B3.1 GAS EXCHANGE
1/12
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
13 Terms
outline gas exchange in organisms
gas exchange is a vital function in all organisms
transport of oxygen into an organism for aerobic respiration
transport of carbon dioxide out as a product of cell respiration and excreted as harmful waste (high conc of CO2 increases internal acidity
size incresases = SA:V ratio decreases
small organisms have sufficient gas exchange by simple diffusion as the distance between the exterior and their center is small
large organisms need body systems for sufficient gas exchange as the distance between the exterior and center is large
outline the properties of gas-exchange surfaces
large surface area:
more surface area available for gas exchange
highly permeable:
gas exchange occurs via diffusion (phospholipid bilayers are permeable to CO2 and O2)
thin tissue layer:
provides short diffusion distances
lungs have single layer cell between air and capillaries
moist:
water helps gases dissolve on exchange surfaces of cells
lung cells secrete moist layer on the interior to
explain the maintenance of concentration gradients at exchange surfaces in mammals
for sufficient exchange, concentration gradients must be maintained
outside: high O2, low CO2
inside: low O2, high CO2
adaptations to help maintain the steep conc gradeint include
dense networks of blood vessels: high SA of blood for increased exchange of gases
continuous blood flow: movement maintains low O2 and high CO2 internally
ventilation with air for lungs and with water for gills: movement maintains high O2 and low CO2 externally
outline the adaptations of mammalian lungs for gas exchange
branched network of bronchioles (high SA)
left/right bronchus branch into numerous bronchioles which branch into many alveoli, increasing surface area for gas exchange
high surface area (numerous alveoli)
alveoli walls composed of 2 cell types
type I pneumocyte cells
single cell layer
extremely thin specialised cell structure for short diffusion distance
type II pneumocytes’
numerous secretory vesicles which secrete a surfactant
water and compounds to break surface tension and lungs from collapsing
moist layer allows for gases to dissolve
extensive capillary beds
many capillaries surround the alveoli (dense network), creating a v short diffusion distance between alveolar space and the blood as it is only a single cell wall thick
high surface area for gas exchange, high blood flow to maintain concentration gradients
explain the process of ventilation of the lungs
ventilation (breathing) : the movement of air into and out of the lungs
muscle contractions change the volume of the lungs
increasing volume, decreasing gas pressure (inhalation, inspiration)
decreasing volume, increasing gas pressure (exhalation, expiration)
inverse relationship
air moves along pressure gradient → high to low pressure
QUIET:
inspiration:
diaphragm contracts (go down) and flattens, increasing the volume of the lungs
external intercostal muscles contract to bring the rib cage up and out, increasing lung volume
internal intercostal muscles are relaxed, decreasing pressure in the lungs
expiration:
diaphragm relaxes (goes up) moving upwards, decreasing the volume of the lungs
external intercostal muscles relax to bring the rib cage down and in, decreasing the lung volume
internal intercostal muscles contract, increasing the internal pressure in the lungs
outline the structure of hemoglobin
protein in red blood cells
composed of 4 polypeptide chains and 4 iron containing heme groups
binds to and transports:
O2 (from lungs to respiring tissues)
CO2 (from respiring tissues to lungs)
explain the term : oxygen affinity
Oxygen affinity' refers to the ability of hemoglobin to bind oxygen at a specific partial pressure of oxygen, influenced by factors like temperature, pH, and organic phosphate concentration
explain the role of hemoglobin in cooperative binding
binding of an oxygen molecule to a heme group changes the hemoglobin conformation
increases hemoglobins affinity to oxygen so the next oxygen molecules binds more easily
higher affinity in oxygen rich areas promotes oxygen loading
release of oxygen molecule changes hemoglobin conformation
decreases the hemoglobins affinity to oxygen
lower affinity in oxygen deficient areas (respiring tissues, eg muscles) promotes oxygen unloading
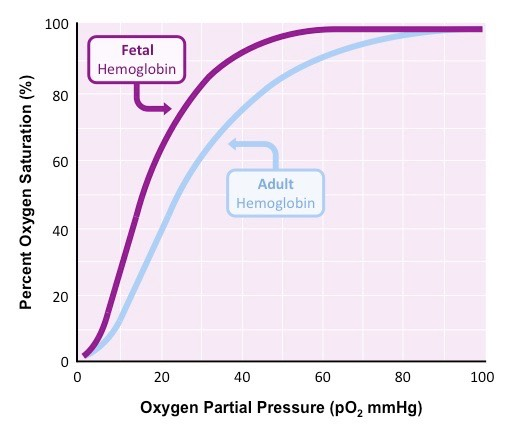
using the oxygen dissociation curve, explain the affinity of hemoglobin for oxygen at different oxygen concentrations in adults
low oxygen saturation in hemoglobin at low oxygen levels in tissue
high oxygen saturation in hemoglobin at high oxygen levels in tissue
SIGMOIDAL (S) SHAPED CURVE:
binding of first O2 molecule is difficult due to low affinity at low partial pressure of oxygen (pO2)
binding of successive O2 molecules are easier due to increase affinity at increasing partial pressure of oxygen (pO2) due to cooperative binding
maximum binding reached when hemoglobin is fully saturated, affinity plateaus at high partial pressure of oxygen
compare fetal hemoglobin (HbF) and adult hemoglobin (HbA)
HbF’s 4 polypeptide chains = 2 alpha chains + 2 gamma chains
HbA’s 4 polypeptide chains = 2 alpha chains + 2 beta chains
gamma polypeptide chains have a higher affinity to oxygen than beta chains, resulting in a higher affinity to oxygen in HbF than HbA
allows for developing fetus to obtain oxygen from mothers hemoglobin in bloodstream in the placenta
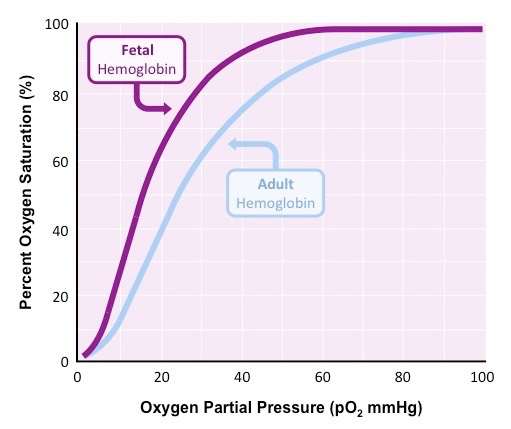
explain the fetal oxygen dissociation curve
as fetal hemoglobins have a higher affinity to oxygen that adult hemoglobin, the fetal graph shifts to the left
#nobabyleftbehind
at lower partial pressure oxygen, the fetal hemoglobin will load oxygen easier than adult hemoglobin
fetal hemoglobin will load oxygen when adult hemoglobin unloads oxygen
explain how an increase in CO2 correlates with an increased dissociation of oxygen
carbon dioxide can also bind to and transport on hemobglobin
CO2 binds at an allosteric site on the hemoglobin and not with the heme group
carbon dioxide can also cause the Bohr effect:
CO2 decreases blood pH due to the presence of carbon, resulting in conformational change so the binding of oxygen becomes less favorable
allows for oxygen unloading in areas of high partial pressure of carbon dioxide and low partial pressure of oxygen (respiring tissues)

Bohr shift: oxygen dissociation curve shifts to the RIGHT due to decreased affinity to O2
respiring tissues produce high amounts of CO2 and require high amounts of oxygen
bohr shift describes hemoglobins decrease in affinity to oxygen leadig to an increase in oxygen unloading at respiring tissues