Venous Thromboembolism
0.0(0)
Card Sorting
1/115
Earn XP
Description and Tags
Last updated 7:50 AM on 3/5/23
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
116 Terms
1
New cards
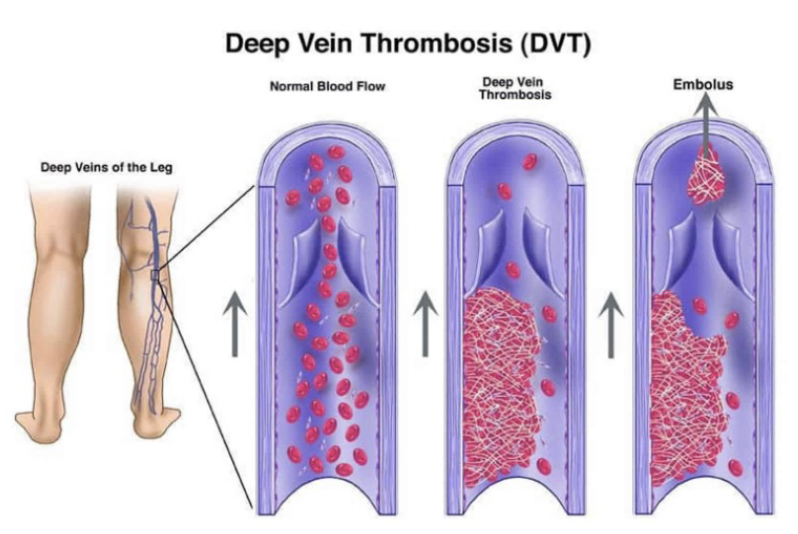
2 Types of Venous Thromboembolism
* Pulmonary Embolism (PE)
* Deep Vein Thrombosis (DVT)
* Deep Vein Thrombosis (DVT)
2
New cards
Venous Thromboembolism Homeostasis
Blood clot forms to prevent excessive bleeding
3
New cards
Venous Thromboembolism Homeostasis - Containment Mechanisms
Natural anticoagulants act to control/limit thrombin formation
4
New cards
Thrombosis
Blood clots block veins or arteries
5
New cards
Risk Factors
* Recent trauma
* Immobilization ≥3 days or surgery in the previous 4 weeks
* Major surgery
* Obesity
* Cancer
* Pregnant
* Replacement hormone therapy
* Smoking
* Burns
* After age 50
* Men > Women
* Ethnicity
* African Americans
* Caucasians
* Genetic Risk Factors
* Factor V Leiden
* Prothrombin 20210
* Antithrombin, Protein C, and Protein S deficiency
* Immobilization ≥3 days or surgery in the previous 4 weeks
* Major surgery
* Obesity
* Cancer
* Pregnant
* Replacement hormone therapy
* Smoking
* Burns
* After age 50
* Men > Women
* Ethnicity
* African Americans
* Caucasians
* Genetic Risk Factors
* Factor V Leiden
* Prothrombin 20210
* Antithrombin, Protein C, and Protein S deficiency
6
New cards
Virchow’s Triad
Thrombosis Formation
* Hypercoagulability
* Vascular damage
* Venous stasis
* Hypercoagulability
* Vascular damage
* Venous stasis
7
New cards
Virchow’s Triad - Hypercoagulability Risk Factors
* Genetic Disorders
* History of VTE
* Anti-phospholipid antibodies
* Pregnancy
* Estrogen
* Cancer
* Sepsis
* Smoking
* History of VTE
* Anti-phospholipid antibodies
* Pregnancy
* Estrogen
* Cancer
* Sepsis
* Smoking
8
New cards
Virchow’s Triad - Vascular Damage Risk Factors
* Trauma/surgery
* Chemical irritation
* Valve disease/replacement
* Atherosclerosis
* Spinal cord injury
* Chemical irritation
* Valve disease/replacement
* Atherosclerosis
* Spinal cord injury
9
New cards
Virchow’s Triad - Venous Stasis Risk Factors
* Immobility/Air travel
* Atrial Fibrillation/Stroke
* Left ventricular dysfunction
* Obesity
* Varicose Veins
* Atrial Fibrillation/Stroke
* Left ventricular dysfunction
* Obesity
* Varicose Veins
10
New cards
Venous Thromboembolism Signs/Symptoms
* Respiratory symptoms
* Signs of massive Pulmonary Embolism (PE)
* __**Anxiety**__
* __**Asymptomatic**__
* Extremity symptoms
* Cardiac symptoms
* Signs of massive Pulmonary Embolism (PE)
* __**Anxiety**__
* __**Asymptomatic**__
* Extremity symptoms
* Cardiac symptoms
11
New cards
Venous Thromboembolism Signs/Symptoms - Respiratory Symptoms
* Cough/rales
* Shortness of breath ( PO2)
* Tachypnea (>20 bpm)
* Shortness of breath ( PO2)
* Tachypnea (>20 bpm)
12
New cards
Venous Thromboembolism Signs/Symptoms - Signs of Massive PE
* Lightheaded
* Cyanotic
* Cyanotic
13
New cards
Venous Thromboembolism Signs/Symptoms - Extremity Symptoms
* Pain in affected extremity
* Redness
* Swelling
* Warmth and tenderness
* Redness
* Swelling
* Warmth and tenderness
14
New cards
Venous Thromboembolism Signs/Symptoms - Cardiac Symptoms
* Chest pain
* Tachycardia (>100 bpm)
* Jugular venous distension
* Hemoptysis
* Diaphoresis (sweating)
* Palpitations
* Tachycardia (>100 bpm)
* Jugular venous distension
* Hemoptysis
* Diaphoresis (sweating)
* Palpitations
15
New cards
Pretest Probability of Deep Vein Thrombosis (Wells Criteria) - Clinical Features and Scoring
* Active cancer (treatment ongoing or within previous 6 months of palliative treatment) - Score 1
* Paralysis, paresis, or recent immobilization of the lower extremities - Score 1
* Recently bedridden for >3 days or major surgery within 4 weeks - Score 1
* Collateral superficial veins (not varicose) - Score 1
* Localized tenderness along the distribution of the deep venous system - Score 1
* Entire leg swollen - Score 1
* Calf swelling by >3 cm when compared with asymptomatic leg - Score 1
* Pitting edema (greater in the symptomatic leg) - Score 1
* Paralysis, paresis, or recent immobilization of the lower extremities - Score 1
* Recently bedridden for >3 days or major surgery within 4 weeks - Score 1
* Collateral superficial veins (not varicose) - Score 1
* Localized tenderness along the distribution of the deep venous system - Score 1
* Entire leg swollen - Score 1
* Calf swelling by >3 cm when compared with asymptomatic leg - Score 1
* Pitting edema (greater in the symptomatic leg) - Score 1
16
New cards
Pretest Probability of Deep Vein Thrombosis (Wells Criteria) - Score Interpretation
* DVT likely ≥ 2, DVT unlikely ≤ 1
* High probability ≥ 3
* Moderate probability 1-2
* Low probability ≤ 0
* High probability ≥ 3
* Moderate probability 1-2
* Low probability ≤ 0
17
New cards
Pretest Probability of Pulmonary Embolism (Wells Criteria) - Clinical Features and Scoring
* Clinical signs and symptoms of DVT (leg swelling and pain with palpation of the deep veins) - Score 3.0
* Alternative diagnosis less likely than PE - Score 3.0
* Heart rate >100 bpm - Score 1.5
* Immobilization ≥3 days or surgery in the previous four week - Score 1.5
* Previous PE or DVT - Score 1.5
* Hemoptysis - Score 1.0
* Malignancy (receiving treatment or treated in past 6 months or palliative) - Score 1.0
* Alternative diagnosis less likely than PE - Score 3.0
* Heart rate >100 bpm - Score 1.5
* Immobilization ≥3 days or surgery in the previous four week - Score 1.5
* Previous PE or DVT - Score 1.5
* Hemoptysis - Score 1.0
* Malignancy (receiving treatment or treated in past 6 months or palliative) - Score 1.0
18
New cards
Pretest Probability of Pulmonary Embolism (Wells Criteria) - Score Interpretation
PE likely > 4; PE unlikely ≤ 4.0
* High probability > 6
* Moderate probability 2-6
* Low probability < 2
* High probability > 6
* Moderate probability 2-6
* Low probability < 2
19
New cards
Laboratory Tests
* D-dimer
* Arterial blood gases
* Arterial blood gases
20
New cards
Laboratory Tests: D-dimer
* Fibrin degradation product
* Sensitive but __NOT__ specific
* Sensitive but __NOT__ specific
21
New cards
Abnormal D-dimer Value
>500 ng/mL
22
New cards
D-dimer False Positives
* Recent surgery or trauma
* Pregnancy
* Increasing age
* Cancer
* Infection
* COVID
* Pregnancy
* Increasing age
* Cancer
* Infection
* COVID
23
New cards
Laboratory Tests - Arterial Blood Gases
* pO2 and pCO2 decreased
* Not reliable diagnostic
* Not reliable diagnostic
24
New cards
Diagnostic Studies - Gold Standard for Pulmonary Embolism (PE)
* Pulmonary angiography (radiographic contrast)
* __**INVASIVE**__
* __**INVASIVE**__
25
New cards
Diagnostic Studies - Gold Standard for Deep Vein Thrombosis (DVT)
* Venogram (radiographic contrast)
* __**INVASIVE**__
* __**INVASIVE**__
26
New cards
Diagnostic Studies - Other Options
* Ultrasonography
* __**Most common for DVT (less invasive than Venogram)**__
* Computed tomography (CT) scan
* __**Most Common for PE (less invasive than pulmonary angiography)**__
* Echocardiogram (ECHO)
* Ventilation-perfusion (V/Q) lung scan
* Reserved for patient’s with an allergy to contrast or those with renal impairment
* __**Most common for DVT (less invasive than Venogram)**__
* Computed tomography (CT) scan
* __**Most Common for PE (less invasive than pulmonary angiography)**__
* Echocardiogram (ECHO)
* Ventilation-perfusion (V/Q) lung scan
* Reserved for patient’s with an allergy to contrast or those with renal impairment
27
New cards
Pulmonary Embolism Classification
* Massive PE
* Submassive PE
* Low-Risk PE
* Submassive PE
* Low-Risk PE
28
New cards
Pulmonary Embolism Classification - Massive PE
Acute PE with sustained hypotension defined as:
* SBP
* SBP
29
New cards
Massive PE are __**NOT**__ Due to
* Arrhythmias
* Hypovolemia
* Sepsis
* Left ventricular dysfunction
* Hypovolemia
* Sepsis
* Left ventricular dysfunction
30
New cards
Pulmonary Embolism Classification - Submassive PE
Acute PE WITHOUT systemic hypotension BUT with either:
* __**Right Ventricular Dysfunction**__ (at least 1 of the following):
* Dilation or systolic dysfunction on echocardiography
* Dilation on Catscan
* Elevation of BNP (>90 pg/mL)
* Elevation of N-terminal pro-BNP ( > 500 pg/mg)
* Electrocardiographic changes
* __**Myocardial Necrosis**__ defined as:
* Elevation of troponin I (>0.4 ng/mL)
* Elevation of troponin T (>0.1 ng/mL)
* __**Right Ventricular Dysfunction**__ (at least 1 of the following):
* Dilation or systolic dysfunction on echocardiography
* Dilation on Catscan
* Elevation of BNP (>90 pg/mL)
* Elevation of N-terminal pro-BNP ( > 500 pg/mg)
* Electrocardiographic changes
* __**Myocardial Necrosis**__ defined as:
* Elevation of troponin I (>0.4 ng/mL)
* Elevation of troponin T (>0.1 ng/mL)
31
New cards
Pulmonary Embolism Classification: Low-Risk PE
Acute PE and the __**ABSENCE**__ of clinical markers of adverse \n prognosis that define massive and submassive PE
32
New cards
Venous Thromboembolism - Goals of Therapy
* Prevent thrombus extension and embolization
* Reduce Recurrent risk
* 33% will have a recurrence within 10 years
* Prevent long-term complications
* Post thrombotic syndrome
* Chronic thromboembolic pulmonary hypertension
* Reduce the risk of bleeding
* Reduce Recurrent risk
* 33% will have a recurrence within 10 years
* Prevent long-term complications
* Post thrombotic syndrome
* Chronic thromboembolic pulmonary hypertension
* Reduce the risk of bleeding
33
New cards
Provoked Venous Thromboembolism (VTE)
Identifiable transient medical or surgical risk factor
34
New cards
Provoked Venous Thromboembolism (VTE) Examples
* Surgery
* Hospital admission
* Immobility
* Pregnancy
* Hospital admission
* Immobility
* Pregnancy
35
New cards
Unprovoked Venous Thromboembolism (VTE)
No identifiable event or provoking risk factor
36
New cards
Hypercoagulable Disorders and Venous Thromboembolism
* Many patients with hypercoagulable disorders experience a first VTE only when experiencing a transient risk factor (surgery or long travel)
* Risk of recurrence therefore is concerning even when a transient event passes
* Risk of recurrence therefore is concerning even when a transient event passes
37
New cards
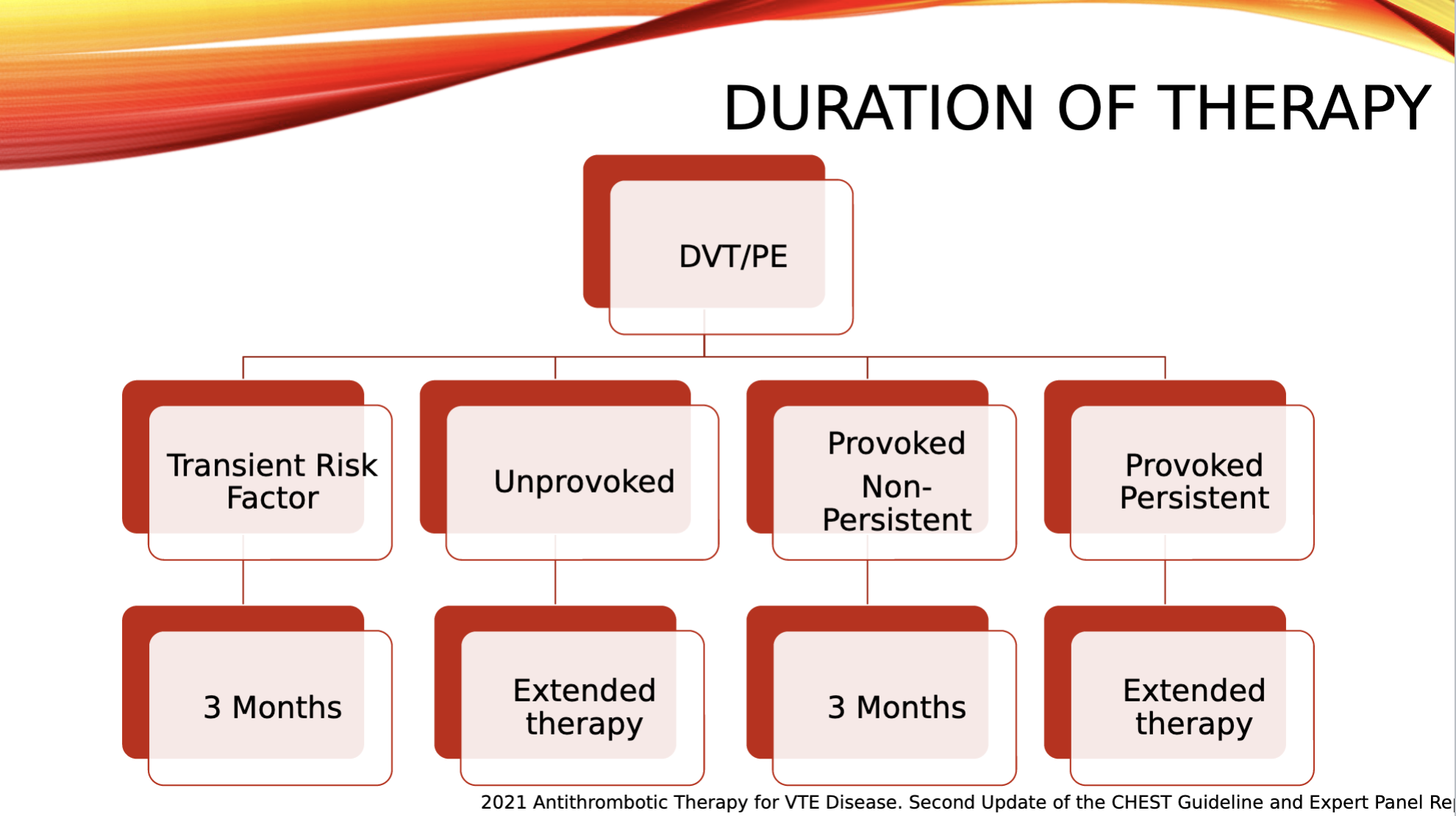
Duration of Therapy: DVT/PE
38
New cards
Provoked/Non-Persistent vs Provoked Persistent
* Provoked/Non-Persistent: Condition that is not persistent and can be __**MODIFIED**__ (ex. surgery)
* Provoked Persistent: Has a condition that is persistent that is NOT going away/__**UNMODIFIABLE**__ (ex. Genetic factors)
* Provoked Persistent: Has a condition that is persistent that is NOT going away/__**UNMODIFIABLE**__ (ex. Genetic factors)
39
New cards
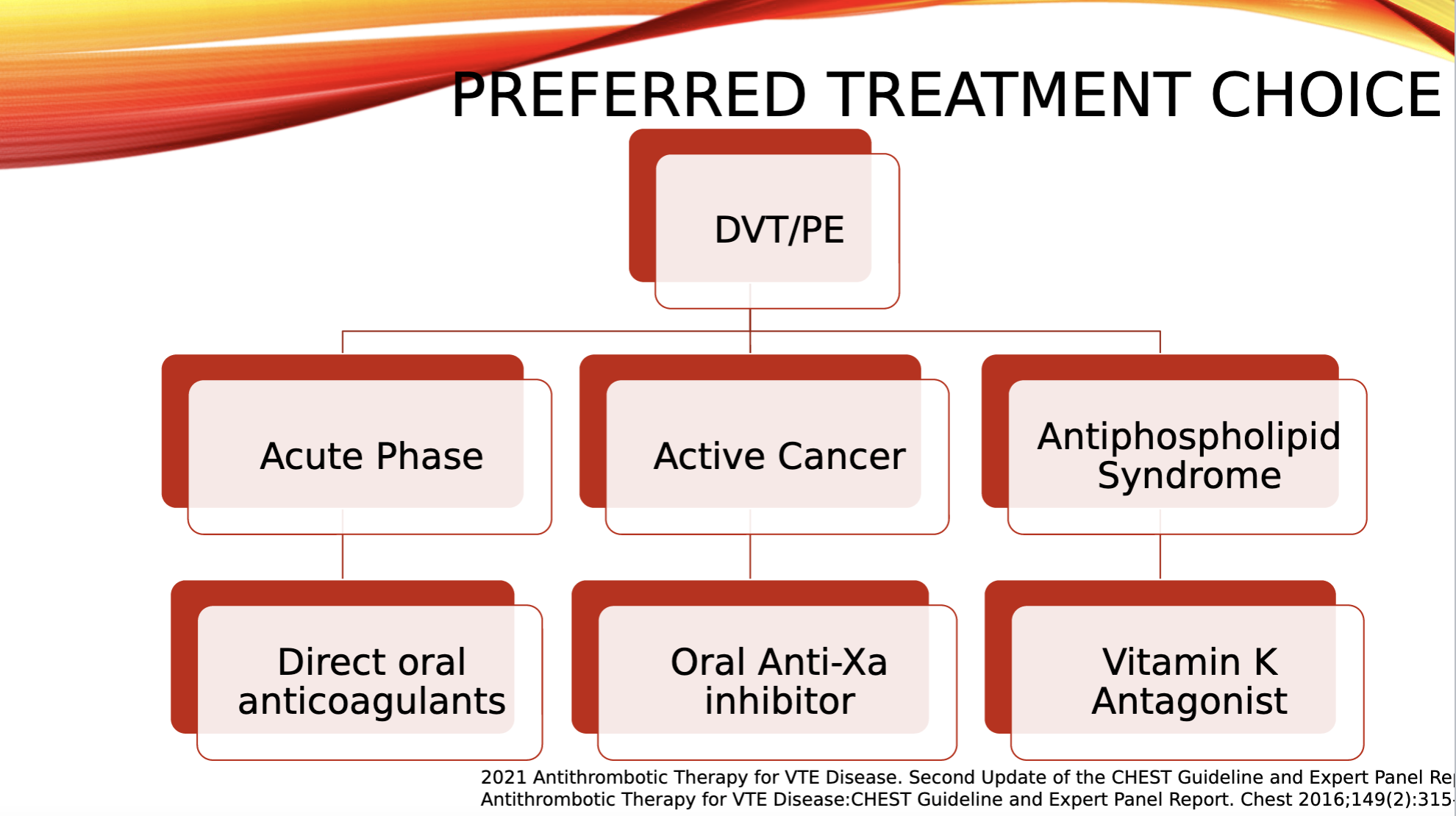
Preferred Treatment Choice: DVT/PE
40
New cards
Preferred Extended Treatment Choice
* Reduced-dose apixaban or rivaroxaban is recommended over full-dose apixaban or rivaroxaban
* Apixaban 2.5 mg PO BID (__**NEVER DOSE REDUCE**__)
* Rivaroxaban 10 mg PO daily
* Alternatively, patients could continue their warfarin or other anticoagulants
* __Warfarin needs to be bridged with heparin__
* Apixaban 2.5 mg PO BID (__**NEVER DOSE REDUCE**__)
* Rivaroxaban 10 mg PO daily
* Alternatively, patients could continue their warfarin or other anticoagulants
* __Warfarin needs to be bridged with heparin__
41
New cards
Aspirin Role in VTE Therapy
* Those with __**unprovoked DVT or PE who are**__ __**stopping anticoagulant therapy**__ and __**do not have a**__ __**contraindication to aspirin,**__ recommend aspirin over no aspirin to prevent recurrent VTE
* Only for patients who refuse anticoagulants
* Extended ASA therapy reduced recurrent VTE by 1/3
* Anticoagulant > ASA at prevention of recurrent VTE
* Only for patients who refuse anticoagulants
* Extended ASA therapy reduced recurrent VTE by 1/3
* Anticoagulant > ASA at prevention of recurrent VTE
42
New cards
Treatment Management DVT/PE - Intravenous Anticoagulation
* Heparin
* Low-Molecular Weight Heparin
* Fondaparinux
* Low-Molecular Weight Heparin
* Fondaparinux
43
New cards
Treatment Management DVT/PE - Oral Anticoagulation
* Warfarin (Coumadin ®)
* Apixaban (Eliquis®)
* Rivaroxaban (Xarelto®)
* Edoxaban (Savasya®)
* Dabigatran (Pradaxa®)
* Apixaban (Eliquis®)
* Rivaroxaban (Xarelto®)
* Edoxaban (Savasya®)
* Dabigatran (Pradaxa®)
44
New cards
Heparin Target
* XIIa
* XIa
* Ixa
* VIIa
* Xa
* XIa
* Ixa
* VIIa
* Xa
45
New cards
Heparin Elimination
Dual mechanisms
46
New cards
Enoxaparin Target
Factor Xa and IIa
47
New cards
Enoxaparin Elimination
Extensively renal
48
New cards
Fondaparnox Target
Factor Xa
49
New cards
Fondaparnox Elimination
Urine (up to 77%)
50
New cards
Unfractionated Heparin MOA
Accelerates the activity of antithrombin III to inactive thrombin
51
New cards
Unfractionated Heparin Dosing
* For VTE: 80 unit/kg IV bolus x1 (maximum bolus dose = 10,000 units)
* Followed by initial infusion rate of 18 units/kg/hr
* Followed by initial infusion rate of 18 units/kg/hr
52
New cards
Unfractionated Heparin Monitoring
* Activated partial thromboplastin time (aPTT)
* Anti-factor Xa activity (anti-Xa level)
* Complete blood count (Hgb, Hct, Plts)
* Anti-factor Xa activity (anti-Xa level)
* Complete blood count (Hgb, Hct, Plts)
53
New cards
Unfractionated Heparin Side Effects
* Bleeding
* Thrombocytopenia
* Alopecia
* Osteoporosis
* Thrombocytopenia
* Alopecia
* Osteoporosis
54
New cards
Unfractionated Heparin Contraindication
* Severe thrombocytopenia
* Heparin-induced thrombocytopenia (HIT)
* Uncontrolled active bleeding
* Heparin-induced thrombocytopenia (HIT)
* Uncontrolled active bleeding
55
New cards
Unfractionated Heparin Counseling Points
If Heparin-induced thrombocytopenia (HIT) develops → __**STOP ALL**__ heparin products
56
New cards
Low Molecular Weight Heparin (LMWH) MOA
Catalyzes the action of antithrombin, leading to inactivation of coagulation factor Xa and factor IIa
57
New cards
Low Molecular Weight Heparin (LMWH) Dosing - Enoxaparin (Lovenox)
* Preferred: 1 mg/kg sc every BID
* Alternative: 1.5 mg/kg sc daily
* Alternative: 1.5 mg/kg sc daily
58
New cards
Low Molecular Weight Heparin (LMWH) Dosing - Dalteparin (Fragmin)
Active cancer: 200 units/kg sc daily
59
New cards
Low Molecular Weight Heparin (LMWH) Monitoring
* Complete blood count (Hgb, Hct, Ptts) and serum creatinine
* __**Routine monitoring with anti-Xa activity not recommended**__
* __**Routine monitoring with anti-Xa activity not recommended**__
60
New cards
Low Molecular Weight Heparin (LMWH) Side Effects
* Bleeding
* Thrombocytopenia
* Spinal hematoma
* Epidural intercranial hemorrhage
* Injection site reaction
* Osteoporosis/Ostropenia
* Thrombocytopenia
* Spinal hematoma
* Epidural intercranial hemorrhage
* Injection site reaction
* Osteoporosis/Ostropenia
61
New cards
Low Molecular Weight Heparin (LMWH) Contraindications
* Severe thrombocytopenia
* Active bleeding
* HIT
* Dialysis patients
* Active bleeding
* HIT
* Dialysis patients
62
New cards
Low Molecular Weight Heparin (LMWH) Counseling Points
CrCl < 30 ml/min, enoxaparin dose adjusted to 1 mg/kg sc daily
63
New cards
Low Molecular Weight Heparin (LMWH) Black Box Warning
Spinal or epidural hematomas
64
New cards
Low Molecular Weight Heparin (LMWH) Adminstration
* Wash & dry your hands thoroughly.
* Sit/lie in a comfortable position, so that you can see your stomach (or SQ site). Choose the area on the right or left side of your stomach, ≥ 2 inches from your belly button, where you will give yourself the shot. Do not use areas close to surgical sites or bandages. __**Be sure to change the site each day**__.
* Clean the chosen area to inject with an alcohol pad.
* Open the pack and remove the syringe. Pull the needle cap off.
* The syringe has a set dose of drug in it. __**Do not push**__ __**the air bubble out**__ from the syringe before you inject it.
* Hold the syringe, like a pencil, in your writing hand. With other hand, use your thumb & forefinger to pinch a fold of skin on the chosen area.
* Insert the entire needle straight (__**90 degrees**__) into the fold of your skin & slowly press the plunger down. Make sure the full dose of has been given.
* Pull the needle straight out, point it down & away from yourself & others, and push down on the plunger to activate needle shield.
* __**Throw away syringe in a “SHARPS” box**__
* Sit/lie in a comfortable position, so that you can see your stomach (or SQ site). Choose the area on the right or left side of your stomach, ≥ 2 inches from your belly button, where you will give yourself the shot. Do not use areas close to surgical sites or bandages. __**Be sure to change the site each day**__.
* Clean the chosen area to inject with an alcohol pad.
* Open the pack and remove the syringe. Pull the needle cap off.
* The syringe has a set dose of drug in it. __**Do not push**__ __**the air bubble out**__ from the syringe before you inject it.
* Hold the syringe, like a pencil, in your writing hand. With other hand, use your thumb & forefinger to pinch a fold of skin on the chosen area.
* Insert the entire needle straight (__**90 degrees**__) into the fold of your skin & slowly press the plunger down. Make sure the full dose of has been given.
* Pull the needle straight out, point it down & away from yourself & others, and push down on the plunger to activate needle shield.
* __**Throw away syringe in a “SHARPS” box**__
65
New cards
Enoxaparin Advantages
66
New cards
Enoxaparin Disadvantages
67
New cards
Unfractionated Heparin Advantages
68
New cards
Unfractionated Heparin Disadvantages
69
New cards
Fondaparinux MOA
Prevents thrombus generation and clot formation by indirectly inhibiting factor Xa activity
70
New cards
Fondaparinux Dosing - Weight Based
*
71
New cards
Fondaparinux Monitoring
* Complete blood count (Hgb, Hct, Ptts)
* Serum creatinine
* Serum creatinine
72
New cards
Fondaparinux Side Effects
* Bleeding
* Spinal hematoma
* Epidural intercranial hemorrhage
* Spinal hematoma
* Epidural intercranial hemorrhage
73
New cards
Fondaparinux Contraindications
* Severe renal impairment
* Body weight
* Body weight
74
New cards
Fondaparinux Black Box Warning
Spinal or epidural hematomas
75
New cards
Heparin Reversal: Protamine
* IV Protamine (cationic) + Heparin (anionic) → Stable salt that results in loss of anticoagulation activity
* Neutralizes in 5 minutes
* Neutralizes in 5 minutes
76
New cards
Protamine Heparin Reversal - Time Heparin Dose was Given
* Within 30- 60 minutes: 1 mg IV protamine for every 100 units of heparin (max = 50 mg)
* If > 60 minutes, need to decrease protamine dose
* May not be beneficial If heparin dose was given > 5-6 hours prior
* If > 60 minutes, need to decrease protamine dose
* May not be beneficial If heparin dose was given > 5-6 hours prior
77
New cards
Reversal of Parenteral Anticoagulant - Enoxaparin (Lovenox®)
Partial reversal with protamine, but degree unclear
* If dosed < 8 hours: 1 mg/ 1 mg enoxaparin
* If dosed >8 hours: 0.5 mg/1 mg enoxaparin
* If dosed < 8 hours: 1 mg/ 1 mg enoxaparin
* If dosed >8 hours: 0.5 mg/1 mg enoxaparin
78
New cards
Reversal of Parenteral Anticoagulant - Fondaparinux (Arixtra®)
* Activated prothrombin complex concentrate (aPCC or FEIBA®)
* Limited data to support its use
* Limited data to support its use
79
New cards
Thrombolytics Data
Many Trials have shown patients with the highest risk of dying from PE and lowest risk of bleed obtain the __**greatest**__ benefit from thrombolytics
80
New cards
Thrombolytics Data - Pulomary Embolism Thrombolysis Trial
* Randomized 1006 patents with PE and RV dysfunction
* Tenecteplase: 30 mg to 50 mg
* Heparin
* Tenecteplase: 30 mg to 50 mg
* Heparin
81
New cards
Pulomary Embolism Thrombolysis Trial - Primary Outcomes
* Efficacy: Composite of death from any cause or hemodynamic decompensation
* Safety: Major Bleed
* Safety: Major Bleed
82
New cards
Pulomary Embolism Thrombolysis Trial Results
__No convincing net benefit from thrombolytic therapy__
* Death or hemodynamic decompensation: 13 tenecteplase and 28 heparin (95% CI: 0.23 - 0.87)
* Major bleeding: 32 tenecteplase and 6 heparin (95% CI: 2.3-13.39)
* Death or hemodynamic decompensation: 13 tenecteplase and 28 heparin (95% CI: 0.23 - 0.87)
* Major bleeding: 32 tenecteplase and 6 heparin (95% CI: 2.3-13.39)
83
New cards
Absolute Contraindication to Thrombolytics
* Previous intracranial bleed
* Structural intracranial disease
* Ischemic stroke (last 3 months)
* Active internal bleed
* Recent brain or spinal surgery/trauma
* Recent head trauma
* Bleeding diathesis
* Structural intracranial disease
* Ischemic stroke (last 3 months)
* Active internal bleed
* Recent brain or spinal surgery/trauma
* Recent head trauma
* Bleeding diathesis
84
New cards
Relative Contraindication to Thrombolytics
* Severe HTN (>180/110)
* Recent bleeding (non-intracranial)
* Recent surgery/trauma
* Ischemic stroke (> 3 months)
* Current use of anticoagulation therapy
* Traumatic CPR
* Pericarditis
* Pregnancy
* Age > 75
* Low body weight < 60 kg
* Recent bleeding (non-intracranial)
* Recent surgery/trauma
* Ischemic stroke (> 3 months)
* Current use of anticoagulation therapy
* Traumatic CPR
* Pericarditis
* Pregnancy
* Age > 75
* Low body weight < 60 kg
85
New cards
FDA Approved Thrombolytics for Massive PE
* Alteplase (Activase®)
* Tenecteplase (TNK) (__**not FDA approved for PE**__)
* __Due to bleeding risk__
* Streptokinase (not available in the US)
* Urokinase (not available in the US)
* Tenecteplase (TNK) (__**not FDA approved for PE**__)
* __Due to bleeding risk__
* Streptokinase (not available in the US)
* Urokinase (not available in the US)
86
New cards
Alteplase (rt-PA) Total Dose
100 mg
87
New cards
Alteplase (rt-PA) PE Dosing
* 10 mg bolus
* Followed by 90 mg over 2 hours, administer through peripheral vein
* Followed by 90 mg over 2 hours, administer through peripheral vein
88
New cards
Alteplase (rt-PA) Adverse Events
* Bleeding complications
* Intracranial hemorrhage
* Intracranial hemorrhage
89
New cards
Key Concepts
* VTE are the LEADING CAUSE of PREVENTABLE death in the US
* Diagnostic Imaging is necessary to rule in or out a VTE event
* Thrombolytics are ONLY indicated in patients who are HYPOTENSIVE
* Parenteral anticoagulation is an appropriate therapy option in patients at risk of hemodynamic instability
* Anticoagulation is the mainstay of treatment and should be continues for at least 3 months
* Diagnostic Imaging is necessary to rule in or out a VTE event
* Thrombolytics are ONLY indicated in patients who are HYPOTENSIVE
* Parenteral anticoagulation is an appropriate therapy option in patients at risk of hemodynamic instability
* Anticoagulation is the mainstay of treatment and should be continues for at least 3 months
90
New cards
Heparin-Induced Thrombocytopenia (HIT)
Immune system causes your platelets to clot in the presence of heparin→ platelet levels dropping → Thrombosis
91
New cards
Heparin-Induced Thrombocytopenia (HIT) Types
* Type I: Heparin Associated Thrombocytopenia (HAT)
* Type II: Heparin-Induced Thrombocytopenia (HIT)
* Type II: Heparin-Induced Thrombocytopenia (HIT)
92
New cards
Heparin Associated Thrombocytopenia (HAT) - Immune Mediated
No
93
New cards
Heparin Associated Thrombocytopenia (HAT) - Onset
* Early
* < 4 days of therapy
* < 4 days of therapy
94
New cards
Heparin Associated Thrombocytopenia (HAT) - Platelet Count
>100 k
95
New cards
Heparin Associated Thrombocytopenia (HAT) - Severity
Transient, mild
96
New cards
Heparin Associated Thrombocytopenia (HAT) -Complications
None usually
97
New cards
Type II Heparin-Induced Thrombocytopenia (HIT) - Immune Mediated
Yes
98
New cards
Type II Heparin-Induced Thrombocytopenia (HIT) - Onset
5-10 days after start of therapy (Earlier if recent exposure)
99
New cards
Type II Heparin-Induced Thrombocytopenia (HIT) - Platelet Count
50% decrease from baseline
100
New cards
Type II Heparin-Induced Thrombocytopenia (HIT) -Severity
Severe