Emergency Dept 101 (Operations, Legal Issues, Culture)
1/17
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
18 Terms
EMTALA (Emergency Medical Treatment and Labor Act)
Federal "anti-dumping" law: applies to all patients regardless of:
• ability to pay or insurance status
• national origin, race, creed, or color
Perform a medical screening examination (non-discriminatory)
Stabilize emergency medical condition
May transfer if:
-stable patient and cannot provide services
-unstable patient needs higher level care
-Call ahead and make arrangement for transfer, secure an accepting physician/provider
-Transfer forms must be completed and sent with patient
$50,000 Fines for hospital and providers
emergency medical condition
a condition manifesting itself by acute symptoms of sufficient severity (including severe pain) such that the absence of immediate medical attention could reasonably be expected to result in:
• placing the individual's health in serious jeopardy
• serious impairment to bodily functions
• serious dysfunction of bodily organs
Medical screening exam (MSE) must be completed by a provider
Emergency Medical Treatment and Labor Act
HIPAA (Health Insurance Portability & Accountability Act)
-Established national standards for protecting the privacy of health information.
-Imposes restrictions on the use and disclosure of protected health
information
-Gives patients greater access to and control over their medical records and how they are used
Only the minimum necessary amount of information should be disclosed
HIPAA (Health Insurance Portability & Accountability Act)
• Various circumstances of Death
• Child/Elder/Domestic Abuse or Neglect
• Sexual Assault (child)/Strangulation (all)
• Knife and Gunshot wounds
• Communicable Diseases
• Animal Bites
• Epilepsy - DMV
• Threat of harm to self or others (SI/HI)
Law Enforcement and Public Health Exemptions
General consent
Patients who present to the ED will sign a general consent form (in preferred native language) which means they are willing to undergo basic evaluation and treatment
Implied consent
Average/reasonable/competent patient would agree to treatment in an emergency situation if they were able to
Informed consent
obtained prior to more studies or procedures that are more invasive or have higher risks/costs (in native/preferred language) Requires that the patient be provided with:
PARQA
• Purpose and Nature of test/treatment
• Alternatives test/treatments
• Risks of doing it vs Consequences of not doing it
• Questions/Answers
Consent: Exceptions for Minors
• Emergency medical situations
• Minors who are married, pregnant, or have children
• Sexually transmitted diseases
• ETOH/Drug abuse
• Domestic/Sexual abuse
• Mental Health Issues
• Pregnancy/Abortion
*Most states a person must be 18yo and clinically/legally competent to consent
Refusal of Treatment
“a person has a constitutionally protected liberty in refusing unwanted medical treatment, even if refusal could result in death.”
Provider should try to understand why:
• ie. Financial, Religious, Misunderstanding
• Document your discussion in the chart, AMA form
• Partial treatment can be offered
Against Medical Advice (AMA)
Requirements:
1. Capacity to make decision
2. Adequate Disclosure of Risks
3. Proper Documentation
Challenges:
• Intoxicated or Psychiatric Patients - must assess decision-making capacity
• Alternative may be involuntary admission
Do Not Resuscitate (DNR)
a legal order to withhold CPR/ACLS if a person’s heart stops or they stop breathing “No-Code”
-With POLST document, can continue IV fluids, Oxygen, Medications, or any other appropriate treatments
-If you don’t have document, do everything as indicated
Negligence (Malpractice)
To prove negligence the plaintiff must establish:
-Duty to Care: the Physician-Patient Relationship was established
-Breach of Duty to Care: the provider failed to provide treatment with the knowledge/skill ordinarily used by reasonably well-qualified providers practicing in similar circumstances
-Proximate Cause: the provider’s negligence more likely than not caused the injury
-Damages: an assigned monetary value by the jury compensating for loss or injury
Statute of Limitations is 2 years in most states
Subpoena
Documents: Make sure the patient has signed a release and that your lawyer has reviewed it and informed you on how to respond correctly
Deposition: If you're deposed as a treating physician and not as a defendant then you're entitled to payment for your time/travel
Testimony: You should limit your testimony to a factual account of your treatment, as recorded in the patient's chart (Document!)
Expert witness: You are entitled to an expert's fee. You should settle the scope of your testimony and fee beforehand with the attorney requesting your appearance.
Good Samaritan Laws
Protects health-care professionals who render aid at the scene of an emergency
-Does NOT apply to ED providers seeing patients in the ED or to EMS in the field in the course of employment
Patient Abandonment
The unilateral termination of the provider-patient relationship without patient consent and without sufficient notice
ED providers have an obligation to:
-Provide adequate discharge instructions (AVS)
-Provide for appropriate follow-up care
-On-Call Provider List (required by EMTALA)
-Return to the ED instructions
-Provide translation services
-At no cost to the patient
-By a trained interpreter, family or even you are not good enough
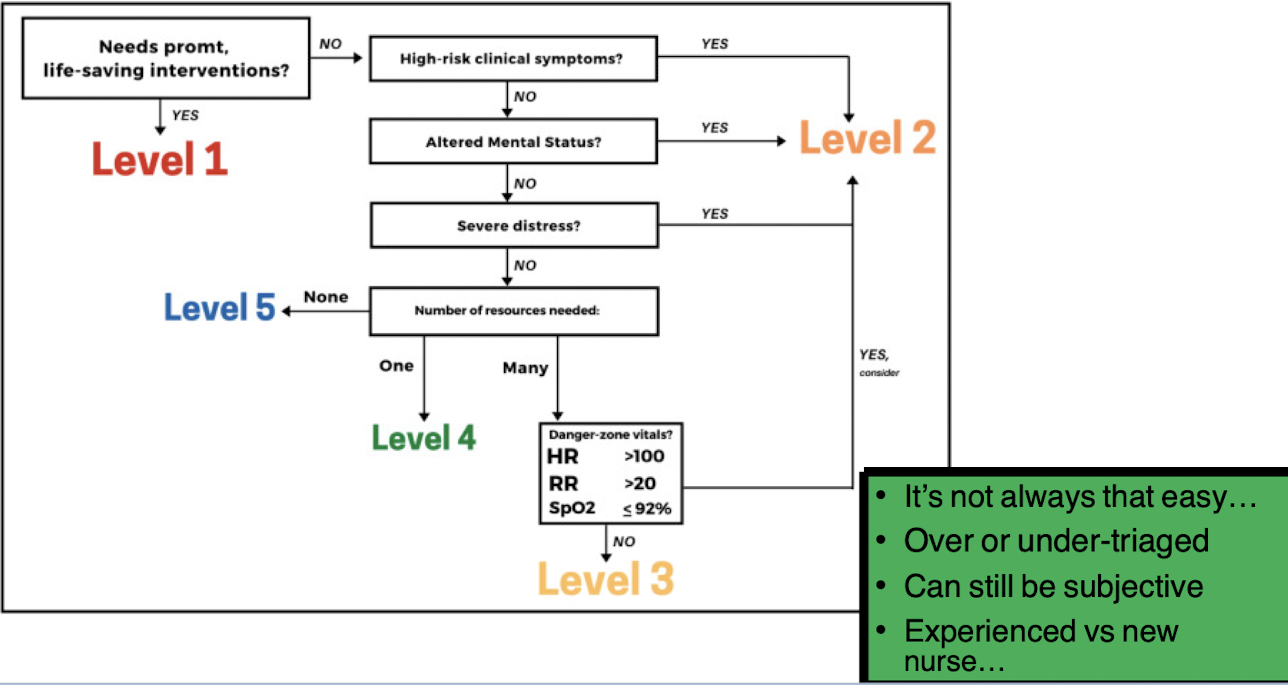
Emergency Severity Index (Triage Acuity)
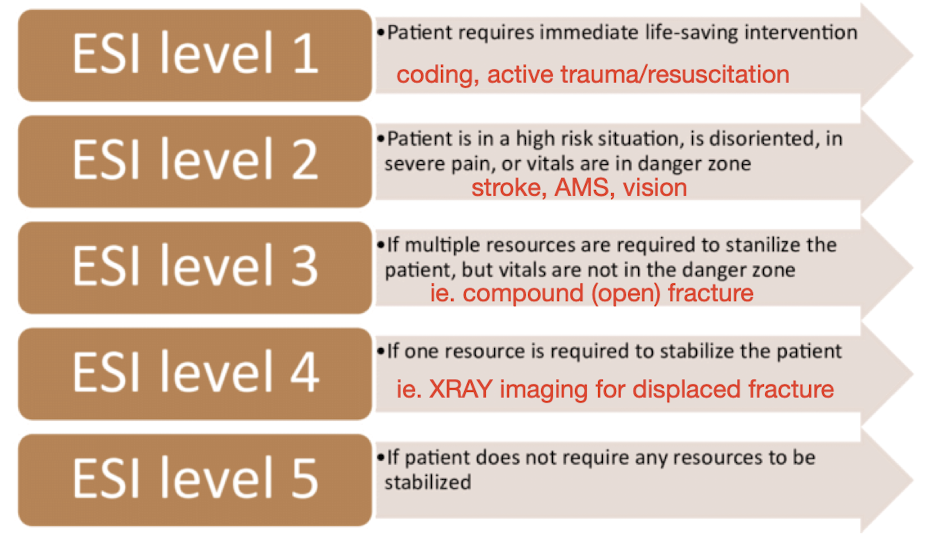
Emergency Severity Index (Triage Acuity)
Joint Commission
Who requires the hospital to assess and manage patient's pain?
Management: treatment for the pain or referral (pain management doctor or a primary care physician)