SAM Exam 6 - Respiratory
1/32
Earn XP
Description and Tags
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
33 Terms
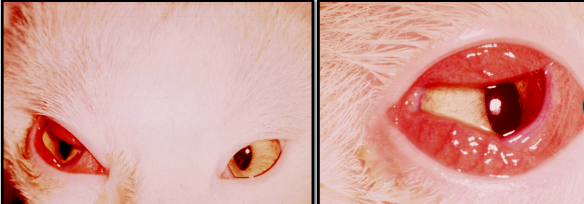
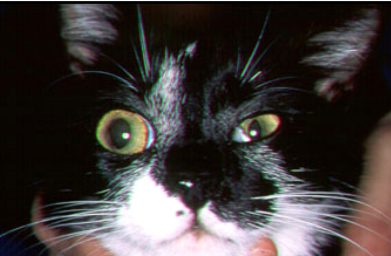
Feline Upper Respiratory Infection
Et: FHV, FVR, FCV, Chlamydophila, Bordetella, Mycoplasma
Cs: Inappetence, lethargy, fever, Sneezing, coughing, Nasal/ocular discharge
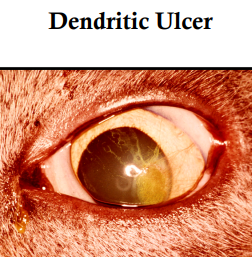
FCV: Oral/nasal ulcers, viral pneumonia
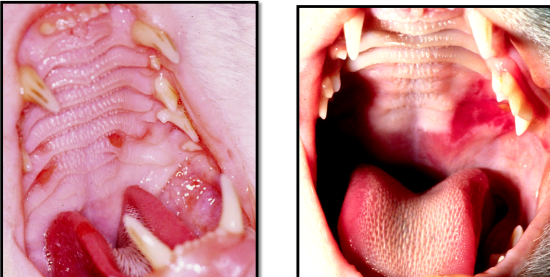
FHV: Conjunctivitis, corneal ulcers
Nasal Turbinate Damage
Chlamydophila felis: Chronic Conjunctivitis
Dt: Not routinely needed, Ab/VI tests
Tx: Self limiting, Antibiotics (cillin/cycline/mycin), Antivirals (-uridine), omega/alpha-2b interferon
Lysine is ineffective
Vax: FVRCP: improves CS only, 8 & 14 weeks, yearly, q 3y
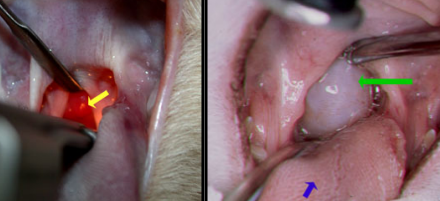
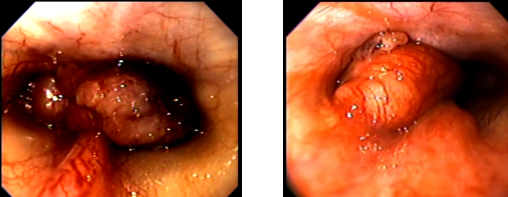
Nasopharyngeal Polyps
Young Cat issues
originate from eustachian tube
Et: Benign growths in young cats
may extend to ear canal, middle ear, pharynx, nasal cavity
Cs: Stertorous breathing, upper airway obstruction, Serous/mucopurulent nasal discharge, Otitis, Head tilt, nystagmus, Horner’s syndrome
Dt: rads/scope, otoscopy, CT, PE/visual, histopath (definitive)
Tx: Removal (Traction avulsion, Ventral bullae osteotomy)
+/- Transient Horner’s Syndrome


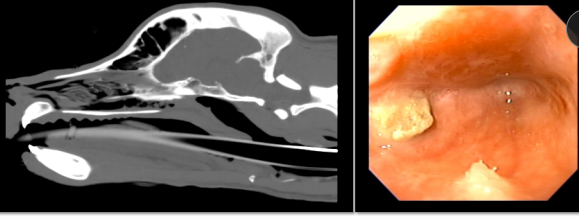
Nasal Tumors
Et: Malignant, older, Dolichocephalic breeds
Dogs:adenocarcinoma, carcinoma, fibrosarcoma, CATS: chondrosarcoma, lymphoma, SCC
Cs: Chronic nasal discharge (#1), Sneezing, Facial deformity, Neuro abnormalities, stertor
Often unilateral → progresses to bilateral
Dt: rads, rhinoscope(retroflexed), CT, PE, histopath (definitive)
Mets: to reginal lymph nodes
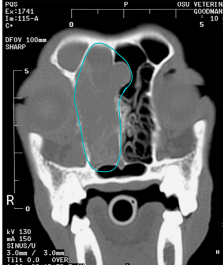
Tx: Sx(not an option), radiation, chemo(lymphoma), NSAIDS, pain meds
Poor prognosis


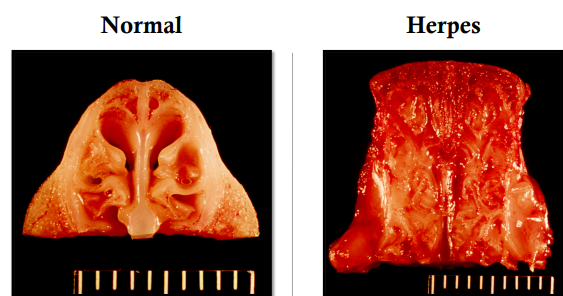
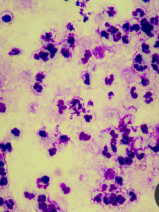
Cryptococcus neoformans
Cats > dogs
Cats: nasal cavity, Dogs: CNS
Lungs can be affected in BOTH species
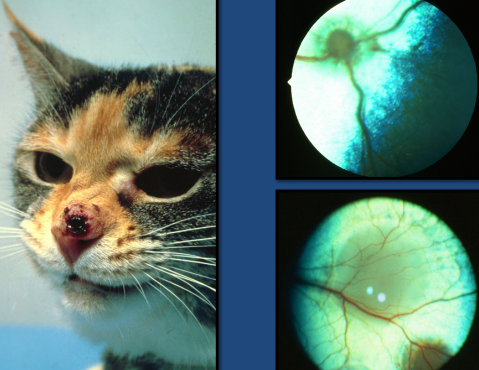
Et: Nasal mycoses, Zoonotic, enviro > direct
Polysaccharide capsule: Inhibits plasma cell function, phagocytosis, leukocyte migration, complement
Dissemination: CNS, eyes, skin, lungs, kidneys, liver
Dt: rads, CT, cytology(neutrophils/macrophages), biopsy, cytology(Cryptococcal yeast )
Capsule stains + used in Ag test
Capsular antigen test
Tx: Itraconazole, Fluconazole
6m + 2m past CS
Good if no CNS issues,
concurrent infect → FeLV/FIV less likely to respond to tx
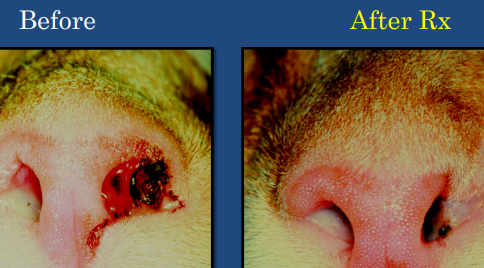


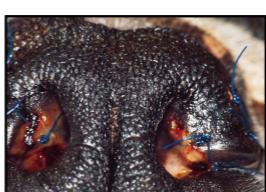
Aspergillus fumigatus (Sinonasal)
Dogs > Cats
young, male
Et: Normal inhabitant of nasal mucosa
Cs: Chronic nasal disease, Nasal discharge, Sneezing, Depigmentation and ulceration of external nares
form fungal “plaques”

Dx: rads, rhinoscopy, CT, PE, histopath, Ab test
Antigen test for systemic NOT nasal!!
Tx: Topical clotrimazole infusions
Make sure cribriform plate is intact

Nasal Parasites
Fly larvae: Cuterebra
Mites: Pneumonyssoides caninum
Nematodes: Eucoleus boehmi, Linguatula serrata
Rhinitis
Bacterial
Et: secondary lesion**
Ddx: FB, Nasal tumor, Fungal disease, Dental disease
Tx: antibiotic responsive but must fix primary issue
Inflam → dx by exclusion
Et: allergic or immune-mediated
Dt: exclusion, histopath
Tx: doxycycline, azithromycin, NSAIDs, corticosteroids
Nasopharyngeal Stenosis
Post anesthetic reflux
Chronic upper respiratory infection
Upper Airway Signs
Inspiratory dyspnea
Inspiratory noise
Stertor (pharynx, palate)
Stridor (larynx)
Vocal dysfunction (larynx)
Cough
Dysphagia, gagging
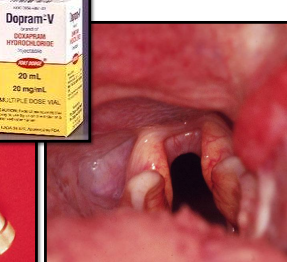
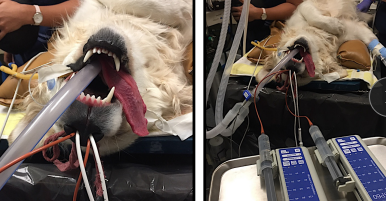
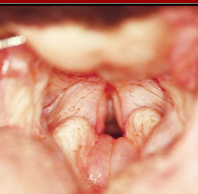
Laryngeal Paralysis (LARPAR)
Et: Failure of arytenoid cartilage to abduct during inspiration, geriatric onset laryngeal paralysis polyneuropathy GOLPP
Older, Lg dogs
Most common: idiopathic
Cs: Stridor, vocal change, coughing, acute decomp, cyanosis, syncope, death, CNS signs, toe scuffing
Progressive / chronic
Dx: Laryngoscopy, thyroid panel, thoracic xrays (mega-esophagus)
ALWAYS use IV catheter and have ET tube ready, dopram
TX:
ECC: Oxygen, Ace, Opioids, ET tube, Tracheostomy, Arytenoid lateralization (tie-back),
Sx complications: no swimming / aspiration pneumonia
Mild: rest, loose weight, no collars, corticosteroids
Prognosis: good

Brachycephalic Airway Syndrome
Et: Stenotic nares, Elongated soft palate, Everted laryngeal saccules, Laryngeal collapse, Hypoplastic trachea (English bulldog)
Not collapsing trachea
Elongated soft palate - Primary malformations
Cs: Signs of upper airway obstruction- Inspiratory issues, cough, vocal change, stertor/stridor, exercise intolerance, cyanosis, syncope
Dt: PE, scope, rads
Tx: medical management: rest, keep cool, corticosteroids, Sx, tracheostomy: last case/ not recommended

Obstructive Laryngitis
Et: Non-neoplastic infiltration of larynx
Inflammation
Cs: Inspiratory issues, cough, vocal change, stridor
Dt: Histopath
Tx: Corticosteroids, excision, radiation

Laryngeal Neoplasia
Neoplasia originating from larynx uncommon
Et: compression/invasion: secondary > primary
Thyroid carcinoma, Lymphoma, SCC
Cs: Inspiratory issues, cough, vocal change, stridor
Dt: Histopath, rads, scope, CT, US, PE → neck palpation
Tx: Sx, chemo, permanent tracheostomy(not common)
Canine infectious respiratory dz complex CIRDC
Aka: Kennel cough, Infectious Tracheobronchitis
Et: CAV-2, CPI, CIV, covid, distemper, CHV1, Bordetella, Strep, Mycoplasma
Cs: Paroxysmal cough, Sneeze, Nasal/ocular discharge, Fever, Secondary infection → VERY contagiousDt: PE, history
Further diagnostics NOT routinely needed
Tx: Self-limiting in 7-10d, Cough suppressants (Hydrocodone, Butorphanol), Humidifier
Antibiotics - Signs > 1 week, or suspected bacterial infection
No improvement = further diagnostics
Vax: CAV-2, CPI: distemper (DHPP), Bordetella, CIV: H3N8 H3N2
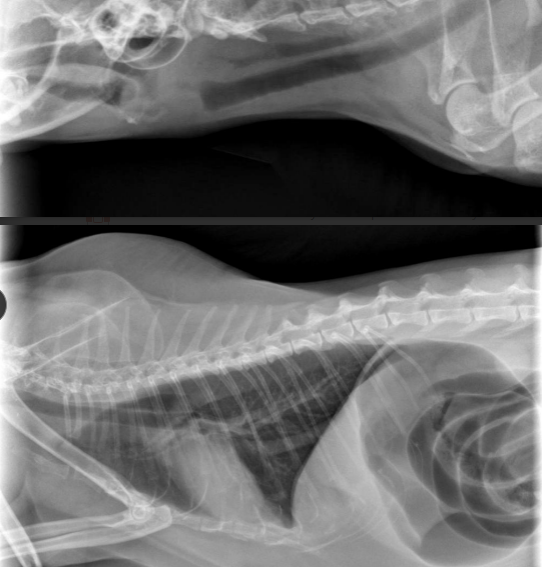
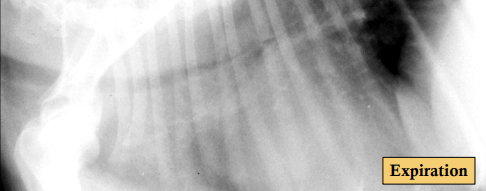
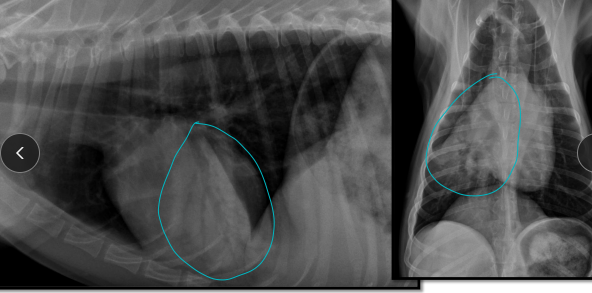
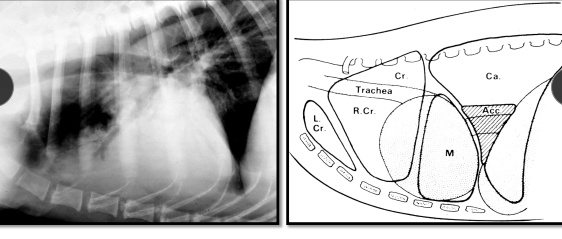
Collapsing trachea
Et: Sm breeds, Middle-aged
Inspiratory effort: extra thoracic collapse/ cervical trachea
Expiratory effort: intrathoracic collapse / thoracic trachea, mainstem bronchi
Cs: Cough, goose honk, exercise intolerance, resp distress, cyanosis, syncope
Complicating dz: Left atrial enlargement, Airway inflammation, Upper airway obstruction, Obesity, hyperadrenocorticism
Dt: Cough elicited by tracheal palpation, Rads, scope
Tx: Medical management: Avoid collars, rest, cough suppressants (Hydrocodone, Butorphanol), Corticosteroids, Sx stenting
Most controlled w/ medical management
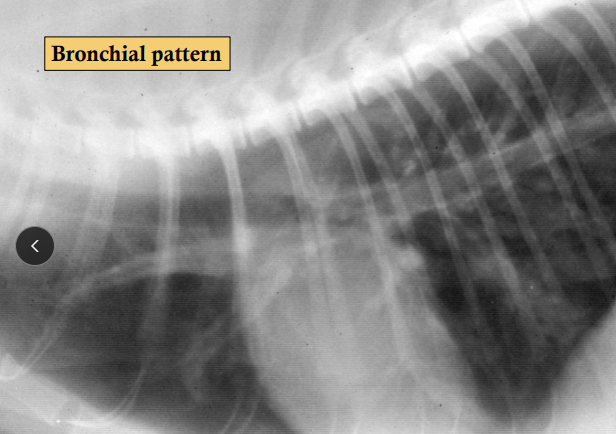
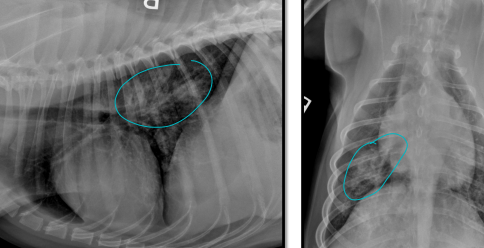
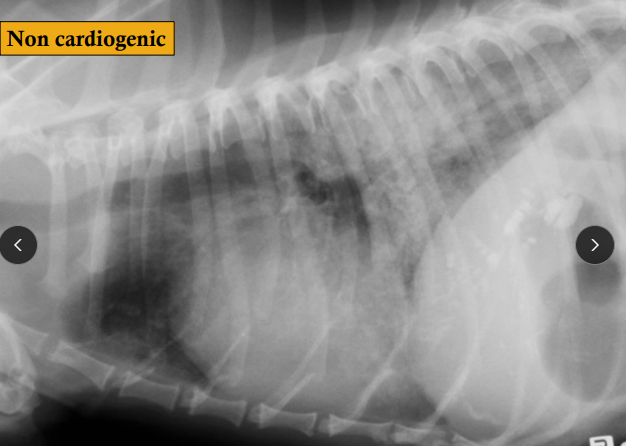
Feline Lower Airway Disease
Et: Inflam, airway hyper-reactivity, mucus hypersecretion, bronchoconstriction, bronchial smooth muscle hypertrophy, Fibrosis & emphysema
Asthma: reversible bronchoconstriction, Type I hypersensitivity, IgE, eosinophilic inflam
enviro, smoking households, allergy
Chronic bronchitis: neutrophilic inflam
permanent airway damage
Cs: Cough, Dyspnea, Wheezing(expiration), Tachypnea, Expiratory distress, Barrel-chested
Episodic
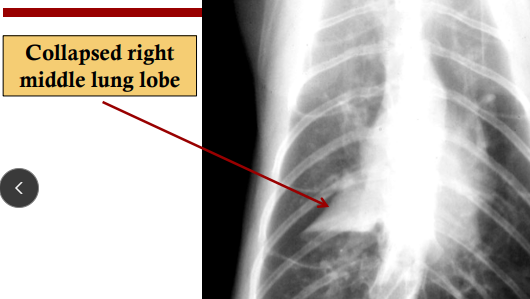
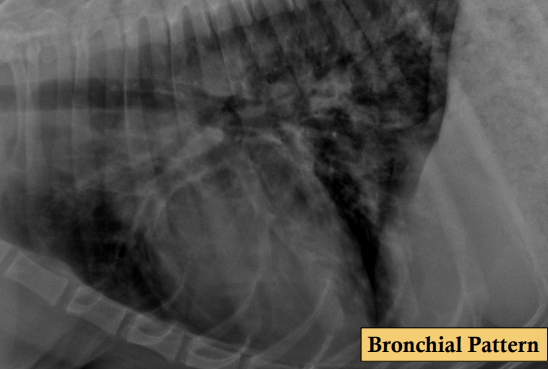
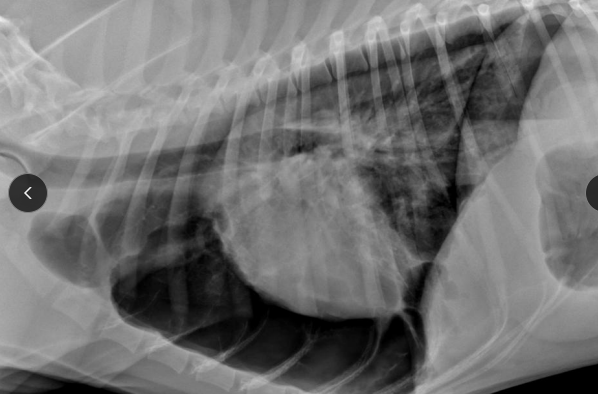
Dt: Eosinophilia, Baermann fecal (larva lung parasites), HW, Scope, Tx response, Airway wash (cytology/culture); Rads w/ Bronchial pattern, infiltrates, Hyper-inflation (air trapping), Collapsed right middle lung lobe, Spontaneous pneumothorax **
Tx: eliminate triggers, corticosteroids (oral → inhalant) (dex, pred), Bronchodilators (terbutaline, albuterol, theophylline), Antibiotics (doxycycline, azithromycin), Oxygen, Cyclosporine (refractory cases)
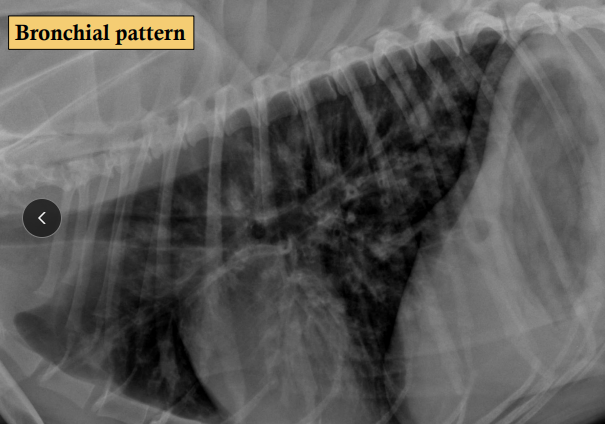
Canine Chronic Bronchitis
Et: Older Sm dogs, increased mucus
#1 chronic cough in older dogs
Cs: Chronic cough, Increased bronchovesicular sounds, Wheezes, Crackles, Mucus hypersecretion
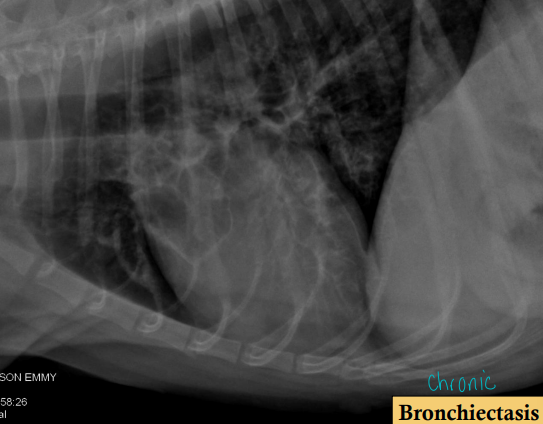
Dt: CBC, Parasite exams (fecal, heartworm), Scope, Tracheobronchial collapse, Bronchiectasis, Airway cytology/culture; rads w/ infiltrates: "donuts", "tramlines", right ventricular enlargement (pulm. hypertension), Atelectasis of right middle lung lobe
Cough present Months → years
Diagnosis of exclusion!!
Tx: Antibiotics (doxycycline, clavamox, azithromycin), Corticosteroids (oral → inhalant), cough suppressants (Hydrocodone, Butorphanol), dental care, controlled exercise
Min rxn to bronchodilators, some rxn to anti-inflammatories
Bronchoalveolar Lavage (BAL)
Paradoxical Abdominal Movement
Upper airway obstruction
Diaghragmatic rupture / paralysis
Decreased lung compliance
Severe pleural effusion
Bacterial Pneumonia
Et: E. coli (G-), Pasteurella (G-), Strep (G+)
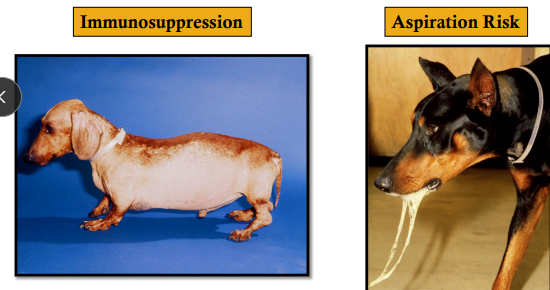
Young/old, immunocomp, dental dx, Laryngeal paralysis, downers, vomiting
Passive: Right cranial, right middle
Forceful: Right caudal
Cs: Cough, tachypnea, dyspnea, fever (uncommon), lethargy, dehydration, crackles/wheezing, Increased bronchovesicular sounds, focal areas of decreased breath sounds
Dt: CS, PE, CBC, Rads, Cytology, Culture
Septic mucopurulent inflam
Tx: Antibiotics, humidifier, lobectomy for unresponsive lobar consolidation, transtracheal washes (lg dogs), endotracheal washes
Avoid antitussives
Pulmonary Parasites
NOT common - ingestion of infective forms
Et: eosinophilic inflam
Capillaria aerophila(whip): Cs rare, worm, routine fecal exams
Paragonimus kellicotti: fluke, snails/crayfish, Right caudal lung, Cats > dogs
Aelurostrongylus abstrusus
Cs: Not all animals show clinical signs, spontaneous pneumothorax, allergic bronchitis
Dt: eggs/larvae in feces or resp samples
Tx: Fenbendazole
Eosinophilic Bronchopneumopathy
Et: Eosinophilic infiltration of lung & bronchial mucosa
2ndary to Immune-mediated hypersensitivity
Young dogs, Siberian Huskies
Cs: Cough, gag, retch, dyspnea
BAR unless pneumonia
Dt: corticosteroid rxn, CS, Rads, Scope, Cytology
MUST Rule out HW, parasites, drugs, allergens
Tx: Prednisone, steroids, deworming (fenbendazole)
Relapses common
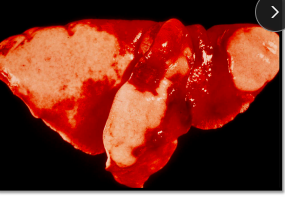
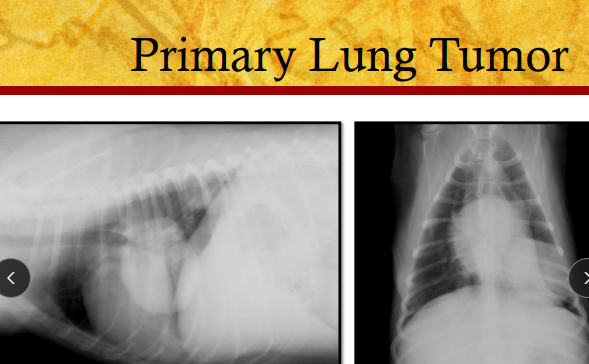
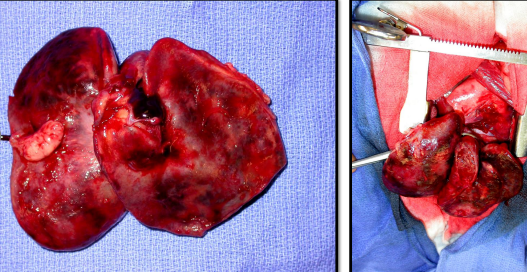
Pulmonary Neoplasia
Et: malignant, secondary > primary
Carcinoma most common
adenocarcinoma, bronchoalveolar carcinoma, SCC
Cs: asymptomatic, cough, exercise intolerance, dyspnea, weight loss, fever (if necrotic), pleural effusion, mediastinal compression, Hypertrophic osteopathy
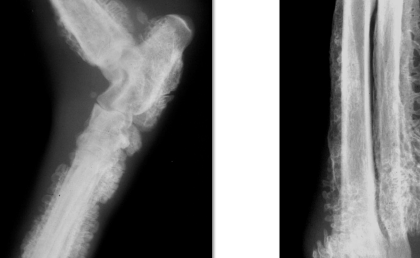
Dt: Rads, Cytology; TTW & BAL(not very useful), FNA, pleural fluid, Biopsy
Tx: Lobectomy, antitussives, NSAIDs, PleuralPort
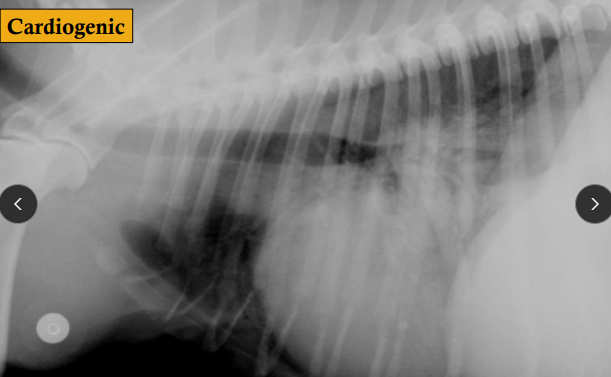
Pulmonary Edema
Et: ↓ Oncotic pressure, ↑ Hydrostatic pressure (volume overload), Lymphatic obstruction, ↑ Vascular permeability (vasculitis)
PLE, PLN, hypoalbuminemia, CHF
Cs: Acute cough, tachypnea, resp distress, crackles, Blood-tinged frothy fluid (pre-death), hypoxia
Dt: Rads w/ interstitial (early), alveolar (late); History of electrocution, seizures
Tx: Oxygen, diuretics(cardio), colloids
Idiopathic Pulmonary Fibrosis
Et: West Highland Terriers, Cairn, Yorkie, Staffordshire
Young to middle-aged
Cs: progressive dyspnea, exercise intolerance, crackles, cough
Chronic, progressive
Dt: labs/rads/bronchoscopy - WNL, Lung biopsy definitive
Tx: Prednisolone, Pirfenidone (antifibrotic)
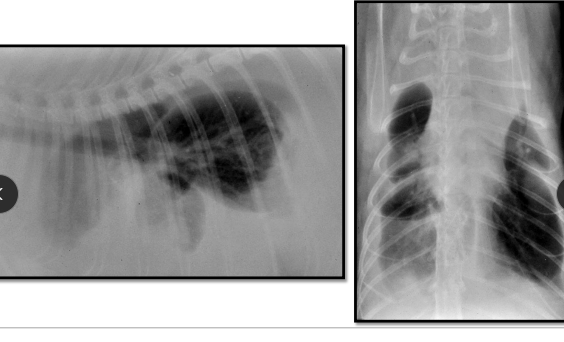
Pleural Effusion Clinical Signs
Radiography - pre/post tap
Emergency xray after
Exercise intolerance
Labored breathing
Dyspnea
Tachypnea
Orthopnea (sternal)
Rapid & shallow - labored breathing
Minimal or no cough
Auscultation - muffled (Ventral)
Percussion - dull
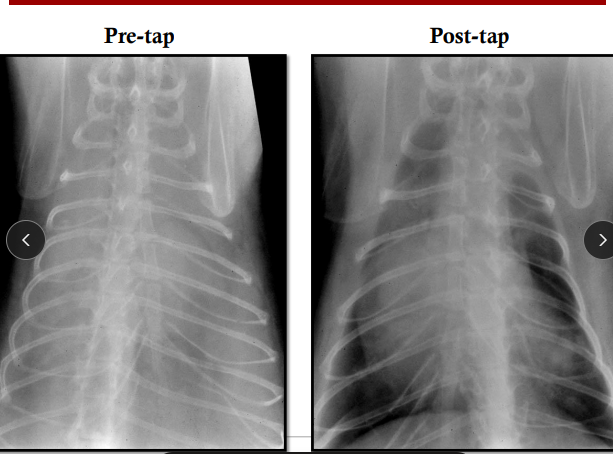
Thoracocentesis
How: Tap 7–9th ICS
Dorsally for air
Ventrally for fluid
Fluid:
Transudate: <1.5p, <1c, clear
Hypoalbuminemia, PLN, Liver dx, PLE, CHF
Always (almost) associated with low Albumin
Modified Transudate: 2.5-5p, 1-7c
CHF, Neoplasia, Diaphragmatic hernia
Corylorus fluid: 2.5-6p, 1-20c, >TG
lymphangiectasia, HF, Vena cava thrombosis, trauma, neoplasia, HW, diaphragmatic hernia, lung lobe torsion
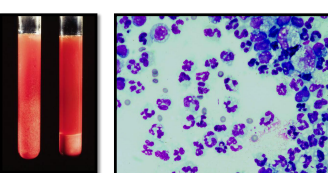
Hemmhorage: 3-6p, 5-20c
Coagulopathy, Trauma, Neoplasia
Neoplastic: 1-6p, Neoplastic cells
Pulmonary carcinoma, Mediastinal lymphoma
Pyothorax
Et: Idiopathic, chest wounds, FB, Actinomyces, Nocardia, Corynebacterium, Staph, Strep, E. coli, Klebsiella, Pasteurella
Cs: Exercise intolerance, labored breathing, no cough, muffled sounds, dull percussion, septic, fever, weight loss, rapid/shallow breathing
Dt: Rads (post tap), Thoracocentesis
Tx: Antibiotics 4-6w, chest tube + lavage, thoracotomy
Unasyn (ampicillin + sulbactam), Timentin (ticarcillin + clavulanate), FQ, Clavamox (amoxicillin + clavulanate)
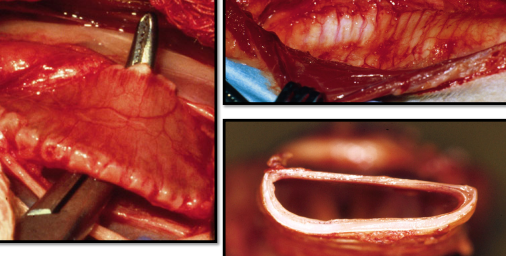
Chylothorax
Et: Idiopathic, Secondary to thoracic disease → lymphangiectasia, HF, Vena cava thrombosis, trauma, neoplasia, HW, diaphragmatic hernia, lung lobe torsion
Cs: Exercise intolerance, labored breathing, no cough, muffled sounds, dull percussion, rapid/shallow breathing
Dt: Rads (post tap), Thoracocentesis, T4 in cats
Fluid triglycerides > serum, cholesterol/TG < 1
Tx: Periodic thoracocentesis, low fat diet, oral rutin, MOST common → thoracotomy, thoracic duct ligation, pericardiectomy, omentalization


FIP Associated Pleural Effusion
Et: covid in cats
Cs: Exercise intolerance, labored breathing, no cough, muffled sounds, dull percussion, rapid/shallow breathing
Dt: Rads (post tap), Thoracocentesis
Hyperglobulinemia, Hypoalbuminemia, High globulins in effusion
Serum A:G ratio often < 0.45
Cardiogenic Effusion
Et: R CHF, Cats: most common (L or R)
modified transudate
Cs: Exercise intolerance, labored breathing, no cough, muffled sounds, dull percussion, rapid/shallow breathing
Dt: Rads (post tap), Thoracocentesis
Hemothorax
Coagulopathy
Trauma
Cancer
Hemangiosarcoma
Lung torsion
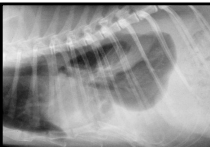
Lung Lobe Torsion Associated Pleural effusion
UNCOMMON
young male pug
Et: Left cranial lobe
Pleural effusion usually present
Cs: Exercise intolerance, labored breathing, no cough, muffled sounds, dull percussion, rapid/shallow breathing
Dt: Rads (post tap), Thoracocentesis
Tx: Sx
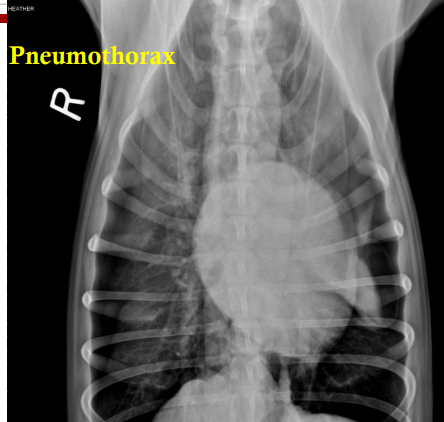
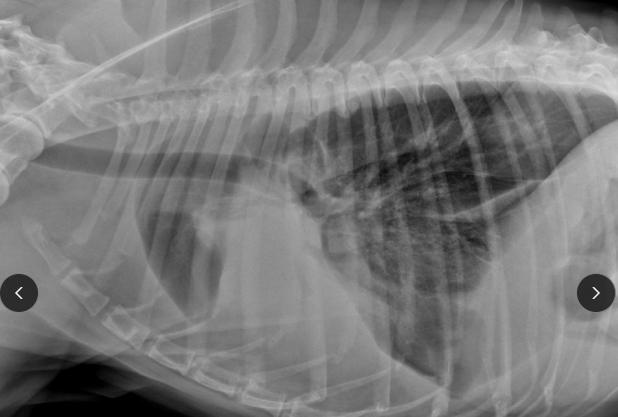
Spontaneous Pneumothorax
Et: Rupture of bullae or cavitary lesion, Pneumonia, Abscesses, Granulomas, Neoplasia
Cs: Acute dyspnea in previously healthy patient
Dt: Rads (post tap), Thoracocentesis
Tx: Thoracocentesis, Chest tube, Sx