Lecture 14 - Secondary Lymphoid Organs
1/20
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
21 Terms
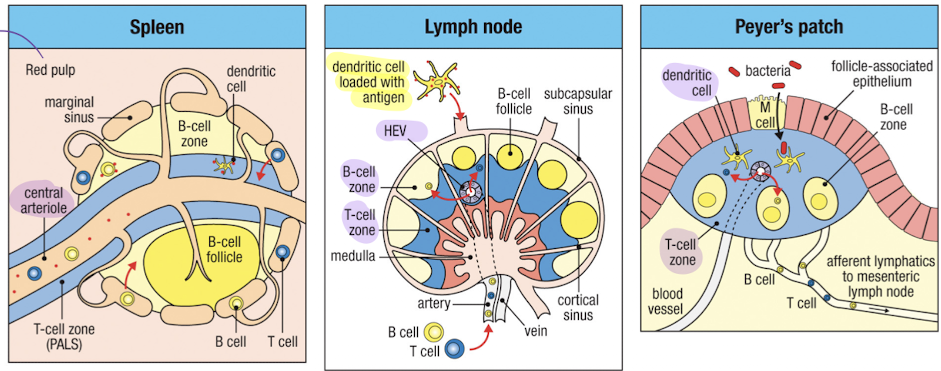
How do lymphocytes and antigens move in the spleen? What is the structure of the spleen?
marginal sinus separates red and white pulp
B cells, T cells, and Antigen enter through the marginal sinus
Macrophages and dendritic cells capture the antigen, and marginal zone b cells respond first
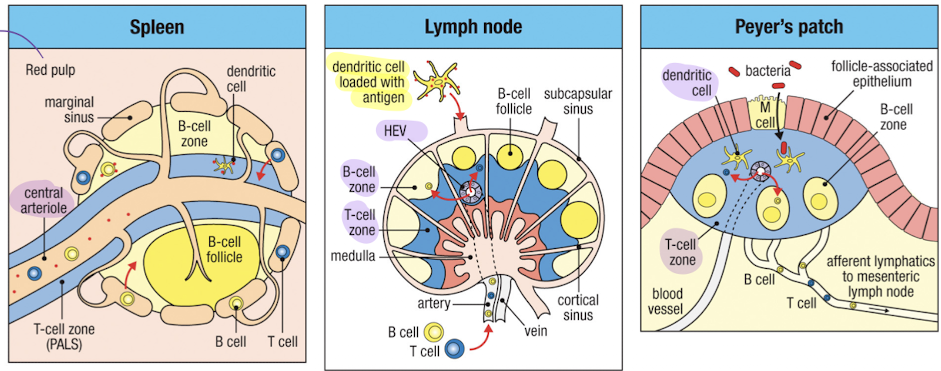
How do lymphocytes and antigens move in the lymph node? What is the structure of the lymph node?
B cells and T cells enter through high endothelial venules (HEVs)
Dendritic cells and antigen enter through afferent lymphatics
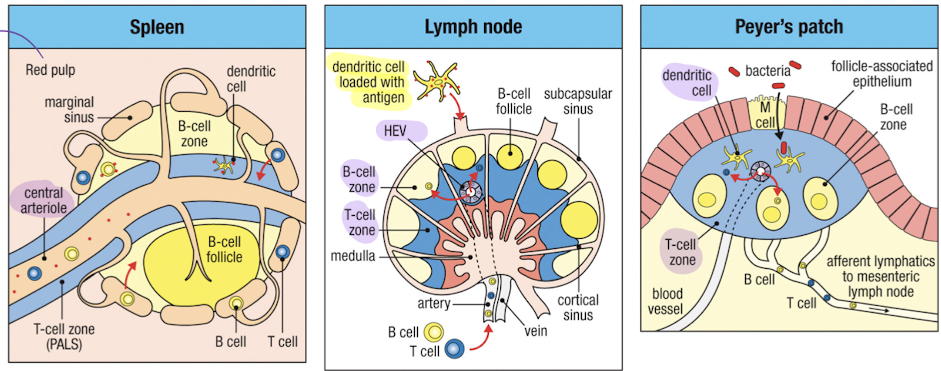
How do lymphocytes and antigens move in the peyer’s patch? What is the structure of the peyer’s patch?
peyer’s patch is part of MALT - mucosa associated lymphoid tissue
antigen enters through M cells, B and T cells enter through blood vessels
afferent lymphatics drain to mesenteric lymph nodes
What is lymph node development initiated by?
lymphoid tissue inducer cells (LTi)
How does the lymphocyte enter the lymph node?
similarly to how neutrophils enter inflamed tissue
lymphocyte enters a high endothelial venule
binding of L-selectin (on lymphocyte) to GlyCAM-1 and CD34 (on endothelial cell) allows for rolling
LFA-1 is activated by CCR7 signaling in response to CCL21 or CCL19 bound to endothelial surface
activated LFA-1 binds to ICAM-1
lymphocyte crosses endothelium and enters LN via diapedesis
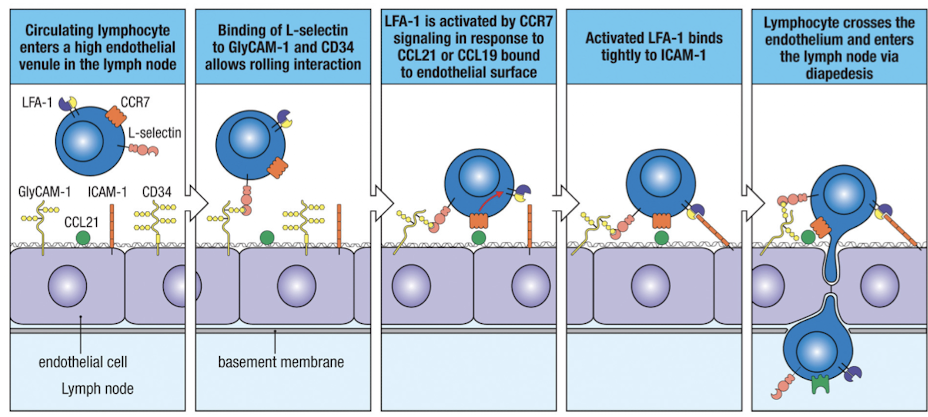
How do selectins help lymphocyte entry?
selectins guide leukocytes to particular tissues
L-selectin (CD62L) binds to sugar groups (Sialyl-Lewisx) on vascular addressins (CD34,GlyCAM-1) on HEVs
L -selectin promotes entry into spleen or mucosal epithelium via binding to MadCAM01
weak interactions, permits rolling
How do integrins help lymphocyte entry?
intergrin heterodimers interact with ligands on endothelium of APCs
LFA-1 helps T cells stick to HEVs and enables interaction of T cells with their targets
α4β7 promotes entry to spleen or mucosal endothelium via binding to MadCAM-1
What is CCR7, and what does it’s signaling promote?
CCR7 - chemokine receptor
CCR7 signaling promotes conformational change to the high affinity form of LFA-1 and LFA-1 clustering
CCL19/21 bind to CCR7 → association with a G protein
G protein dissociation → activation of Rap1
Activates Rap1 induces LFA-1 aggregation
What are FRCs and what are their purpose?
FRC - fibroblastic reticular cell; those in T cell zone facilitate interactions of T cells and dendritic cells
FRCs make conduits
CCL19/21 are present on surface of FRC network
DCs and T cells express CCR7, attracted to/crawl on FRC
free antigen enters via afferent lymphatics, collected by DCs for presentation to T cells
FDCs in follicles make CXCL13 which attracts B cells, expressing CXCR5
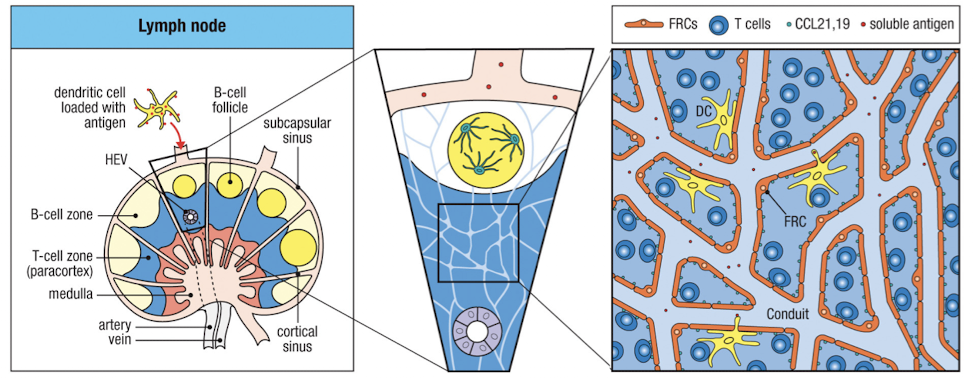
How do Naive T cells become activated in the lymph nodes?
Naive T cells enter LN through HEV in paracortex
DCs presenting antigen localize to the paracortex, interacting with CD4 and CD8 T cells there
T cells that aren’t activated drain back into the lymph through cortical sinuses to efferent lymphatics within hours
while in the LN, non activated T cells receive survival signals through self-peptide:MHC complexes and IL-7
If a T cell recognizes the Ag presented by a DC, it stops migration and begins to proliferate within the LN (clonal expansion, new cells with identical antigen specificity)
once a T cell has proliferated for a few days, it acquires effector functions and the ability to leave the LN via cortical sinus
Time stamps of T cell activation
10 hrs after T cell entry, long lasting contact with DCs occurs
Proliferation starts at 2 days
in 2 days, all antigen specific T cells are trapped in the draining LN
within 5-6 days, T cells emigrate to the periphery to carry out effector functions
only 1 in 10^5-10^6 T cels recognize a given peptide
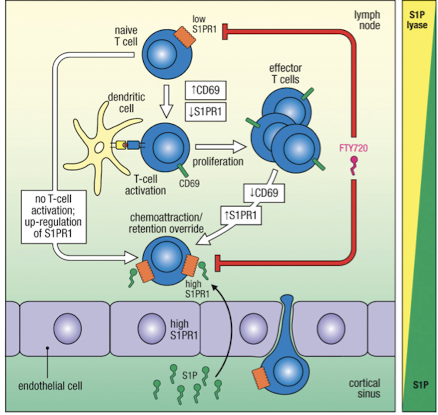
How does egression from LN follow a chemical gradient via GPCR signaling?
S1P (ligand) has high concentrations in lymph and blood, but scarce in LN due to S1P lyase
S1PR1 (receptor) is low on naive T cells when entering LN because receptor is downregulated by binding S1P in circulation
if T cell is not activated, S1PR1 increases and cell leaves through cortical sinus
S1PR1 is downregulated on T cells for several days after T cell activation, allowing cells to stay in LN
S1PR1 is upregulated as stimulation stops to promote egress
What are the 3 professional antigen presenting cells (APCs)
dendritic cells
macrophages
B cells
they are professional because they express MHCII and co stimulatory molecules B7.1 and B7.2
dendritic cells
perform macropinocytosis and phagocytosis
Low MHC when immature, high MHC in lymphoid tissues
ubiquitous throughout body
results in activation of naive T cells
Macrophages
perform macropinocytosis and phagocytosis
MHC inducible by bacteria and cytokines
found in lymphoid tissue, connective tissue, and body cavities
results in activation of macrophages by effector and memory T cells
B cells
perform antigen specific receptor mediated endocytosis
MHC constitutive
found in lymphoid tissue (follicle) and peripheral blood
results in delivery of help to B cell by T cells
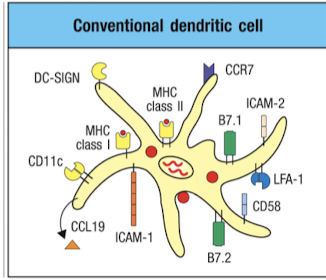
Conventional Dendritic cells
activate Naive T cells
matue cDCs express many molecules to aid in T cell activation
multiple types
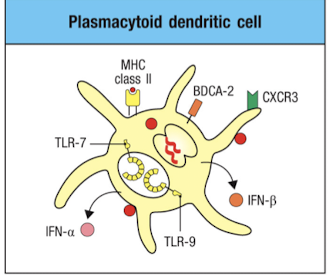
Plasmacytoid dendritic cells
respond to viral infection by secreting large amounts of type I interferons
dont stimulate naive T cells
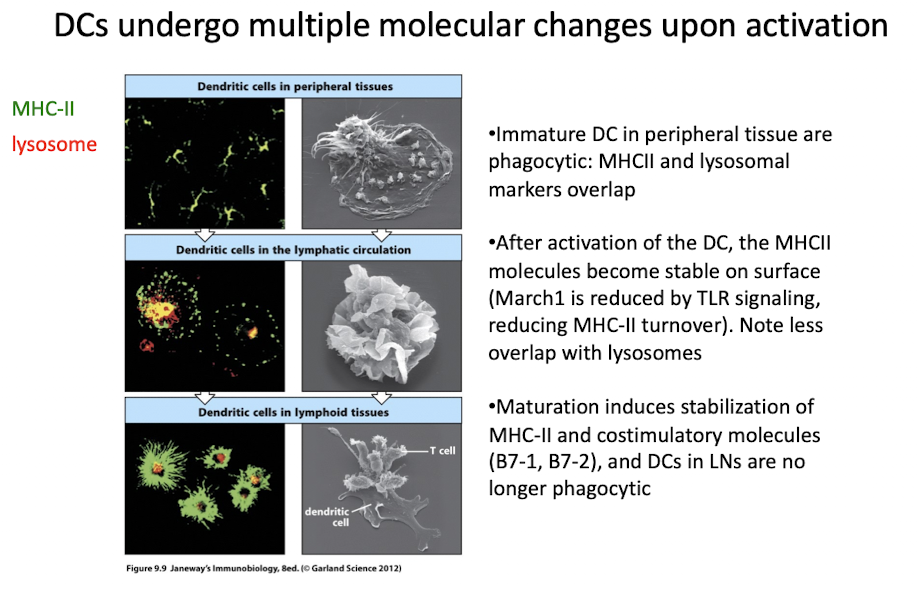
How do Resting DCs change properties to activate T cells
when DCs encounter pathogens, PRRs are triggered
TLRs (except TLR8) are expressed, DEC205 enables phagocytosis, etc
activated DCs become licensed to activate T cells
CCR7 expression = LN migration
PRR signaling enhances antigen processing
In lymph node mature DCs are no longer phagocytic
they ugregulate MHC-I, B7.1, B7.2, adhesion molecules, and stabilize MHC-II on cell surface
mature DCs interact with T cells in paracortex
enter the LN through afferent lymphatics, dump directly to T zones through marginal sinus
DC are versatile in their ability to uptake/process pathogens
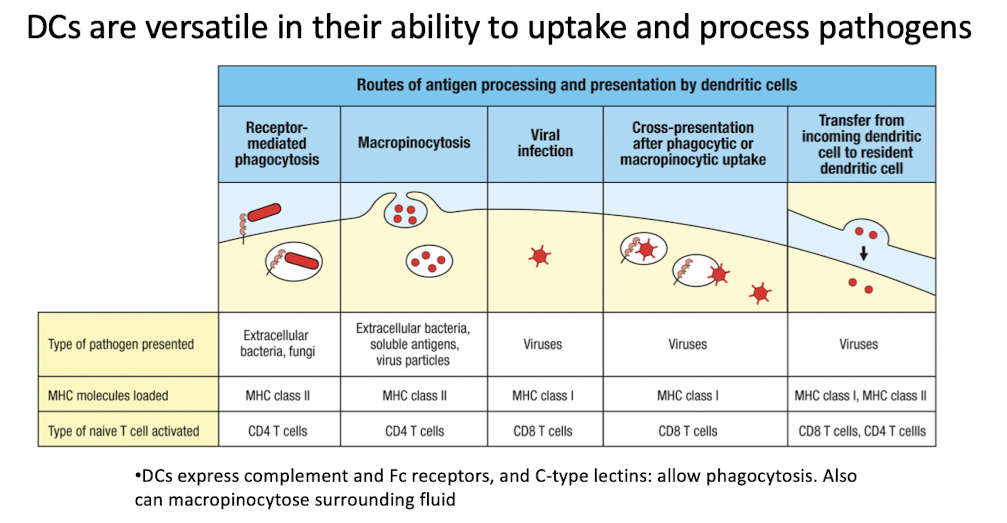
DCs migrating to LN can prime T cells directly or transfer Ag to resident DC
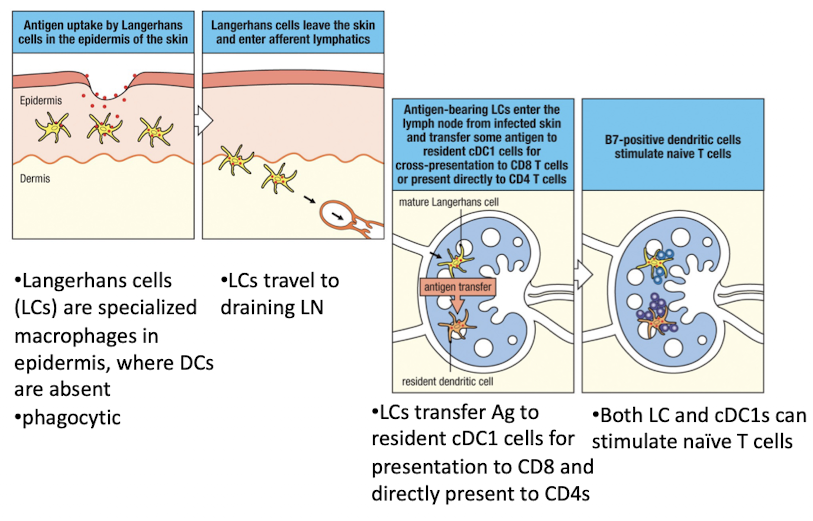
Langerhans cells are specialized macrophages in epidermis where DCs are absent
LCs travel to draining lymph nodes and trandfer Ag to cDC1 cells for presentation to CD8 and directly present to CD4s
both LC and cDC1s can stimulate naive T cells