HLA Polymorphism and Allograft Rejection
1/27
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No study sessions yet.
28 Terms
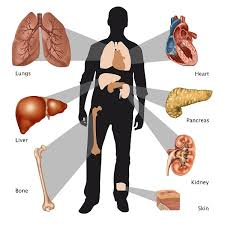
Define transplantation
Transfer of cells, tissues or organs between two individuals
Define rejection
Failure of graft (transplanted organ) to survive in recipient

Define histocompatibility and tissue typing.
Histocompatibility- Having the same/similar MHC/HLA alleles
Tissue typing- Establishing MCH/HLA type
What are the four types of graft?
Autologous (autograft): within individual (e.g. skin graft)
Syngeneic (isograft): between genetically identical individuals (e.g. twins)
Allogeneic (allograft): between genetically different individuals of the same species
Xenogeneic (xenograft): between two individuals from different species (e.g. pig heart, bovine heart valve)
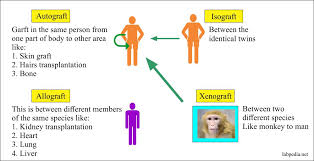
What is the most common type of graft?
allogeneic (allograft)
Rejection occurs with which type of graft?
allogeneic (allograft)
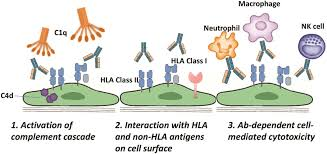
What causes rejection?
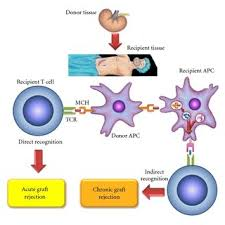
Adaptive immune response to allogeneic differences in MHC/HLA molecules between donor and recipient.
Also minor histocompatibility antigens (MnAgs/non-MHC)
What are differences in MHC/HLA molecules due to?
genetic polymorphism in the MHC (HLA in humans)
Rejection shows the same kinetics as adaptive immunity:
First-set rejection (slow initial response)
Second-set rejection (rapid secondary response to second transplant from the same donor/immunological memory response)
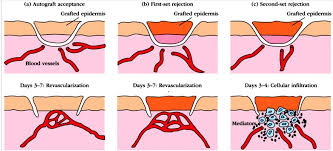
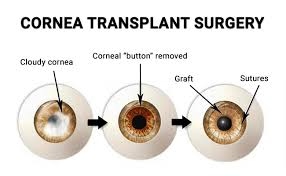
Why are corneal transplants generally successful?
Low rejection
Eye is “immune privileged” site
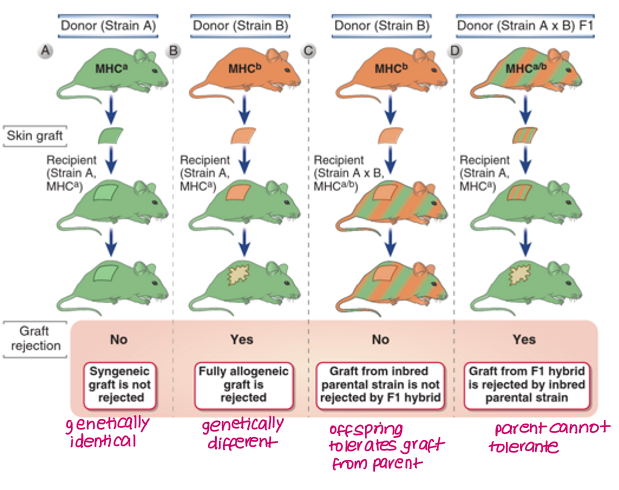
What did Bencerraf, Dausset and Snell observe with regards to transplantation between parent and offspring strains?
F1 offspring from parents A and B differing in MHC will not reject graft due to codominant expression of parental genes
Either parent will reject graft from F1 offspring
Siblings share 25%, parents cannot tolerate graft because of other parent’s MHC
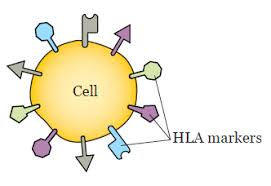
What are alloantigens and which ones are the most significant?
Alloantigens are donor antigens expressed on graft tissue that are not found in the recipients. When an antigen is present in some members of the same species but is not common to all members of that species, it is called an alloantigen.
Recognised by alloreactive B/T cells.
Most significant alloantigen is MHC encoded molecules.
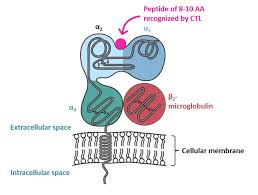
Polymorphic differences in MHC-encoded molecules are greatest in which part of the molecule?
peptide-binding site
How does rejection occur in allografts and which type of immune response does it involve?
Adaptive immune response
Alloreactive T/B cells recognise alloantigens on graft
Alloreactive T cells drive the immune response which may lead to rejection
Rejection in patients is clinically managed by?
anti-rejection drugs (immunosuppressants)
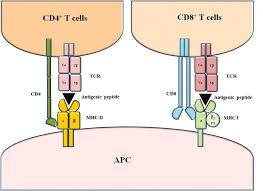
What are the structural differences between MHC Class I and II molecules?
Class I
αβ heterodimer (1 α chain, 1 β2-microglobulin)
α chain MHC encoded
1 transmembrane segment
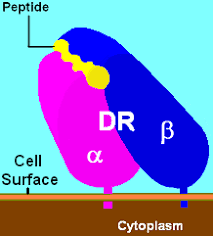
Class II
αβ heterodimer (1 α chain, 1 β chain)
both α and β chains MHC encoded (forms peptide binding site)
2 transmembrane segments

What are the functional differences between MHC Class I and II molecules?
Class I
present ENDOgenous Ag peptide (e.g. viruses) to CD8+ T cells
Class II
present EXOgenous Ag peptide (e.g. bacteria) to CD4+ T cells
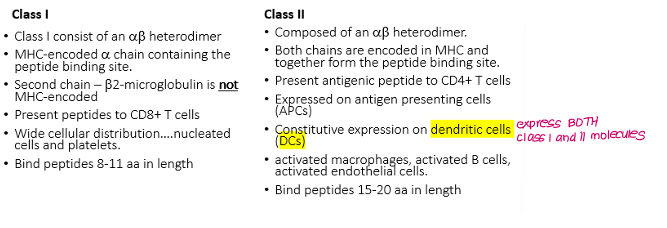
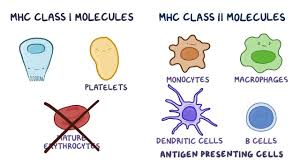
MHC Class I molecules are found on which type of cells?
All nucleated cells and platelets
MHC Class II molecules are found on which type of cells?
dendritic cells
APCs
Activated macrophages, B cells, endothelial cells
Ag peptide presented on the MHC molecule recognises and binds to?
T cell receptor (TCR)
Which chromosome is the HLA gene cluster located on?
Chromosome 6
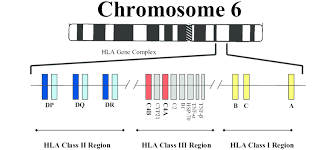
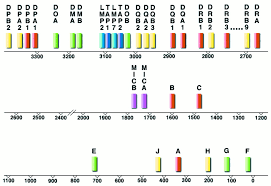
HLA Class I molecules are encoded at how many loci? What are they called?
3 loci
HLA-A
HLA-B
HLA-C

HLA Class II molecules are encoded at how many loci? What are they called?
3 loci in D region
HLA-DP (a1, a2, b1, b2)
HLA-DQ (a1, a2, b1, b2)
HLA-DR (DRa, DRb)
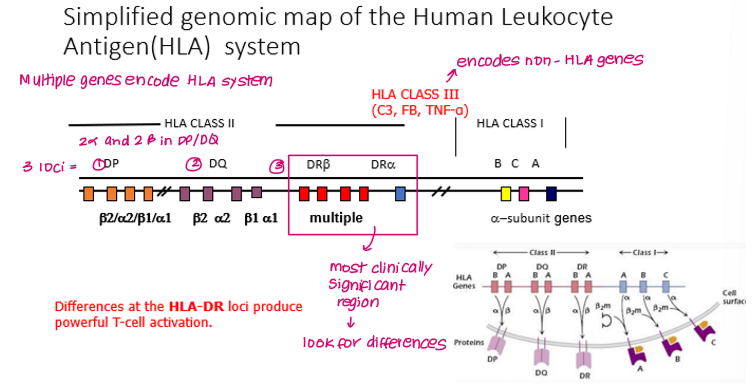
Parental HLA alleles are co-dominantly expressed. If two alleles are expressed at each locus, how many HLA encoding alleles are there in total?
12
Which region in the HLA genomic system is the most clinically significant and gives rise to the polymorphism observed?
DR region
What are HLA Class III molecules?
Complement proteins (e.g. C3)
Fibrinogen
Cytokines
Which laboratory methods are used to identify HLA variation in genes?
Molecular typing methods (no longer using serology) used to minimise mismatches between donor and recipient
Which HLA antigen is common in all populations?
HLA-A2