ER 6 - Chest Pain and Cardiology Emergencies
1/42
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
43 Terms
Which condition is more likely to pain that is precisely located, sharp, and reproducible with palpation and movement?
a. pneumothorax
b. esophageal spasm
c. costochondritis
d. pericarditis
c. costochondritis
PTX is pleuritic pain (increased by deep breathing, coughing, laying back); pericarditis is visceral and changes with movement; esophageal spasm is also visceral
What deadly diagnosis that often presents with chest pain often occurs immediately after an episode of forceful vomiting and may have palpable crepitus?
esophageal rupture
True or False - In someone presenting with chest pain and symptoms suspicious for ACS, you can rule out ACS with a normal EKG.
False - you need to check labs; repeat EKG every 10-15 minutes if suspicion is high and initial EKG not diagnostic
example: myoglobin, cardiac troponins, CK-MB, IMA, H-FABP
In STEMI, Door to PCI goal is < ____ min; door to fibrinolysis goal < ___ min if they aren’t at a PCI center (or can’t get there reliably to be treated at cath lab in time, or if pt is unstable)
door to PCI goal <90 min
door to fibrinolysis goal < 30 min
note: fibrinolytics NOT given in NSTEMI
contraindicated in suspected aortic dissection/pericarditis and prolonged CPR >10 mins
What is the treatment for cocaine related chest pain?
benzodiazepines
True or False; Someone presents with NSTEMI and cannot get to a PCI center in <120 mins. You should give them fibrinolytics.
False - Fibrinolytics aren’t indicated for NSTEMIs
true or false - typical treatment for stable angina is nitro
true
In Unstable Angina, why do you need to admit and give antiplatelet therapy (Clopidogrel or Brilinta+ASA) or Anti-coag therapy (UFH or Lovenox or Arixtra)? What do you give them prior to discharge?
UA is significant because it indicates stenosis that has enlarged via thrombosis, hemorrhage, or plaque rupture, and this may lead to total occlusion of a coronary vessel. need to prevent this from happening.
on DC for UA: give beta blockers and statins
Which of the following best describes typical findings in Non-ST Elevation Myocardial Infarction (NSTEMI)?
A. ST segment elevations in contiguous leads with reciprocal depressions and pathologic Q waves
B. Diffuse ST elevations with PR depressions and no biomarker elevation
C. ST segment depressions or deep T wave inversions without Q waves, often with positive cardiac biomarkers
D. No ECG changes and normal cardiac biomarkers
E. Peaked T waves and widened QRS due to hyperkalemia
C. ST segment depressions or deep T wave inversions without Q waves, often with positive cardiac biomarkers
Rationale:
NSTEMI involves subendocardial ischemia that doesn't fully penetrate the myocardial wall.
ECG may show ST depressions, T wave inversions, or even no ECG changes at all.
Troponin is elevated, distinguishing it from unstable angina.
Which of the following best describes typical findings in unstable angina?
A. ST elevations in contiguous leads with elevated cardiac biomarkers and pathologic Q waves
B. ST depressions or T wave inversions with normal cardiac biomarkers
C. ST elevations and PR depressions with pericardial friction rub
D. No ECG changes and elevated cardiac biomarkers
E. ST depressions or Q waves with elevated troponin levels
B. ST depressions or T wave inversions with normal cardiac biomarkers
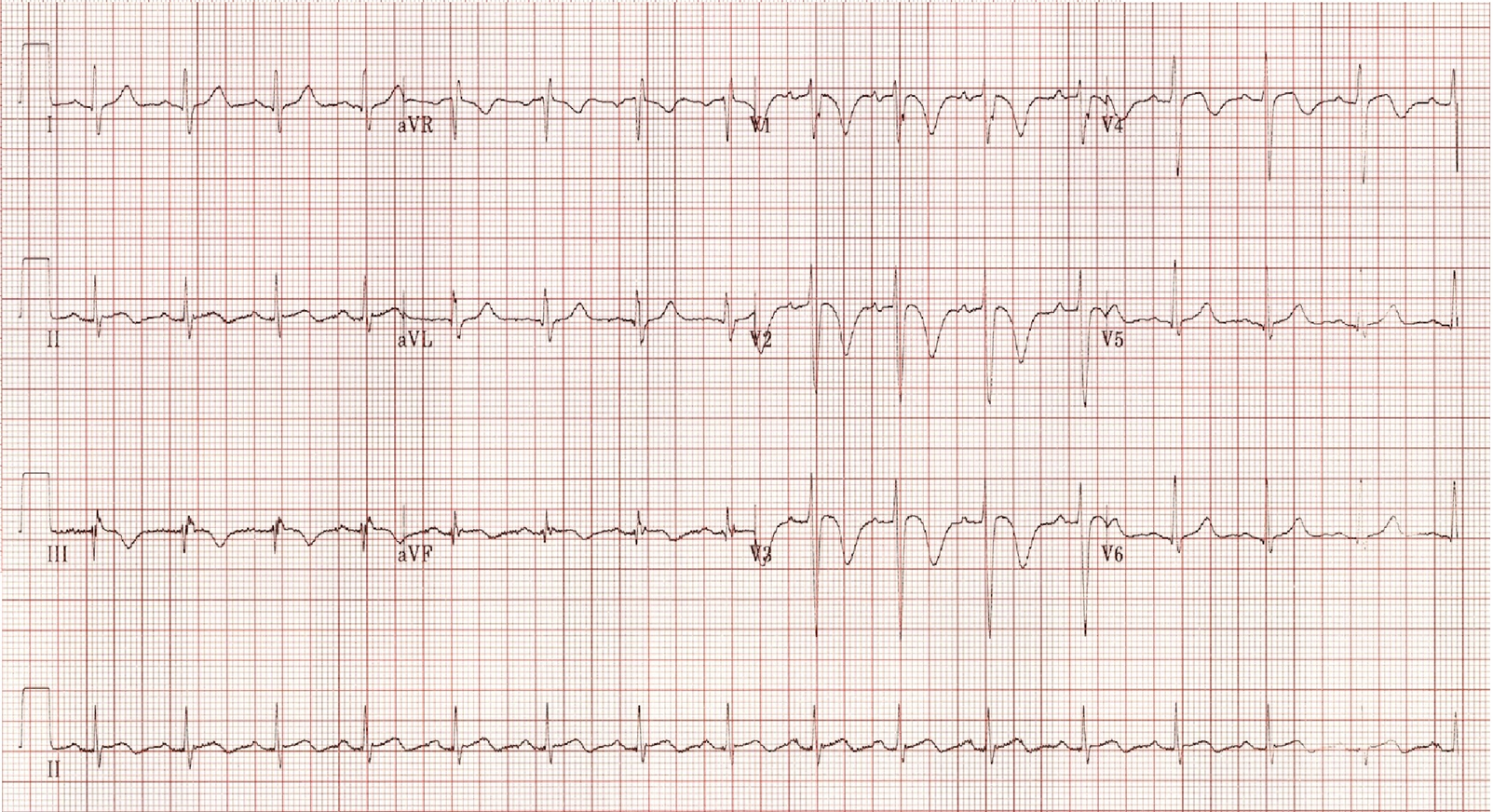
STEMI
ST elevation in leads II, III, and aVF
What artery is affected? Can you give nitro?
right coronary artery
NO nitro, can lead to hypotension
What artery is affected
STEMI in leads I, aVL, V5, V6
Left Circumflex Artery (Lateral wall of heart affected)
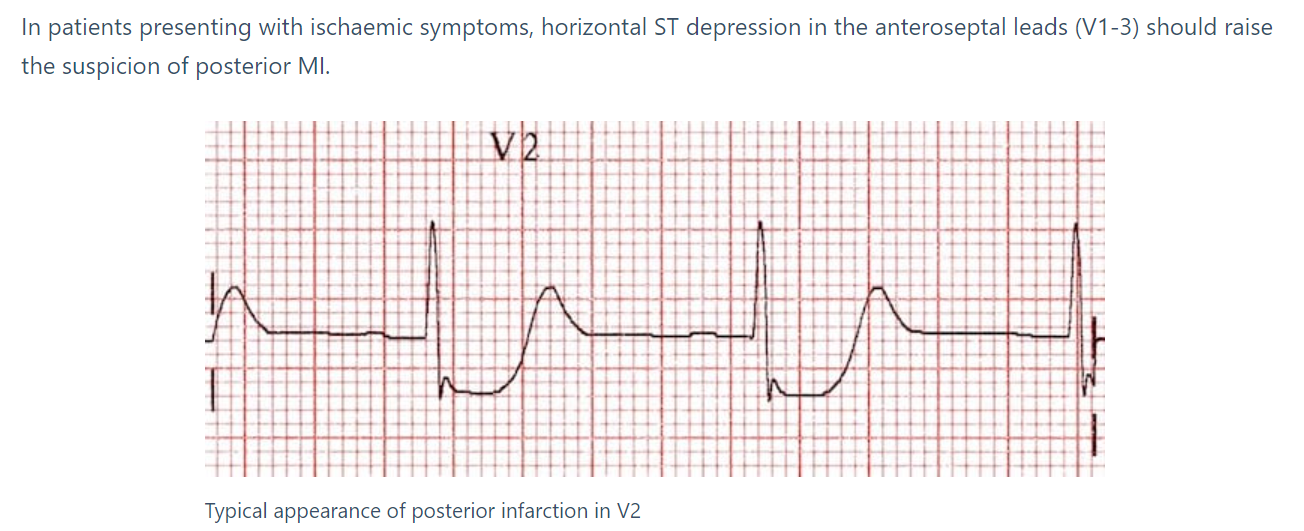
True or False - ST depression in leads V1-V3 may indicate anterior wall MI.
False - ST depression in leads V1-V3 may indicate posterior wall MI
True or False - Fibrinolytic therapy should only be performed after results of cardiac biomarkers have confirmed diagnosis.
What are some fibrinolytic options?
False; fibrinolytic therapy shouldn’t await availability of results if dx is reasonably certain
Alteplase (t-Pa) and Tenecteplase (TNKase)
Which of the following is a sign of irreversible cell death?
a. T wave inversion or ST depression
b. ST elevation
c. Q waves
c. Q waves are a sign of infarction - irreversible cell death
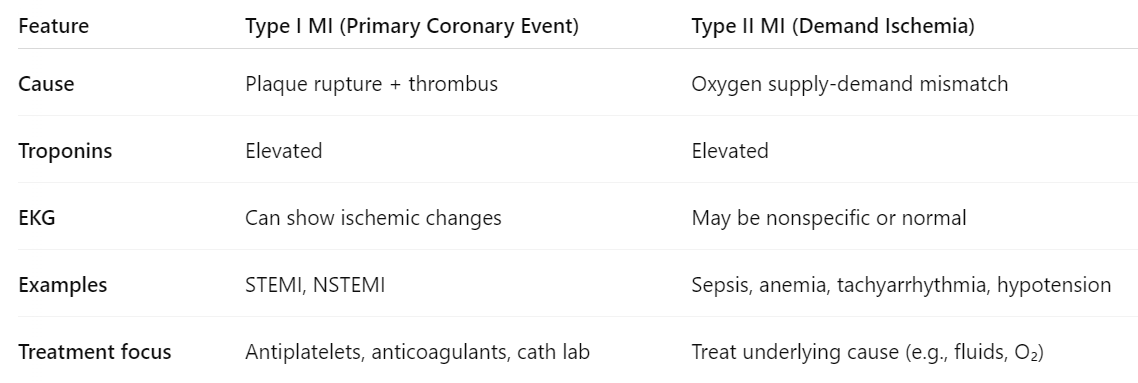
Which type of MI is due to a primary coronary event, and which is due to demand ischemia?
Type I - primary coronary event
Type II - demand ischemia
SEE CHART! 🙂
What is the HEART score used for (and what is it based on?)
HEART - risk stratification tool; predict risk of major cardiac events in 6 weeks; low risk can be safely DC home
History
EKG
Age
Risk Factors
Troponin
What is the most common finding of PE on EKG? What are a couple of other findings?
Sinus Tachycardia
RV strain (T wave inversions in V1-V4, II, III, aVF)
Cor Pulmonale (S1Q3T3)
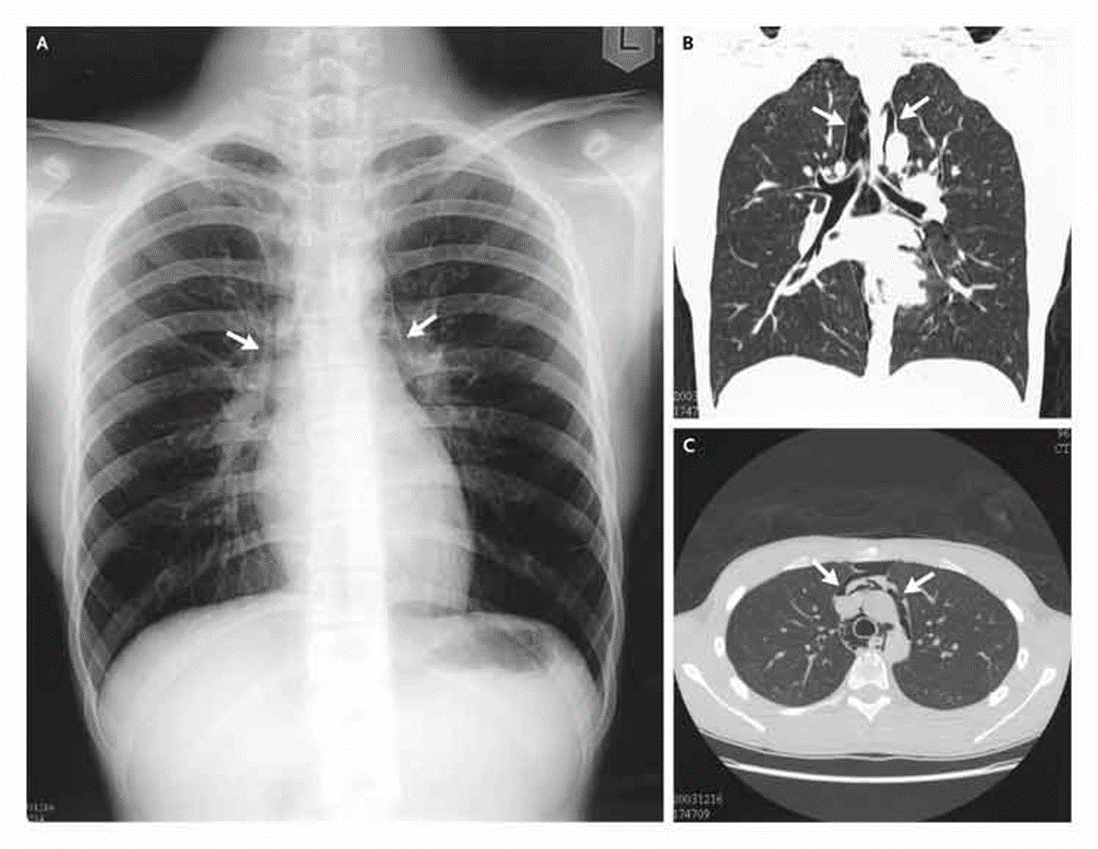
What is the gold standard (imaging) for PE?
CTA
True or False - esophageal rupture can cause a pneumomediastinum, which is visible CT scan
True
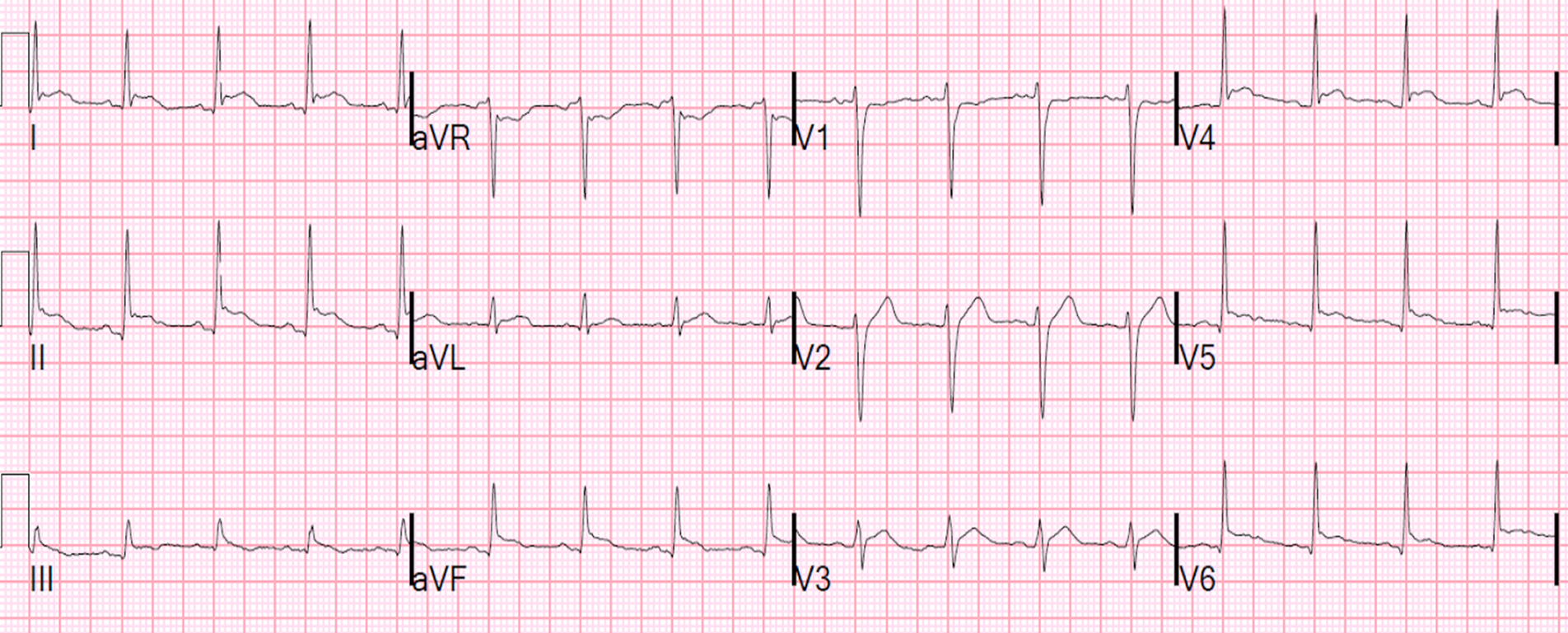
Electrical alternans is a classic EKG finding most commonly associated with which of the following conditions?
A. Acute myocardial infarction
B. Pulmonary embolism
C. Pericardial tamponade
D. Hyperkalemia
E. Aortic dissection
c. pericardial tamponade
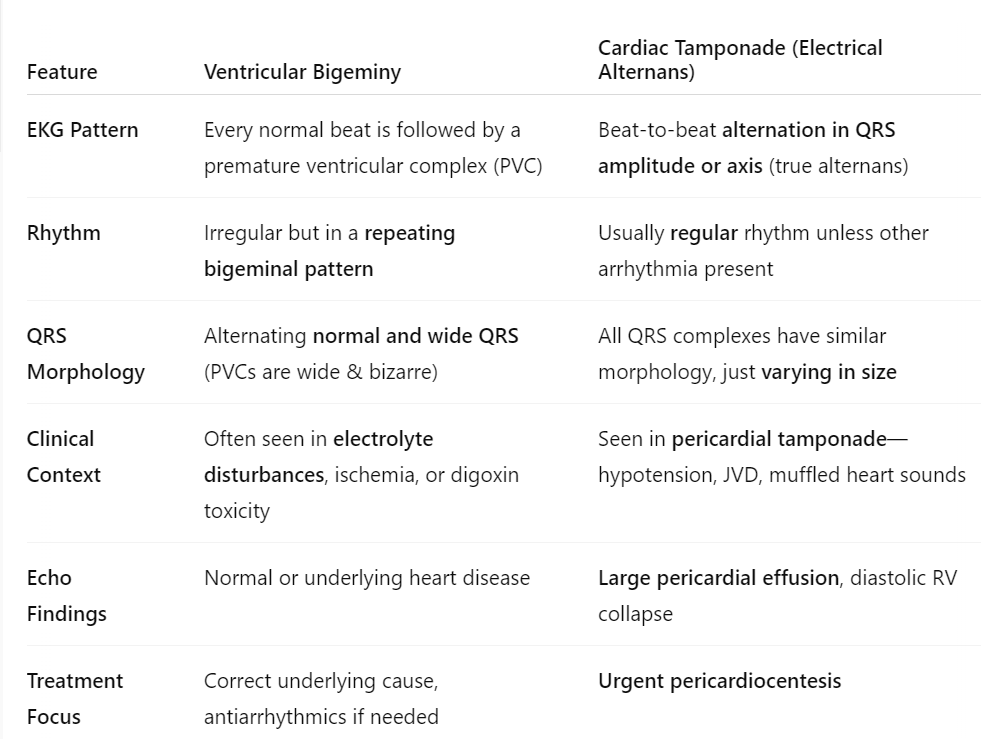
NOTE: don’t confuse it with ventricular bigeminy or PVCs, which can look similar to electrical alternans. see chart
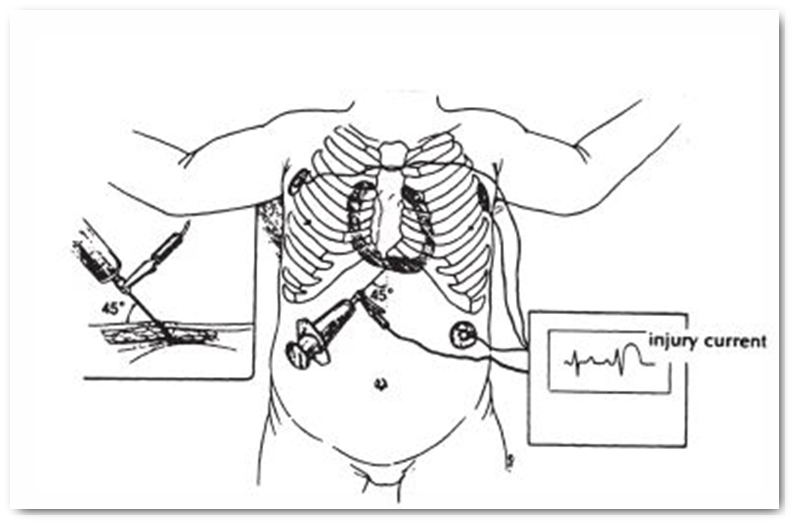
When performing pericardiocentesis, you should verify that the aspirated liquid is indeed pericardial fluid, and not blood. How can you verify this?
once aspirated, squirt fluid into a basin; pericardial fluid won’t clot
Tx for Pericarditis?
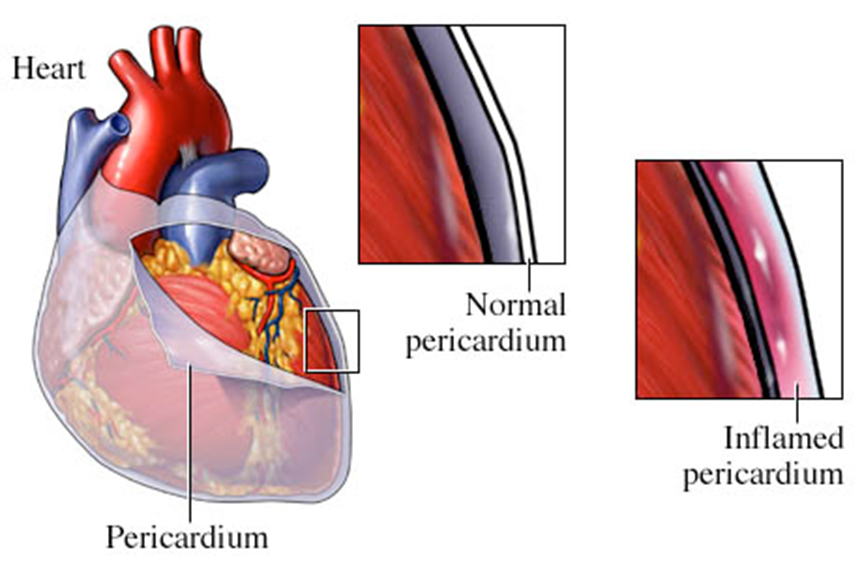
NSAIDs or Colchicine
Steroids for resistant Sx
The following agents are used for chemical cardioversion (stable patients) of WHAT rhythms? What is a non-pharm treatment you can try first?
adenosine
amiodarone
Diltazem
atropine
Adenosine (SVT)
Amiodarone (A-fib)
Diltazem (Sinus tach, Afib/Aflutter)
Atropine (Sinus Brady)
Note: may attempt vagal maneuver first; can also use fluids
Vagal maneuvers: name a few: bear down, start and IV, ICE ICE BABY (diving reflex), blow a straw/syringe
Blow, recline, lift leg as a passive leg raise
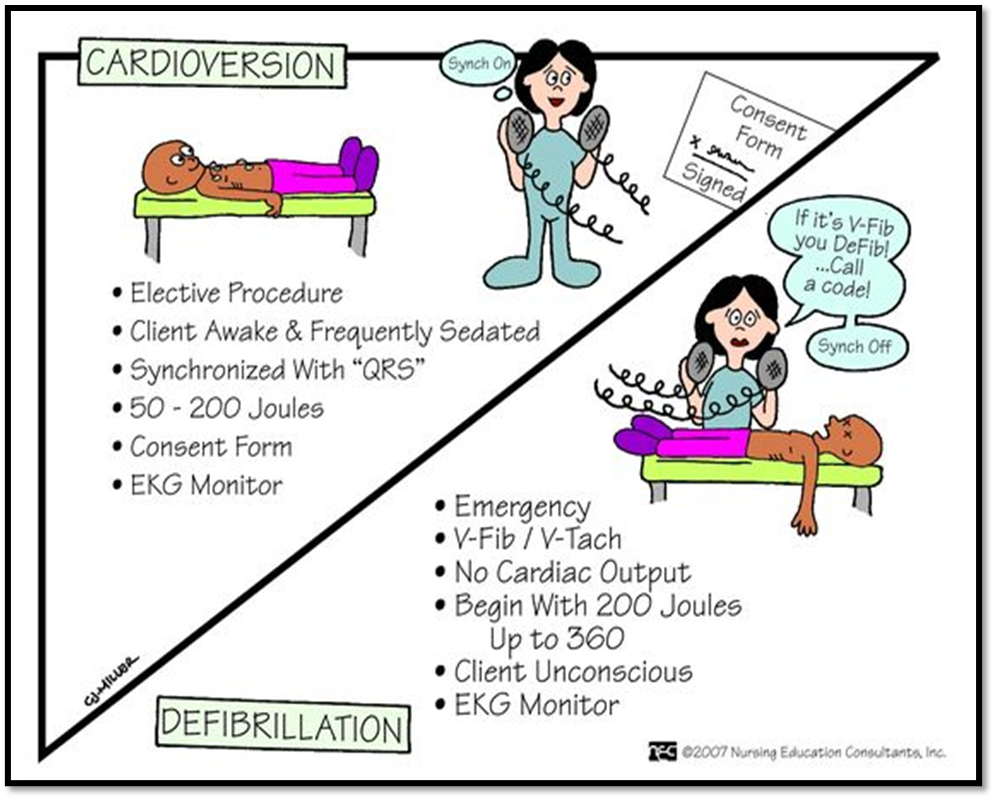
True or False - Pulseless V-tach and V fib should NOT be shocked
FALSE - DEFIB VFIB VTACH
True or False - Asystole and PEA are NOT shockable rhythms
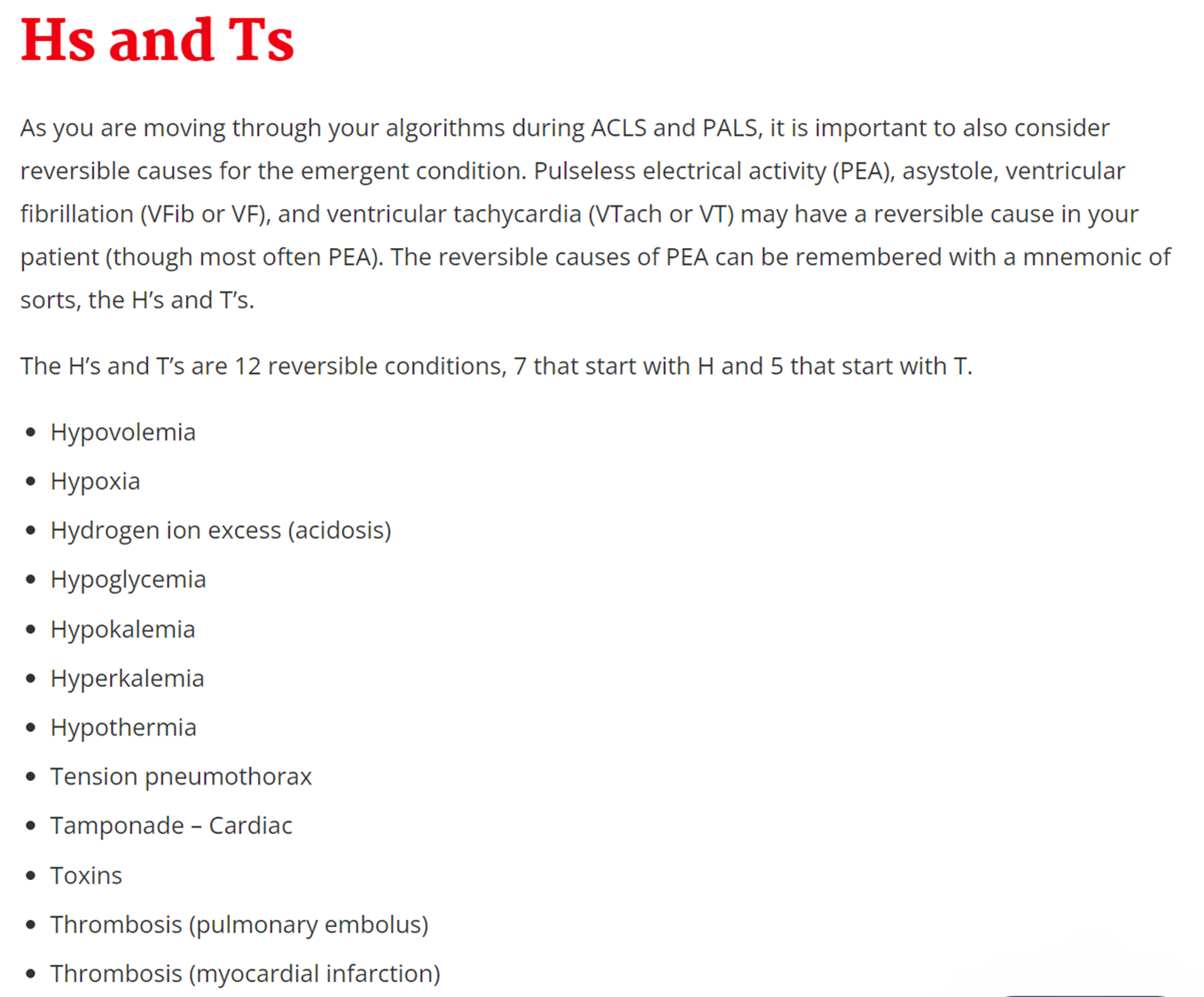
True; treatment is epinephrine, ACLS protocol (check Hs and Ts - see image)
When do we use transcutaneous pacing?
a. unstable bradycardia or 3rd degree heart block
b. pulseless V-tach / V-fb arrest
c. A-fib
d. Sinus Bradycardia
a. unstable bradycardia or 3rd degree heart block
True or False - Quinidine, Lidocaine, and Flecainide are potassium channel blockers that may increase the risk of Torsades
False - these are sodium channel blockers the lead to lower amplitude and lower conduction velocity
Note: Potassium channel blockers, such as amiodarone and sotalol may increase risk of Torsades
True or False - Diltazem, Verapamil, Digoxin, Magnesium, and Adenosine are all examples of CCBs.
True
When does Sinus Tachycardia become Supraventricular Tachycardia?
Treatment?
when rate >160
Treatment:
•Stable:
•Vagal maneuvers
•Chemical Cardioversion: adenosine (may repeat)
•Amio, cardiology consult
•Unstable:
•Synchronized Cardioversion
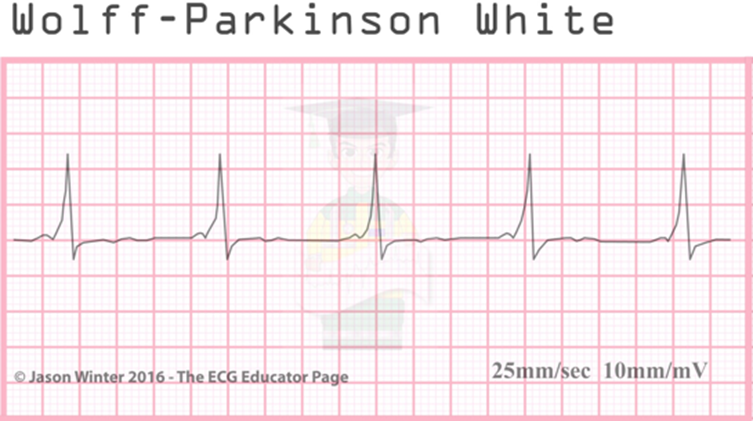
True or False - Diltazem and Digoxin are contraindicated for the treatment of Supraventricular Tachycardia
False; this is the first line therapy (beta blockers can also be used first line) EXCEPT in WPW Syndrome
True or False - Diltazem and Digoxin are contraindicated for the treatment of SVT associated with WPW syndrome, as they may lead to Vfib.
True; an alternative would include flecainide, sotalol, or ablation therapy
Which arrythmia has a congenital accessory pathway “Bundle of Kent” associated with a delta wave, is usually asymptomatic, and is associated with tachyarrhythmias and small risk of sudden cardiac death?
Wolff-Parkinson White
What is the treatment for atrial flutter?
CCB and beta adrenergic blockers
A patient with A-fib (new onset 12 hours ago) presents to ED, and they are hemodynamically stable. Next step?
next step: cardioversion
However, if it were >48 hours, you would need to do rate control with beta blockers or CCBs (if patient doesn’t have HFrEF) and anticoagulate for 3 weeks before cardioversion.
A patient who is hemodynamically unstable presents with Afib, onset 72 hours ago. Next step?
immediate electrical cardioversion
True or False - Warfarin is preferred for anticoagulation in patients with a mechanical heart valve
True
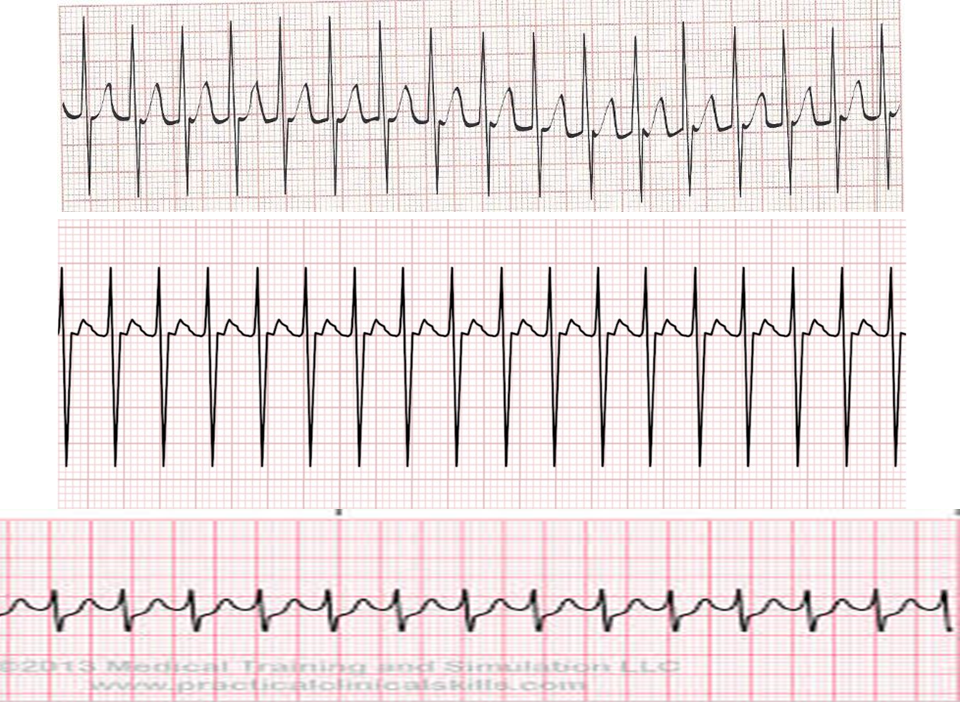
What is this rhythm?
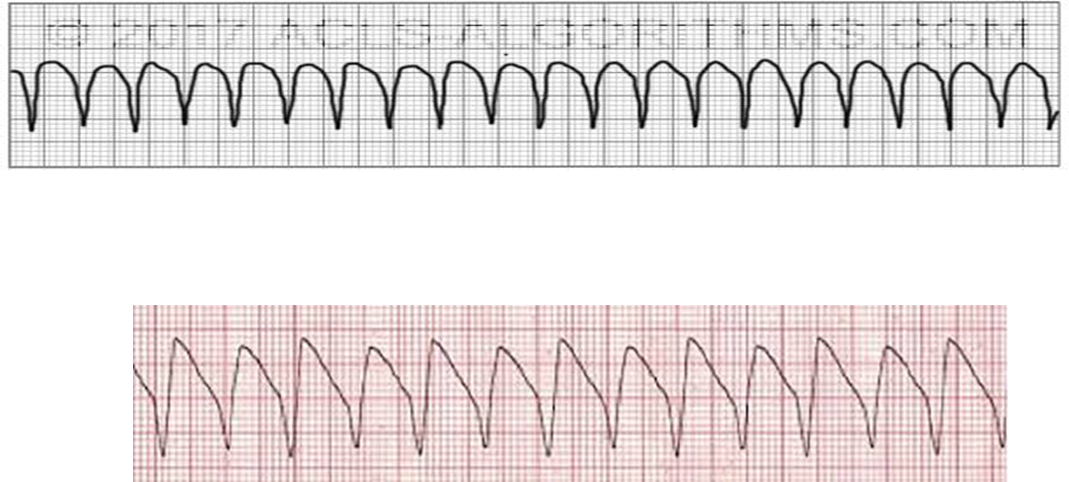
V-Tach - defib pulseless Vtach
if pulse, synchronized cardioversion
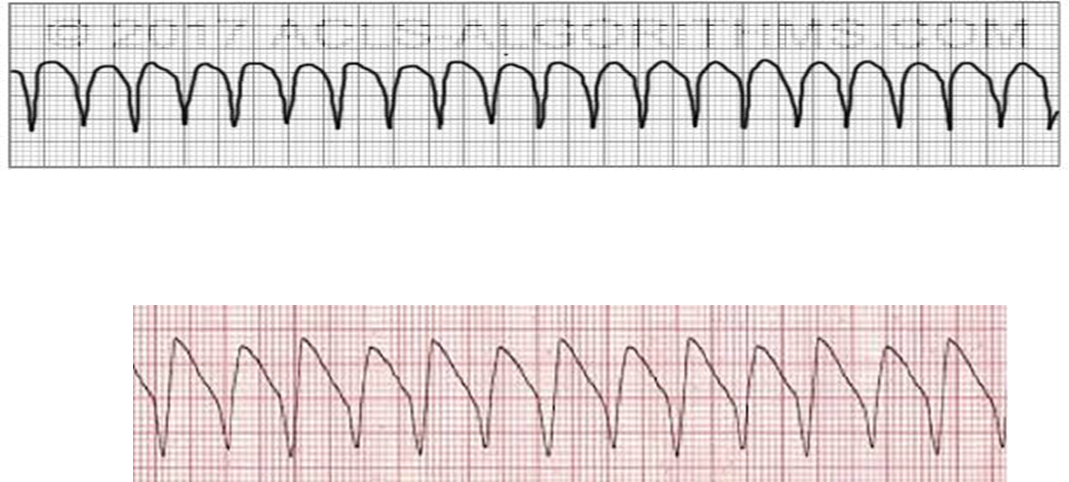
Treatment for this rhythm (and what is it?)
Torsades - Treatment is IV Mg
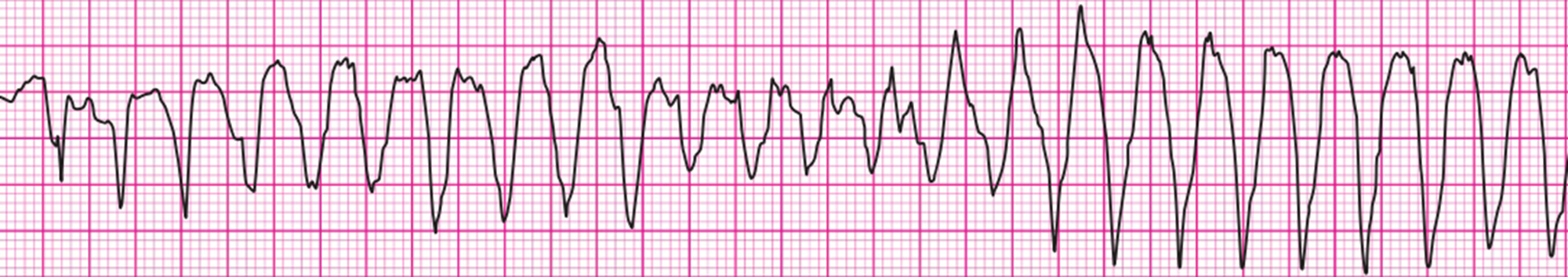
What do you do for this person?

they are dead…
Defib Vfib also chest compressions
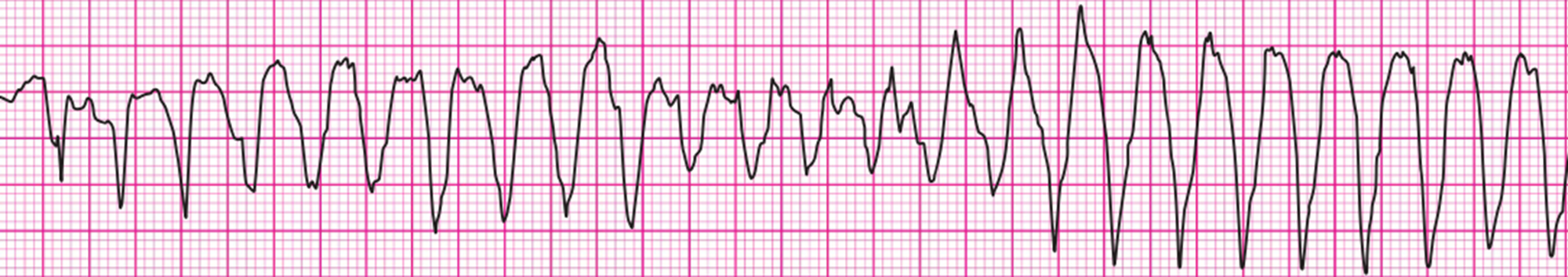
this person doesn’t have a pulse. what do you do?
PEA - chest compressions, epinephrine, H’s and T’s
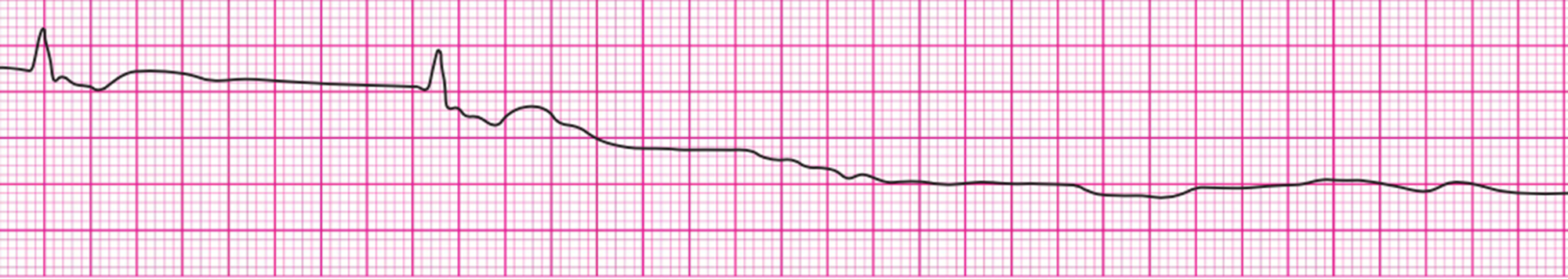
What do you do for this person?
Asystole:
make sure you aren’t missing very fine V-fib; check monitor and lead placement
treatment: CPR and Epi, H’s and T’s
DON’T SHOCK
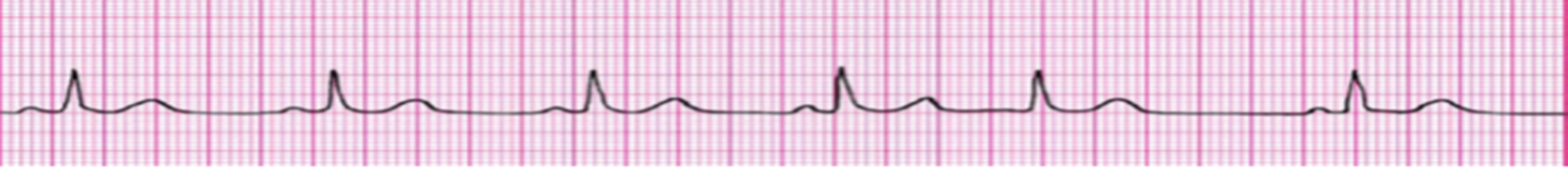
All of these heart blocks should be treated if they have a symptomatic brady arrhythmia. Which one needs a pacemaker?
a. 1st Degree heart block
b. 2nd Degree Mobitz Type 1 (Wenckebach)
c. 2nd Degree Mobitz Type 2
d. Third Degree or Complete Heart Block
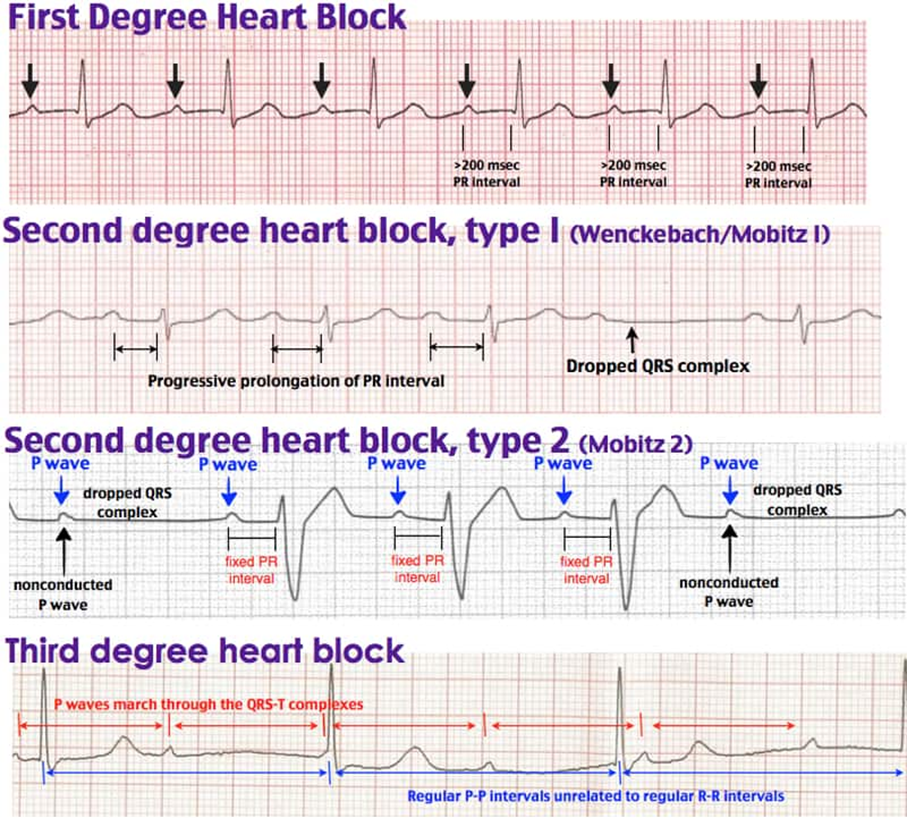
d. Third Degree of Complete Heart Block