Concentration and Dilution of Urine
1/11
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
12 Terms
What is Water Balance?
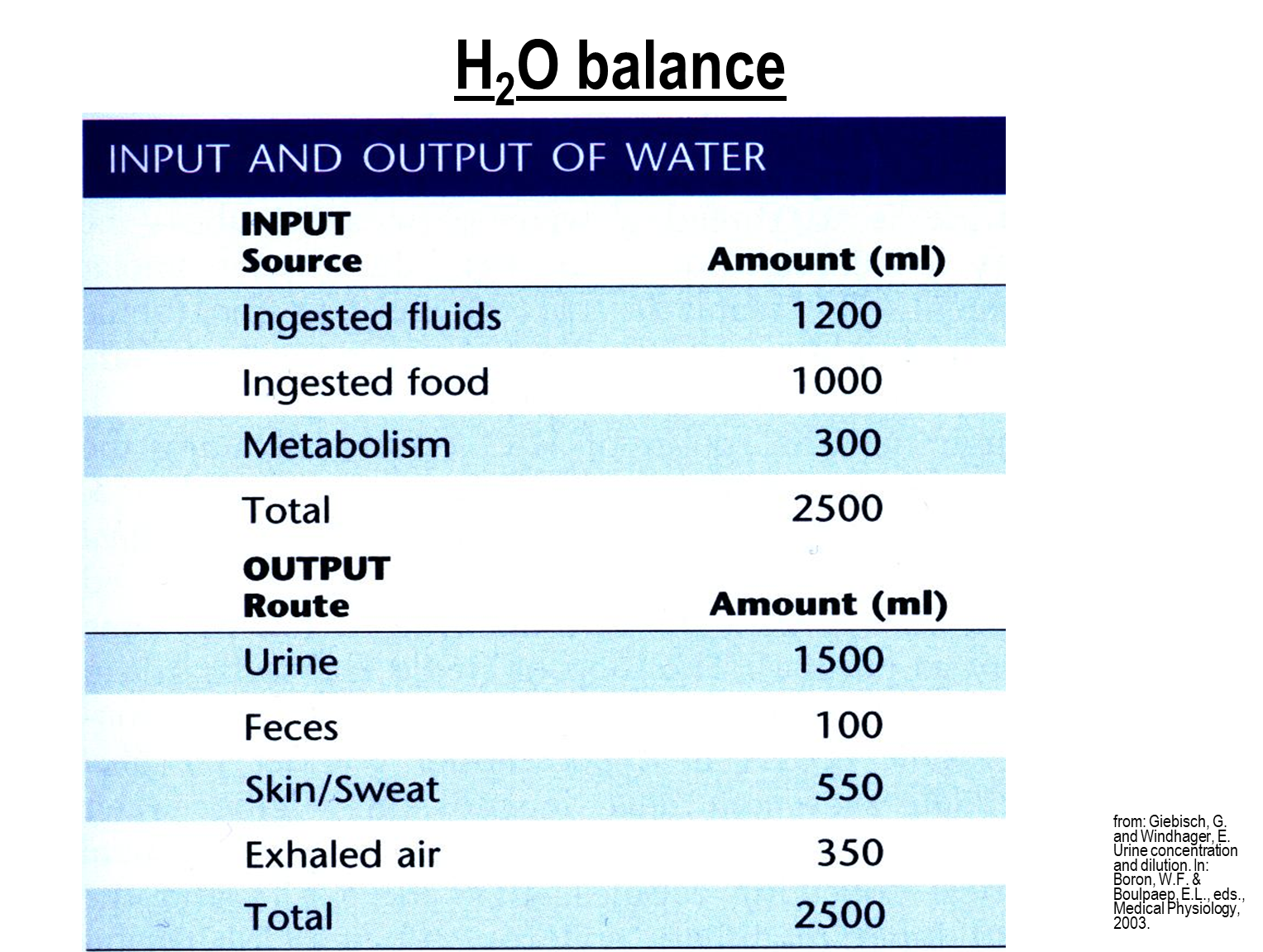
Water balance is the equilibrium between water intake and water loss in the body
1) The majority of water taken in is from ingestion of fluids and ingestion of fluids and a small amount of metabolism
2) The main output is from urine with a small amount in feces, sweat, and exhaled air
the balance is around 2500 ml in both pathways
How do the Kidneys generate a dilute urine?
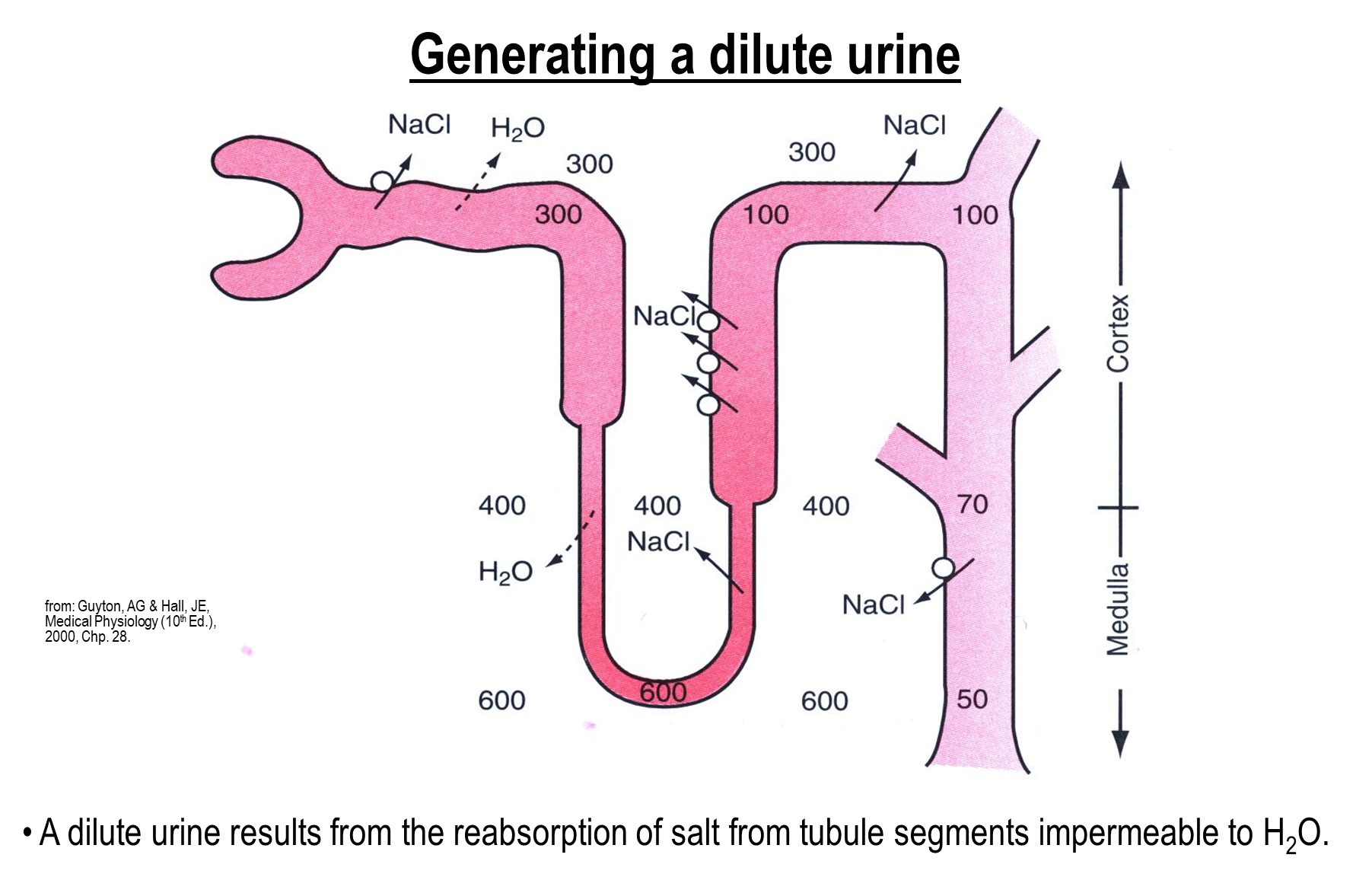
the ability of the nephron to create dilute urine comes from salt reabsorption from tubule segments that are impermeable to water
1) This occurs at the ascending limb which actively reabsorbs solutes while being impermeable to water
→ this will create a hypoosmotic tubule fluid at the end of the ascending limb
→ sodium will then be actively reabsorbed at the distal convoluted tubules which will create a further hypoosmotic tubule fluid
How does the kidney generate a concentrated urine
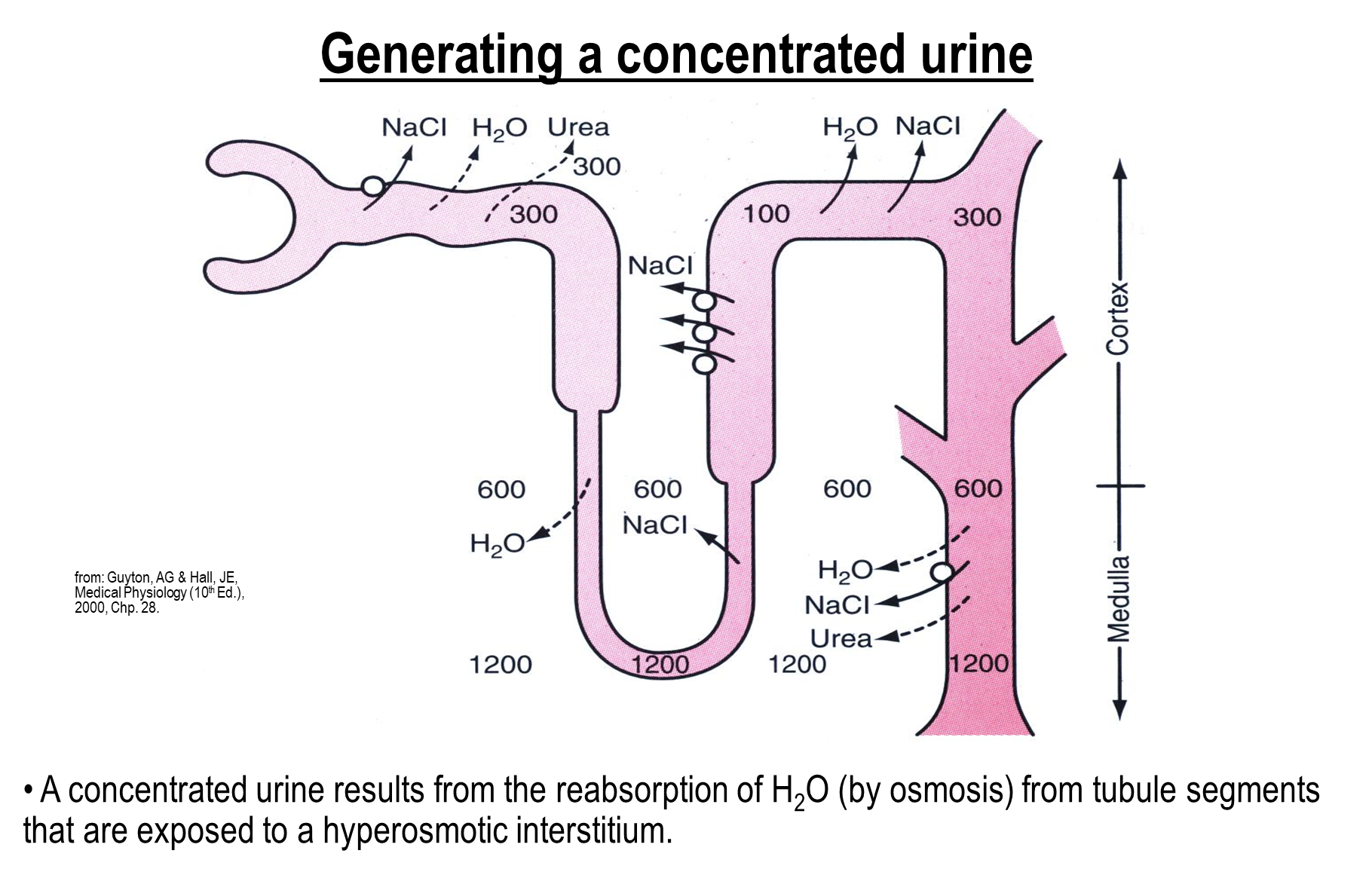
The ability to concentrate urine is dependent on permeability of water at the distal nephron as well as a hyperosmotic medullary interstitium
What is the effect of Anti diuretic hormone?
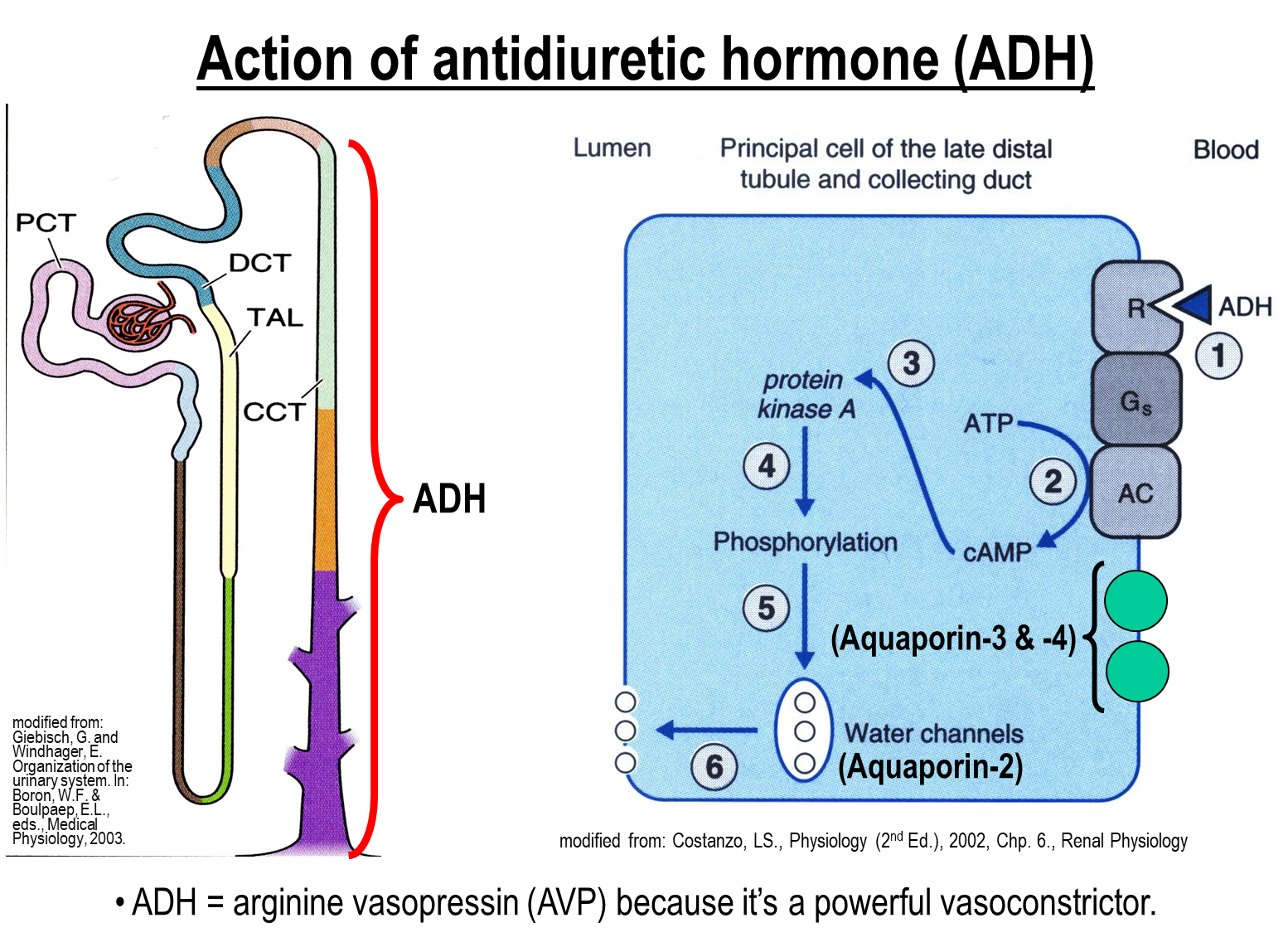
ADH is released from the posterior pituitary gland which will stimulate the receptors on the basolateral membrane on principal cells primarily at the collecting duct and then late distal tubule
1) ADH binds to receptors leading to adenylate cyclase and cAMP increase
→ leads to activation of protein kinase A and allows for insertion of aquaporin 2 onto the apical membrane
→ triggers an increased transcellular absorption of water
What stimulates the release of ADH?
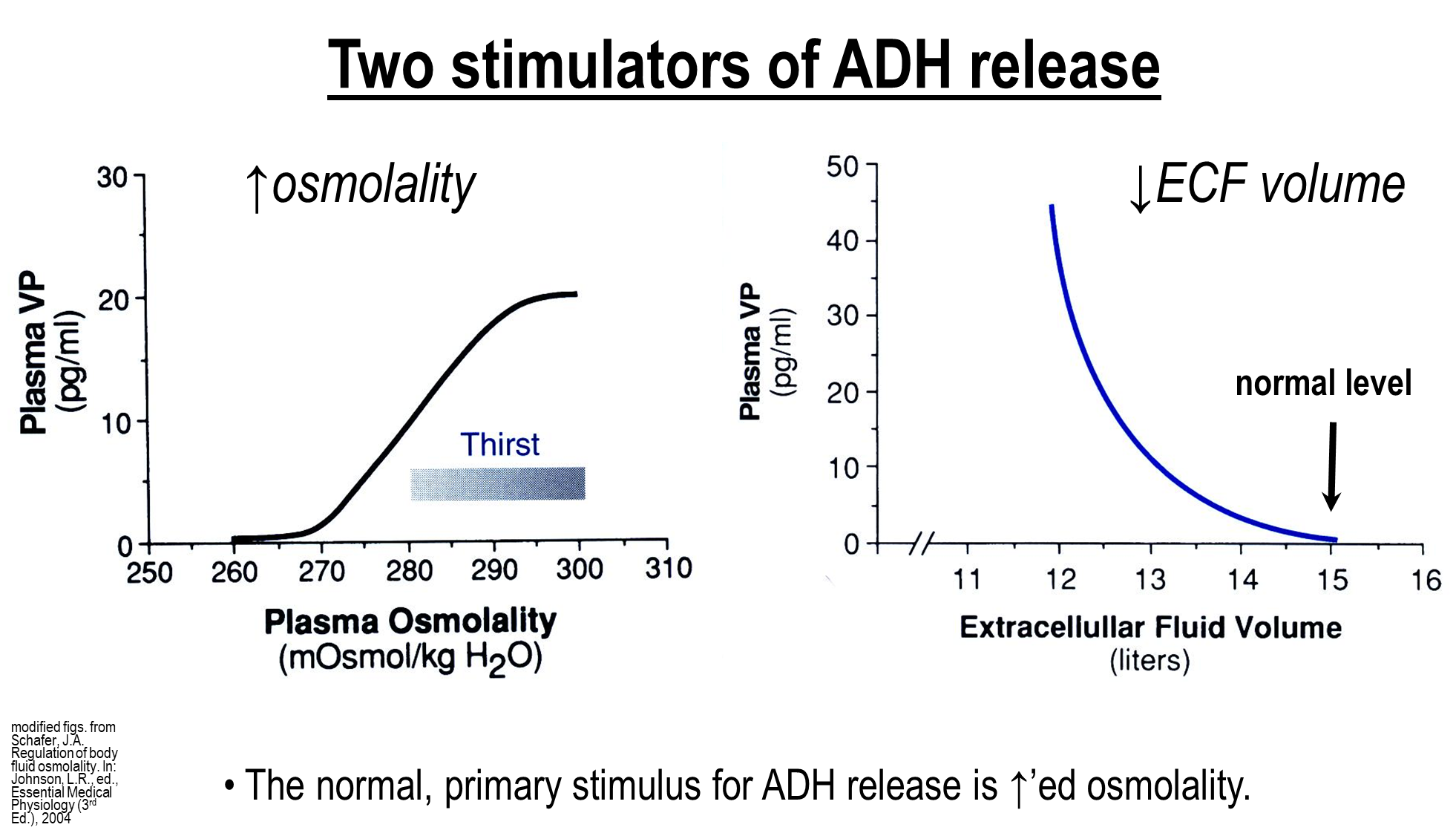
There is a primary stimulus and secondary stimulus for ADH release
1) Primary Stimulus - Increase in Plasma Osmolality works in a two pronged path
1 → increased plasma osmolality will cause an activation of osmoreceptors leading to activation of the hypothalamic thirst centers causing us to drink more water
2 → activation of osmoreceptors in the supraoptic nucleus will send signals to the posterior pituitary leading to ADH release
2) Secondary Stimulus - Decreased Extracellular Fluid Volume
→ ADH is released to promote water reabsorption to protect against rapid fluid loss
How does the tubule fluid osmolality progress along the nephron?
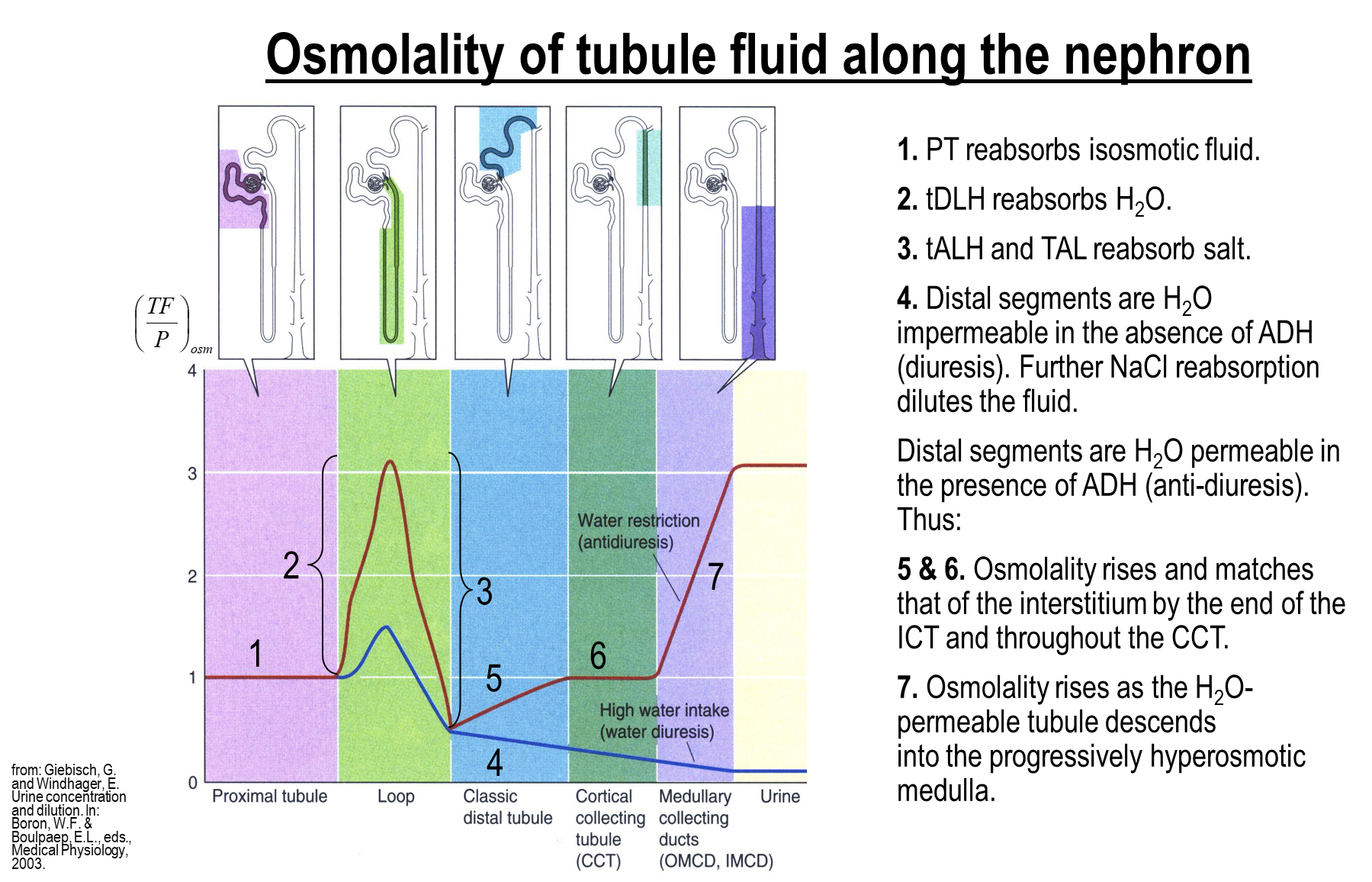
1) Proximal tubule reabsorbs isosmotic fluid
2) Descending Limb reabsorbs only water, leading to an increase in osmolality
3) Ascending Limb reabsorbs only salt, leading to a decrease in osmolality
4) Distal segments are water impermeable if ADH is not present, this will lead to further salt reabsorption, further diluting the tubule fluid
5) Distal segments are permeable to water in the presence of ADH leading to more water reabsorption causing osmolality to rise
→ important to know that the osmolality will level off and plateau at 300 in the cortical collecting tubule because the cortical collecting tubule interstitium only has a osmolality of 300
→ more water will be reabsorbed at the medullary portions as it becomes more hyperosmotic in the surrounding interstitium
What is the countercurrent multiplier?
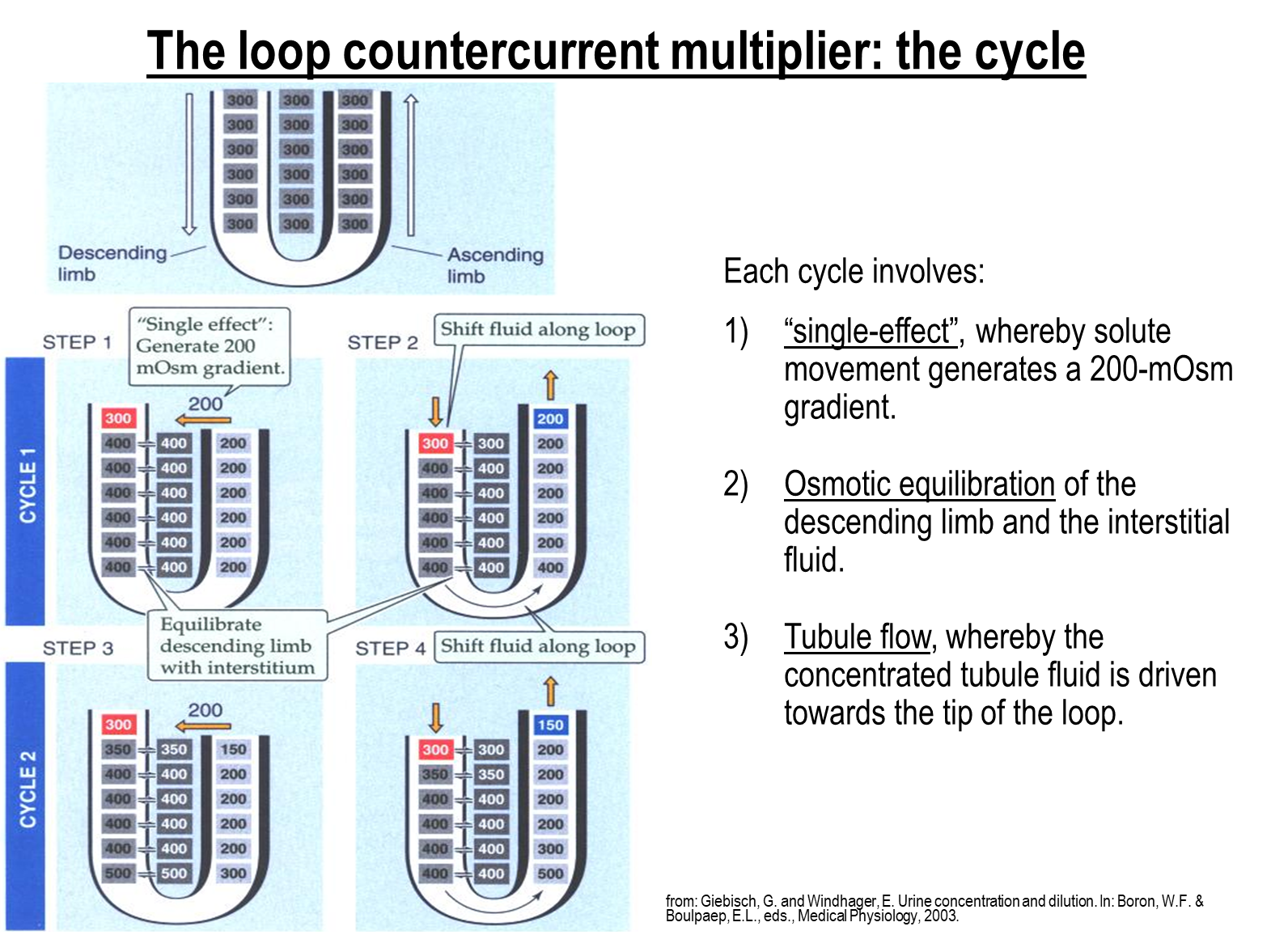
The countercurrent multiplier is a physiological process that generates an osmotic gradient for concentration of urine in the Loop of Henle. Occurs in three steps
1) Single Effect is the difference in osmolarity between the ascending limb and the interstitial fluid
→ created by solute actively transported out at the ascending limb
→ generates a 200 miliosmol gradient
2) Osmotic Equilibration occurs where water is pulled out of the descending limb due to the created gradient
2) Tubule Flow is constant through the descending and ascending limb
→ the concentrated fluid created in the descending limb will reach the ascending limb allowing for further solute reabsorption into the interstitium
What is the vasa recta responsible for?
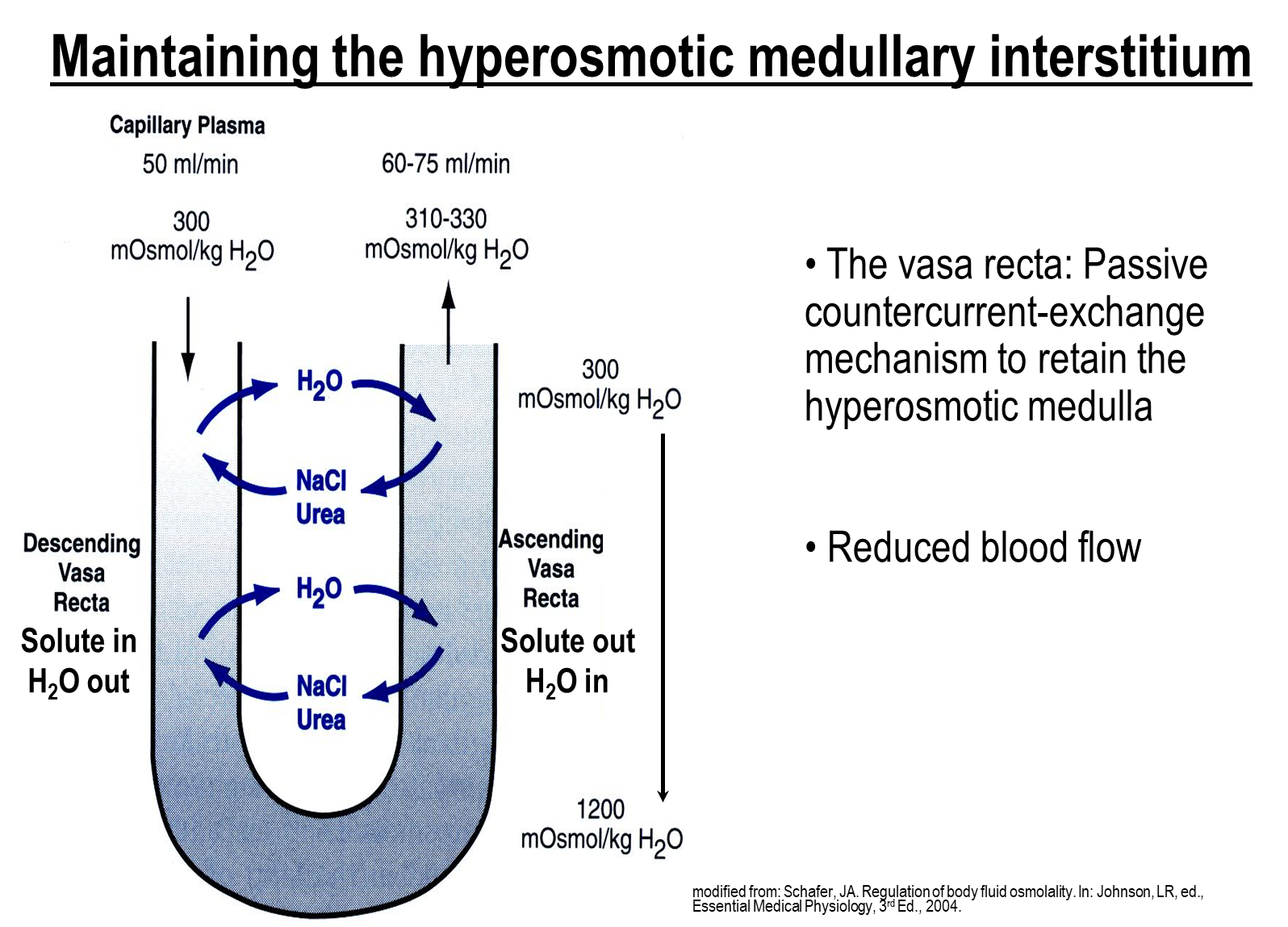
The Vasa Recta are a series of specialized capillaries that aid in facilitating countercurrent exchange by preventing washout and keeping the interstitium osmolarity high
1) The Vasa recta has a hairpin shape and runs parallel to the loop of Henle
→ descending vasa recta loses water passively and absorbs solutes from the hypertonic interstitium
→ this process reverses at the ascending vasa recta, which is now hypertonic relative to the interstitium and causes water absorption and solute secretion into the interstitium
What is the purpose of urea in the kidney?
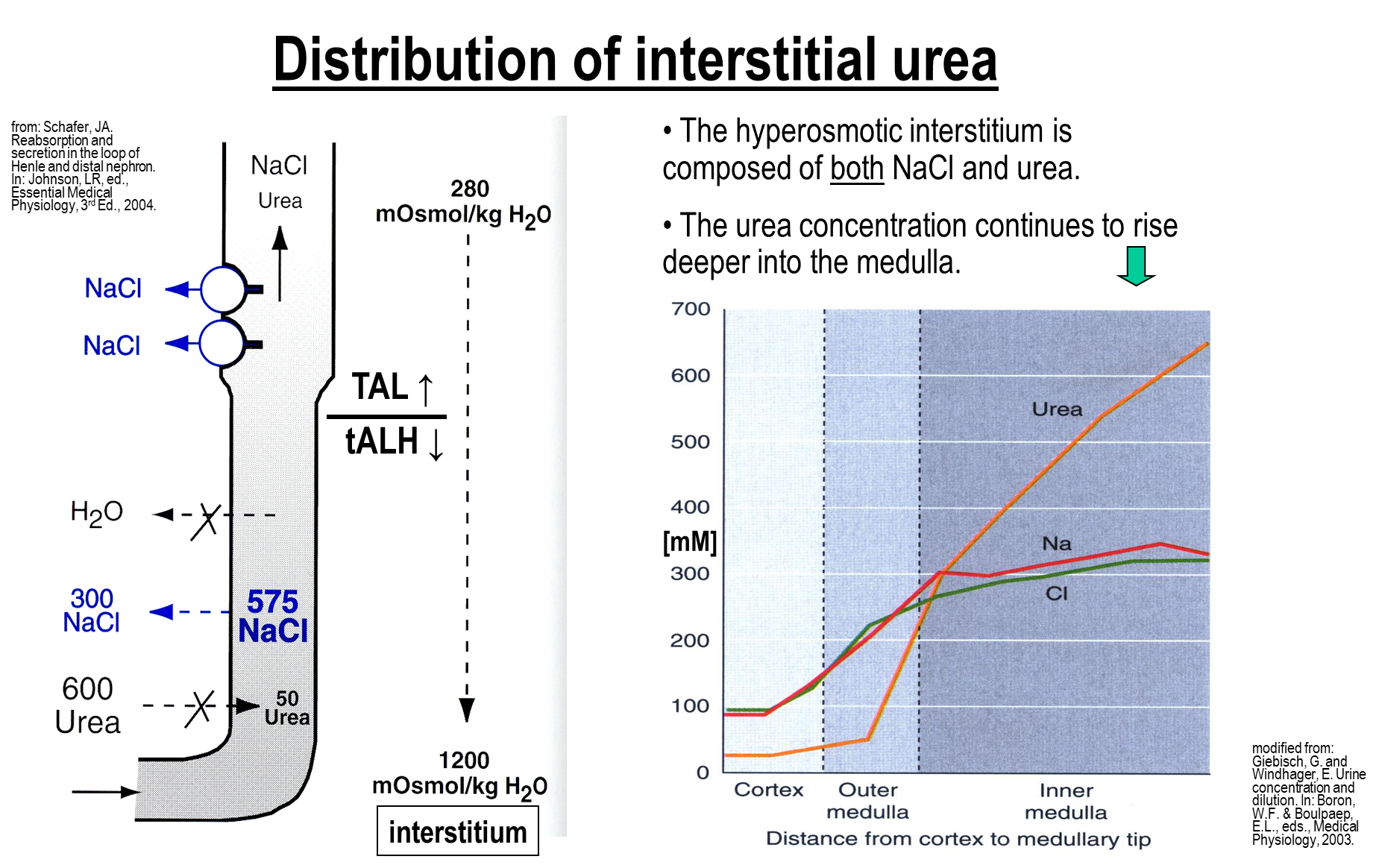
Urea concentration, along with NaCl is responsible for generating the hyperosmotic interstitium
1) While Sodium Chloride levels will rise to around 600 mM before leveling off in the inner medulla, the levels of urea will continue to rise the further you get into the medulla
2) in an extreme case of antidiuresis half of the osmolality is from NaCl and half is from urea
How is the thin ascending limb in the loop of henle able to passively reabsorb when the osmolality is so high?
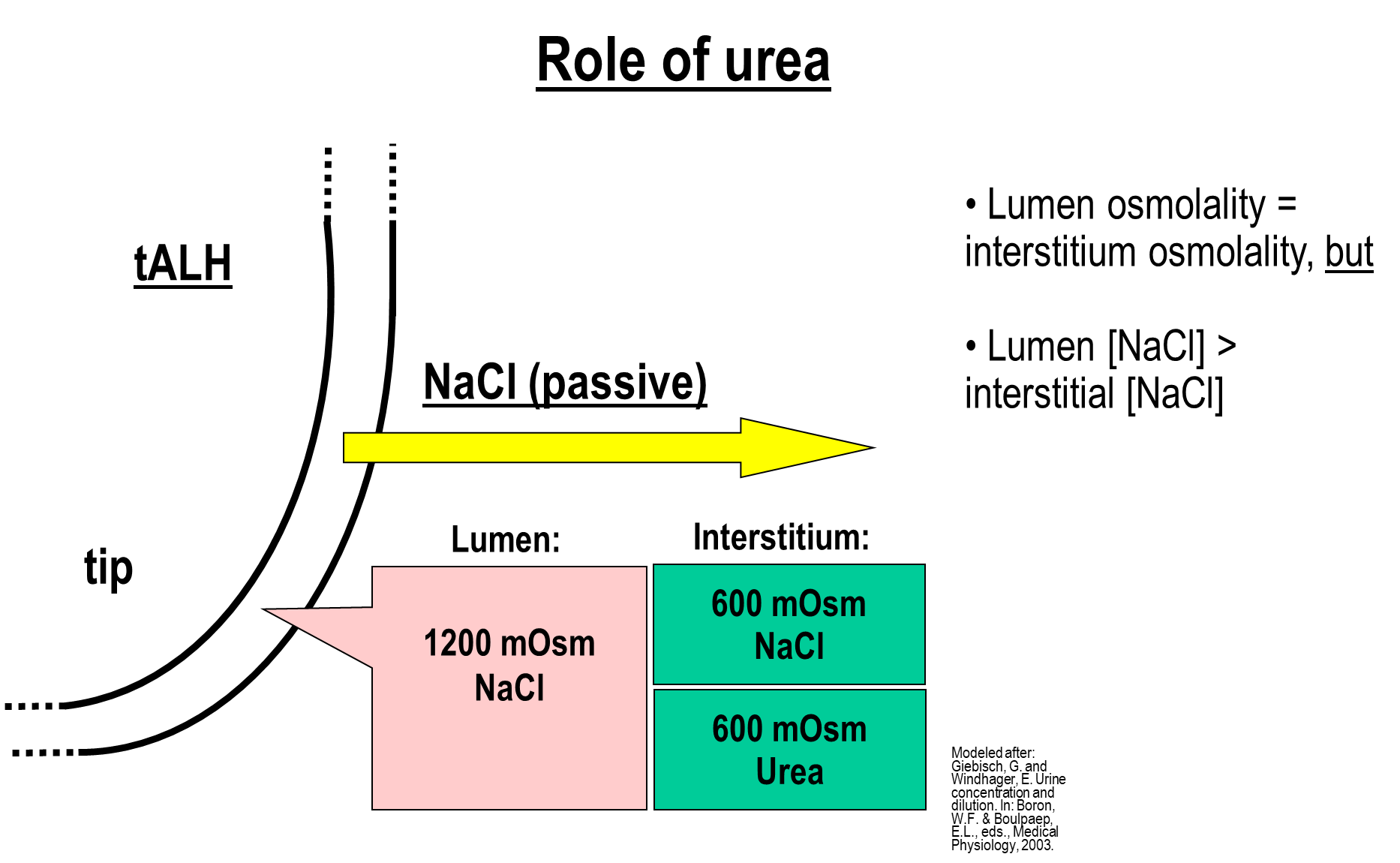
The point where the ascending limb and the descending limb meet is where the osmolality in the interstitium and tubule is the highest
1) Despite this, the thin ascending limb uses passive salt reabsorption because the composition of the concentrated environment in the tubule vs the interstitium is different
2) While both the interstitium and lumen have an osmolality of 1200, the composition of these two are different, allowing for passive reabsorption to occur
→ in the lumen the concentration is primarily due to sodium chloride
→ in the interstitium the concentration is due to half urea and half sodium chloride
This means that salt can be passively reabsorbed even when osmolality is the same
What is Urea Recycling
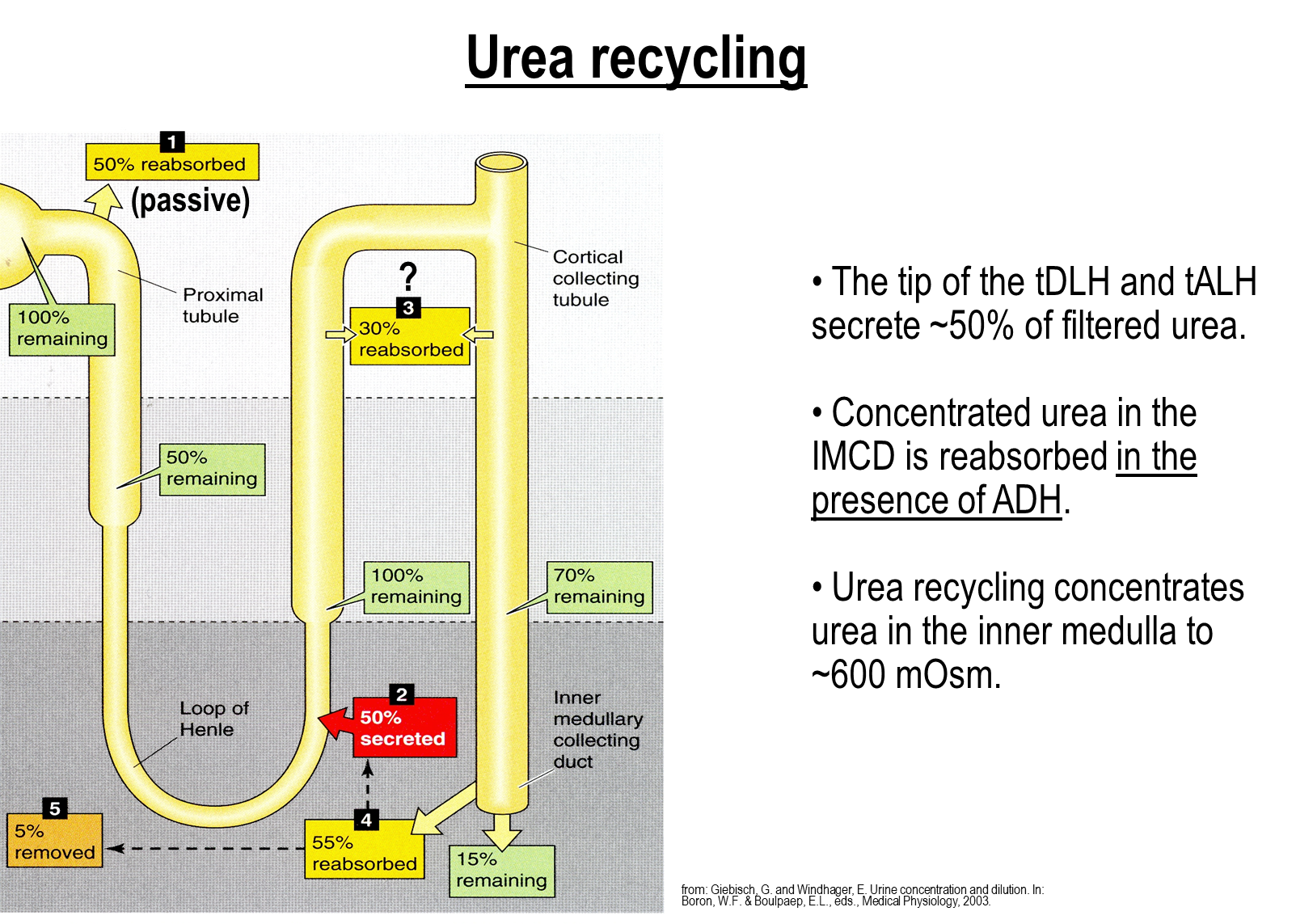
Urea recycling is where the last portions of the collecting duct will reabsorb urea and dump it into the interstitium.
1) In the proximal tubule around fifty percent is reabsorbed, which is then secreted back into the tubule at the early ascending limb
→ this means there is 100 percent filtered load of urea still present at the remaining nephron segments
2) This high concentration of urea will reach the inner medullary collecting duct where it is reabsorbed and then dumped into the interstitium
→ this process is stimulated by ADH, which will lead to water reabsorption leading to concentration of urea in the collecting duct
→ ADH will also stimulate Urea Transporter 1 (UT1) on the inner medullary collecting duct allowing for transport of urea
What six factors would affect urinary concentration
1) Length of the Loop of Henle
→ the longer the loop, the more concentrated the urine
2) Rate of Active NaCl reabsorption in the Ascending Limb
→ interrupting the NaKCl transporter will impair potassium secretion into the lumen and impair cation reabsorption
3) Protein Content in Diet
→ protein leads to higher concentrations of urea
4) Medullary Blood Flow
→ low blood flow promotes a high interstitial osmolality
5) Osmotic Permeability of the Collecting Ducts and Tubules
6) Luminal Flow in the Loop of Henle