Cornea, Sclera, Conj
1/140
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
141 Terms
What is the purpose and characteristics of the sclera?
Form a protective shell to protect the internal structures of the eye
Opaque - prevents light entering and minimises internal light scatter
Rigid - prevents eyeball from being distorted when rotated
Resists changes in shape from changes in IOP
What is the sclera innervated by?
Long and short ciliary nerves
Has widespread nervous plexus
What Sx are present if the nervous plexus is inflamed?
Dull ache
Pain on eye movement - EOM attached to sclera
How many layers does the sclera have?
1) Tenon’s capsule or Fascia Bulbi
2) Episclera
3) Scleral Stroma
4) Lamina Fusc
What is Tenon’s capsule?
Connective tissue layer made up of radial collagen bundles which commence at the limbus
Avascular structure
What is the Episclera?
Made up of loosely arranged collagen bundles in a circumferential arrangement
Highly vascular structure fed by the anterior ciliary arteries
What is Scleral Stroma?
Consists of dense layers of collagen bundles arranged in an irregular pattern
Irregular pattern = opacity of the sclera
Viscoelastic structure - can respond to external forces
Receives a small blood supply from the anterior and posterior ciliary arteries
What is Lamina Fusca?
Innermost layer e.g forms an interface c Choroid
Faint brown appearance - melanocytes
Collagen fibres passing from sclera to choroid form a weak attachment
Why may the sclera appear yellow?
Age - increased fatty deposits
Liver disease

Why may the sclera have a blue tinge?
Seen in infants - due to underlying uveal tract showing through
Seen in Px with connective tissue disorder

What is a scleral hyaline plaque + RF?
Innocuous condition seen in elderly px, close to the insertion of the medial or lateral muscles
RF; age, females, moderate to high myopia and degenerative arthritis
What is the corneal epithelium?
Consists of 5-7 layers of cells - connected by tight junctions which prevent entry of water from TF
Squamous cell layer - shows microvilli
Cell division occurs at limbus - then migrate to centre of cornea - approx 7 days for corneal epithelium to be replaced
What is the function of microvilli?
Assist in the retention of tears on the eye
Secrete a glycocalyx substance which connects with the mucin layer of TF
What is Bowman’s layer?
Dense acellular fibrous layer of collagen which terminates at limbus
What is corneal stroma?
Thickest layer (90% of CT)
Regular matrix of collagen fibrils embedded in glycosaminoglycans - regular pattern - ensures cornea remains transparent
Any disruption to the regular spacing = reduction in transparency e.g penetrating injury
What is Descemet’s membrane?
Basement membrane of the corneal endothelium
Continuous with the TM - Schwalbe’s line
Thickens with age
What is corneal endothelium?
Single cell layer - hexagonal & regular in shape
Where does the cornea receive its nutrients from?
Avascular structure - receives nutrients via diffusion from the aqueous and vessels of the limbus
Central cornea - oxygen from the atmosphere indirectly via TF
Where do the vessels at the limbus arise from?
Anterior ciliary arteries of the conjunctiva and sclera
Why is the cornea immune privileged and what does it mean?
Due to an absence of BV
It means that there is a reduced risk of a corneal graft being rejected
How is the cornea innervated?
Sensory nerves arising from the long and short ciliary nerves - they arise from the Ophthalmic division of the trigeminal nerve
Corneal nerves are unmyelinated - don’t interfere with corneal transparency
Nerves terminate at the corneal epithelium
Dense nerve endings account for the cornea’s pain response to even a slight touch
What occurs with a loss of corneal innervation?
Neurotrophic Keratopathy
What is the conjunctiva?
A thin mucous membrane which covers the outer surface of the eye
What are the two layers of the conjunctiva?
Outer stratified epithelium - contains goblet cells - responsible for producing the mucus content of TF
Inner connective tissue layer - BV of conjunctiva are located alongside nerves
Conjunctiva also contains accessory lacrimal glands
How does the conjunctiva receive its blood supply?
Palpebral arcades of the eyelids OR anterior ciliary arteries
What is the conjunctiva’s nerve supply?
From the trigeminal nerve via Ophthalmic division - as with cornea
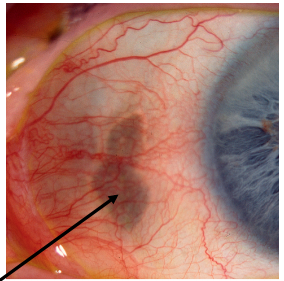
What is episcleritis?
An inflammatory condition affecting the episclera
Can be recurrent
Many cases idiopathic but association possible in bilateral cases with rheumatoid arthritis and IBS
More frequent in Females
No tarsal conj, AC/Corneal involvement
Peaks at 12 hours and typically lasts 2-3 days
May lead to dry eyes due to association with RA
Mostly Unilateral
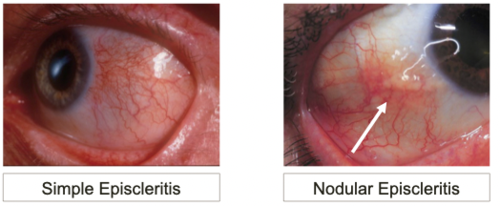
What is Simple Episcleritis?
80% of cases
Sectoral or diffuse redness - dilated episcleral vessels WITH areas of WHITE unlike Scleritis
Px reports mild ache or burning sensation of acute onset
Eye will be tender to touch + watery, painful
No affect on VA, rarely photophobia

What is Nodular Episcleritis?
20% of cases
Less acute onset with redness increasing over a couple of a days
Elevated nodule is seen
Can be more persistent
No affect on VA, rarely photophobia

Simple v Nodular Appearance
What can be useful in the diagnosis of Episcleritis?
Use 2.5% Phenylephrine - check if vessels blanch - e.g area of redness to now quiet
Use cotton bud to see if redness/vessels move
What is the management for either case of Episcleritis?
Nothing as usually self resolves within 7-10 days if mild
Advise cold compress, ocular lubricants + NSAIDs e.g ibuprofen to ease sx
In severe cases/nodular - refer for mild topical steroids + systemic NSAIDs
In recurrent cases - refer to secondary care for investigation for any underlying systemic disease
What is scleritis?
Inflammation of the sclera - scleral + episcleral tissues - can also involve cornea and uveal tissues
Rare but sight threatening
More frequent in females - aged 40-60
30-40% of cases are associated with autoimmune conditions
Small proportion due to infectious origin from organisms - Herpes Zoster Ophthalmicus
Can affect both anterior and posterior sclera
Vessels would not blanch with phenylephrine
May see uveitis alongside
Bilateral in 30-50% of cases
Sx worse at night
What is anterior scleritis?
Usually in 50s and over - females
Redness can be diffuse or nodular due to dilated scleral vessels
Diffuse - generalised or sectoral redness - in top and lower fornix
Nodular - raised areas about 3-4mm from the limbus - becomes translucent as scleritis resolves
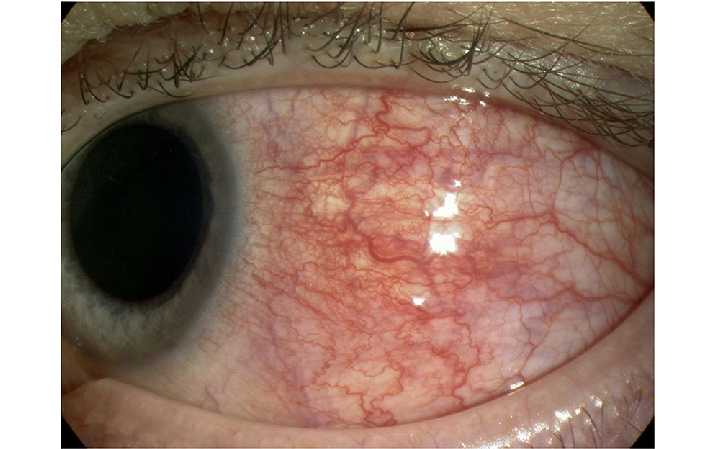
Diffuse
Nodular
What are the sx of anterior scleritis?
Intense, Severe and deep pain, may radiate to face and brow area - may wake them up from sleep
Eye is tender on eye movement
Reduced Vision
Photophobia
What is Necrotizing anterior scleritis?
15% of cases - more aggressive form
Px generally older ~ 60yrs
60% cases are bilateral
Can suffer severe ocular damage if treatment is delayed
What is posterior scleritis + sx?
10% of scleritis cases
Sight loss can be rapid
35% cases bilateral
Can present in healthy px under 40 yrs
When it occurs in older px, they generally have systemic disease e.g rheumatoid arthritis
Associated inflammation of EOM (myositis) = px may experience pain on eye movement + painful to touch
NO PHOTOPHOBIA
What is posterior scleritis associated with?
May lead to;
exudative RD
Choroidal folds
Disc Oedema
Management for different types of scleritis?
Necrotizing Anterior Scleritis + posterior scleritis = emergency same day referral
Non-necrotizing Anterior Scleritis - seen within a week - semi-urgent referral
Advise analgesia
Advise Sun Rx to minimise photophobia

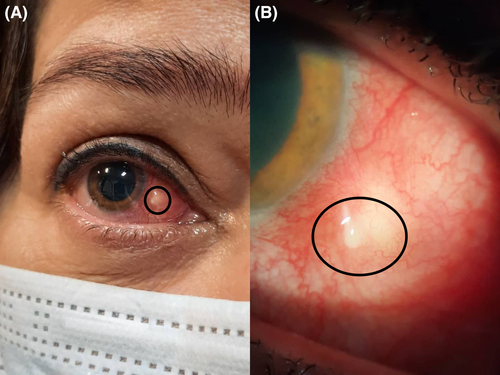
What does Chemosis mean?
Oedema of the Conjunctiva

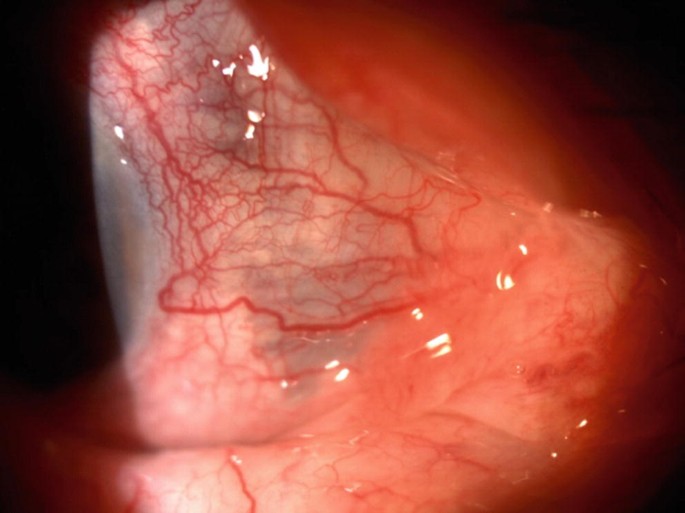
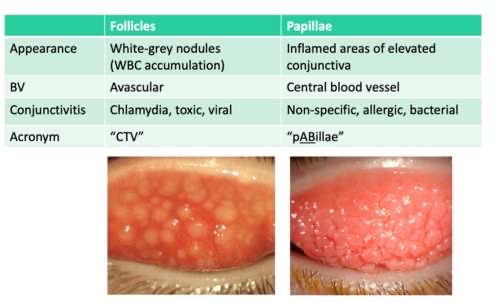
What are follicles?
Discrete raised translucent lesions with blood vessels running around them
Indicate prolonged inflammation has been present

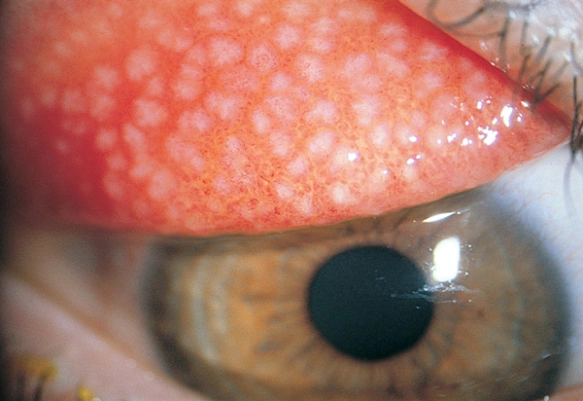
What are Papillae?
Discrete raised lesions with a central vascular core
Macro papillae <1mm diameter
Giant papillae >1mm diameter
Indicate prolonged inflammation has been present
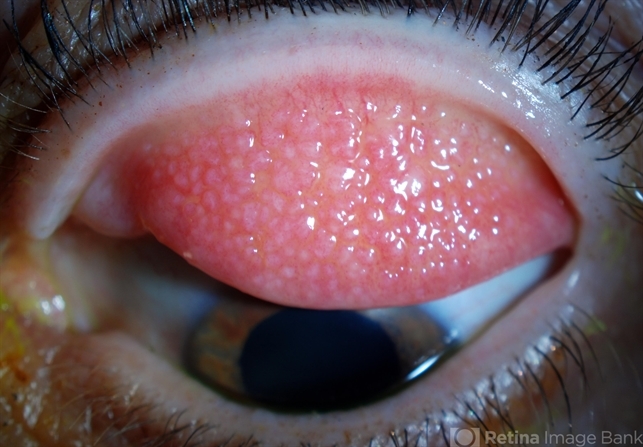
Img of Follicle vs Papillae

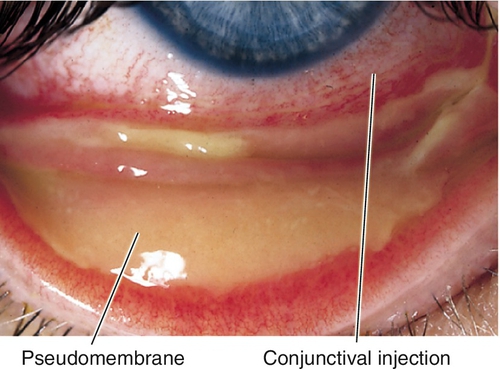
What is a pseudo membrane?
Coagulated exudative material which can be peeled away from the conjunctiva
Conjunctivitis - monocular/binocular
B - starts mono, bino within 1-2 days
V - starts mono, bino within 1-2 days
A - acute onset mono/bino - depends on allergen type
Conjunctivitis - redness
B - towards fornixes
V - generalised redness - more severe than others - poten. haemorrhage
A - generalised redness
Conjunctivitis - VA
B - normal
V - mildly affected
A - Fluctuates
Conjunctivitis - chemosis
B - No
V - No
A - YES
Conjunctivitis - Papillae/Follicles
B - P
V - F
A - P
Conjunctivitis - Discharge
B - muco-purulent
V - watery, sticky
A - watery with increase in mucous
Conjunctivitis - irritation
B - mild, burning, gritty
V - mild, burning, gritty
A - itchy
Conjunctivitis - photophobia
B - NO
V - MILD
A - NO
Conjunctivitis - cornea
B - superficial punctate stains
V - Microcysts, punctate epithelial stains within 7-10 days, corneal infiltrates if severe
A - generally clear
Conjunctivitis - Eyelids
B - Stuck together in the morning
V - Oedema
A - Oedema
Conjunctivitis - Lymph node signs
B - absent unless very severe
V - enlarged preauricular nodes - in front of the ear
A - absent
Conjunctivitis - GH
B - possible compromised immune system e.g Diabetes
V - YES - sore throat, flu-like sx
A - history of allergies
What is the treatment for Bacterial Conjunctivitis?
Usually resolves itself within 5-7 days s Tx
FUSIDIC ACID + CHLORAMPHENICOL
Return if persists longer than 7 days
What is the treatment for Viral Conjunctivitis?
Ocular Lubricants + Cold compress
May last 7-21 days
What is the treatment for Allergic Conjunctivitis?
Avoid Allergen
Cold compress + Ocular lubricants
Topical antihistamines + mast cell stabilisers may be used
Avoid eye rubbing
Bacterial Conjunctivitis summary
Contagious
Eyes stuck together in the morning - yellow/green muco-purulent discharge
Young Children + Elderly more at risk
Onset - over 24hrs
2nd eye involvement after 1-2 days
Papillae present
Vision is normal
Mild, burning, gritty
NO photophobia
Superficial punctate stains
In very severe cases - lymph node signs
Resolves without Tx - usually within 5-7 days
Viral Conjunctivitis Summary - adenovirus
Highly contagious
Sticky discharge in morning, watery discharge during day
Onset - 12 hours - 2/52
Severe redness compared to others
Vision affected - mildly
Mild, burning, gritty
Follicles
Mild Photophobia
Swollen eyelids
Microcysts, punctate epithelial stains, corneal infiltrates
Conjunctival Haemorrhages
Lymph node signs
PRESENCE OF PSEUDOMEMBRANE
Recent flu sx/sore throat
Ocular lubricants + cold compress
Lasts 7-21 days
Allergic Conjunctivitis Summary - Seasonal/Perennial
Not Contagious
Vision fluctuates
Common in young px - LESS COMMON with increasing age
Oedema of conjunctiva - chemosis!
Papillae
Watery discharge
No photophobia
Swollen eyelids
Itchy
NO lymph nodes
Cornea clear
Cold compress + Lubricants
Oral Antihistamine + Mast Cell Stabiliser e.g Sodium Cromoglicate
Can you continue wearing CL with Conjunctivitis?
NO - must cease until issue is resolved
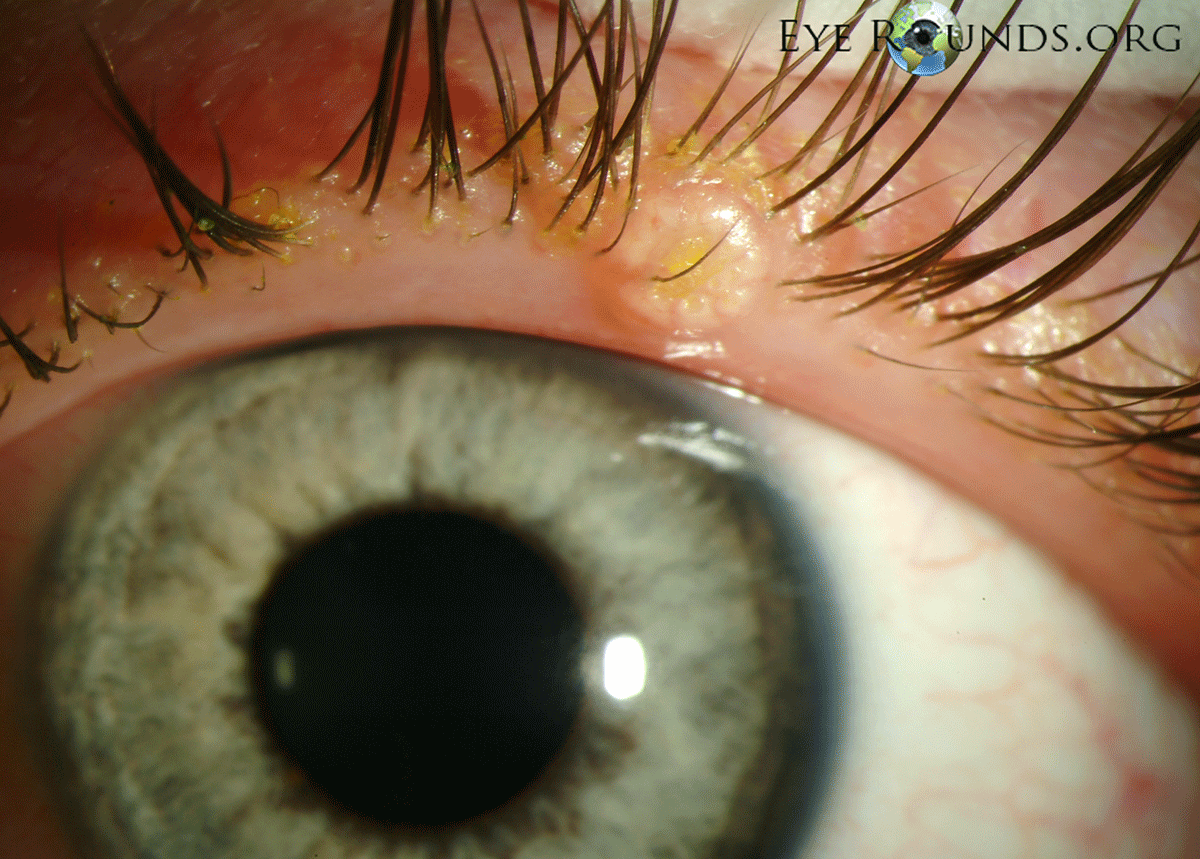
What is GPC / CLAPC + Signs?
Conjunctival reaction due to mechanical action - CL / Ocular Prosthesis
Reaction is exacerbated by protein deposits on the surface of a CL / Prosthesis
Mucus discharge and papillae under upper lid
Sx of GPA?
FB sensation
Itching
Mucous discharge
What is the treatment for GPC?
Ensure Optimum fit + cleaning process of CL / Prosthetic
Mast Cell Stabilizers - to alleviate acute Sx
Temp. cease lens wear
What is Molluscum Contagiosum?
Associated with chronic unilateral conjunctivitis - mild redness + irritation
Usually in children aged 2-4
Assessment of eyelid may reveal a small wart lesion on lid margin and a follicular conjunctivitis - follicles under eyelids
More severe in immunocompromised individuals
Referral indicated for lesions on eyelid margin
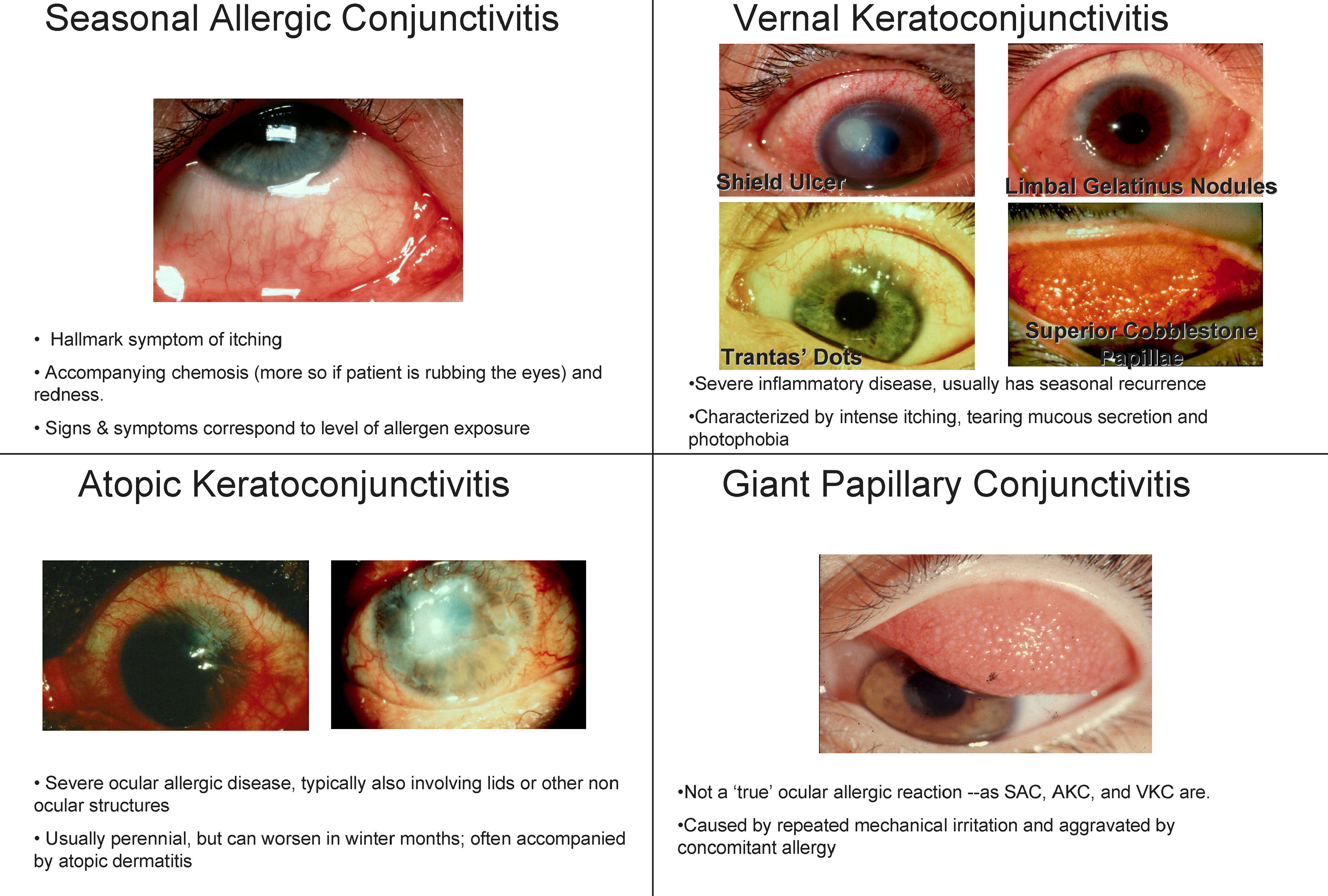
What is Vernal Keratoconjunctivitis?
Inflammatory condition that affects both conjunctiva + cornea
Combined IgE and Histamine modulated
Mediated due to immune reaction
Occurs mainly in boys from 5 to teenage years before resolving
Recurrent, rare in UK
90% of Px have a history of Atopy - asthma / eczema
Bilateral
More common in Africa + Indian subcontinent
What are the sx of Vernal Keratoconjunctivitis?
Itchy, watery eyes
FB sensation
Pain + Photophobia if corneal involvement
Blurry vision
What are the signs of Vernal Keratoconjunctivitis?
Reduced VA - corneal involvement
Thick, stringy mucous deposit may be seen
Papillae on palpebral conjunctiva >1mm in size - cobblestone c large hyperaemia -
Superior punctate epithelial erosions - can become ulcerative in future - leads to corneal ulcer - photophobia
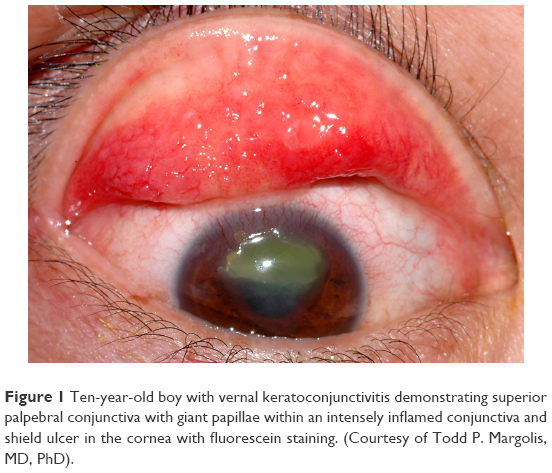
Management of Vernal Keratoconjunctivitis?
Referred to Ophthalmologist due to sight threatening nature
Corneal involvement - emergency
No corneal involvement - see within 2/52 - semi urgent
What is Atopic Keratoconjunctivitis?
Similar sx to VKC but occurs in adult population - 30-50 yrs
IgE and type 4 hypersensitivity mediated reaction
Due to overreaction of immune system as with VKC
Sx are more severe and unremitting than VKC
History of Atopy as with VKC - greater link in AKC
Affects both genders evenly unlike VKC
May see cracked skin
Tarsal papillae
Typically a year round condition unlike VKC - OFTEN WORSE IN WINTER
Management of Atopic Keratoconjunctivitis
Referral to Ophthalmologist within 1/52 if active corneal involvement - urgent
If stable then routine
Allergen avoidance, cold compress
Advise seeing GP for oral and topical antihistamine
If GP management fails then semi urgent

AKC
What is a Sub-Conjunctival Haemorrhage (SCH)?
Arise due to bursting of either the episcleral or conjunctival vessels
Blood collects in the subconjunctival space due to BV located in inner connective tissue layer of conjunctiva
Associated with coughing or vomiting - temporary increase in venous pressure = vessel burst
Most commonly found on the temporal or inferior conjunctiva - unilateral
Seen in over 50s
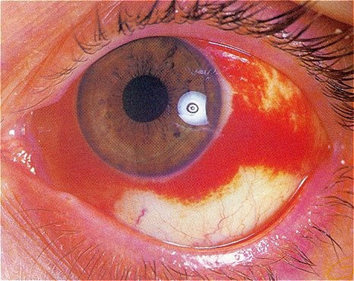
RF / causes of SCH?
Hypertension / DM2 / Anticoagulant Meds
Ocular Trauma - orbital / skull fractures - blood enters conjunctival space from retrobulbar vessels
Eye rubbing
Surgery

What are the sx of SCH?
Asymptomatic
May report mild irritation
What is the management of SCH?
If cause is due to Orbital / skull fractures - Emergency referral due to blunt trauma
Spontaneous SCH - managed in practice as it will resolve over next 1-2 weeks - return if persists longer
Recurrent SCH - referral to GP to check bleeding / clotting disorders
What is Pinguecula?
Small lump on the bulbar conjunctiva adjacent to the limbus
More common on Nasal side but CAN have on both sides
Typically Bilateral but Asymmetric

Why does Pinguecula occur and when is treatment necessary?
Due to the effect of UV on Collagen fibres of the conjunctival stroma
Tx only required if it becomes inflamed /cosmetically unacceptable
What is the Tx for Pinguecula?
Short course of mild steroids
What is Pterygium and its signs?
Triangular fibrovascular growth which often commences in the nasal bulbar conjunctiva
Growth is slow but progresses towards cornea - leading to chronic dryness of cornea
Will interfere with CL wear
Causes astigmatic changes
Reduced vision if crosses visual axis / pupil area
Typically Bilateral but Asymmetric
What causes Pterygium?
Occurs more often in Px c UV exposure + Hot Dry Climates
Related to chronic dryness
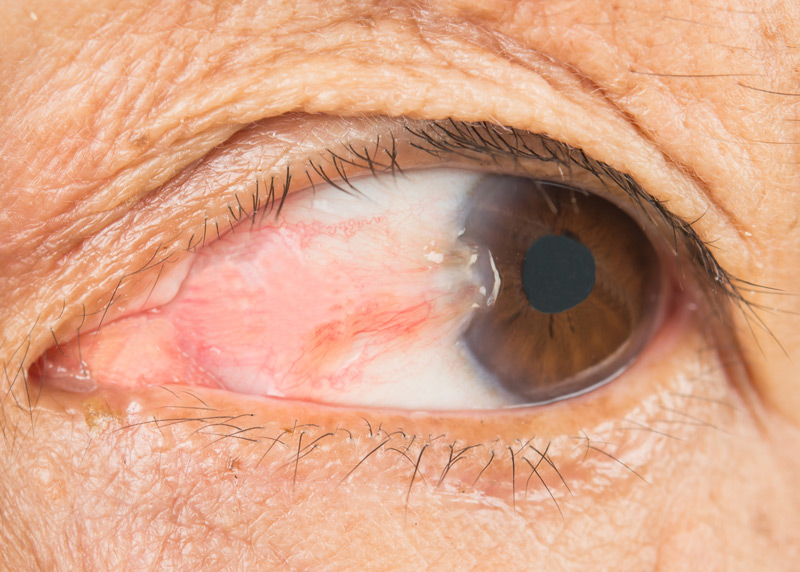
What is the management of Pterygium?
Use of Ocular Lubricants
Referred for surgery if pterygium is affecting vision, astigmatism / chronically inflamed / cosmetically unacceptable
What is Keratoconus (KC)?
Corneal shape - conical in profile - due to thinning of corneal stroma - causes a bulge forward
Bilateral BUT Asymmetric
Changes initially occur at the posterior corneal surface
Topographer used to aid diagnosis
When does KC typically manifest?
Manifests in 2nd or 3rd decade of life
Stabilises by 4th
What is the sx of Keratoconus?
Blurred vision
Potentially Monocular Dipl - due to irregular astigmatism
What are the signs of KC?
Myopic shift
Irregular Astigmatism - leading to monocular diplopia
Scissor reflex via retinoscopy
Vogt Striae
Fleischer ring
Munson Sign
Increased visibility of corneal nerves
Corneal scarring if progression
more common in younger Px + CL wearers
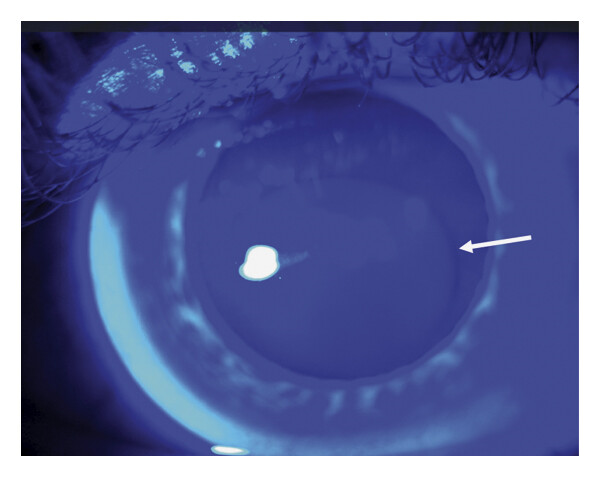
What is Vogt Striae?
Fine vertical lines / stretch marks seen in the posterior stroma of Descemet’s membrane

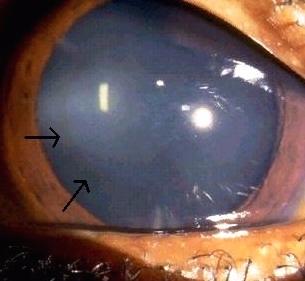
What is the Fleischer Ring?
Iron Oxide Hemosiderin deposits in the corneal epithelium seen at the base of the cone
What is Munson's sign?
Bulging of the lower lid on downgaze created by the conical appearance of the cornea
Creating a V shape of the lower eyelid

RF for KC?
Atopic conditions - persistent eye rubbing
Systemic conditions which involve abnormal connective tissue - Marfan Syndrome or Ehlers-Danlos
Downs syndrome
Middle Eastern / Asian ethnicity
FMH
What is the management of KC?
In mild cases vision may be correctable with specs
As it progresses - RGP may be used to correct irregular astigmatism
90% of px c irregular corneas use CLs to correct vision c majority RGPs
Refer for Corneal cross linking using riboflavin - increase biomechanical stability of the cornea - prevent progression - only in younger px
Routine referral in majority of cases
When is Cross linking contraindicated?
If cornea has <400 micrometres thickness
Px will still require CL post treatment
What percentage of Keratoconics require corneal transplants?
15 - 20%
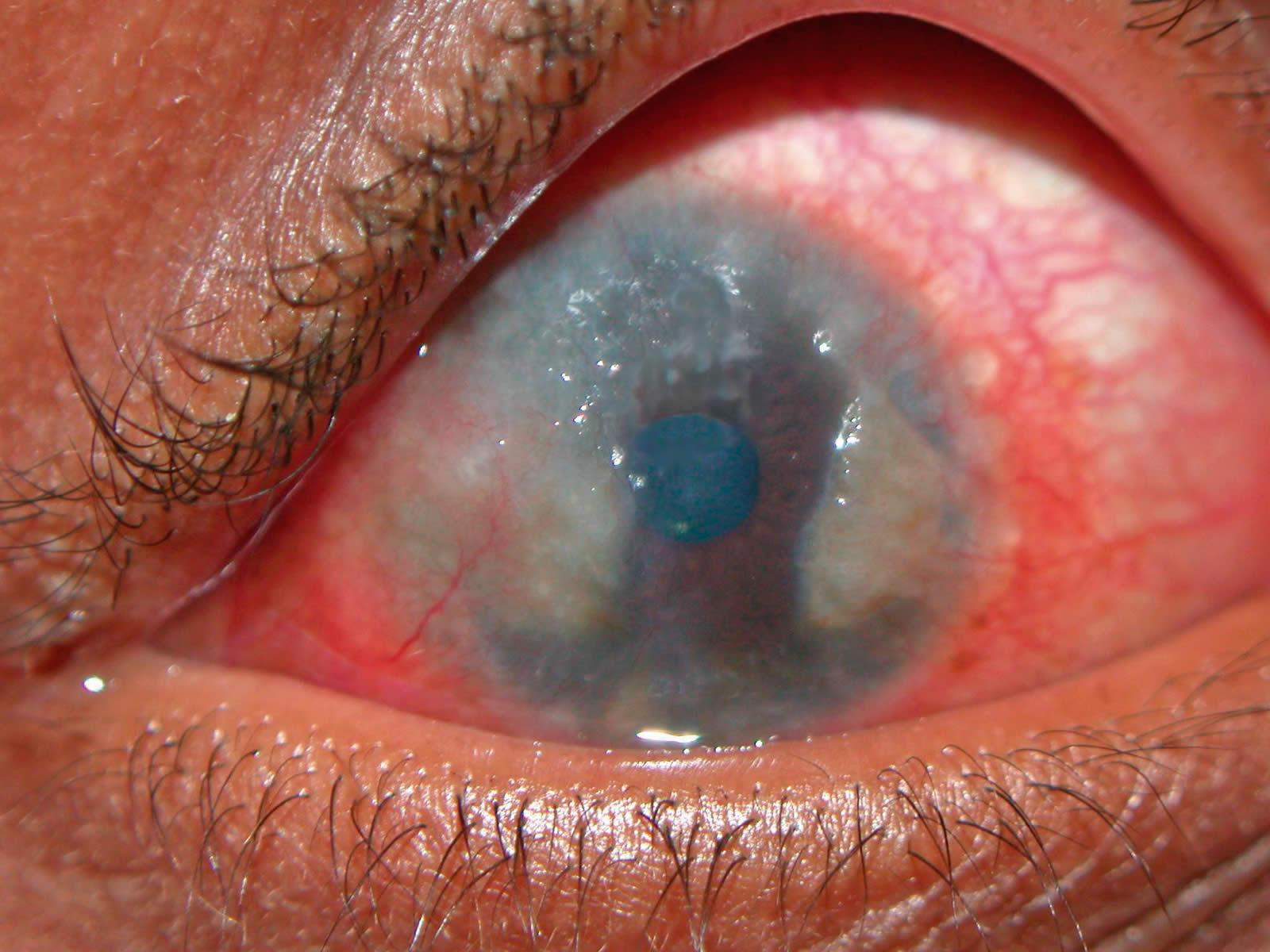
What are Acute Hydrops + RF?
Corneal steepening becomes so great that breaks occur in Descemet’s Membrane
Aqueous enters corneal stroma + epithelium causing CORNEAL OEDEMA
MEN 2-3x affected
Complication of KC
Eye rubbing
VKC
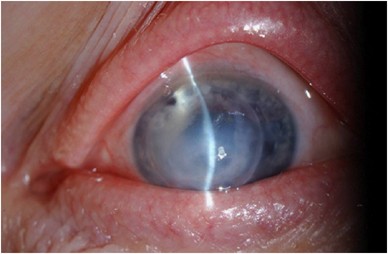
What are the sx of Acute Hydrops?
Reduced vision
Pain
Photophobia
Watery eye
Intolerable CL wear

What is the management of Acute Hydrops?
Breaks can repair themselves so condition should subside in approx. 3/12
No sign of Neovas - then can be managed by Optoms - review weekly
IF sign of Neo - refer URGENTLY
What is Fuchs endothelial dystrophy + RF?
Non inflammatory disease of corneal endothelium
Progressive dysfunction of endothelial pump mechanism results in corneal oedema and reduced vision
Most cases develop in 4th decade or later
Bilateral but ASYMMETRIC
More common in Females
Genetic RF
Smoking