ELISA
______
•Vector-borne virus first in North America in 1999
•Caused by a Flavivirus
•Humans, horses, and birds are incidental hosts
•Wetland and terrestrial birds involved in natural cycle
•Routes of infection in man thru blood transfusions, organ donations, breastmilk, via placenta
•Many horses infected with WNV do not become ill
•Other symptoms: colic, lameness, anorexia, fever
•Approximately ___ die
West Nile Virus
33%
WNV
Prevention
1.Vaccination –95% control rate
2.WNV Antibody for horses already
infected (____, Inc.)
Control
•Mosquito control
•Eliminate standing water
•Mosquitoes can breed in as little
as an inch of water
Novartis Animal Vaccines
_____
•Acute upper respiratory infection caused by an RNA Arterivirus, family Togaviridae
•Similar to influenza and rhinopneumonitis
•All age groups susceptible
•Most common in_____
•Degenerative and inflammatory changes in the endothelium
•Transmission:
1.Inhalation of droplets from infected horses
2.Ingestion
3.Venereal transmission by stallion
4.Tissues and fluids from aborted fetus
5.Shedding in the urine
Equine Viral Arteritis
Saddlebreds and Standardbreds
Clinical Signs of______
1.Fever (38.8-41.1ºF)
2.Nasal discharge
3.Can cause abortion (approximately
50%)
4.Edema of the limbs
5.Increased respiratory rate
6.Skin rash
Treatment
•Most animals recover without treatment
•Vet may prescribe antibiotics to prevent secondary infection
EVA
Prevention
•Vaccination
Control
•Sound management practices
Equine Viral Arteritis
____
•Neurotropic Lyssavirus, Rhabdoviridae
•Saliva of infected animal à horse
•Travels up the NERVES to the brain
•Reproduces in the brain
•Sheds virus through the salivary glands
•BLOOD TEST WON’T DIAGNOSE DISEASE
Symptoms:
1.Neurological disorder, choking, weakness, staggering, unprovoked excitement
2.Behavioral changes are most common
3.May take 2-6 weeks or even 3 months to show symptoms after infection
NO EFFECTIVE TREATMENT
Prevention - annual vaccination
•Problem in horses in the Mid-Atlantic where raccoon strain is predominant
Rabies
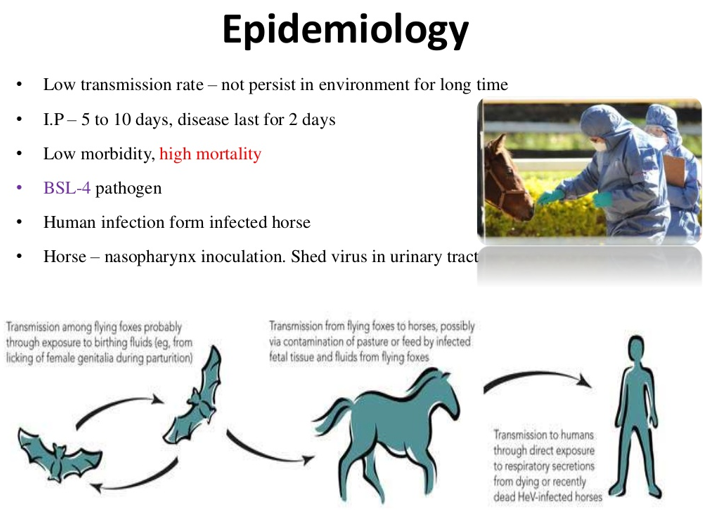
____ is prototype species of the new genus Henipavirus of the subfamily Paramyxovirinae
•A pleomorphic enveloped RNA virus
•First identified in Australia in 1994 as an acute respiratory disease in a Thoroughbred and a human
•Endemic in fruit bats or flying foxes of the suborder Megachiroptera, _____reservoir host and suspected to facilitate transmission of HeV to horses
•Classified as a biosafety ____ agent
•Horses only species naturally infected
•Zoonotic
•Infection via oro-nasal route and excretion via the urine, saliva, and respiratory secretions
Case fatality rate in horses and humans high
•Transmission in very close contact among horses and from horse to people
•Virus not considered highly contagious
•Equine veterinarians considered at occupational risk
Hendra Virus (Equine Morbllivirus)
Pteropus sp.
Level 4
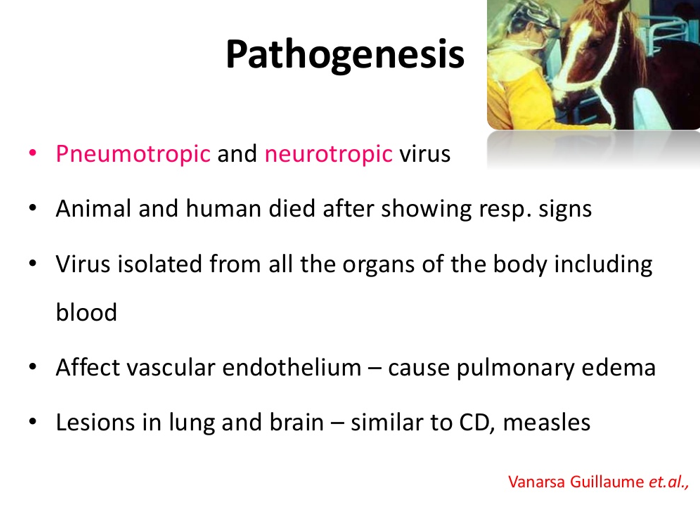
Clinical Signs of Hendra Virus
1.Severe and often fatal respiratory disease characterized by dyspnea, vascular damage, pulmonary edema, respiratory difficulty and frothy nasal discharge, jaundice
3.Depression
4.Anorexia
5.Fever
6.Ataxia
7.Tachycardia
Treatment
•Supportive treatment
•No specific treatment against the virus
Prevention
1.Commercial HeV vaccination available for release to veterinarians who have completed an online training program
•Horses must have microchip to be vaccinated
•Vaccine consists of soluble forms of G glycoproteins of HeV and does not contain modified or inactivated virus
2.In humans, prevent contact with infected horses and use appropriate personal protective equipment
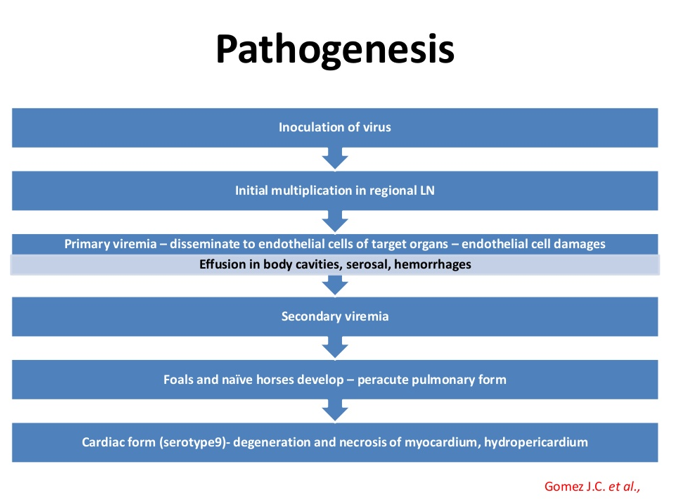
African horse sickness
An infectious, contagious disease of equine characterized by abscessation of the lymphoid tissues of the upper respiratory tract
Causative Agent: ______, a Gram-positive, capsulated, B-hemolytic, Lancefield group C coccus which is an obligate parasite and a primary pathogen
•Highly host-adapted affecting only___
Pathogenesis:
•Highly contagious, produces high morbidity but low mortality in susceptible animals
•Transmission is via ________with infectious exudates
•_______ is important source of infection and could initiate outbreaks in premises previously free of the disease
Organism is susceptible to dessication, extreme heat and exposure to sunlight
Under favorable conditions, the organism can survive ____ outside of the host but under field conditions, do not survive ___
Strangles (distemper)
Streptococcus equi
horses, donkeys and mules
fomites and direct contact
Carrier animal
4 weeks
96 hours
Clinical Findings Strangles (Distemper)
1.Incubation period is ____
2.First sign is fever of _____
3.Mucoid to mucopurulent nasal discharge
4.Depression
5.Submandibular lymphadenopathy
6.Horses with involvement of the ______ have difficulty in swallowing, inspiratory respiratory noise due to compression of the dorsal pharyngeal wall, and extended head and neck
7.Animals with_______ develop atypical or catarrhal form of the disease with mucoid nasal discharge, cough and mild fever
3 to 14 days
39.4 to 41.1’C
retropharyngeal lymph nodes
residual immunity
Characterized by abscessation in other lymph nodes particularly those in the abdomen and less frequently in the thorax
• Most common cause of brain abscess in horses although it is rare
Diagnosis:
1.Bacterial culture of exudates from abscesses and nasal swab samples
2.CBC – ________
3.Endoscopic examination of the upper respiratory tract
4.Ultrasonography of the retropharyngeal area
5.X-ray of the skull to determine retropharyngeal abscessation
METASTATIC STRANGLES (Bastard Strangles)
neutrophilic leukocytosis and hyperfibrinogenemia
Treatment of METASTATIC STRANGLES (Bastard Strangles)
1.Keep environment warm, dry and dust free
2.Warm compress will facilitate maturation of abscesses
3.Facilitated drainage of mature abscesses will speed up recovery
4.Flush ruptured abscesses with _______ until discharge ceases
5.______ to reduce pain and fever and improve appetite
6._______ for horses with retropharyngeal abscessation and pharyngeal compression
7.Antimicrobial therapy provides temporary relief from fever but delays maturation of abscess; indicated in dyspnea, dysphagia, prolonged high fever and severe lethargy or anorexia
______ during early stage of infection , < 24 hours of onset of fever will arrest abscess formation
Early antimicrobial treatment fails to mount protective immune response rendering horses susceptible to infection after cessation of treatment
______ at 22,000 IU/kg, IM, bid is the antibiotic of choice
Untreated guttural pouch infection can lead to ____________
3 to 5% povidone-iodine
NSAIDS
Tracheotomy
Penicillin
Procaine penicillin
persistent guttural pouch empyema
Prevention:
1.Post-exposure immunity produced after natural exposure to the disease; local production of antibodies against __________
2.Vaccination with IM products that do not induce mucosal immunity
3.Intranasal live attenuated strain to elicit mucosal immunologic response
Side effects: Abscess at site of IM injection, submandibular lymphadenopathy, serous nasal discharge and purpura hemorrhagica
antiphagocytic M protein
Caused by specific neurotoxin produced by ________
Almost all mammals susceptible, dogs and cats relatively more resistant
_______quite resistant
_________ most sensitive of all species
Etiology and Pathogenesis:
•Caused by C. tetani, an anaerobe with terminal, spherical spores, found in the soil and intestinal tracts
•Introduced into the tissue through wounds that provide suitable anaerobic environment
•In lambs, often follows docking or castration
•Spores of the organism unable to grow in normal tissue and circulating blood
•Bacteria remain localized in_________
•Toxin is absorbed by the motor nerves and causes spasmodic, tonic contractions of voluntary muscles by interfering with the release of inhibitory neurotransmitter from presynaptic nerve endings
•Spasms affecting the larynx, diaphragm, and intercostal muscles lead to________
Tetanus (Lockjaw)
Clostridium tetani
Birds
Horses and lambs
necrotic tissue
respiratory failure
Clinical Findings of Tetanus (Lockjaw)
1.Incubation period averages from ______
2.Localized stiffness of masseter muscles, muscles of the neck, hindlimbs and region of the infected wound which become more pronounced
3.Tonic spasms and hyperaesthesia
4.Difficulty in prehension and mastication, hence lockjaw
In horses: ears erect, tail stiff and extended , anterior nares dilated and third eyelid prolapsed; stiffness of the leg muscles causes the animal to assume a ______
5.Sweating is common
6.Generalized spasms disturb circulation and respiration resulting to increased heart rate, rapid breathing and congestion of mucous membranes
7.Sheep, goats and pigs fall to the ground and exhibit opisthotonus
8.Temperature remains slightly above normal but may rise to ______ toward end of fatal attack
9.Mortality is about ____
10.Convalescent period is about _______; protective immunity does not develop after recovery
10 to 14 days
“sawhorse” stance
42-43’C
80%
2-6 weeks
Diagnosis of Lockjaw
1.Clinical signs and history of recent trauma
2.Demonstration of toxin in ____ of affected animal
3.Anaerobic culture and demonstration of bacteria from wound
serum
Treatment and Control of Lockjaw
1.In early stages of disease: _______ (muscle relaxants), tranquilizers or barbiturate sedatives in conjunction with 300,000 IU of ______
2.%0,000 IU of ________ into the subarachnoid space thru the cisterna magna
3.Draining and cleaning of wounds and administering ___________
4.Place in quiet, darkened stall box with feeding and watering devices
5.Sling for horses with difficulty in standing or rising
curariform agents
tetanus antitoxin
tetanus antitoxin
penicillin or broad spectrum antibiotics
Prevention of Lockjaw
1.Active immunization with _______; wound after immunization, another toxoid
2.If not previously immunized, give ______ of tetanus antitoxin which provides protection for 2 weeks
3.Toxoid given simultaneously with antitoxin and repeated in _______
4._______ toxoid booster
5.Mares vaccinated during _______ week of pregnancy
6.Foals at _____ weeks of age; in high risk foals, given antitoxin immediately after birth then __________ then given toxoid
tetanus toxoid
1,500-3,000 IU
30 days
Yearly
last
5-8
every 2-3 weeks until 3 months old
________
• Rare in horses but fatal
• Caused by toxins produced by _______
• _________ acts on the peripheral nervous system by preventing transmission of the nervous impulses
• Found in soil and decaying plant or animal matter
• Adult horses and foals less than________ affected
Clinical Signs
Foals
1. Impaired suckling
2. Inability to swallow
3. Decreased eyelid and tail tone and dilated pupils
4. Respiratory paralysis
Adults
1. Many of same signs seen in foals
2. Eventual muscle weakness, tremors and collapse
3. Respiratory paralysis which causes death
Botulism
Clostridium botulinum
Botulinum toxin
8 mos. old
Treatment of botulism
1. ________
Prevention
1. Vaccine recommended for endemic areas
Polyvalent equine antitoxin
Contagious Equine Metritis
•Caused by _____
• Transmission through direct breeding , AI and contact with contaminated items
Clinical Signs
1. Highly contagious, often asymptomatic though affected mares show mucoid vaginal discharge
2. Infertility or abortion in mares, no clinical signs in stallions
Infertility can last for ______ breeding cycles
Treatment
1. __________
Prevention
1. Clearance of stallion
Stallion allowed to undergo test breeding to negative mares
3. Process takes _____to declare stallion negative
4. Average to clear stallion takes ___
5. Good hygiene practices
Contagious Equine Metritis
Taylorella equigenitalis
one or more
Topical and systemic antibiotics
35 days
6-8 weeks
Tyzzer’s Disease
• Rare disease caused by ________
• Characterized by severe and peracute hepatitis affecting foals ______
• Foals infected by ingestion of spores from _______
• Following colonization of _____ it infects the liver causing _____
Clinical Signs
1. Foals simply found dead
2. Weakness, lethargy, anorexia, dehydration, pyrexia, diarrhea, tachycardia, tachypnea and icterus
3. Seizures, coma and death may rapidly ensue
• Prognosis for foals poor and most affected foals found dead
Clostridium (Bacillus) piliforme
1 to 6 weeks old
feces or environment
intestinal tract,
severe hepatic necrosis
Treatment of Tyzzer’s disease
1. IV fluids
2. Anti-inflammatories
3. Antibiotics such as ampicillin and gentamycin
4. Parenteral nutrition
•Pneumonia in Foals
• Caused by _______ in foals
• Also causes ulcerative enterocolitis, colonic-mesenteric lymphadenopathy, immune-mediated synovitis and uveitis, osteomyelitis, pyogranulomatous dermatitis, brain abscess, immune mediated anemia and septic arthritis
• Inhalation of _______ most important route for pneumonic infection in foals
• Facultative intracellular parasites of _______
Clinical Signs
1. Most common is suppurative bronchopneumonia with extensive abscess formation and suppurative lymphadenitis
2. Early signs include slight increase in respiratory rate and mild fever
3. More commonly __________ (105-106’F or 40-41’C)
4. Intestinal manifestations characterized by granulomatous or suppurative inflammation of Peyer’s patches and mesenteric or colonic lymph nodes
Rhodococcus equi
contaminated dust
monocytes and macrophages
acute respiratory distress and high fever
Treatment of Pneumonia in foals
1. Administration of _______ (25 mg/kg PO every 8 hours) and ______ (5 mg/kg PO every 12 hours)
Costly and labor intensive and can result to diarrhea and hyperthermia in treated foals
______ (10 mg/kg PO every 24 hrs. for first 5 days then every other day and ______ (7.5 mg/kg PO every 12 hrs.)
Used in combination with rifampin
_______(10 mg/kg PO every 12 hrs.)
erythromycin
rifampin
Azithromycin
Clarithromycin
Doxycycline
Prevention of Pneumonia in Foals
1. ______– stocking density, proper ventilation, dust control
2. _______ – transfusion of hyperimmuned plasma 1L during first 24 hrs. and 25 days later
3. _________ – development of superinfections, bacterial resistance and antimicrobial-induced colitis
Husbandry
Passive immunity
Chemoprophylaxis
Lyme Disease
• Caused by _________
• 2-year enzootic dual infection with ________ cycle involving Ixodes ticks and mammals (deer and white-footed mouse)
• Ticks must be attached to mammal for at least ________
Clinical Signs
1. Low-grade fever
2. Stiffness and lameness in more than one limb
3. Muscle tenderness, hyperaesthesia, swollen joints
4. Lethargy and behavioral changes
Borrelia burgdorferi
Anaplasma phagocytophilum
24 hrs.
Treatment of Lyme Ds.
1. _______ - 6.6 mg/kg IV every 24 hrs. for 1 week before treatment with doxycycline
2. _______ – 10 mg/kg PO every 12 hrs. for 1 month
3. ________- – 2-4 mg/kg IV or IM every 12 hrs.
Prevention
1. Preventing tick exposure or prolonged attachment
2. Early antimicrobial treatment after exposure
3. Vaccination
Tetracycline
Doxycycline
Ceftiofur
Leptospirosis
• Caused by highly invasive Leptospira
1.____________ – North America (skunk most common maintenance host)
2.__________– Western Europe
3.___________ – Eastern Europe
4__________ – host-adapted serovar of the horse
Leptospira interrogans serovar Pomona type kennewki
Leptospira kirschneri serovar Grippotyphosa strain duster
Leptospira kirschneri serovar Grippotyphosa strain moskva
.L. interrogans serovar Bratislava
Clinical Syndrome of Leptospirosis
1. Reproductive Tract
________
•Responsible for most Leptospira abortions but serovars Grippotyphosa and Hardjo has also been reported
•Abortion after 9 months, infected fetuses carry Leptospira in placenta, umbilical cord, kidney and liver
•Aborting mares shed the organism in their urine for 2-3 months
•May develop uveitis weeks later
2. Acute Renal Failure
____
•Ever and acute renal failure; tubulointerstitial nephritis and pyuria without visible bacteria
L. interrogans serovar Pomona
L. Pomona
Clinical Syndrome of Leptospirosis
3. Recurrent Uveitis
L. interrogans serovar Pomona
•Most common is ___________
•_________ against Leptospira antigens cross-reacting with tissues of the lens, cornea and retina
•Live Leptospira organisms in the uveal tissue, aqueous and vitreous fluid of horses with recurrent uveitis
•Genetic factors in recurrent uveitis; ________genetically predisposed
•ERU most common cause of blindness in horses
equine recurrent uveitis (ERU) and immune-mediated keratitis
IgG and IgA
Appaloosas
Treatment of leptospirosis
1.Systemic administration of antimicrobials; fever and acute renal failure: ________
2.Fluid therapy
3._________ – temporary relief
4.______ – inoculation of gentamycin lavage
penicillin, ampicillin,cephalosporin, enrofloxacin, tetracycline and doxycycline
Corticosteroid and cyclosporine
Vitrectomy
Prevention of Leptospirosis
1.Acutely infected horses isolated for _________
2.Urine detected by ______
3.Limiting exposure to stagnant water and potential maintenance hosts
4.Vaccination
14 to 16 weeks
FAT
Salmonella and Nosocomial Infections
_______________
Clinical Signs
1. Enterocolitis
2. Diarrhea
3. Fever
4. Leukopenia
• Danger of fecal shedding
Treatment
1. Antimicrobial treatment
Prevention
1. Cleaning and disinfecting of horse facilities
2.Temporarily close, empty wards and institute thorough and intensive cleaning and disinfecting procedures
3.Strict traffic of humans and animals
4.Adequate ventilation and distance between cases
Salmonella enterica subspp. Enterica serotype Typhimurium, Newport, Anatum and Agona