Chapter 20: Respiratory Management and Mechanical Ventilation
1/24
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
25 Terms
Chapter 20: Respiratory Management and Mechanical Ventilation
Oxygen Basics
Oxygen is a tasteless, colorless gas.
Makes up ~21% of atmospheric air.
Purpose of Oxygen Therapy
Maintains adequate cellular oxygenation.
Used to treat acute and chronic respiratory conditions.
Oxygen Administration Goals
Maintain SaO₂ between 95%–100%.
Use the lowest effective oxygen concentration.
Prevent oxygen-related complications (oxygen toxicity, CO₂ retention).
Mechanical Ventilation Overview
Required when a client cannot breathe spontaneously.
Provides respiratory support in the following situations:
Severe respiratory disease (impaired ventilation or gas exchange).
General anesthesia (suppressed respiratory drive).
Trauma (neurologic or thoracic impairment).
Other critical illnesses affecting breathing.
Key NCLEX Focus
Oxygen is a medication.
Always titrate oxygen to the lowest dose that achieves target saturation.
Mechanical ventilation replaces or supports spontaneous breathing, not just oxygen delivery.
Oxygen Delivery Devices
Supplemental oxygen is delivered based on the client’s condition and oxygenation needs.
Oxygen concentration is expressed as FiO₂ (fraction of inspired oxygen).
Continuously monitor vital signs and SaO₂.
Adjust therapy based on response and clinical status.

Nasal Cannula
Tubing with two small prongs inserted into the nares.
FiO₂ 24%–44% at 1–6 L/min.
Advantages
Safe, simple, comfortable, well tolerated.
Allows eating, talking, and ambulation.
Disadvantages
FiO₂ varies with flow rate and depth of breathing.
Prolonged use can cause skin breakdown and dry mucous membranes.
Easily dislodged.
Nursing Actions
Assess patency of nares.
Ensure proper prong fit.
Use water-soluble lubricant for dry nares.
Add humidification at ≥4 L/min.

Simple Face Mask
Covers nose and mouth.
FiO₂ 35%–60% at 5–10 L/min.
Minimum flow 5 L/min to flush CO₂.
Advantages
Easy to apply.
May be more comfortable than a nasal cannula.
Disadvantages
Flow <5 L/min causes CO₂ rebreathing.
Poor tolerance with anxiety or claustrophobia.
Interferes with eating, drinking, talking.
Aspiration risk with vomiting or decreased LOC.
Moisture and pressure can cause skin breakdown.
Nursing Actions
Ensure snug fit over nose and mouth.
Switch to nasal cannula during meals.
Partial Rebreather Mask
Covers nose and mouth.
FiO₂ 50%–90% at 10–15 L/min.
Advantages
Reservoir bag without valves allows rebreathing of up to one-third exhaled air.
Disadvantages
Reservoir bag deflation causes CO₂ buildup.
FiO₂ varies with breathing pattern.
Poor tolerance with anxiety or claustrophobia.
Interferes with eating and talking.
Aspiration risk.
Nursing Actions
Keep reservoir bag inflated.
Assess mask fit and skin integrity.
Monitor bridge of nose and mask edges.
Use nasal cannula during meals.
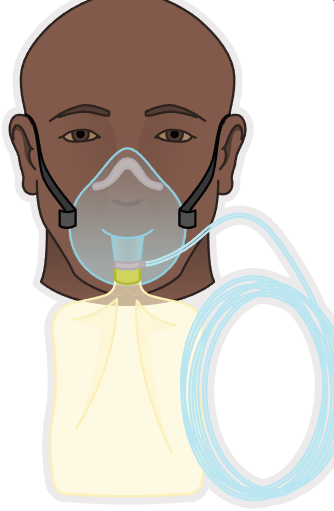
Nonrebreather Mask
Covers nose and mouth.
FiO₂ 80%–95% at 10–15 L/min.
Reservoir bag should remain two-thirds full.
Advantages
Highest oxygen concentration without intubation.
One-way valves prevent room air entry.
Disadvantages
Valves and flaps must function properly.
Poor tolerance with anxiety or claustrophobia.
Interferes with eating and talking.
Aspiration risk.
Nursing Actions
Check valves and flaps at least hourly.
Ensure proper seal.
Monitor skin integrity.
Use nasal cannula during meals.
Low-Flow Oxygen Delivery Systems
Nasal Cannula
Tubing with two small prongs inserted into the nares.
FiO₂ 24%–44% at 1–6 L/min.
Advantages
Safe, simple, comfortable, well tolerated.
Allows eating, talking, and ambulation.
Disadvantages
FiO₂ varies with flow rate and depth of breathing.
Prolonged use can cause skin breakdown and dry mucous membranes.
Easily dislodged.
Nursing Actions
Assess patency of nares.
Ensure proper prong fit.
Use water-soluble lubricant for dry nares.
Add humidification at ≥4 L/min.
Simple Face Mask
Covers nose and mouth.
FiO₂ 35%–60% at 5–10 L/min.
Minimum flow 5 L/min to flush CO₂.
Advantages
Easy to apply.
May be more comfortable than a nasal cannula.
Disadvantages
Flow <5 L/min causes CO₂ rebreathing.
Poor tolerance with anxiety or claustrophobia.
Interferes with eating, drinking, talking.
Aspiration risk with vomiting or decreased LOC.
Moisture and pressure can cause skin breakdown.
Nursing Actions
Ensure snug fit over nose and mouth.
Switch to nasal cannula during meals.
Partial Rebreather Mask
Covers nose and mouth.
FiO₂ 50%–90% at 10–15 L/min.
Advantages
Reservoir bag without valves allows rebreathing of up to one-third exhaled air.
Disadvantages
Reservoir bag deflation causes CO₂ buildup.
FiO₂ varies with breathing pattern.
Poor tolerance with anxiety or claustrophobia.
Interferes with eating and talking.
Aspiration risk.
Nursing Actions
Keep reservoir bag inflated.
Assess mask fit and skin integrity.
Monitor bridge of nose and mask edges.
Use nasal cannula during meals.
Nonrebreather Mask
Covers nose and mouth.
FiO₂ 80%–95% at 10–15 L/min.
Reservoir bag should remain two-thirds full.
Advantages
Highest oxygen concentration without intubation.
One-way valves prevent room air entry.
Disadvantages
Valves and flaps must function properly.
Poor tolerance with anxiety or claustrophobia.
Interferes with eating and talking.
Aspiration risk.
Nursing Actions
Check valves and flaps at least hourly.
Ensure proper seal.
Monitor skin integrity.
Use nasal cannula during meals.

Venturi Mask
Covers nose and mouth.
FiO₂ 24%–60% at 10–15 L/min using color-coded adapters.
Advantages
Most precise oxygen concentration without intubation.
No humidification required.
Ideal for chronic lung disease (controlled oxygen delivery).
Disadvantages
More expensive.
Nursing Actions
Verify correct adapter and flow rate.
Ensure tubing is free of kinks.
Monitor skin around mask and nares.
Use nasal cannula during meals.

Aerosol Mask, Face Tent, Tracheostomy Collar
Loose-fitting devices for face or tracheostomy.
FiO₂ 24%–100% at ≥10 L/min.
Provide high humidification.
Advantages
Useful when masks are not tolerated.
Ideal for facial trauma, burns, thick secretions.
Disadvantages
Requires frequent monitoring due to high humidity.
Nursing Actions
Empty condensation from tubing frequently.
Ensure adequate water in humidifier.
Verify visible mist during inspiration and expiration.
Prevent tubing from pulling on tracheostomy.
T-Piece
Used with tracheostomy, laryngectomy, or ET tube.
FiO₂ 24%–100% at ≥10 L/min.
Advantages
Delivers humidified oxygen directly to artificial airway.
Disadvantages
High humidification requires frequent monitoring.
Nursing Actions
Keep exhalation port open.
Prevent traction on tracheostomy or ET tube
Ensure visible mist during inspiration and expiration.
High-Flow Oxygen Delivery Systems
Deliver precise FiO₂ when properly fitted.
Venturi Mask
Covers nose and mouth.
FiO₂ 24%–60% at 10–15 L/min using color-coded adapters.
Advantages
Most precise oxygen concentration without intubation.
No humidification required.
Ideal for chronic lung disease (controlled oxygen delivery).
Disadvantages
More expensive.
Nursing Actions
Verify correct adapter and flow rate.
Ensure tubing is free of kinks.
Monitor skin around mask and nares.
Use nasal cannula during meals.
Aerosol Mask, Face Tent, Tracheostomy Collar
Loose-fitting devices for face or tracheostomy.
FiO₂ 24%–100% at ≥10 L/min.
Provide high humidification.
Advantages
Useful when masks are not tolerated.
Ideal for facial trauma, burns, thick secretions.
Disadvantages
Requires frequent monitoring due to high humidity.
Nursing Actions
Empty condensation from tubing frequently.
Ensure adequate water in humidifier.
Verify visible mist during inspiration and expiration.
Prevent tubing from pulling on tracheostomy.
T-Piece
Used with tracheostomy, laryngectomy, or ET tube.
FiO₂ 24%–100% at ≥10 L/min.
Advantages
Delivers humidified oxygen directly to artificial airway.
Disadvantages
High humidification requires frequent monitoring.
Nursing Actions
Keep exhalation port open.
Prevent traction on tracheostomy or ET tube
Ensure visible mist during inspiration and expiration.
A nurse is caring for a client who has dyspnea and will receive oxygen continuously. Which of the following oxygen devices should the nurse use to deliver a precise amount of oxygen to the client?
a
Non-rebreather mask
b
Nasal cannula
c
Venturi mask
d
Tracheostomy collar
c
Venturi mask
NCLEX Focus
Low-flow systems deliver variable FiO₂.
High-flow systems deliver precise FiO₂.
Nonrebreather masks are for short-term, high-acuity oxygen needs.
Humidification is essential with high flows or artificial airways.
Oxygen Therapy
Indications
Treatment of hypoxemia and hypoxia.
Potential Diagnoses
Hypoxemia
Inadequate oxygen level in the blood.
Caused by hypovolemia, hypoventilation, or impaired arterial blood flow.
Hypoxia
Decreased tissue oxygenation.
Client Presentation
Early Findings
Tachypnea
Tachycardia
Restlessness
Pale skin and mucous membranes
Elevated blood pressure
Signs of respiratory distress:
Use of accessory muscles
Nasal flaring
Tracheal tugging
Adventitious lung sounds
Late Findings
Confusion or stupor
Cyanotic skin and mucous membranes
Bradypnea
Bradycardia
Hypotension
Cardiac dysrhythmias
Oxygen Therapy Considerations
Preparation of the Client
Explain procedures to reduce anxiety.
Position in semi-Fowler’s or Fowler’s (improves chest expansion).
Verify oxygen equipment is functioning properly.
Ongoing Care
Administer oxygen at the lowest flow rate that corrects hypoxemia.
Monitor:
Respiratory rate, rhythm, effort
Lung sounds
SaO₂
Assess for:
Hypoxemia: dyspnea, anxiety, tachypnea, tachycardia, restlessness, pallor or cyanosis, adventitious sounds, confusion.
Hypercarbia (↑ CO₂): restlessness, hypertension, headache.
Review diagnostics related to oxygenation (ABGs).
Promote oral hygiene.
Encourage turning, coughing, deep breathing, incentive spirometry, suctioning as needed.
Promote rest and reduce environmental stimuli.
Provide emotional support for anxiety.
Assess nutritional status and provide supplements as prescribed.
Monitor skin integrity and use pressure-relief or moisture-barrier measures.
Document response to oxygen therapy.
Titrate oxygen to prescribed saturation goals.
Discontinue supplemental oxygen gradually.
Interventions
Respiratory Depression
Monitor for decreased respiratory rate and decreased level of consciousness.
Notify the provider if present.
Respiratory Distress
Position in Fowler’s or semi-Fowler’s.
Perform focused respiratory assessment.
Encourage deep breathing.
Administer supplemental oxygen as prescribed.
Stay with the client to reduce anxiety.
Promote airway clearance (coughing, oral or oropharyngeal suctioning).
Oxygen Therapy Complications
Oxygen Toxicity
Risk factors:
FiO₂ >50%
Prolonged therapy (>24–48 hours)
Underlying lung disease
Manifestations:
Nonproductive cough
Substernal chest pain
Nasal stuffiness
Nausea and vomiting
Fatigue
Headache
Sore throat
Hypoventilation
Nursing Actions
Use the lowest FiO₂ needed to maintain prescribed SaO₂.
Monitor ABGs and notify provider of abnormal results.
Use CPAP or BiPAP if prescribed to reduce oxygen requirement.
Use PEEP during mechanical ventilation as prescribed.
Oxygen-Induced Hypoventilation
Occurs in COPD clients with chronic hypoxemia and hypercarbia.
Nursing Actions
Monitor respiratory rate, pattern, LOC, and SaO₂.
Use the lowest effective oxygen flow rate.
Prefer Venturi mask for precise FiO₂ if tolerated.
Notify provider for signs of respiratory depression.
Combustion Risk
Oxygen supports combustion.
Nursing Actions
Post “No Smoking” or “Oxygen in Use” signs.
Know location of fire extinguisher.
Educate client and visitors about fire hazards.
Use cotton gowns (reduce static electricity).
Ensure electrical devices are functioning properly.
Ensure equipment is grounded.
Avoid flammable products near oxygen (alcohol, acetone).
Noninvasive Positive Pressure Ventilation
Continuous Positive Airway Pressure (CPAP)
Provides continuous positive pressure via a leak-proof mask.
Keeps airways open throughout the respiratory cycle.
Improves alveolar gas exchange.
First-line therapy for sleep apnea.
Bi-Level Positive Airway Pressure (BiPAP)
Provides:
Higher inspiratory pressure
Lower expiratory pressure
Requires a leak-proof mask.
Commonly used in COPD requiring ventilatory assistance.
Nursing Actions
Assess skin around mask for breakdown.
Verify oxygen concentration and pressure settings.
Transtracheal Oxygen Therapy
Delivers oxygen directly into the lungs via a small catheter inserted into the trachea.
Less visible than nasal cannula.
Reduces irritation from nasal prongs.
Endotracheal Tube and Endotracheal Intubation
Tube inserted through the mouth or nose into the trachea for emergency airway management.
Oral intubation
Fastest and easiest method.
Common in emergency settings.
Nasal intubation
Used with facial or oral trauma.
Contraindicated with clotting disorders.
Placement
Performed by:
Nurse anesthetist
Anesthesiologist
Critical care or emergency physician
Pulmonologist
Placement confirmation:
Chest x-ray (gold standard).
ET tubes may be cuffed or uncuffed.
Inflated cuff forms a seal against the tracheal wall.
Prevents air leakage.
Ensures adequate tidal volume delivery.
Client cannot speak when cuff is inflated.
Nursing Actions
Keep manual resuscitation bag with face mask at bedside at all times.
Limit intubation attempts to ≤30 seconds.
Reoxygenate between attempts.
Verify placement:
End-tidal CO₂
Chest x-ray
Auscultate bilateral breath sounds.
Observe for symmetrical chest rise.
Secure tube with holder or tape.
Monitor for hypoxemia, dysrhythmias, aspiration.
Mechanical Ventilation
Provides breathing support until lung function improves.
Delivers warmed, humidified oxygen.
FiO₂ range 21%–100%.
Positive-pressure ventilation keeps alveoli open and prevents collapse.
Benefits
Forced lung expansion.
Improved oxygenation.
Decreased work of breathing.
Routes
Endotracheal tube.
Tracheostomy tube.
Ventilator Cycling
Pressure
Volume
Time
Flow
Indications
Maintain patent airway and SaO₂ ≥95%.
Potential Diagnoses
Hypoxemia
Hypoventilation with respiratory acidosis
Airway trauma
COPD exacerbation
Acute pulmonary edema (MI or heart failure)
Asthma attack
Head injury, stroke, coma
Neuromuscular disorders (MS, myasthenia gravis, Guillain-Barré)
Obstructive sleep apnea
Postoperative respiratory support
General anesthesia or heavy sedation
Mechanical Ventilation Considerations
Preparation of the Client
Explain the procedure.
Establish communication method:
Yes/no questions
Writing tools
Communication board
Lip reading
Ongoing Care
Airway Management
Assess tube position and placement.
Keep tubing free of condensation.
Document tube depth at teeth or lips.
Use two staff members to reposition tube.
Use caution when moving the client.
Ventilation and Assessment
Suction oral and tracheal secretions as needed.
Support ventilator tubing to prevent erosion or displacement.
Assess respiratory status every 1–2 hr:
Breath sounds
Symmetry
Respiratory effort
Verify ventilator settings each shift and hourly:
Rate
FiO₂
Tidal volume
Mode
PEEP or CPAP
PIP or plateau pressure
Alarm limits
Ventilator Alarms
Never turn off alarms.
Volume (low pressure):
Disconnection
Cuff leak
Tube displacement
Pressure (high pressure):
Secretions
Kinked tubing
Biting tube
Coughing
Pulmonary edema
Bronchospasm
Pneumothorax
Apnea:
No spontaneous breaths detected.
Cuff Management
Maintain minimal occlusive pressure.
Check cuff pressure at least every 8 hr.
Target <20 mm Hg or 20–30 cm H₂O.
Signs of cuff leak:
Air hissing
Client vocalizing
Decreasing SaO₂
Medications
Analgesics: morphine, fentanyl.
Sedatives: propofol, diazepam, lorazepam, midazolam, haloperidol.
Neuromuscular blockers:
Pancuronium
Atracurium
Vecuronium
Require sedation and analgesia.
Ulcer prevention: famotidine, lansoprazole.
Antibiotics as indicated.
Skin and Oral Care
Reposition ET tube every 24 hr or per protocol.
Provide oral care at least every 12 hr.
Older adults require frequent gentle skin care.
Nutrition
Assess GI function every 8 hr.
Monitor bowel habits.
Administer enteral or parenteral nutrition as prescribed.
Weaning Monitoring
RR >30 or <8/min.
HR or BP change >20% from baseline.
SaO₂ <90%.
Dysrhythmias or ST elevation.
Decreased tidal volume.
Increased work of breathing.
Diaphoresis.
Anxiety or decreased LOC.
Extubation Care
Keep bag-mask and oxygen at bedside.
Keep reintubation equipment available.
Suction oropharynx and trachea.
Deflate cuff and remove tube during peak inspiration.
Monitor closely for airway obstruction:
Stridor
Dyspnea
Ineffective cough
Monitor SpO₂ and vital signs every 5 min initially.
Encourage coughing, deep breathing, incentive spirometry.
Reposition frequently to mobilize secretions.
Older adults need more frequent repositioning.
Mechanical Ventilation Complications
Trauma
Barotrauma: pneumothorax, subcutaneous emphysema, pneumomediastinum.
Volutrauma: lung damage from excessive volume.
Fluid Retention
Caused by decreased cardiac output and RAAS activation.
Monitor intake/output, weight, breath sounds, secretions.
Oxygen Toxicity
Risk with FiO₂ >50% or prolonged therapy.
Monitor for:
Fatigue
Restlessness
Severe dyspnea
Tachycardia
Tachypnea
Crackles
Cyanosis
Hemodynamic Compromise
Increased intrathoracic pressure reduces venous return.
Monitor for:
Hypotension
Tachycardia
Urine output ≤30 mL/hr
Cool, clammy skin
Decreased LOC
Aspiration
Keep HOB ≥30° at all times.
Check enteral feeding residuals every 4 hr.
Gastrointestinal Ulceration (Stress Ulcer)
Monitor drainage and stool for occult blood.
Administer ulcer prophylaxis.
Infection
Related to intubation or suctioning.
Monitor for:
Fever
Sputum changes
Crackles or rhonchi
Elevated WBCs
Use strict aseptic technique during suctioning.
NCLEX Focus
Always confirm ET tube placement.
Alarms signal problems first, patient assessment comes first.
Bag the patient first if ventilator failure occurs.
Sedation does not equal pain control.
Keep HOB elevated to prevent aspiration.
Modes of Ventilation
Assist-Control Ventilation (AC)
Preset respiratory rate and tidal volume.
Client initiates a breath, ventilator delivers full preset breath.
Ventilator can fully control ventilation in intubated clients.
Risk of hyperventilation and respiratory alkalosis.
Sedation may be required to reduce respiratory rate.
Synchronized Intermittent Mandatory Ventilation (SIMV)
Preset respiratory rate and tidal volume for mandatory breaths.
Client can initiate spontaneous breaths with variable tidal volume.
Mandatory breaths are synchronized with client effort.
Used as a primary mode or as a weaning mode.
Allows more spontaneous ventilation than AC.
Can increase work of breathing and cause respiratory muscle fatigue.
Inverse Ratio Ventilation (IRV)
Prolongs inspiratory time to improve oxygenation.
Used for severe hypoxemia refractory to PEEP.
Often requires deep sedation or neuromuscular blockade.
Risks include volutrauma and decreased cardiac output due to air trapping.
Airway Pressure Release Ventilation (APRV)
Allows spontaneous breathing throughout the ventilatory cycle.
Time-triggered and pressure-limited.
Uses brief releases in pressure to allow exhalation.
May reduce ventilator-induced lung injury.
Fewer adverse cardiovascular effects compared with other modes.
Independent Lung Ventilation (ILV)
Uses double-lumen endotracheal tube.
Allows each lung to be ventilated separately.
Indicated for unilateral lung disease.
Requires two ventilators.
Requires sedation and often neuromuscular blockade.
High-Frequency Ventilation
Delivers very small tidal volumes at rapid rates (up to 3,000 cycles/min).
Commonly used in pediatric or neonatal clients.
Requires sedation and or neuromuscular blockade.
Breath sounds are difficult to assess.
Adjunctive Therapies
Positive End-Expiratory Pressure (PEEP)
Preset pressure applied at end of expiration.
Added to ventilator settings to treat persistent hypoxemia.
Keeps alveoli open and prevents collapse.
Improves oxygenation by enhancing gas exchange.
Typical range: 5–15 cm H₂O.
Weaning Modalities
Pressure Support Ventilation (PSV)
Provides positive pressure during inspiration.
Prevents alveolar collapse during expiration.
Decreases work of breathing.
Allows lower FiO₂ requirements.
Can be used alone or with SIMV or AC.
Typical setting: 5–20 cm H₂O.
Pressures >20 cm H₂O increase risk of lung injury.
Continuous Positive Airway Pressure (CPAP)
Delivers constant positive pressure during spontaneous breathing.
Client breathes independently without set ventilator breaths.
Often used with SIMV during weaning.
Risks include volutrauma, decreased cardiac output, and increased intracranial pressure.
NCLEX Focus
AC provides full ventilatory support.
SIMV and PSV are common weaning modes.
PEEP improves oxygenation but can reduce cardiac output.
High pressures increase risk of barotrauma and hypotension.
Always correlate ventilator mode with patient work of breathing and hemodynamic status.