Social Determinants of Health
1/24
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
25 Terms
Beyond Healthcare in the U.S.
Historically, the U.S. looked to healthcare systems as the main driver of health and health outcomes
Over time, we've realized that achieving health equity requires looking broader – "outside the box"
Despite significant spending, U.S. outcomes are among the lowest for developed countries, including significant inequities22
What is “Health Equity?”
Everyone has a fair and just opportunity to be as healthy as possible.
Equality vs Equity
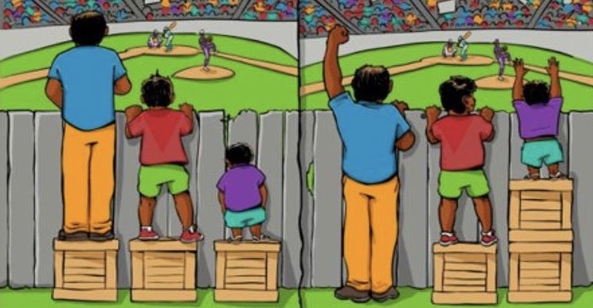
Health Equity
Achieved by addressing the underlying issues that prevent people from being healthy.
Benefits everyone
A healthy nation improves
Economic growth
Healthier environment
National security
Requires
Cross-sector collaborations
Policies and regulations
Community interventions
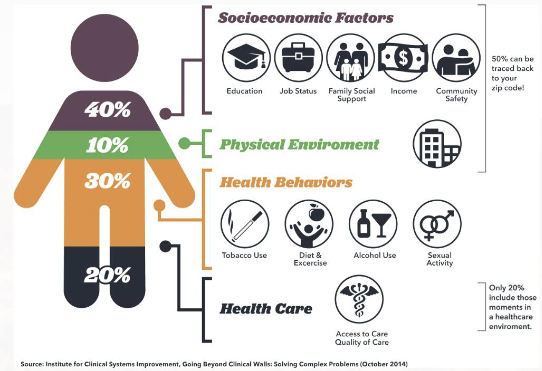
What determines our health?
“The complex interactions between biological and social elements and their influence on health”
(Raingruber, 2017, p. 98)Medical Factors
Biologic
Age
Gender
Infection
Genetic
Family
Origins
Race
Genetic predisposition
Non-medical factors
Behaviors, lifestyle
Education
Employment
Reliable transportation
Public safety
Language and literacy
Culture
What are the Social Determinants of Health?
The conditions and environment where people are born, live, learn, work, worship, and age.

Social Needs
Individual-level nonmedical acute resource needs related to SDOH
Housing
Reliable transportation
Strong support system
Person-centered
Varies from person-to-person
SDOH Factors
The 5 factors (SDOH) affect:
Overall health and well-being
Quality of life outcomes
Health risks
And are influenced by
Distribution of money, power, and resources
Policies at national, state, and local levels
Identify and explain health inequalities
Unfair and avoidable differences in health status seen within and between populations
Only promoting healthy choices won’t eliminate health disparities
We need to take action to improve the conditions in people’s environments
Social Determinants of Health
Education Access and Quality
Health Care Access and Quality
Neighborhood and Built Environment
Social and Community Context
Economic Stability
SDOH: Economic Stability
Employment
Jobs, employment, workplace conditions
Food insecurity
Limited or uncertain access to quality food
Housing instability
Ability to remain housed
Poverty
2025 federal poverty levels
Individual: $15,650 annual income
Family of 4: $32,150
Examples of Economic Stability Health Outcomes
Higher income associated with lower likelihood of disease and premature death
Lower income associated with higher rates of disease (including heart disease, stroke, diabetes, liver disease, and arthritis) and higher rates of preventable disease
Poverty may increase the onset of mental illness, intensify the experience, or prevent people from accessing proper treatment
<$35,000 annual income: 6.4% report feelings of sadness, 3.8% feelings of worthlessness
$75,000-99,999 annual income: 1.3% report feelings of sadness, 0.6% feelings of worthlessness
Health and socio-economic disadvantages accumulate over a lifetime and can persist across generations
SDOH: Education Access and Quality
Early childhood development and education
Enrollment in higher education
High school graduation
Language and literacy
Examples of Education Access and Quality Health Outcomes
High school graduation
Students who graduate from high school on time are more likely to pursue postsecondary education or skills training
Earn higher wages, generally healthier than those who do not graduate on time
Language and literacy
Limited literacy is a barrier to accessing health care services and understanding health information
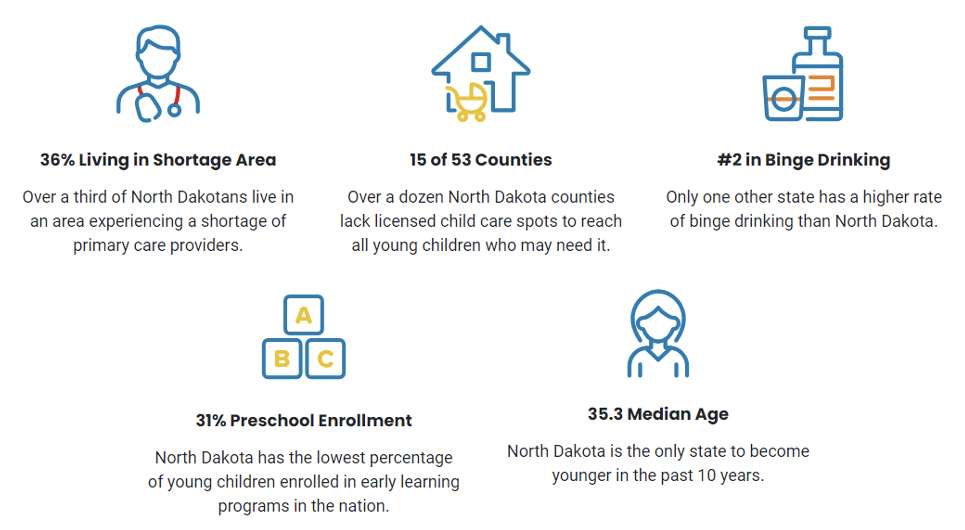
SDOH: Health Care Access & Quality
Access to services
Health insurance, costs, dept, quality
Access to primary care
Early detection and treatment of disease
Health literacy
Ability to use information to inform health-related decisions
Examples of Access to Health Care Outcomes
Access to primary care prevents illness and death and is associated with positive health outcomes
Factors: health insurance coverage, limited availability of health care providers -> leading to limited access to services
Those without health insurance less likely to receive preventative care, and care for major health conditions and chronic disease
Uninsured people often delay or forgo care because of its cost and are less likely to have a usual source of care which can lead to serious illness
In the U.S., racial and ethnic disparity in insurance coverage
SDOH: Neighborhood & Built Environment
Access to foods that support healthy dietary patterns
Quality and quantity of foods
Crime and violence
Environmental conditions
Playgrounds, walking paths
Water and air quality, natural disasters
Quality of housing
Examples of Neighborhood & Built Environment Health Outcomes
Housing and Instability and Homelessness
People need stable housing to be healthy
Food Insecurity
Food deserts
Environment & climate change
Health hazards
More likely to exist in low-income communities
Natural disasters
Low-income residents have less capacity to move when risks become evident and during forced evacuation or displacement
SDOH: Social and Community Context
Civic participation
Voting, volunteering, community activities
Discrimination
Unfair or unjustified harm to individuals and groups
Incarceration
Social cohesion
Relationships, support networks
Rurality
Geographic barriers to high-quality health care
~20% of Americans live in rural areas
39.3% in North Dakota
28.9% in Minnesota
Injury and death:
Higher death rates across 5 leading causes of death in U.S.
Higher death rates in unintentional injuries
Health care and insurance
Uninsured rural residents face greater difficulty in accessing care
Limited supply of rural health care workers who can provide low-cost or charitable health care
Transportation and internet access
Increased travel time, costs, and time away from work to access care
More likely to travel long distances for care
May lack reliable transportation (like public transit options)
Telehealth: helping to mitigate transportation challenges
Requires broadband internet services (~33% of rural areas lack access to highspeed internet)
Vulnerability
As a result of health inequities, some people are more vulnerable than others
More susceptible to effects of risk factors
More likely to develop health problems when exposed to risk factors
More likely to have poor health outcomes
Cumulative Effects
The cumulative effects of multiple risks make it more difficult to be resilient in the face of stressors
Example: People who don't have access to grocery stores with healthy foods
Less likely to have good nutrition —> Raises risk of health conditions like heart disease, diabetes, and obesity —> Lower life expectancy relative to people who do have access to healthy foods
Upstream Thinking
All nurses have the opportunity to work upstream though advocacy for policy changes
Most nurses in midstream and downstream
Castrucci and Auerbach (2019)
Upstream – SDOH factors that affect communities in a broad, inequitable way
Midstream – social needs, individual needs that might affect a person’s health
Downstream – disease treatment and chronic disease management
Nurses primarily work mid & downstream
Individual-level interventions
To fully comprehend health on an individual level, must understand interrelationships across all levels
SDOH in North Dakota
Role of Nursing in SDOH
Ask the right questions
Understand the relationship between upstream and midstream on downstream care services
Collaborate
Advocate
Summary
SDOH affect everyone
Disproportionately affected
Higher burden of poor health among lower socioeconomic status, rural populations, communities of color (compared to high socioeconomic status, urban populations, and white)
Inequities are unnecessary, unjust, and avoidable
Positive and negative aspects that support or challenge health status
A pattern of social risk factors (negative SDOH) contributes to increased morbidity and mortality
Improving population health = improving health for everyone