12 ATAR Human Bio: Immune System
1/66
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
67 Terms
Pathogens
disease causing organisms (Eg. Bacteria, viruses, parasites etc.)
Vectors: host of a pathogen
these foreign organisms that invade the body + multiply cause communicable/infectious diseases
Bacteria
Single-celled organisms; 0.5 - 2 micrometers
found all over body, particularly on skin and in the alimentary canal.
Mostly harmless, some beneficial, some harmful
Classified by their cell shape
enter body through sites of entry (nose, mouth, open wounds) where they reproduce + colonise area
they then produce toxins which breakdown surrounding tissue cells
Disease symptoms often allergic responses to products of bacterium
diseases it cause= Anthrax, Gastroenteritis, Pneumonia, Tetanus, Tuberculosis (TB)
bacterial infections can be treated by antibiotics
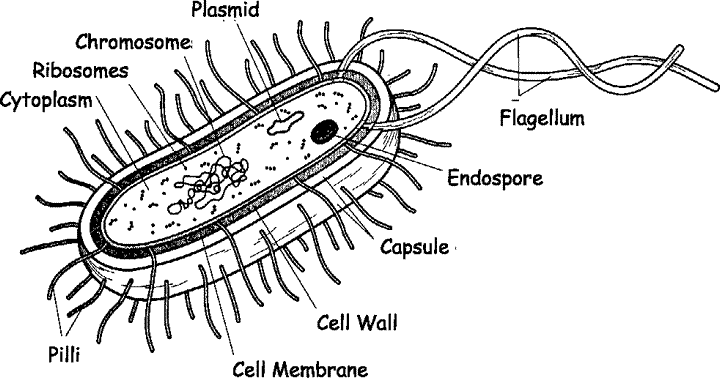
Bacteria structures
Slime layer- around outside of some bacteria
Cell Membrane- similar to other cells
Flagella- for movement; may have 1 or many but not found on all bacteria
Cytoplasm- appears granular due to presence of ribosomes, bacteria don’t have membrane bound organelles
Capsule- formed of complex carbohydrate by some bacteria; for protection
DNA- no nuclear membrane so DNA forms a tangle inside cell; some of DNA is in form of loops called PLASMIDS that can be exchanged during reproduction
Cell Wall- composition varies but often made of peptidoglycan; a combined carb-protein
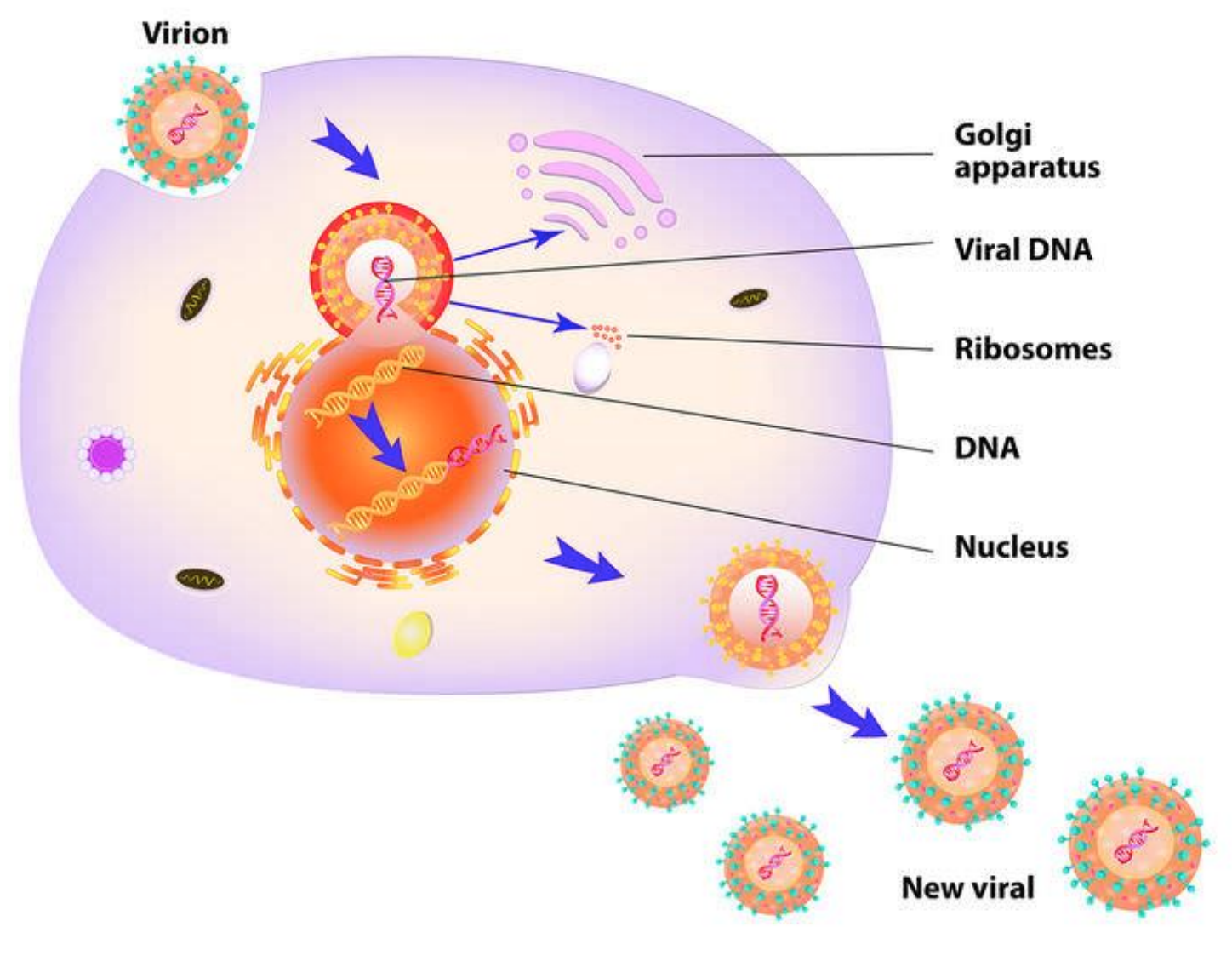
Viruses
Seen under electron microscopes
Distinctive structures containing DNA OR RNA, surrounded by a protein coat and lipid envelope, some have additional lipid envelopes.
Infect cells by introducing it’s own DNA (through host cell), so the cell manufactures virus particles.
diseases it causes= HIV/AIDS, chickenpox, colds, COVID-19, influenza, measles
TREATMENT; some drugs (anti-virals) can control infections, no drugs known to kill them, antibiotics cannot be used to treat viral infections (no cell wall)
Bacteriophages, Fungi + Parasites
Bacteriophages: Bacteria infected by a virus
Fungi: eg. ring worm, tinea
Parasites: eg. Malaria, Tapeworms, Lice, Scabies, Ticks
Transmission of Pathogens
Contact- direct + indirect
Body fluids
Droplets
Airborne Transmission (Aerosols)
Ingestion
Vectors
Contact- direct + indirect
DIRECT; Touching an infected person (skin infections and some STDs)
INDIRECT: Touching an object that has been touched by an infected person (drinking from the same cup)
Body Fluids
Blood/ other body fluids from an infected person come into contact with another person. (with mucous membranes (In nose/ mouth/genitals))
EG. being pricked by an infected needle. Hepatitis B & C are transmitted in this way.
Droplets
Tiny droplets of moisture may contain pathogenic organisms.
emitted when you breath, talk, sneeze or cough.
Droplets may be breathed in by another person or settle on food and then ingested.
EG. Cold and flu are spread by droplets.
Airborne Transmission
When airbourne moisture evaporates, some bacteria and viruses are able to survive (viable) as spores.
can be inhaled and can cause infection.
EG. Anthrax Spores, COVID-19
Ingestion
Contaminated food or drink may result in disease.
EG. Food poisoning (salmonella), dysentery and typhoid are transmitted this way.
Vectors
Transfer of pathogens by other animals. (spread pathogen to food and then it is ingested)
EG. Insects, ticks, mites, mosquitoes (malaria) and flies
Non-specific defences
work against all pathogens
body’s first line of defence
stop pathogens entering the body and limit their effect
External defenses: prevent pathogens entering the body
Protective reflexes: ejecting pathogens from the body
Inflammatory response: reduce the spread of pathogens
Fever response
External Defences
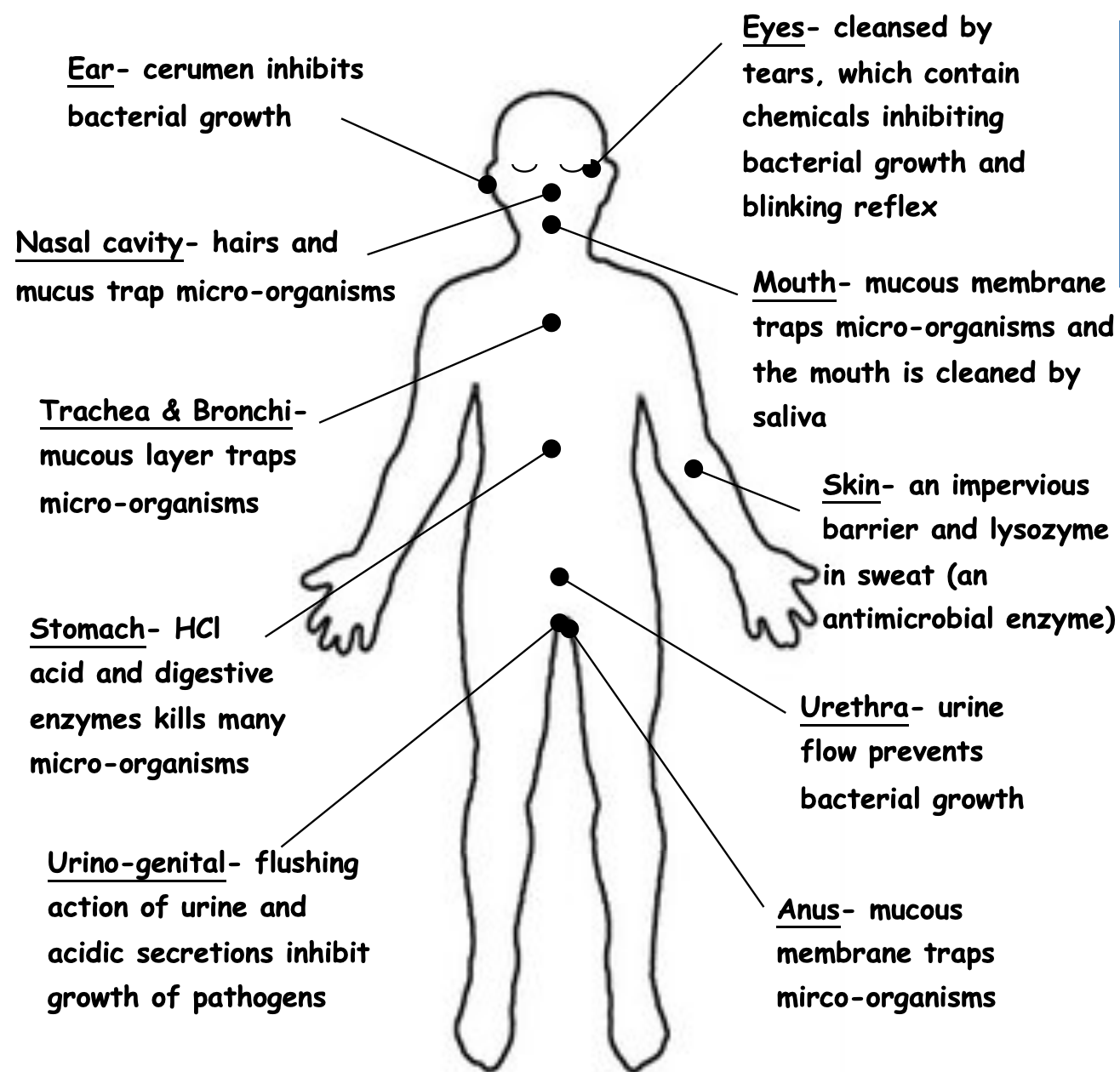
External Defences- skin
SKIN:
An IMPERVIOUS BARRIER, prevents entry of microorganisms, provided it is not broken by cuts.
Large numbers of bacteria live on the skin naturally, so new bacteria often find it hard to become established.
Sebaceous glands secrete SEBUM an oily substance that contains antibacterial substances that kill pathogenic bacteria
Sweat glands produce lysozyme (sweat- salts + fatty acids) that prevents growth of microorganisms.
External Defences- mucous membranes
line body cavities that open to the exterior.
Traps microorganisms and inhibits entry.
Digestive, Urinary and Reproductive tracts- Trachea + Bronchi, Nasal Cavity, Mouth Cavity , Anus, Stomach
External defences- hairs + cilia
Hairs – nose cavity and ears, traps any foreign particles.
Cilia – tiny hair like projections from cells, lines nose and trachea + bronchi
Beating motion moves mucous containing trapped particles upwards towards throat where they can be coughed up or swallowed
External defences- lysozyme + acids
Lysozome- enzyme found in tears, saliva, sweat and secretions from nose and tissue fluid that kills bacteria.
Acids –
HCl in stomach is concentrated enough to kill bacteria that has been ingested/those contained in mucous swallowed from nose + windpipe
Vagina also has acidic secretions that reduces growth of microorganisms.
Sweat is slightly acidic
External defences- cerumen + flushing
Cerumen (ear wax) – inhibits bacterial growth, protects outer ear against infections, slightly acidic and contains lysozyme.
Flushing action – urine flowing through urethra has a cleansing action which prevents bacterial growth. Women have a shorter urethra than men so tend to suffer from more bladder infections. Tears, saliva and sweat also have flushing action.
Protective Reflexes
reflex is an automatic, involuntary response to a stimulus.
4 reflexes that help to protect against infection:
Sneezing
Coughing
Vomiting
Diarrhoea
Sneezing
forceful expulsion of air from the lungs to eject air, mucous, foreign particles and/or irritating gases.
Stimulus= irritation of the walls of the nasal cavity.
Coughing
Caused by irritation to the lower respiratory tract. (Bronchi & bronchioles)
Air and mucous is forced from the lungs out, via the mouth.
Vommiting
Response to excess stretching of the stomach or to bacterial toxins.
results in contraction of the abdominal muscles & diaphragm to expel the stomach contents.
Diarrhoea
Caused by irritation of the intestines
response is increased contractions of the muscles of the intestinal walls, so irritant is removed quickly.
As most of the water is absorbed from within the large intestine, the swiftness of the contents moving through this area does not allow for the water to be removed
Internal non-specific defences
PHAGOCYTES: Engulf and digest microorganisms and cell debris
LEUCOCYTES (WBCs): Able to leave blood capillaries and migrate through tissues to site of infection or injury; Some secrete substances that destroy bacteria before engulfing it, others engulf live bacteria and then digest them.
MACROPHAGES: Large phagocytic cells that develop from leucocytes, wandering or fixed, engulf, digest or release chemicals to destroy other cells
Purpose of Inflammation
Reduce the spread of pathogens
Destroy pathogens
Remove damaged tissues & cells
Repair damaged tissue
‘-itis’ refers to inflammation, e.g. tonsilitis
Inflammatory response
1) Damage to cells causes mast cells to release histamine & heparin
Histamine increases blood flow (redness) & permeability of capillaries (swelling)
Heparin prevents clotting
These abnormal conditions cause pain
2) These chemicals attract phagocytes to consume debris & micro-organisms
The micro-organisms & phagocytes die and form pus
3) New cells are produced by mitosis
Lymphatic system
Lymph Vessels- more fluid will leak out of arterioles due to HP than will return to capillaries + veins, diameter larger than capillary=more volume collected
Lymph Nodes- each surrounded by CT that extends into the node, mass of lymphoid tissue; containing- lymphocyte, macrophages and plasma cells
ROLE-
trap large particles (bacteria)
macrophages destroy these particles- usually within 10-30 mins of being trapped
when infections occur= increase production of lymphocytes
specific immunity
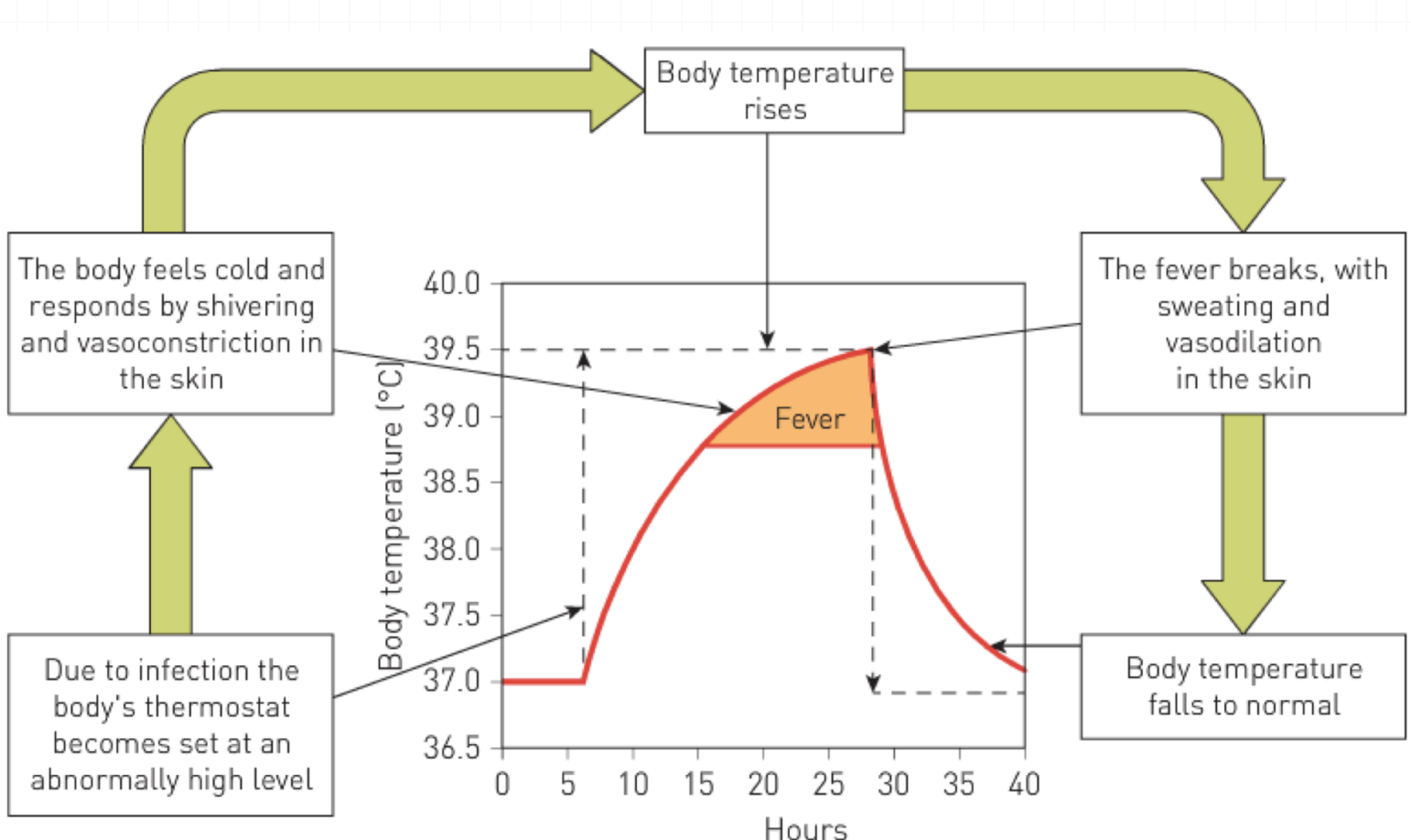
Fever Response
During infection (the inflammatory response) WBCs (or pathogens) release pyrogens= stimulus
Hypothalamus responds to the pyrogens to reset the body’s thermostat.
body “feels” cold and responds by shivering and vasoconstriction of arterioles in the skin.
Body temp rises
Macrophages drawn to the area and engulf the pathogen, then stimulated to release interleukins/cytokines (enhance the pyrogens= increase fever)
Eventually fever breaks, with sweating and vasodilation and body temp returns to normal.
Benefits of a fever
Inhibit growth of some bacteria and viruses
Speeds up chemical reactions in the body: promotes cells repair
enhance WBC function
enhance presentation of antigens to macrophages
increase production of antibodies
Specific defences
directed at a particular pathogen,
Only work on one particular disease
2 parts to immune response:
Antibody mediated/humoral- involves the production of special proteins= antibodies, which circulate around the body (blood + lymph) and attack invading agents
Cell mediated- involves formation of special lymphocytes (cells) that destroy invading pathogens. (inside cells)
Lymphocytes
Both these cells are produced in the bone marrow, and end in the lymphoid tissue:
About half the cells go to the thymus where they mature into T cells.
The other half of the cells mature in the bone marrow to become B cells.
Lymphoid tissue contains thousands of different types of B cells- each capable of responding to a specific antigen
Antigens
Both antibody-mediated and cell-mediated immunity are triggered by antigens.
any substance capable of causing a specific immune response, (generally causes the body to produce specific antibodies).
can be:
large molecules.
proteins, carbohydrates, lipids or nucleic acids.
a whole micro-organism, (virus particle/bacterial cell)
part of a bacterium- flagella, cell wall or capsule.
toxins produced by bacteria.
contained within tissues transplanted from another person, such as blood cells of a foreign blood group, and such things as pollen grains and egg white
Antibodies
a specialised protein that is produced in response to a non-self-antigen.
can combine with that antigen to form an antigen–antibody complex.
Antigen molecules have specific active sites and at these sites the antibody can combine with the antigen.
Antibody-mediated immunity (humoral response)
involves the production and release of antibodies into the blood and lymph.
provides resistance to viruses, bacteria and bacterial toxins before these micro-organisms or substances enter the body’s cells.
Humoral response process
Pathogen invades the body
An antigen (pathogen) is detected by a macrophage.
Macrophage engulfs the pathogen (breaks it apart) & presents antigen to B cells/B lymphocytes by displaying it on its cell membrane.
antigen activates B cells, they enlarge and divide into a group of cells called a clone.
Most of the clones become plasma cells, which secrete the specific antibody capable of attaching to the active site of the antigen.
antibodies circulate in the blood, lymph and extracellular fluid to reach the site of the invasion of microorganisms or foreign material.
B cells of the clone that did not differentiate into plasma cells remain as memory cells.
These memory cells spread to all body tissues to allow the response to occur more rapidly should the antigen enter the body again.
How do antibodies work to provide resistance to infection?
combine with foreign enzymes or bacterial toxins, or inactivate them by inhibiting reaction with other cells or compounds.
bind to the surface of viruses and prevent the viruses from entering cells coat bacteria so that the bacteria are more easily consumed by phagocytes.
cause particles such as bacteria, viruses or foreign blood cells to clump together — agglutination.
dissolve organisms.
react with soluble substances to make them insoluble and thus more easily consumed by phagocytes.

Primary vs Secondary Response
first exposure to an antigen the immune reaction= primary response.
body’s immune system usually responds fairly slowly, often taking several days to build up large amounts of antibodies
takes time for the B cells to multiply + differentiate into plasma cells.
However, primary response leaves immune system with a memory of that particular antigen.
second/subsequent exposure to same antigen= much faster response because of activity of memory cells.
plasma cells are able to form very quickly, with antibody levels in the blood plasma rising rapidly
Often response is so quick that the antigen has little opportunity to exert any noticeable effect on the body and no illness results.
Cell-mediated immunity
provides resistance to the intracellular phase of bacterial and viral infections
also important in providing resistance to fungi and parasites
involved in the rejection of transplants of foreign tissue
also appears to be important in fighting cancer cells.
Cell-mediated immunity process
T lymphocytes are responsible for cellular immunity, but it starts in the same way as antibody-mediated.
A macrophage (APC)/B cell encounters the foreign antigen, travels to the nearest lymph node and presents it to the T cells (Helper T-cells secrete cytokines to enhance this process)
antigen activates more T cells to become sensitised
The sensitised T cells enlarge and divide, each giving rise to a clone, a group of identical T cells.
Some cells of the clone remain in the lymphoid tissue as memory cells- able to recognise the original invading antigen.
If infection w/ same antigen should occur again, these memory cells can initiate a much faster response to the second and subsequent infections.
The T cells that don’t become memory cells develop further, producing 3 different types of T cells: Killer, Helper + Suppressor
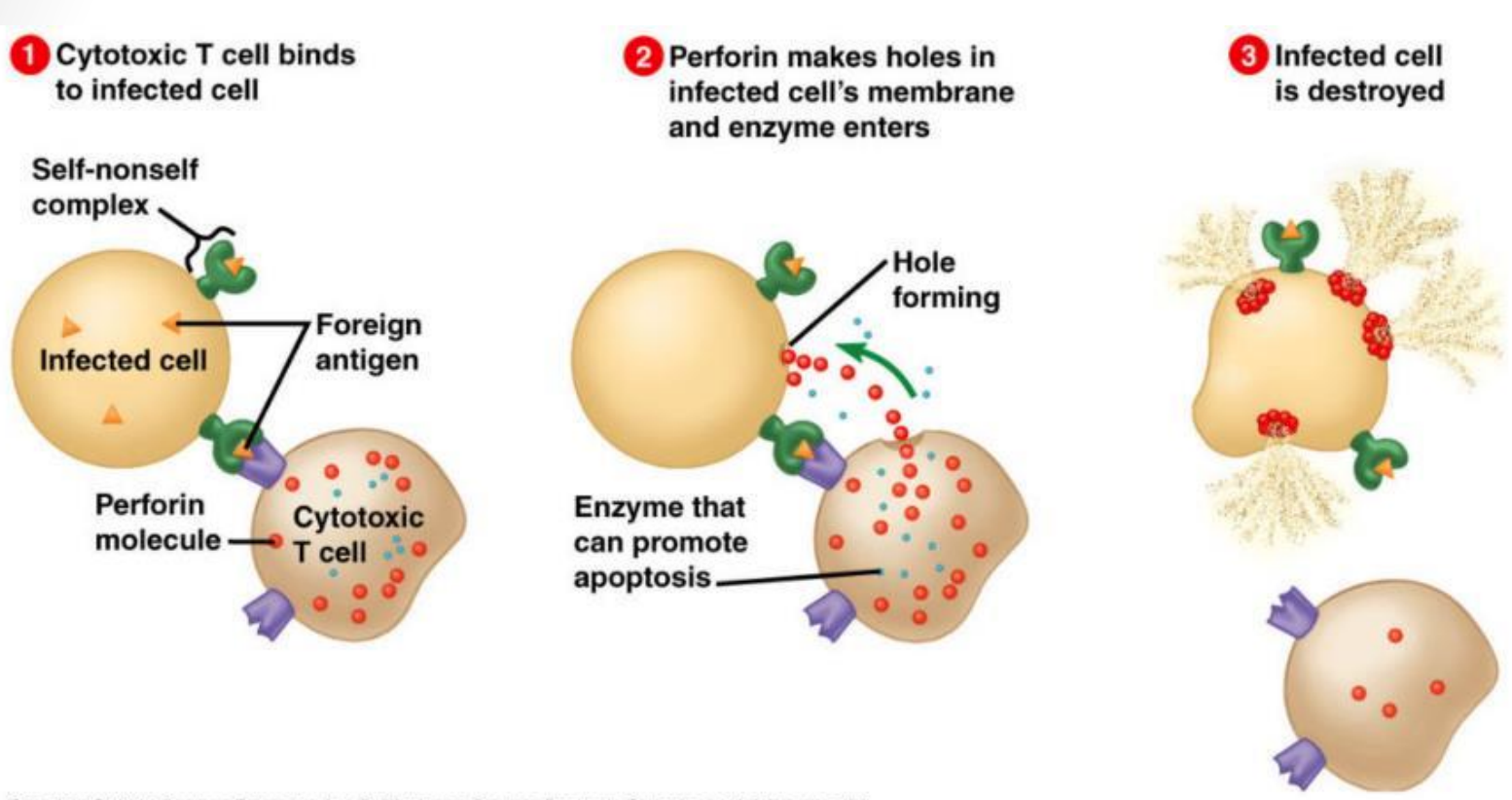
Killer T-cells
migrate to the site of infection and deal with the invading antigen.
attach themselves to the invading cells and secrete + inject a substance that will destroy the cell, and then go off in search of more infected cells.
Helper T-cells
secrete cytokines (substances) that:
cause more lymphocytes at the infection site to become sensitised= intensifying response.
attract macrophages to the place of infection so that the macrophages can destroy the antigens by phagocytosis.
intensify the phagocytic activity of macrophages
Suppressor T-cells
act when the immune activity becomes excessive/when the infection has been dealt with successfully.
release substances that inhibit T and B cell activity, thus slowing down the immune response.
Antibody-mediated VS Cell-mediated Immunity DIFFERENCES
Works against bacteria, toxins + viruses before they enter the body’s cells; also against RBCs of a different blood group than the person — Works against transplanted tissues and organs, cancer cells and cells that have been infected by viruses/bacteria; also provides resistance to fungi + parasites.
Most new B cells develop into plasma cells, which produce antibodies + release them into blood and lymph — Most new T cells develop into killer/helper T cells, which migrate to the site of the infection.
Antibodies combine w/ specific antigen and inactivate/destroy it — Killer T cells destroy the antigen, while helper T cells promote phagocytosis by macrophages.
Antibody-mediated VS Cell-mediated Immunity SIMILARITIES
Foreign antigen reaches lymphoid tissue
Certain B/T Lymphocytes stimulated to undergo rapid cell division
Some of the new B cells / sensitised T-cells form memory cells.
Types of immunity- Natural vs Artificial
NATURAL – occurs without any human intervention ARTIFICIAL – results from giving people an injection of an antibody or antigen that triggers an immune response so they will make their own antibodies (requires human intervention)
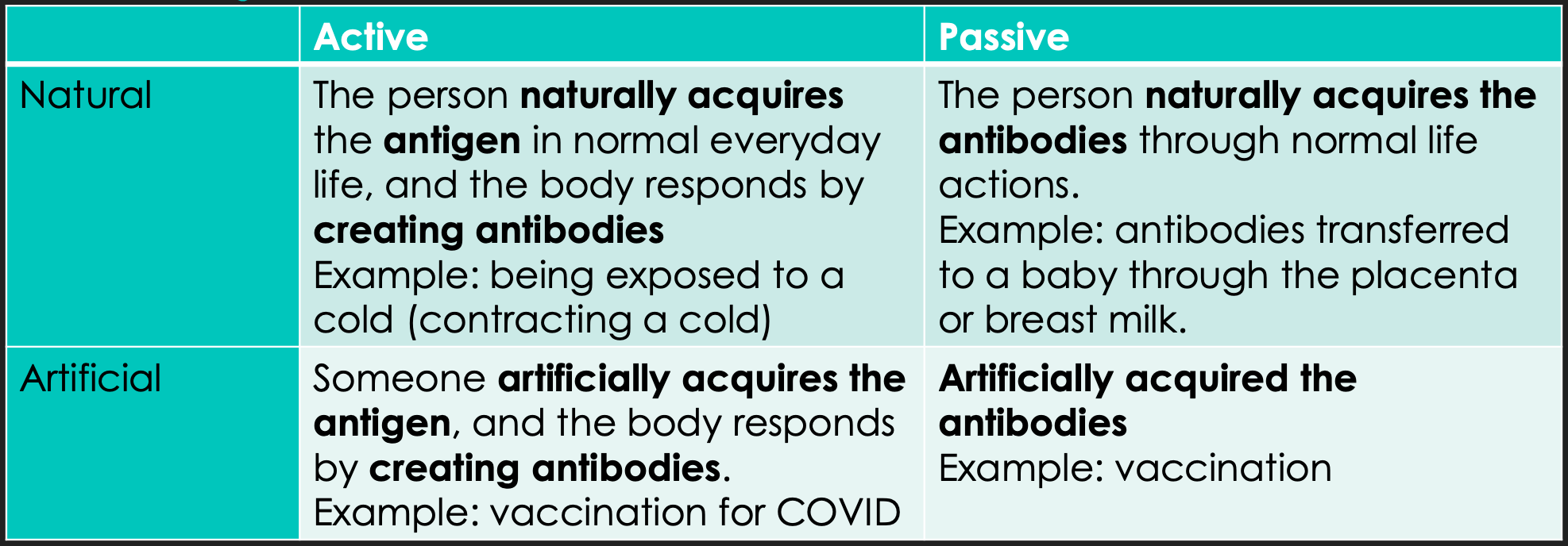
Types of Immunity- Passive vs Active
PASSIVE – person is given antibodies produced entirely by someone else; short-lived (lasts only as long as the antibodies are in the body); No memory cells produced- person’s own immune system is never activated= permanent immunity cannot occur + may get ill on subsequent exposures.
ACTIVE- results when the body is exposed to a foreign antigen + manufactures their own antibodies; long-term, due to the manufacture of memory cells, should a subsequent infection occur involving the same antigen, the appropriate antibodies can be produced very quickly→avoid the worst symptoms/may not develop any symptoms at all
Herd Immunity
Vaccinating a large enough proportion of the population to stop the transmission of a pathogen amongst the community.
By vaccinating enough individuals it:
Stops the chain of transmission
Does not give the pathogen a host so it can die out.
Types of Vaccines
Live attenuated- contain weakened micro-organisms (reduced virulence: reduced ability to produce disease symptoms) Eg. Polio, TB, MMR
Dead/inactivated micro-organism- not as long lasting. Eg. whooping cough
Toxoid - if bacteria/virus produces a toxin, toxin can be filtered + used as antigen in a vaccine to initiate immune response Eg. Tetanus
Sub-unit- Instead of using whole pathogen, fragment of microorganism used to provoke an immune response. Eg. HPV
Biosynthetic- Using recombinant DNA (mRNA): bacterial/viral DNA can be manipulated to become harmless. Eg. COVID-19
Vaccine delivery
Injections: using a syringe into the body
Oral: a syrup that is swallowed
Aerosol spray: nasal spray (for flu’s)
In development: Skin patches Food
Vaccination schedule
WHO has set a schedule to vaccinate infants; starts at 2 months old which gives enough time for a baby’s immune system to begin to develop.Then continues throughout childhood: 2, 4, 6, 12, 18 months etc.
timing of boosters after the initial vaccination are important:
Too soon: antibodies present in the blood will destroy the antigen
Too late: not enough memory cells are left for the booster to be effective
Risks of Vaccines
Most common side effects: Redness, swelling, heat & pain (all at injection site) Fever
Allergic reaction: Generally not from the vaccine but the medium they are cultured in.
Cross-species disease: not from the vaccine but the medium they are cultured in: animal tissue
Use of chemical preservatives- Concerns about health risks of chemicals, Side effects, Misinformation
Ethical concerns of Vaccines
Manufacturing:
vaccines require a host to be developed for viruses to reproduce- Chicken embryos/mice used to culture vaccines (Animal welfare)
Sometimes human tissue needs to be used, so cells initially created in the IVF process are used- people unhappy with origin of these cells
Testing of vaccines:
Before clinical trials: drugs are tested on animals
People who volunteer need to be well informed of risks. Often volunteers from underdeveloped nations w/ less education- concern they may not understand risks adequately/fairly.
Decisions:
Parents making decisions on behalf of their children – but risk of a side effect may affect the child for life
children too young to understand + make informed decisions
Antibiotics
A substance that kills or inhibits the growth of bacteria
Egs. Penicillin, Streptomycin, Cephalosporin
Can be broad spectrum/affect a wide range of bacteria or can narrow spectrum/effective only against specific types of bacteria
Bacteriostatic antibiotics inhibit growth of bacteria by interfering with protein synthesis
Bactericidal antibiotics destroy bacterial pathogens by targeting cell walls, cell membranes or metabolic pathways/action of enzymes found inside bacteria.
Antibiotic resistance (timing)
4 years for resistance to occur, more consideration before prescribing
Multiple drug resistant: resistant to many types of antibiotics.
prescribed antibiotics- advised to take full course (typically 10 days), even if feeling better earlier, as resistant bacteria survive the antibiotic treatment & reproduce to pass on the resistant trait= Reinfection + sickness occurs again
Natural selection:
Some bacteria may be more resistant to an antibiotic, therefore take longer to be killed.
Stopping the antibiotic early, means the bacteria with resistance, live & reproduce + go on to infect others with an antibiotic resistant strain of bacteria.
Antivirals
Viruses enter a host cell & the DNA or RNA induces the cell to produce new virus particles.
These particles leave the cell and infect others.
Scientists attempting to find viral proteins that that can be disabled.
Any drug that interferes with the replication process is likely to be toxic to the host cell.
many antiviral drugs available and more being developed
Hygiene Hypothesis
increased incidence of children w/ allergies (that can lead to greatly increased susceptibility to disease) is due to improved hygiene practices and living standard
less exposure to bacteria and virus
no immune response to pathogens triggered
decrease immunity for wide range infections (no natural immunity/memory cells)
increased chance of being infected
over-production of histamine—> allergies
Genetic engineering
the introduction of foreign/modified DNA into another cell
Uses:
identify mutated genes + replace faulty genes with healthy ones (therefore treat disorders like cancers)
Producing synthetic hormones: Insulin for Diabetics, hGH, Factor VIII for people with Haemophillia
Producing Vaccines
TRANSGENIC ORGANISMS
an organism whose genome has been altered by adding gene/genes from another organism.
introduced genes become part of the organisms DNA and can thus be passed on from one generation to the next
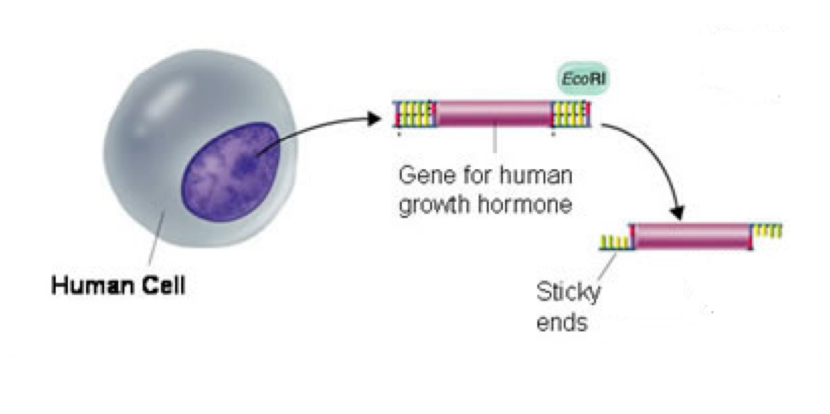
Enzymes within Genetic Engineering
RESTRICTION ENZYMES (in bacteria)- used to cut (viral) DNA at RECOGNITION SITE (specific sequence of bases), restricting duplication of viruses
DNA LIGASE – enzyme that can join or recombine separate pieces of DNA by forming bonds between last nucleotides in process called LIGATION
Straight vs Staggered Cuts
Some restriction enzymes produce a STRAIGHT CUT= produces BLUNT ENDS
Others produce STAGGERED CUTS= produce bits that overhang called STICKY ENDS
Sticky ends are useful because the single-stranded overhang can combine with any other fragment of DNA that has a complimentary ending - corresponding sequence (Including ones from different organisms)
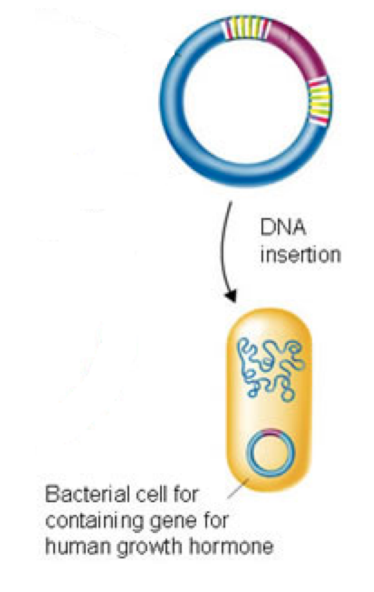
Producing organisms w/ recombinant DNA OVERVIEW
Isolate the gene
Insert gene into a plasmid (vector) and clone
Insert large quantities of the vectors into host cells to produce the foreign protein using instructions in the recombinant DNA
EG. Bacteria- the gene from insulin production has been introduced, are used to manufacture insulin for treatment of diabetes
Recombinant DNA- STEP 1
STEP 1 – Isolate Gene and cut using restriction enzyme
Isolate the gene of interest (stated in question)
Then use restriction enzymes to cut DNA on either side of required gene at restriction sites.
Recombinant DNA- STEP 2
STEP 2 – Isolate a plasmid and cut with same restriction enzyme
Cut the plasmid with the same restriction enzyme used in cutting the gene to be inserted
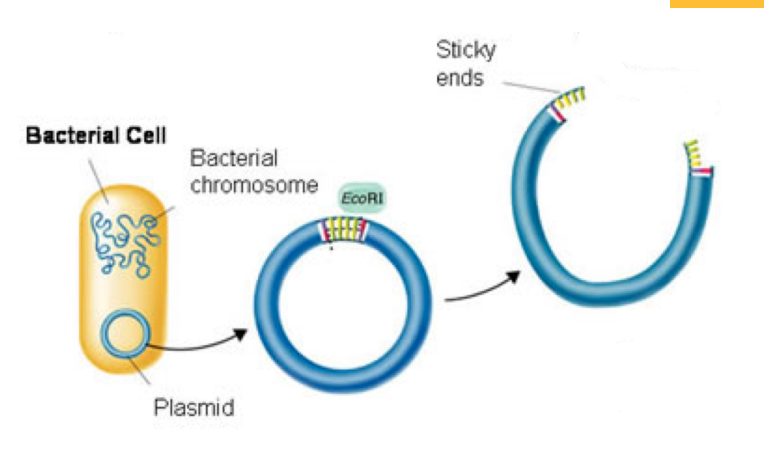
Vector + Plasmids
Vector- molecule of DNA that can transfer genetic material
undergoes replication
common vectors= bacterial plasmids (recombinant tech) & viral phages- virus that infects bacteria (gene therapy)
Plasmids= usually circular, double-stranded unit of cytoplasmic DNA, found in bacteria that are capable of replicating within a cell independent of chromosomal DNA (mitosis)
Recombinant DNA- STEP 3
STEP 3 – Splice the Human DNA into the Plasmid using DNA ligase
The sticky ends of the Human and Plasmid DNA anneal to each other and are spliced together by ligase
The gene foreign to the vector (ie. The human gene) is now referred to as RECOMBINANT DNA (it has recombined)
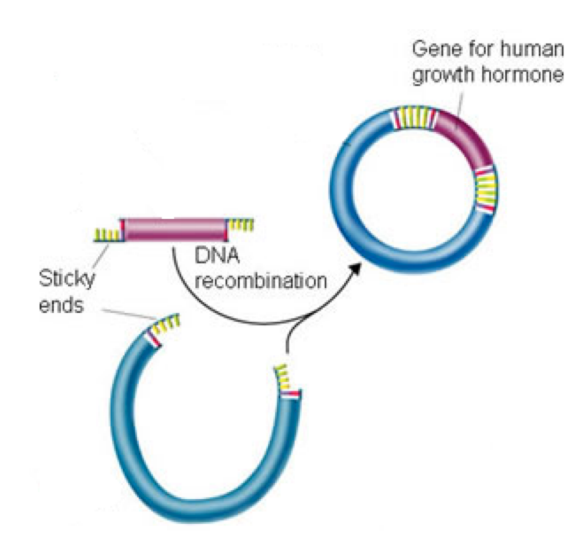
Recombinant DNA- STEP 4
STEP 4 – Bacteria takes up recombinant plasmid and then multiplies
Copies of the recombinant plasmid/vector are made
Copies are placed into host cells (ie. bacterial cells)
The host cells then produce the protein that the gene codes for