PSYC 169 - Midterm 2
1/63
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
64 Terms
Primary areas
Neocortical regions that receive sensory signal or send motor commands
Secondary areas
Areas that elaborate sensory information received from primary areas
Located adjacent to primary areas and are interconnected with them
Association areas
All cortex not directly responsible for sensory input or motor output
Mediate complex activities such as language, planning, memory & attention
Located between the various secondary areas
Can receive signal from or send signal to secondary areas
The lateralized forebrain
Most sensory and motor neurons cross after entering the brain
One side of the forebrain is responsible for the opposite side of body
Primary visual cortex “V1” (striate cortex)
Large strip of cortex in the occipital lobe
Responsibilities: process basic visual information & sends info to secondary visual areas
V1 must function so that secondary visual areas can carry out their processing
Sensation
The effects of a stimulus on the sensory organs
Perception
The elaboration & interpretation of a sensory stimulus based on, for example, knowledge of how objects are structured
Visual Processing
1) From eye to V1
2) From V1 to rest of the brain
Retina
The internal surface of the eyes that contains specialized cells
Photoreceptors
Located in the retina
Convert (or transduce) light into neural signals
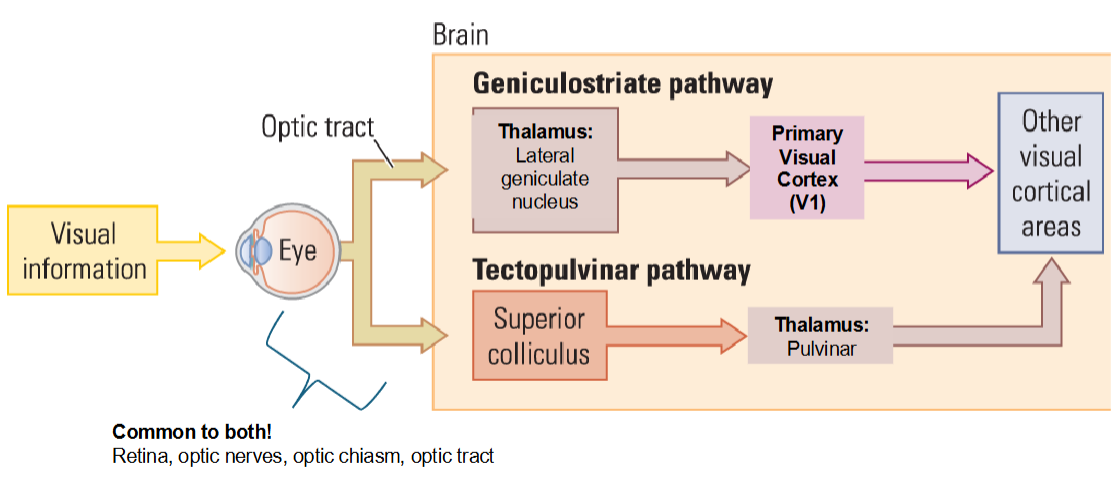
Geniculostriate pathway
Light from each visual field hits both eyes
Information from the nasal portion of the retina (traveling through the optic nerve) crosses at the optic chiasm
Information from the temporal portion of the retina (traveling through the optic nerve) remains ipsilateral
Information from both eyes is processed in the LGN
The information travels from the LGN through the optic radiations to V1
Basic visual information, such as orientation, is processed in V1
Blindsight happens because perception is impaired
Physical damage to V1 in one hemisphere causes ‘cortical blindness’ in the contralateral visual field
Retinotopic map of V1
Neurons that are ‘close’ together process information that is ‘close’ together in the visual fields
Hemianopia
A type of blindness that occurs on half of the visual field
Describe the two general ways hemianopia can occur
Can occur in the early visual pathway before V1
Can occur when there’s damage to V1
Damage to V1 & the retinotopic map
The amount of damage in V1 is proportional to loss of information within the retinotopic map
“Cortical blindness” is caused by damage to V1 and not the eye or early visual pathways
Patient D.B.
A portion of the right V1 was lesioned during surgical removal of an angioma
He couldn’t consciously “see” but sometimes “felt” something was moving
He could still accurately point to light shining in his left visual field despite no conscious awareness!
Angioma
Collection of blood vessels that cause abnormal blood flow
Blindsight “cortical blindness”
The conscious awareness of “seeing” is missing even though visual information is not reaching V1
Tectopulvinar pathway
Evolutionarily ‘old’ compared to geniculostriate
Transcranial magnetic stimulation (TMS)
Uses electrical pulses to inhibit or activate areas of the brain
Evidence for blindsight
Secondary visual areas
V2: assists V1 to integrate basic visual information & sends information to the other secondary visual areas
V3-V5: all do some form of color, form, or motion processing
V4 is more functionally specialized for color
V5 is more functionally specialized for motion
Color vision deficiency (CVD)
The decreased ability to see color as most people do
CVD can impair seeing:
The difference between color
How bright colors are
Different shades of colors
Typically CVD is inherited due to genetic mutations that caused missing cones
Describe the three patients with damage to secondary visual areas & their symptoms & deficits
Patient J.I - Had achromatopsia
Patient P.B - color perception in a blindsight patient
Patient L.M - Had akinetopsia
Patient J.I
Before his accident, he was an accomplished painter
He had no missing or damaged cones and saw color “normally” his whole life
He suffered a severe concussion (TBI) after a car accident
He could no longer distinguish any color whatsoever
His physical world, dreams and memory appeared in black and white
His diagnosis was achromatopsia
Achromatopsia ‘cortical color blindness’
Failure to perceive color causing the world (or even dreams!) to appear in grayscale
Caused by damage only to area V4
Not the ‘typical’ color blindness (color vision deficiency)
Patient P.B
Patient P.B was electrocuted, resulting in cardiac and respiratory arrest resulting in damage to V1 and V2
He had blindsight but could still perceive light…even colored light!
Conclusion: it’s likely some visual information reached area V4 even though his V1 and V2 were damaged
Akinetopsia “motion-blindness”
Inability to perceive motion
Occurs when there’s damage to V5/MT
Patient L.M
Was an 43-year-old woman whose area V5/MT was damaged after a stroke
She had difficulty pouring tea into a cup because the fluid appeared to be frozen
L.M found being in a room with other people disturbing because she could not see them moving
Two streams of hypothesis of object recognition
A model of how visual information travels through association areas to support higher-level cognitive functions
It proposes there are two anatomically distinct processing streams that originate from the occipital lobe
Dorsal stream
Ventral stream
Dorsal stream
The “how/where” pathway because it’s responsible for processing where objects are in space and their function
Leads to the parietal lobe
Ventral stream
The “what” pathway because it’s responsible for recognizing “what” something is
Leads to the temporal lobe
Recognition
The experience of “knowing”
Agnosia
“Without knowledge”
A rare disorder whereby a patient is unable to recognize & identify objects, persons or sounds using one or more of their senses despite otherwise normally functioning senses
Visual agnosia
A result of brain damage to the association areas within the ventral “what” pathway
Causes a selective impairment
Patient Gottlieb L.
Suffered a head injury after a wooden fence was blown into his head during a storm
Ended up getting visual agnosia
Symptoms: when shown a pair of glasses, he named them as ‘a lamp’, yet he could recognize them by touch
He could perceive the object but he couldn’t associate them with a meaning
Lissauer’s classic model of object recognition
Heinrich Lissauer examined Gottlieb L. in 1888 & proposed there were two major stages in object recognition
1) Create a coherent percept of the object as a single entity
2) Attach meaning to the percept
What was Lissauer’s classic model of object recognition and what were the two agnosias derived from it?
Lissauer’s classic model of object recognition is that a person creates a coherent percept of the object as a single entity & attaches meaning to the percept. The agnosias derived from it are visual form agnosia & associative agnosia.
Agnosias derived from Lissauer’s “classic” model of object recognition
Visual form agnosia (VFA)
Associative agnosia
Visual form agnosia
The inability to group visual information together to create a coherent perceptual image of what one is seeing
Associative agnosia
The inability to attach meaning to the perceptual image of an object
Patient Mr. S - visual form agnosia
Clinical presentation: 25 year old male veteran with carbon monoxide poisoning
Behavioral performance:
Could follow moving visual stimuli
Could hardly recognize and name objects based vision alone
Could recognize objects by touch
Appeared “blind” for object recognition
He could not 1) copy or 2) match simple letter, shapes or objects
His deficits were due to the inability to group information into one visual image within his own mind
Patient D.F - visual form agnosia
She was unable to copy the model drawings…but when asked to draw the model objects from her own memory she could!
This demonstrates visual form agnosia:
Is an impairment in grouping visual information into a coherent mental image
Is not an impairment in memory
She was unable to visually identify or copy a list of letters or numbers but she could identify 3D shapes of letters and numbers by touch and write them by memory
More evidence that VFA is a deficit in perception
Perceptual tests of VFA: Incomplete Pictures Test
Predicted Performance
Healthy controls can recognize the object by the second drawing
VFA patients need more visual information or are completely unable to recognize the object
Healthy controls can pick which individual objects are in the overlap picture whereas VFA patients are impaired
Perceptual tests of VFA: Unusual Views Test
Everyday common objects are shown from two angles
Normal performance requires the visual information to be grouped into one object and rotated in the mind’s eye
What are some examples of test performance that would indicate a patient has visual form agnosia?
Unable to visually recognize objects
Can recognize objects by touch
Unable to copy, match or identify drawings of objects
Able to draw objects from memory
Patient F.L - associative agnosia
Patient FL had brain damage from alcoholism
Symptoms:
Could copy line drawing copies very well but could not name to objects he was drawing
Could not “understand” objects because he couldn’t recognize them
He didn’t know how to use a key or to open an umbrella when it was raining because he couldn’t understand “what” the object was
What are some examples of test performance that would indicate a patient has associative agnosia?
Success on perceptual tests
Impairment on tests assigning meaning to a visual mental image
Matching by function tests
Challenge to Lissauer’s model: patient HJA’s performance on copying
HJA could copy all the drawings very well but couldn’t name/recognize what he drew
St. Paul’s cathedral
Everyday objects
Expected diagnosis?
Associative agnosia
Patient HJA’s performance on copying
End result looks great! But what about the strategy?
Copied one small section in great detail & then moved on to the next small section
Most people copy by drawing the outline & then fill in the details
HJA was perceiving the world abnormally due to deficits in featural binding
Featural binding
Combining different characteristics, such as color, shape, size, orientation and location to perceive objects
Patient HJA
Had symptoms of both visual form and associative agnosia
Had integrative agnosia
Integrative agnosia
A form of visual agnosia in which individuals are able to perceive the elements of an object but find it difficult to combine them into an integrated whole
Prosopagnosia
Neurological disorder characterized by the inability to recognize familiar faces
Patients with prosopagnosia cannot visually recognize any previously known faces, including their own as seen in a mirror or photograph
Specific brain regions involved with face processing
Occipital face area
Fusiform face area
Occipital face area
Responsible for structural processing of faces
Fusiform face area
Higher-order face processing such as identity
Cause of prosopagnosia
Developmental prosopagnosia
Acquired prosopagnosia
Developmental prosopagnosia
Alterations in the face processing areas are present from birth and are likely caused by genetic mutations or deletions that are inherited
Acquired prosopagnosia
Strokes, head trauma, inflammation, infection, oxygen deprivation, etc. which damage the face processing areas
Three basic stages of face processing
Visual analysis
Perceptual analysis
Identity analysis
Visual analysis
Decoding the visual information from a visual scene
Perceptual analysis
Grouping the information together to “know” that it is a human face
Identity analysis
“Knowing” that this face is one that you have encountered before