Folliculogenesis
1/13
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No study sessions yet.
14 Terms
What is folliculogenesis?
Folliculogenesis is the process of follicle growth and development, beginning with primordial follicles laid down during fetal life, through to the formation of a dominant follicle ready for ovulation. This includes oocyte growth, granulosa and theca cell proliferation, antrum formation, and hormonal regulation.
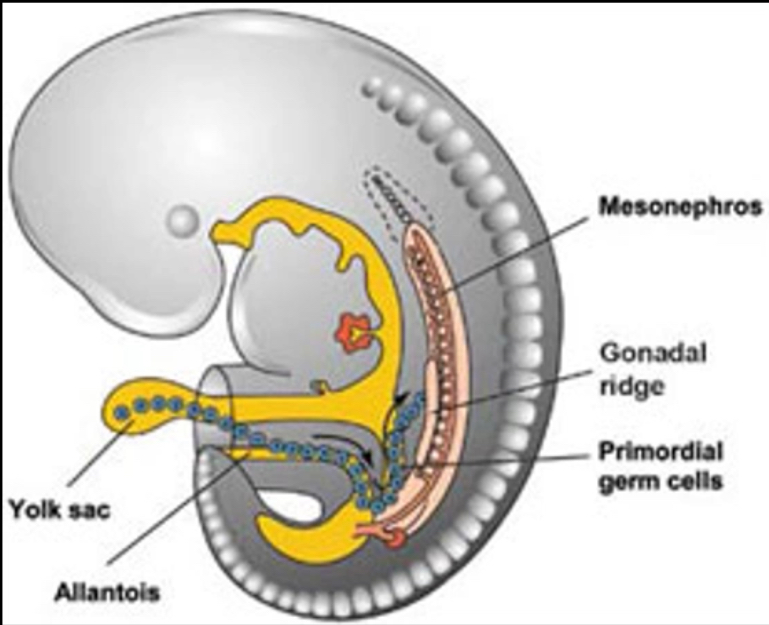
Germ cells enter the gonad
Cells that will become eggs or sperm originate from primordial germ cells (PGC)
PGCs first identifiable in the yolk sac of the developing foetus at 3 weeks after conception
Primordial germ cells
Undergo many cycles of mitosis
They migrate to the genital ridge in the foetus
The genital ridge becomes the gonad
Further differentiation of the PGC into male/female gametes depend on the sexual differentiation/development of the gonad i.e. into ovary or testis
If PGCs enter the ovary they become oocytes
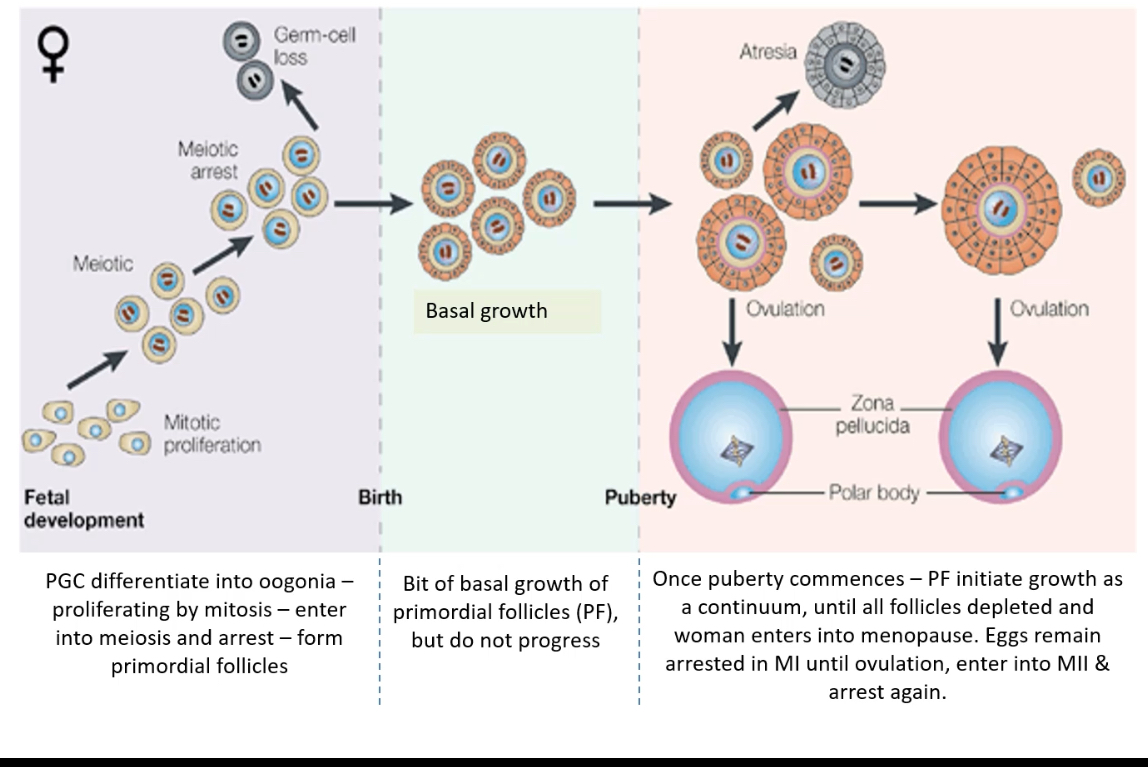
Primordial germ cells migrate to the fetal ovary early in development.
They divide by mitosis to form oogonia.
Oogonia enter meiosis I during fetal life and are then called primary oocytes.
Meiosis arrests in prophase I and remains arrested until puberty (or ovulation).
Each primary oocyte becomes surrounded by a single layer of flattened pre-granulosa cells derived from ovarian somatic cells.
This structure (primary oocyte + flattened granulosa cells) forms a primordial follicle.
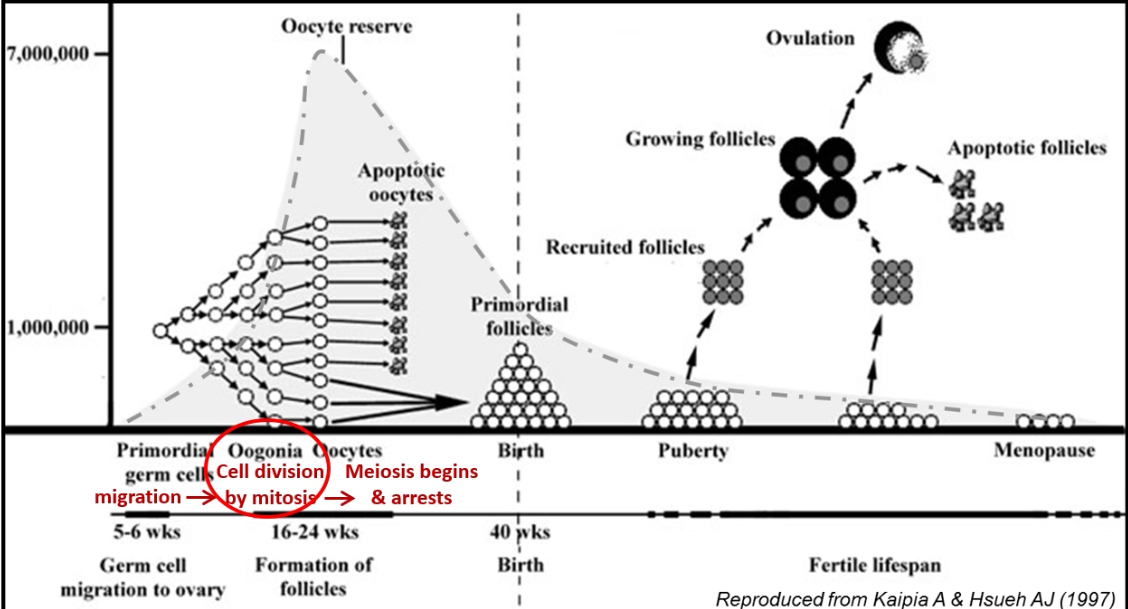
Large numbers of oocytes undergo apoptosis before birth, greatly reducing the oocyte pool.
At birth, a fixed number of primordial follicles remains (the ovarian reserve).
From puberty, small numbers of primordial follicles are recruited each cycle; most undergo atresia, and usually one ovulates.
The ovarian reserve continues to decline throughout life until menopause, when follicles are depleted.
All the eggs a woman will ever have
What is the structure of a primordial follicle and its significance?
A primordial follicle consists of a primary oocyte arrested in meiosis I, surrounded by a single layer of flattened granulosa cells and an acellular basal lamina. It represents the ovarian reserve available throughout reproductive life. These are dormant until recruited to grow.
Folliculogenesis and Oogenesis
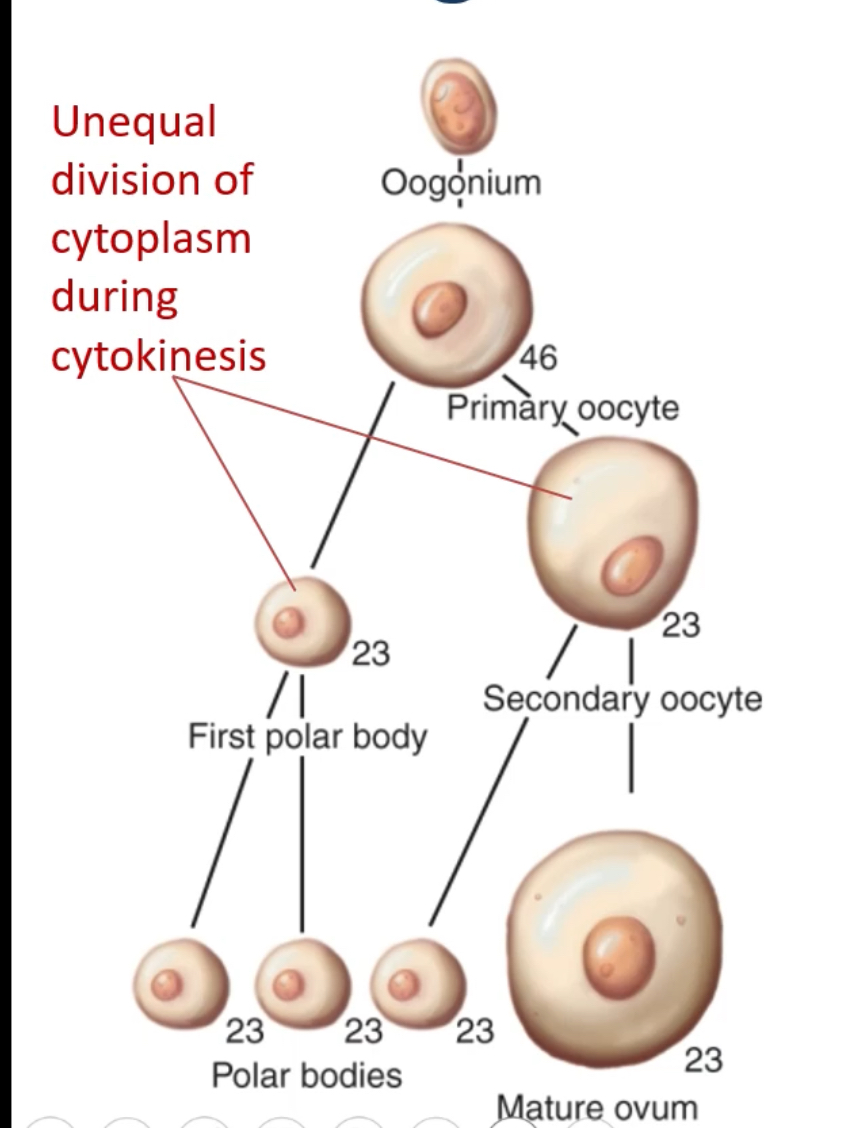
Oogenesis
Oogonium (46) develops into a primary oocyte (46).
The primary oocyte completes meiosis I with unequal cytokinesis, producing:
One secondary oocyte (23)
One first polar body (23)
The secondary oocyte begins meiosis II and arrests.
Meiosis II is completed only if fertilisation occurs, producing:
One mature ovum (23)
Additional polar bodies (23)
Unequal division ensures one large, cytoplasm-rich ovum capable of supporting early embryonic development, while polar bodies discard extra chromosomes.
Folliculogenesis and oogenesis — concise summary
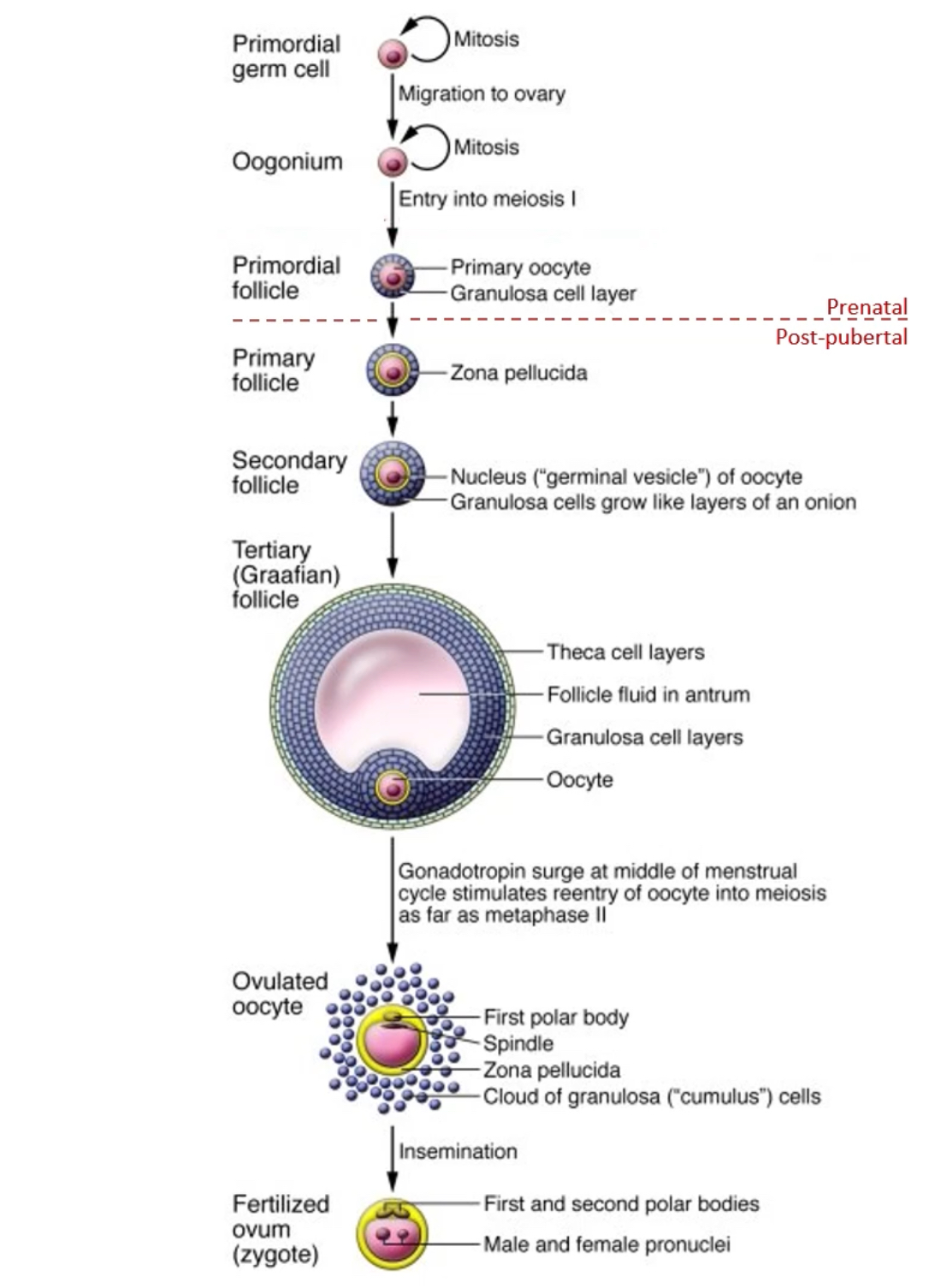
Primordial germ cells migrate to the fetal ovary and divide by mitosis to form oogonia.
Oogonia enter meiosis I during fetal life and become primary oocytes, which arrest in prophase I.
Each primary oocyte surrounded by a single layer of granulosa cells forms a primordial follicle (all formed before birth).
Post-puberty follicle development:
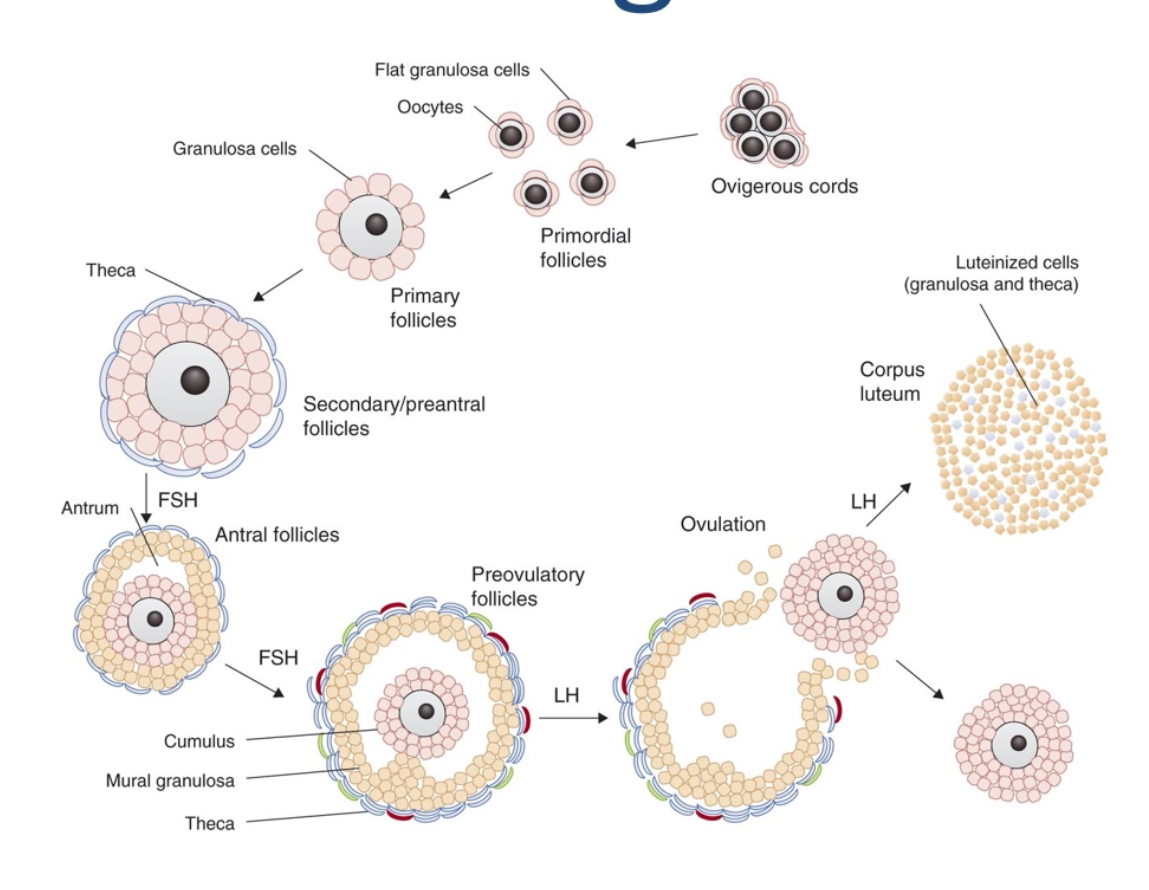
Primordial follicles are recruited to become primary follicles (zona pellucida forms).
They develop into secondary follicles, with multiple granulosa layers.
Further growth produces a tertiary (Graafian) follicle, characterised by:
An antrum (follicular fluid)
Theca cell layers
A mature oocyte surrounded by granulosa cells.
Ovulation and fertilisation:
The LH surge causes the primary oocyte to complete meiosis I, forming a secondary oocyte and the first polar body.
The secondary oocyte enters meiosis II and arrests at metaphase II.
This secondary oocyte is ovulated, surrounded by the zona pellucida and cumulus granulosa cells.
Meiosis II completes only if fertilisation occurs, producing:
A mature ovum
Additional polar bodies
Fusion of male and female pronuclei forms the zygote.
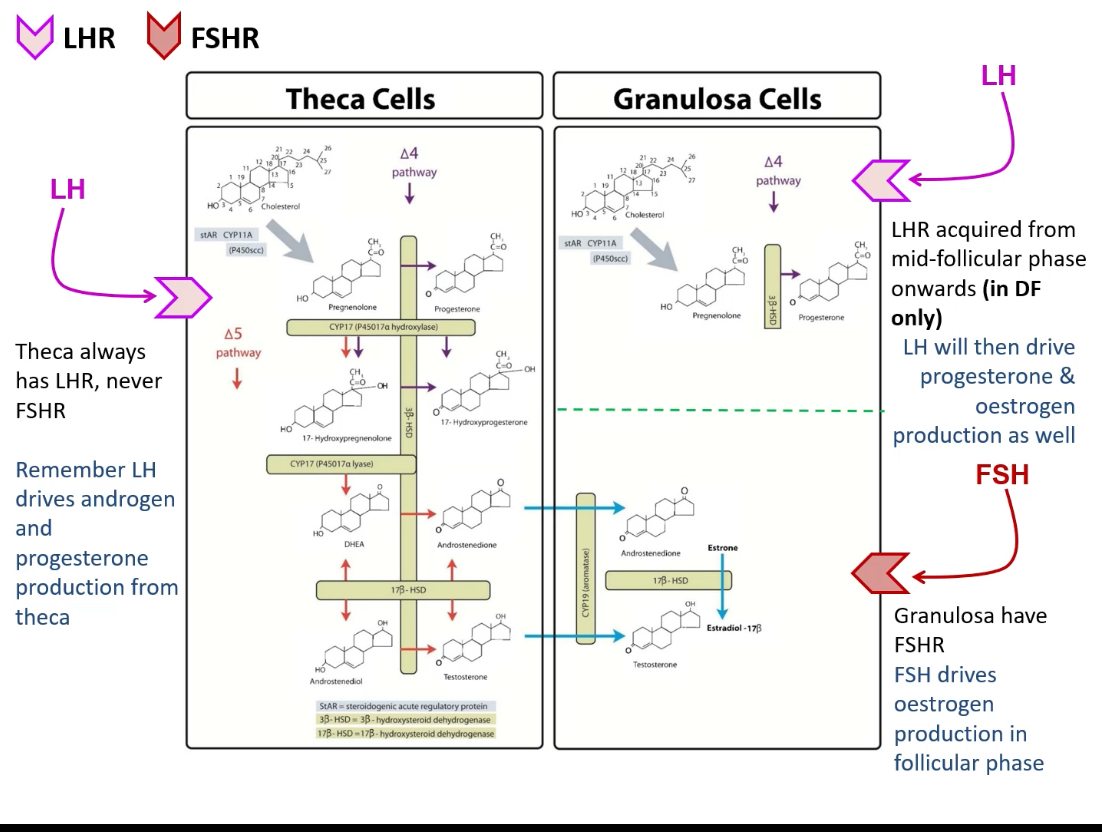
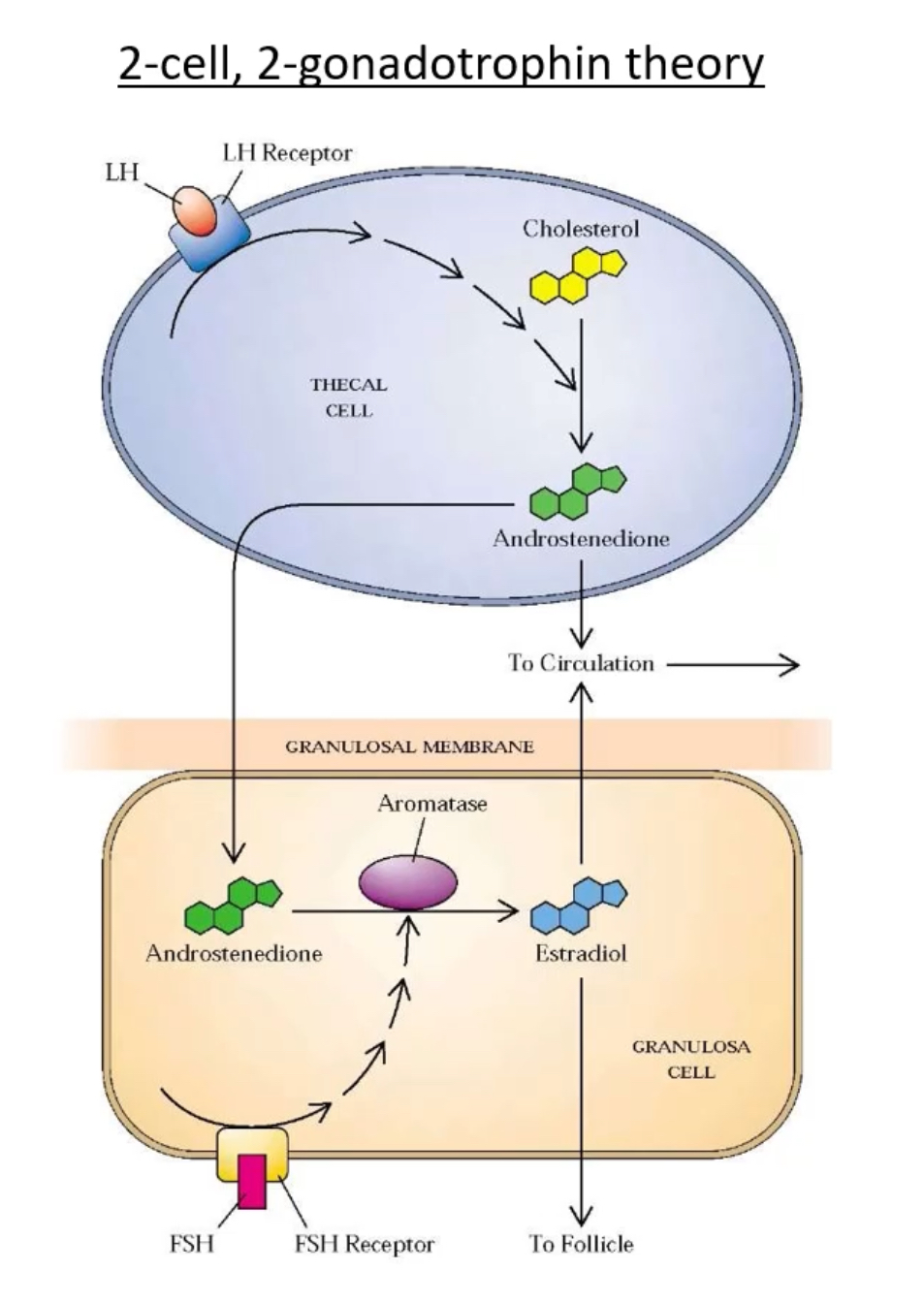
How do granulosa cells and theca cells differ in structure and function?
Granulosa cells (GCs): Arise from surrounding somatic cells, avascular, respond to FSH, produce estrogen via aromatase.
Theca cells: Form a vascularized outer layer around follicles at later stages, respond to LH, produce androgens and progesterone that GCs can convert to estrogen.
Follicle Growth
Early follicle growth starts mainly from local ovarian signals (FSH-independent). Once follicles reach the stage where they need to make an antrum and produce lots of oestrogen, growth becomes FSH-dependent.
Step-by-step:
1) A follicle “wakes up” and starts growing
• The trigger for the very start is not fully known.
• As it starts:
• Granulosa cells multiply
• The oocyte enlarges
• The oocyte is still arrested in meiosis (not dividing)
2) Early growth does not need FSH
• Even though FSH drives most folliculogenesis, the earliest stages are FSH-independent.
• Meaning: the follicle can grow at first using local ovarian factors (paracrine/autocrine signals), not pituitary FSH.
• Early follicles still grow in people with:
• FSH deficiency, or
• FSH receptor (FSHr) mutations
• Also explains the pill:
• On the combined oral contraceptive pill (COCP), FSH is suppressed
• Follicles may still start early growth, but can’t progress, so they die (atresia)
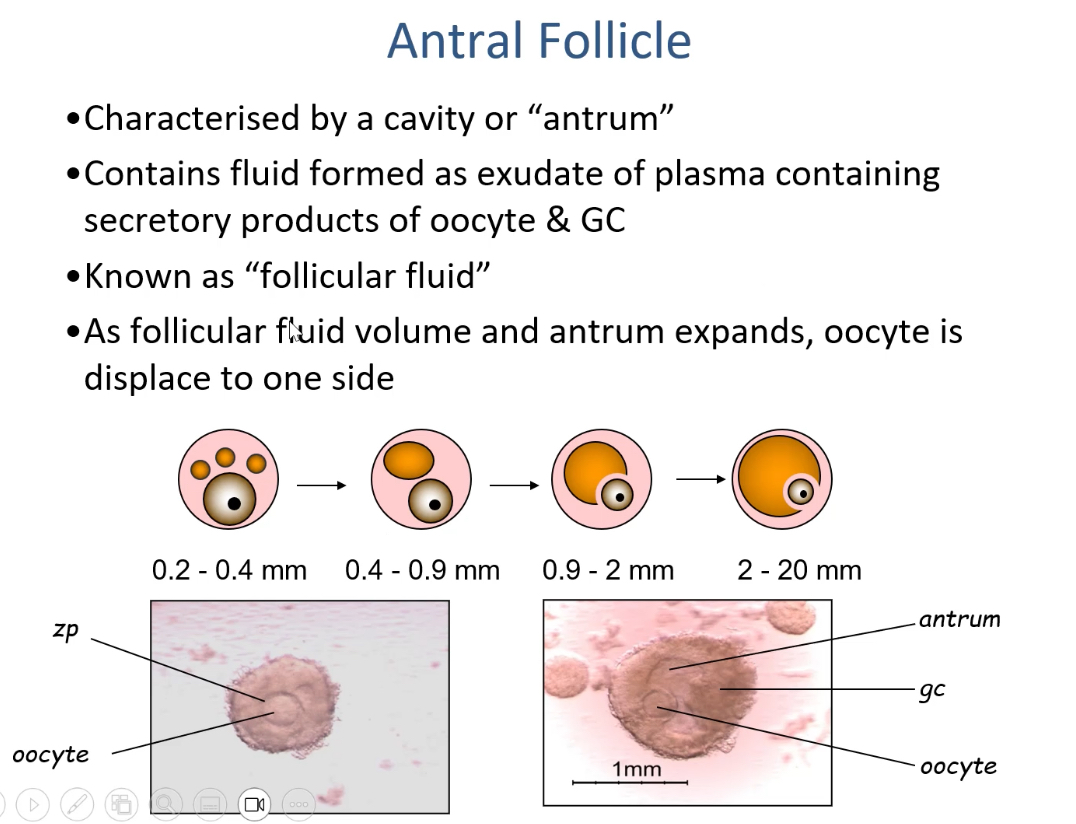
3) As the follicle grows, it changes shape internally
• The follicle increases quickly in diameter
• Granulosa cell division increases
• Small gaps appear between granulosa cells
4) Those gaps fill with fluid and merge
• The gaps become fluid-filled spaces
• These spaces join to form a central cavity called the antrum
• The antrum is filled with follicular fluid
5) Follicle growth is split into two phases (based on the antrum)
• Pre-antral phase: no antrum yet
• Antral phase: antrum present
6) What “antral/secondary follicle” means
• Once a follicle has an antrum, it’s called an:
• Antral follicle
• (Often also called a secondary follicle in many teaching schemes)
Oocyte → Zona pellucida → Granulosa cells → Antrum → Theca cells
The oocyte is a single cell.
• The oocyte is surrounded by the zona pellucida.
• Outside the zona pellucida are granulosa cells.
• The antrum is a fluid-filled cavity that forms between granulosa cells.
Explain meiosis in oocytes and where they are arrested.
Oogonia enter meiosis I to become primary oocytes and are arrested at prophase I until puberty and ovulation.
The primary oocyte resumes meiosis only when the follicle is selected for ovulation. It then progresses to metaphase II and arrests again until fertilized.
What is follicle arrest and why is it significant?
Arrest refers to oocytes halting development in meiosis I for years. It’s necessary to protect DNA integrity and coordinate with reproductive timing. Arrest also allows selection of oocytes for ovulation when hormonally appropriate.
What is follicle recruitment and selection?
Recruitment: Early antral follicles become responsive to rising FSH levels in the menstrual cycle.
Selection: Among recruited antral follicles, one becomes dominant (best at estrogen production and FSH uptake) and continues growth while others undergo atresia.
Each cycle, many follicles start growing (recruitment), but only one is chosen to ovulate (selection) based on FSH sensitivity and oestrogen production.
Recruitment (what it means)
• When: Early follicular phase of the menstrual cycle
• What: A cohort of small antral follicles (≈5–15) begins to grow together
• Why it happens:
• A rise in FSH at the end of the previous cycle stimulates growth
• Key point:
• Recruitment is not selective — multiple follicles respond initially
Result: several follicles are “in the race.”
Selection (what it means)
• When: Mid–follicular phase
• What: One follicle becomes dominant; the rest undergo atresia
• Why one wins: The dominant follicle:
• Has more FSH receptors
• Makes more oestradiol
• Produces inhibin B
• These hormones lower FSH levels, so:
• The dominant follicle (most sensitive) keeps growing
• The others lose support and die
Result: one dominant follicle remains.
Outcome
• The dominant follicle:
• Continues to grow
• Triggers the LH surge
• Ovulates
• Non-dominant follicles:
• Undergo atresia
What are preantral and antral follicles?
Preantral (primary) follicles: No fluid-filled cavity, GCs proliferate, zona pellucida forms.
Antral (secondary) follicles: Contain an antrum (fluid-filled cavity), larger, grow under hormonal control (FSH and LH).
What hormonal feedback loops regulate folliculogenesis?
GnRH from hypothalamus → FSH and LH from anterior pituitary → estrogen and progesterone from ovaries.
Other factors produced by granulosa cells of the follicle:
Inhibin (from GCs) inhibits FSH at PT
Activin activates FSH at PT
AMH (Anti-Müllerian Hormone) from small follicles inhibits recruitment of follicles
What’s the significance of the granulosa-theca cell cooperation in steroid production?
Theca cells synthesize androgens under LH.
Granulosa cells convert androgens to estrogens via aromatase under FSH.
Late-stage granulosa cells acquire LH receptors allowing them to also produce progesterone.
What is follicular atresia and how common is it?
Atresia is the programmed degeneration of follicles not selected for ovulation. It affects 99.9% of follicles throughout reproductive life; only about 400–500 ovulate.
Why is ovarian angiogenesis important in folliculogenesis?
The vascular theca layer provides follicles with essential nutrients, oxygen, and hormonal signals. It supports steroidogenesis, especially during antral stages and luteinization.