ch 21 pt 2 immune system
1/125
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
126 Terms
what does the adaptive immune system do?
– Protects against infectious agents and
abnormal body cells
– increase inflammatory response
– Must be primed by initial exposure to specific foreign substance which takes time
Adaptive Defenses:specific
recognizes and targets specific antigens
Adaptive Defenses:Systemic
not restricted to initial site(any particular organ or tissue)
Adaptive Defenses:Have memory
Each activation will create memory cells to remember the antigen, which create stronger attacks to "known" antigens
Adaptive Defenses: Improvement
response strengthens on next exposure
Adaptive Defenses: Two overlapping components
– Humoral (antibody-mediated) immunity(B CELLS)
– Cellular (cell-mediated) immunity(T CELLS)
Humoral Immunity
Antibodies produced by lymphocytes,
circulating freely in body fluidsAntibodies bind temporarily To target cell
mark the cell for phagocytes
Humoral immunity has
extracellular targets(going after pathogens that havent made it to a host cell yet)
Cellular Immunity:Lymphocytes act against target cell in 2 ways
Directly – by killing infected cells
Indirectly – by releasing chemicals that enhance inflammatory response; or activating other lymphocytes or macrophages
Cellular immunity has
Cellular targets(virally infected cells)
Antigens
Substances that can activate adaptive defenses and provoke an immune
response
they are the targets of all adaptive immune responses
Most are large, complex molecules not normally found in body (nonself)
Complete Antigens:Important functional properties
Immunogenicity: ability to stimulate
a rapid increase of specific lymphocytes(once activated, it initiates reactivity)Reactivity: ability to react with activated lymphocytes and antibodies released by immunogenic reactions
Examples: non self proteins or peptides
Haptens (Incomplete Antigens)
Not immunogenic(being able to produce an immune response) by themselves
May be immunogenic if attached to body protein and no longer recognized to cell
Cause immune system to mount harmful attack against unsually non-harmful substances
• Examples: poison ivy, animal dander,
detergents, and cosmetics
Antigenic Determinants
• Only certain parts (antigenic
determinants) of entire antigen are
immunogenic
• Antibodies and lymphocyte receptors bind
to them as enzyme binds substrate
Antigenic Determinants: Most naturally occurring antigens have numerous antigenic determinants that
Mobilize several different lymphocyte
populationsForm different kinds of antibodies against them
Self-antigens: MHC Proteins
marks our cells as belonging so our immune system doesnt attack them
Protein molecules (self-antigens) on
surface of cells not antigenic to self but antigenic to others in transfusions or grafts
• Example: MHC glycoproteins
Cells of the Adaptive Immune System:Three types of cells
– Two types of lymphocytes
• B lymphocytes (B cells)—humoral immunity
• T lymphocytes (T cells)—cellular immunity
– Antigen-presenting cells (APCs)
• Do not respond to specific antigens
• Play essential auxiliary roles in immunity
– Two types of lymphocytes
• B lymphocytes (B cells)—humoral immunity
• T lymphocytes (T cells)—cellular immunity
– Antigen-presenting cells (APCs)
• Do not respond to specific antigens
• Play essential auxiliary roles in immunity
Lymphocyte Development, Maturation, and
Activation: 5 steps
– Origin – all originate in red bone marrow
– Maturation
– Seeding secondary lymphoid organs and circulation
– Antigen encounter and activation
– Proliferation and differentiation
lymphocyte development, maturation, and activation. step 1
Origin
• Both B and T lymphocyte precursors originate in red bone marrow
lymphocyte development, maturation, and activation. step 2
Maturation
Lymphocyte precursors destined to become T cells migrate (in blood) to the thymus and mature there.
B cells mature in the bone marrow.
During maturation lymphocytes develop immunocompetence
and self-tolerance.
lymphocyte development, maturation, and activation. step 3
Seeding secondary lymphoid organs and circulation
• Immunocompetent lymphocytes leave the thymus and bone marrow.
• They “seed” the secondary lymphoid organs and circulate through blood and lymph.
lymphocyte development, maturation, and activation. step 4
Antigen encounter and activation
• When a lymphocyte’s antigen receptors bind its antigen, that lymphocyte can be activated.
lymphocyte development, maturation, and activation. step 5
Proliferation and differentiation
• Activated lymphocytes multiply and then
differentiate into effector cells and memory cells.
• Memory cells and effector T cells circulate continuously in the blood and lymph and secondary lymphoid organs
Maturation
"Educated" to become mature; B cells in
bone marrow, T cells in thymus
– Immunocompetence
lymphocyte can recognize one specific antigen by binding to it
• B or T cells display only one unique type of antigen receptor on surface when achieve maturity – bind only one antigen
Self-tolerance
• Lymphocytes unresponsive to own antigens
T cells
mature in thymus under negative
and positive selection pressures
T cell– Positive selection
• Selects T cells capable of recognizing self-MHC proteins (MHC restriction); failures destroyed by apoptosis(death by cell suicide).
T cells– Negative selection
• T cells must not recognize self-antigens. Recognizing self-antigen results in apoptosis(death by cell suicide). This eliminates self-reactive T cells that could cause
autoimmune diseases
• Ensures self-tolerance
B cells
• B cells mature in red bone marrow
• Positively selected if successfully make
antigen receptors
• Those that are self-reactive
– Eliminated by apoptosis
Seeding Secondary Lymphoid Organs and
Circulation
• Immunocompetent B and T cells not yet
exposed to antigen
• Exported from bone marrow and thymus to "seed" lymph nodes, spleen, etc.
– Increases chance of encounter with antigen
Antigen Encounter and Activation: Clonal selection
– Naive lymphocyte's first encounter with
antigen → selected for further development
– If correct signals present, lymphocyte will
complete its differentiation
Proliferation and Differentiation
• Activated lymphocyte proliferates(increase rapidly) → exact clones
• Most clones → effector cells that fight
infections
• Few remain as memory cells
- Able to respond to same antigen more quickly
second time
• B and T memory cells and effector T cells
circulate continuously
B cells: type of immune response
Humoral
B cells:antibody secretion
yes
B cells:primary targets
extracellular pathogens:bacteria, fungi, parasites, some viruses in extracellular fluid
B cells: site of origin
red bone marrow
B cells site of maturation:
red bone marrow
B cells: effector cells
plasma cells
B cell: memory cell formation
yes
T cells:type of immune response
Cellular
T cells: antibody secretion
no
T cells:Primary targets
intracellular pathogens(virus infected cells) and cancer cells
T cells:site of origin
red bone marrow
T cells: site of maturation
thymus
T cells:effector cells
cytotoxic T cells
Helper t cells
regulatory T cells
T cells:memory cell formation
yes
Antigen-presenting Cells (APCs)
• Engulf antigens
• Present fragments of antigens to T cells
for recognition
Antigen-presenting Cells (APCs) Major types
– Dendritic cells in connective tissues and
epidermis
– Macrophages in connective tissues and
lymphoid organs
– B cells
APCs: Dendritic Cells and Macrophages
• Dendritic cells phagocytize pathogens,
enter lymphatics to present antigens to T
cells in lymph node
• Macrophages widespread in lymphoid
organs and connective tissues
APCs: B Lymphocytes
• Do not activate naive T cells
• Present antigens to helper T cell to assist
own activation
Adaptive Immunity: Summary
• Uses lymphocytes, APCs, and specific
molecules to identify and destroy nonself
substances
• Depends upon ability of its cells to
– Recognize antigens by binding to them
– Communicate with one another so that whole
system mounts specific response
Activation and Differentiation of B Cells
• B cell activated when antigens bind to its
surface receptors and cross-link them →
• Receptor-mediated endocytosis of cross-
linked antigen-receptor complexes (clonal
selection) →
• Proliferation and differentiation into effector cells
Fate of the Clones
• Most clone cells become plasma cells
– Secrete specific antibodies at rate of 2000
molecules per second for four to five days,
then die
Fate of the Clones: Clone cells that do not become plasma cells become
Memory cells
– Provide immunological memory
– Mount an immediate response to future
exposures to same antigen
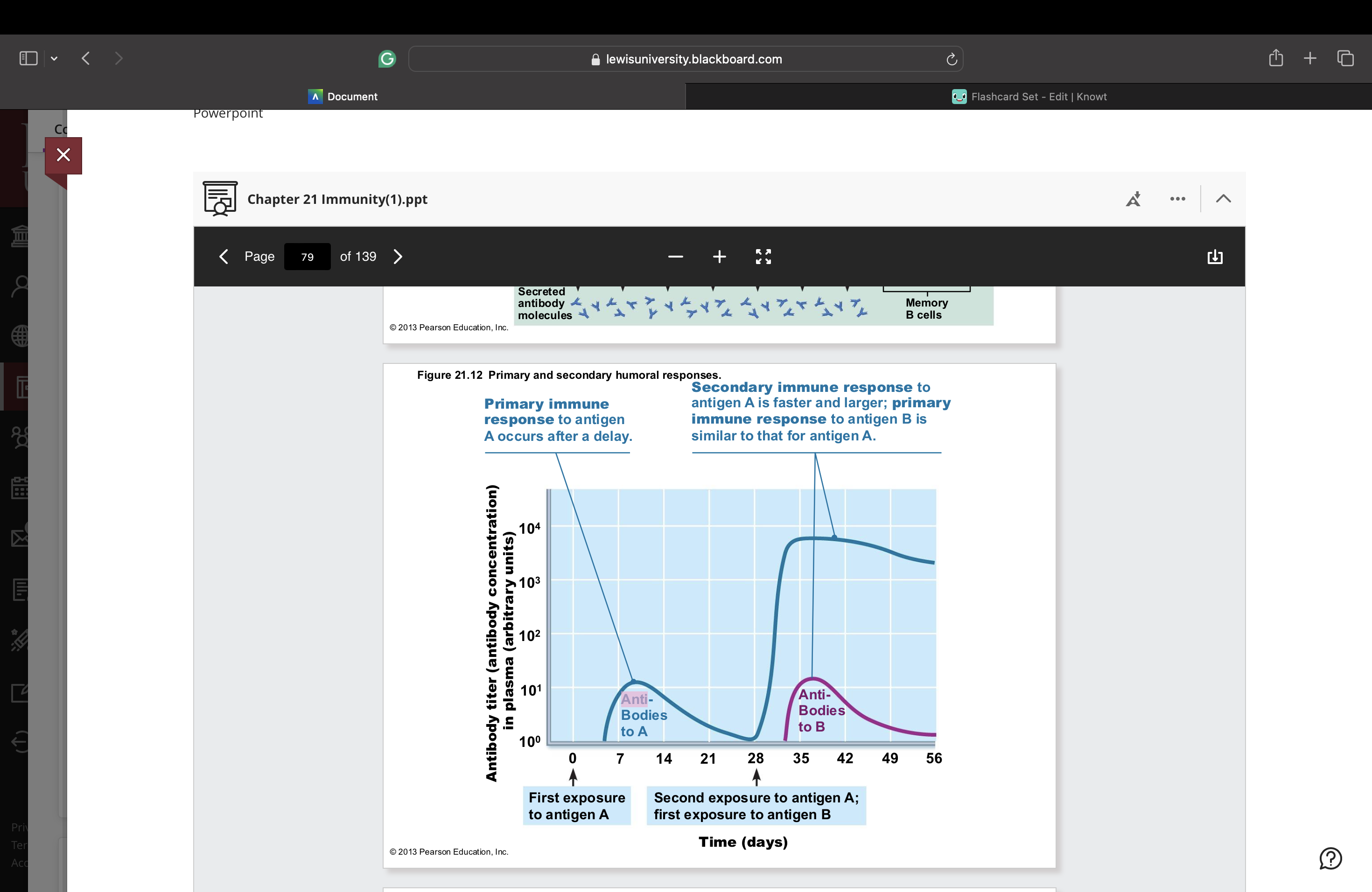
Immunological Memory: Primary immune response
– Cell proliferation and differentiation upon first
antigen exposure
– Lag period: three to six days
– Peak levels of plasma antibody are reached in
10 days
– Antibody levels then decline
Immunological Memory:Secondary immune response
– Re-exposure to same antigen gives faster,
more prolonged, more effective response
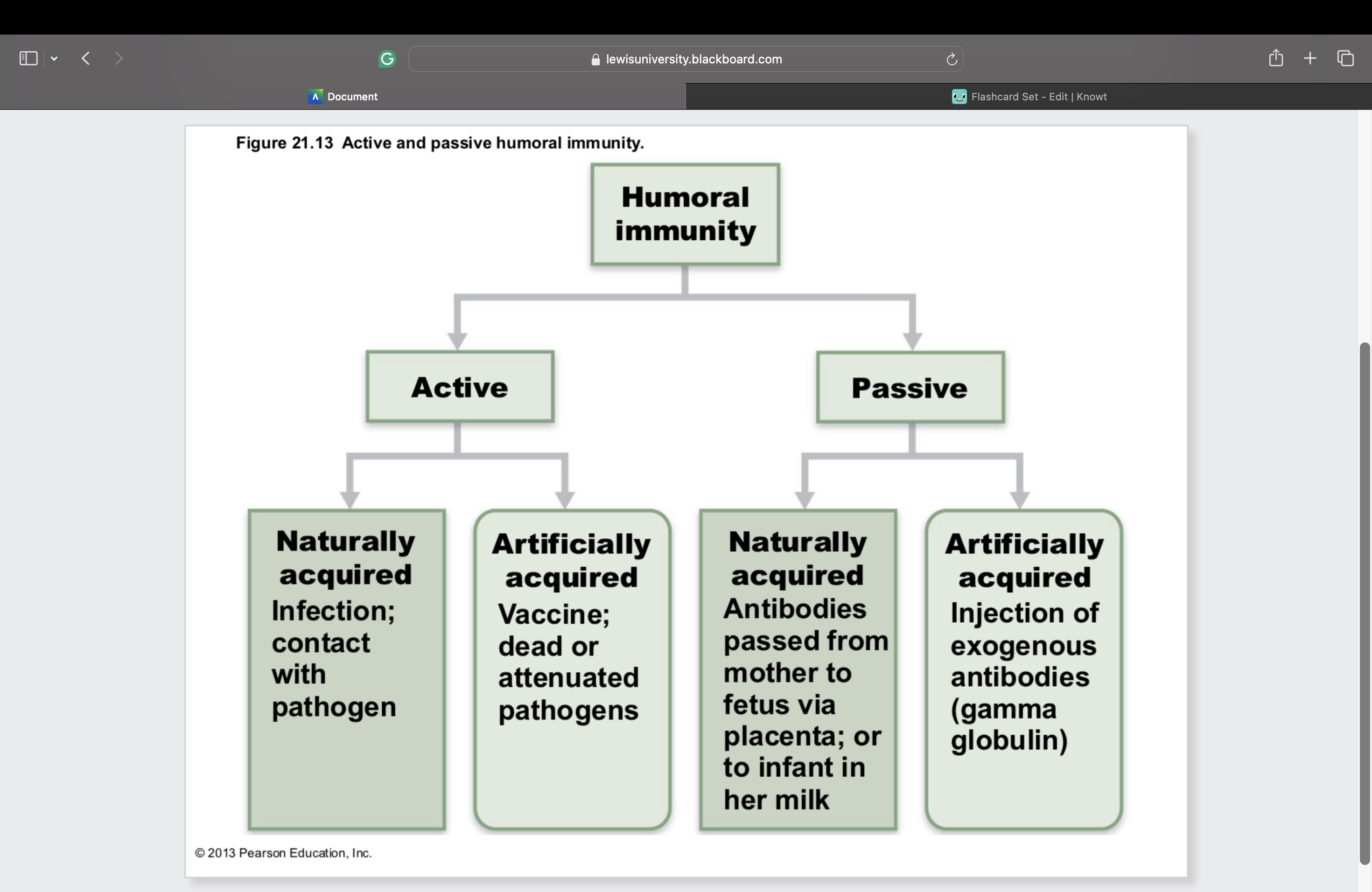
Active Humoral Immunity
When B cells encounter antigens and
produce specific antibodies against them
Two types of active humoral immunity:
– Naturally acquired—response to bacterial or
viral infection
– Artificially acquired—response to vaccine of
dead or reduced force(not as strong as the initial pathogen) pathogens
Active Humoral Immunity: Vaccines
– Most of dead or attenuated pathogens
– Spare us the symptoms of primary response
– Provide antigenic determinants that are
immunogenic and reactive
Passive Humoral Immunity
• Readymade antibodies introduced into
body
• Immunological memory does not occur
• Protection ends when antibodies degrade
Passive Humoral Immunity: Two types
1. Naturally acquired—antibodies delivered to
fetus via placenta or to infant through milk
2. Artificially acquired—injection of serum,
such as gamma globulin
Antibodies
• Immunoglobulins—gamma globulin portion
of blood
• Proteins secreted by plasma cells
• binding specifically with antigen detected by B cells
Basic Antibody Structure
• T- or Y-shaped antibody monomer of four
looping polypeptide chains
• Two identical heavy (H) chains
• Two identical light (L) chains
• Variable (V) regions at one end of each
arm combine to form two identical
antigen-binding sites
Classes of Antibodies: IgM
– Pentamer (larger than others); first antibody
released
– Potent agglutinating agent
– Readily fixes and activates complement
Classes of Antibodies: IgD
– Monomer attached to surface of B cells
– Functions as B cell receptor
Classes of Antibodies:IgA (secretory IgA)
– Monomer or dimer; in mucus and other
secretions
– Helps prevent entry of pathogens
Classes of Antibodies:IgG
– Monomer; 75–85% of antibodies in plasma
– From secondary and late primary responses
Classes of Antibodies: IgE
– Monomer active in some allergies and
parasitic infections
– Causes mast cells and basophils to release
histamin
Antibodies inactivate and tag
antigens; do not destroy them
– Form antigen-antibody (immune)
complexes
Defensive mechanisms used by antibodies
– Neutralization and agglutination (the two most
important)
– Precipitation and complement fixation
Neutralization
Simplest defensive mechanism
• Antibodies block specific sites on viruses
or bacterial toxins
• Prevent these antigens from binding to
receptors on tissue cells
• Antigen-antibody complexes undergo
phagocytosis(ingestion of bacteria)
Agglutination
• Antibodies bind same determinant on
more than one cell-bound antigen
• Cross-linked antigen-antibody complexes
agglutinate(combine)
– Example: clumping of mismatched blood cells
Precipitation
• Soluble molecules are cross-linked
• Complexes precipitate and are subject to
phagocytosis
Complement Fixation and Activation
• Main antibody defense against cellular
antigens (bacteria, mismatched RBCs)
Summary of Antibody Actions
• Antigen-antibody complexes do not
destroy antigens; prepare them for
destruction by innate defenses
• Antibodies do not invade solid tissue
unless lesion present
• Can act intracellularly if attached to virus
before it enters cell
Cellular Immune Response
• T cells provide defense against
intracellular antigens
• Some T cells directly kill cells; others
release chemicals that regulate immune
response
• Two populations of T cells based on which
glycoprotein surface receptors displayed
– CD4 cells usually become helper T cells (TH);
activate B cells, other T cells, macrophages,
and direct adaptive immune response
• Some become regulatory T cells – which
moderate immune response
– Can also become memory T cells
Cellular Immune Response
– CD8 cells become
cytotoxic T cells (TC)
• Destroy cells harboring foreign antigens
• Also become memory T cells
– Helper, cytotoxic, and regulatory T cells are
activated T cells
– Naive T cells simply termed CD4 or CD8 cells
MHC Proteins and Antigen Presentation
• T cells respond only to processed
fragments of antigens displayed on
surfaces of cells
• Antigen presentation vital for activation of
naive T cells and normal functioning of
effector T cells
MHC Proteins:Two types of MHC proteins important to T cell activation
– Class I MHC proteins – displayed by all
nucleated cells except RBCs
– Class II MHC proteins – displayed by APCs
(dendritic cells, macrophages, and B cells)
• Both types are synthesized at ER and bind
to peptide fragments
Class I MHC Proteins
• Bind with fragment of protein synthesized in the cell
• Endogenous antigen is self-antigen in normal
cell; a nonself antigen in infected or abnormal
cell
• Inform cytotoxic T cells of microorganisms hiding in cells (cytotoxic T cells ignore displayed self-antigens)
• Act as antigen holders; form "self" part that T
cells recognize
Class II MHC Proteins
• Bind with fragments of exogenous
antigens that have been engulfed and
broken down in a phagolysosome
• Recognized by helper T cells
• Signal CD4 cells that help is required
MHC Restriction
• CD4 and CD8 cells have different
requirements for MHC protein that
presents antigens to them
CD4 and CD8 cells have different
requirements for MHC protein that
presents antigens to them
– CD4 cells that become TH – bind only class II
MHC proteins typically on APC surfaces
– CD8 cells that become cytotoxic T cells – bind
only class I MHC proteins on APC surface
• CD8 cells activated by class I MHC
proteins
T cell Activation: two-step process
– Antigen binding (MCH and TCR and CD
protien)
– Co-stimulation
– Antigen binding (MCH and TCR and CD
protien)
– Co-stimulation
• Both occur on surface of same APC
• Both required for clonal selection
T cell Activation: Co-stimulation
Without co-stimulation, anergy occurs
– T cells
• Become tolerant to that antigen
• Are unable to divide
• Do not secrete cytokines
T cell Activation: Proliferation and
Differentiationd
T cells that are activate
– Enlarge and proliferate in response to
cytokines
– Differentiate and perform functions according
to their T cell classPrimary T cell response peaks within a week
T cell apoptosis occurs between days 7 and 30
– Benefit of apoptosis: activated T cells are a hazard –
produce large amount inflammatory cytokines →
hyperplasia, cancerEffector activity wanes as amount of antigen
declinesMemory T cells remain and mediate secondary
responses
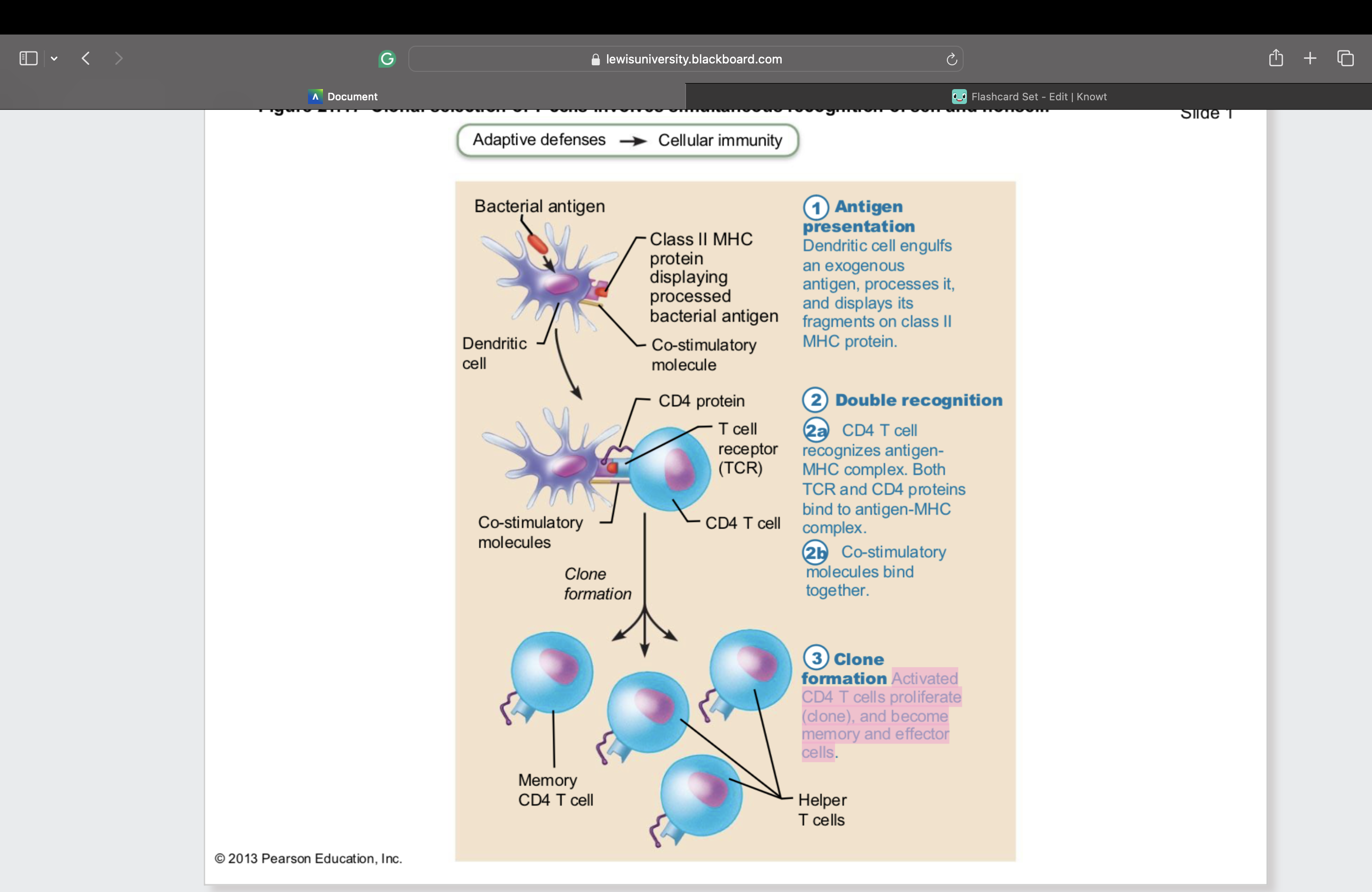
Clonal selection of T cells involves simultaneous recognition of self and nonself
Antigen
presentation
Dendritic cell engulfs
an exogenous
antigen, processes it,
and displays its
fragments on class II
MHC proteinDouble recognition
2a. CD4 T cell
recognizes antigen-
MHC complex. Both
TCR and CD4 proteins
bind to antigen-MHC
complex.
2b. Co-stimulatory
molecules bind
together.clone formation Activated
CD4 T cells proliferate
(clone), and become
memory and effector
cells
Roles of Helper T (TH) cells
adaptive immune response
• Help activate T and B cells
• Induce T and B cell proliferation
• Their cytokines recruit other immune cells
• Without TH, there is no immune
response
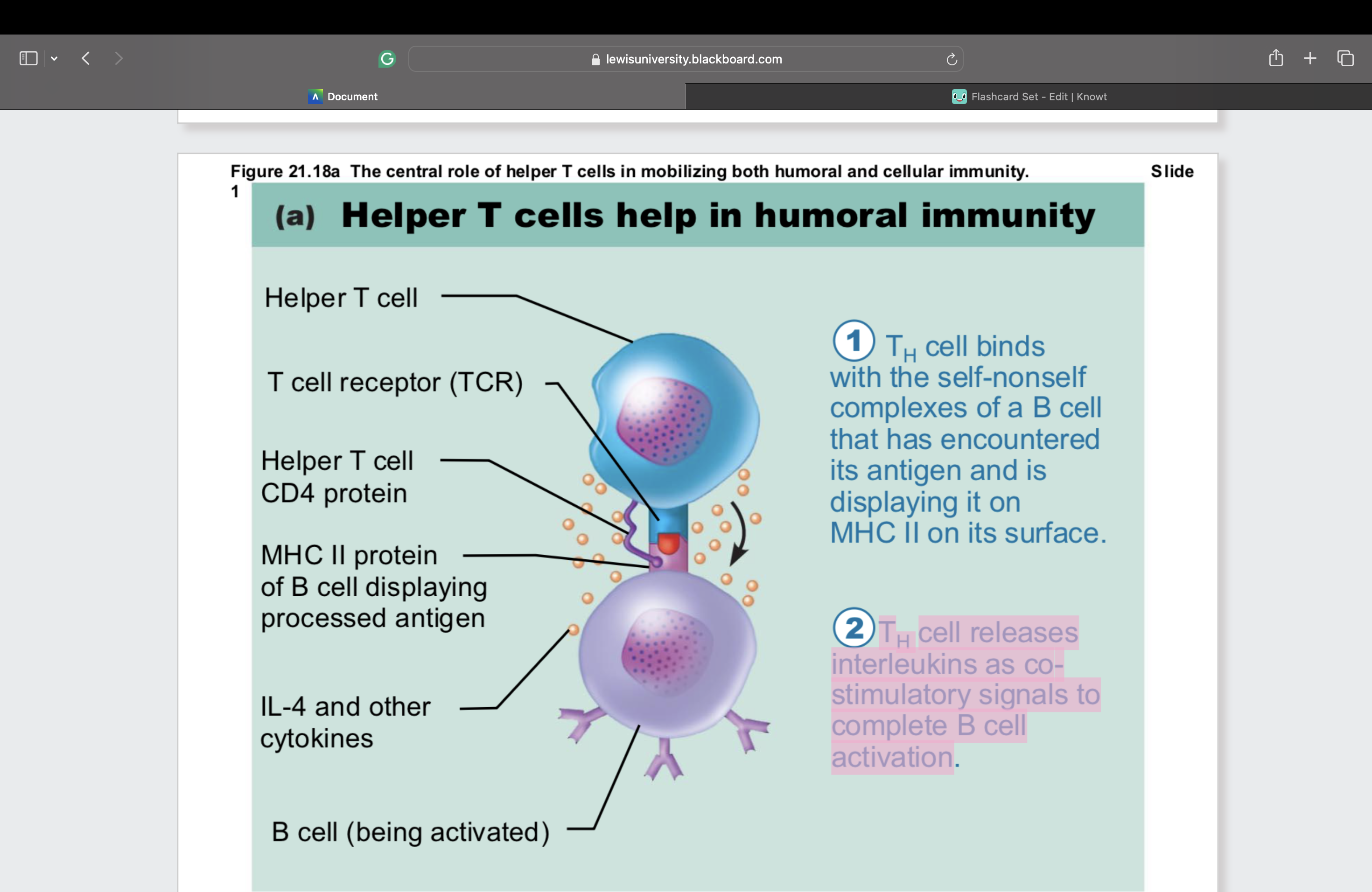
Helper T cells: Activation of B cells
• Interact directly with B cells displaying antigen
fragments bound to MHC II receptors
• Stimulate B cells to divide more rapidly and
begin antibody formation
B cells may be activated without TH cells by
binding to
T cell–independent antigens
– Response weak and short-lived
Most antigens require TH co-stimulation to
activate B cells:
T cell–dependent antigens
Helper T cells help in humoral immunity
TH cell binds with the self-nonself
complexes of a B cell that has encountered its antigen and is
displaying it on MHC II on its surfaceTH cell releases interleukins as co-
stimulatory signals to complete B cell
activation
Helper T cells: Activation of CD8 cells
• CD8 cells require TH cell activation into
destructive cytotoxic T cells
• Cause dendritic cells to express co-
stimulatory molecules required for CD8
cell activation