Red & White Patches
1/34
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
35 Terms
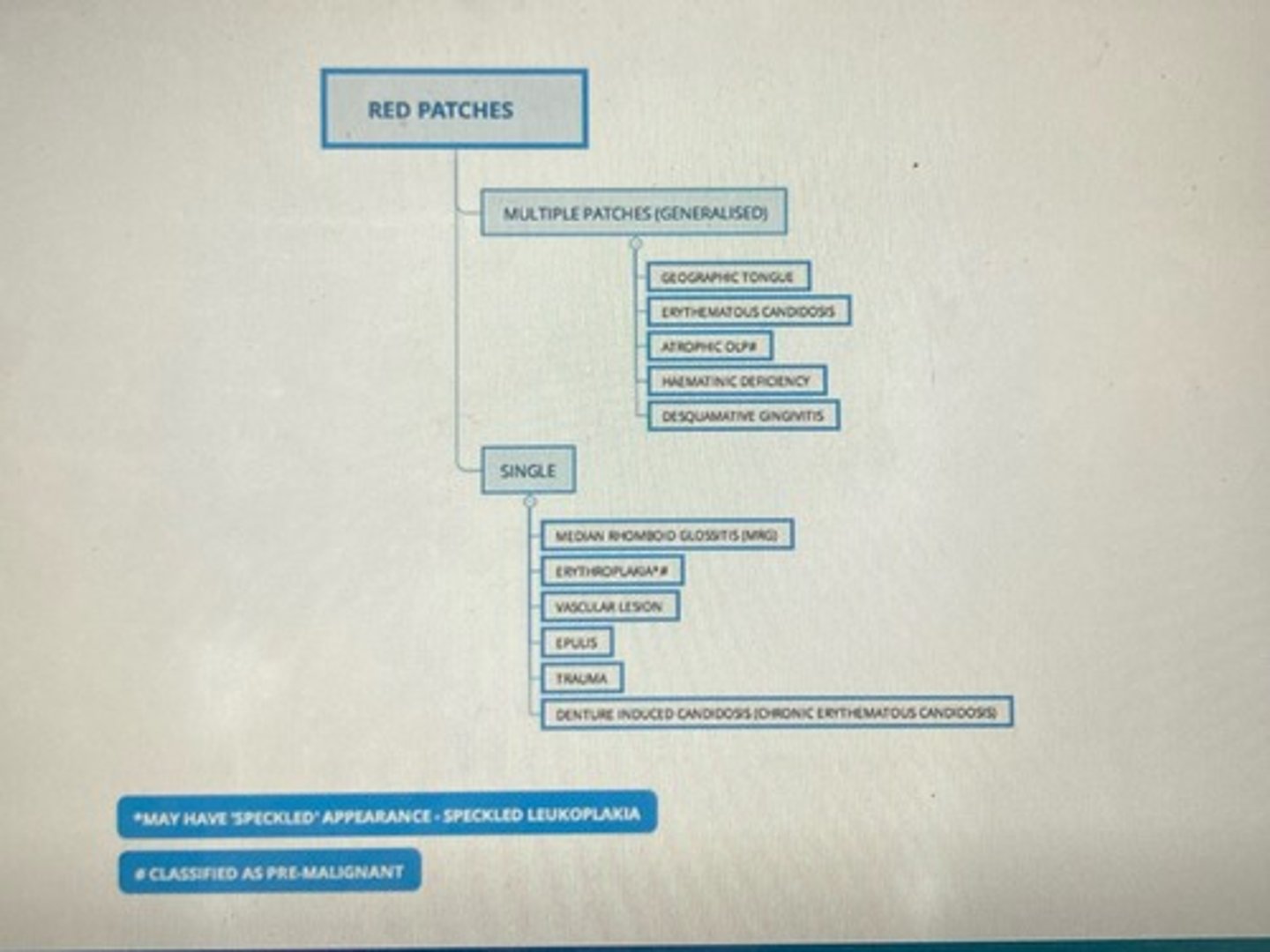
Red patches: multiple & single
You are planning to carry out a restoration in the LL4 but the patient is a bit concerned as they have noticed an unusual appearance on their tongue
• 31 year old male
• CO: red patches on his tongue
• RMH: F&W
• SH: Bank clerk, non-smoker, alcohol 10 units/week
• EO: No lymphadenopathy, no asymmetry, no skin lesions, looks well
Case 1 background
- multiple smooth areas on dorsum of tongue w/ red borders & white margin surrounding it
- areas well demarcated but irregular in shape
- fungiform papillae reddened at the tip of the tongue
Describe the appearance of the lesions:

How long have the tongue lesions been present for? 6 months
Do the lesions come & go? Yes
Do the lesions move around? Yes
Are they sore? Sometimes
Does anything make them better or worse? Spicy/acidic foods makes it sore
Have you tried any MW/medication etc? No
Does anyone in your family have them? Brother
Are they getting better or worse? Staying the same
What questions would you ask the patient?
geographic tongue/ benign migratory glossitis/ erythema migrans
diagnosis made on clinical app
What do you think the diagnosis is?
- reassurance
- avoid acidic & spicy foods
- advice benzydamine HCl (Difflam) oral rinse = OTC or prescribed
- BISOM PIL
What management would you suggest?
doesn't need referring to OM unless uncertain of diagnosis or tongue is persistently sore
in this case, pt would need blood tests to investigate for anaemia & haematinic deficiencies
Would you refer the patient and if so why?
reassure pt this is not an infectious condition
common benign condition & can run in families
The patient is worried about sharing cutlery with his family, what would you advise him?
- glossitis (anaemia & harmatinic deficiencies)
- mucositis (radio/chemo)
- mucosal disease (eg LP)
What are some other causes of smooth tongue?
You are seeing this patient to commence a course of oral hygiene instruction at the request of his Orthodontist & you notice redness on the patient’s palate
• 12 year old male (attends with Mum)
• CO: Nil
• RMH: Asthma, eczema
• Meds: Salbutamol, hydrocortisone cream
• SH: School student
• OE: No lymphadenopathy, no asymmetry, no skin lesions, looks generally well
Case 2 background
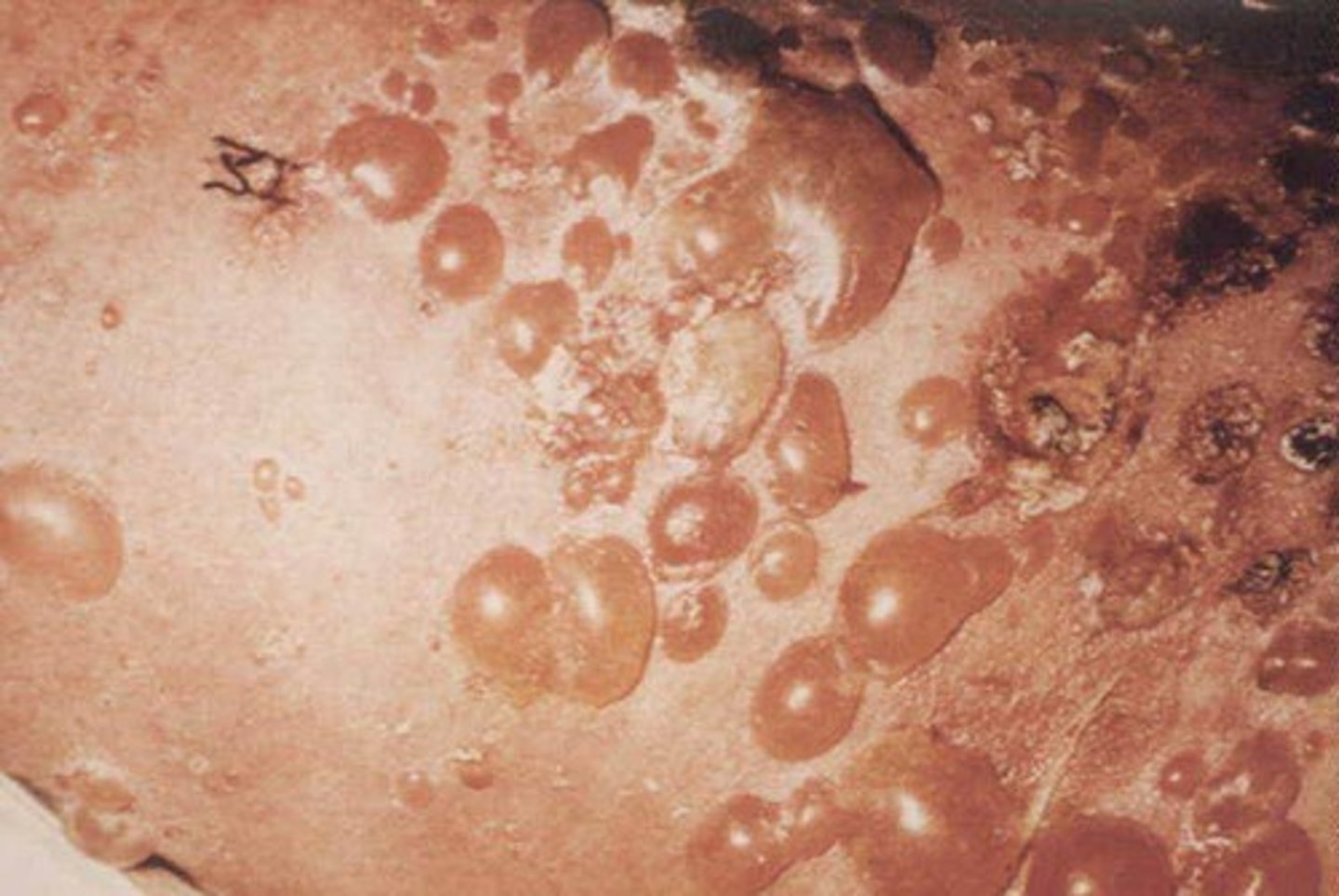
- pt's palate is erythematous over whole area > generalised
- swelling around gingival margins & incisive papilla & palatine rugae
- some inflammatory papillary hyperplasia of the mucosa overlying the hard palate anteriorly
- caries
Describe the appearance of the lesions:

Is your mouth sore? No
Do you wear a removable orthodontic appliance? Yes
How often do you clean the appliance? Normally x1 day
What do you clean it with? Rinse with water
What questions would you ask the patient?
chronic erythematous candidosis
What is the likely diagnosis?
poor hygiene of removable orthodontic appliance
What has made the patient more susceptible to this condition?
- check w/ orthodontist whether it is possible for the pt to leave the appliance out while treating the candidal infection
- CHX MW GSL (general sales list) > can be prescribed
- advice on how to clean ortho appliance (brushing w/ tp & soaking in CHX MW)
- R/v
How would you manage the patient?
- if no resolution w/ improving hygiene of appliance & use of CHX MW the pt will need a topical antifungal prescribing
- if this doesn't resolve, the pt will need referral to OM (blood tests can be done to investigate underlying factors, microbiology swabs for culture & sensitivity & for prescription or a wider range of antifungals etc)
Does the patient require referral and if so why?
You are planning to carry out a s&p. The patient asks you to be gentle as her gums are a bit sore at present.
• 56 year old female
• CO: soreness of gums
• RMH: Hypothyroidism, history of breast cancer,
• Meds: Levothyroxine
• Non-smoker
• Alcohol 0 units/week
• EO No lymphadenopathy, no asymmetry, skin rash on wrists
Case 3 background
- shiny erythematous gingivae, generalised in both arches
- some recession of gingivae & staining of teeth
Describe the appearance of the lesions:

Are your gums sore? Yes
Do they bleed easily? Yes
When did it start? About 12 months ago
Does anything make it better or worse? Some toothpastes & spicy foods make it worse
Have you tried any medication? Corsodyl but made it burn
Do you get any ulcers/blisters in the rest of the mouth? Get occasional mouth ulcers
What questions would you ask the patient about her gum lesions?
Is the pt's breast cancer in remission or is she undergoing tx (surgery/chemo/radio)? In remission, treated surgically
Has she had any genital/scalp/eye/nail lesions in addition to her skin lesions? No
Is the rash itchy? Yes & leaves purple patches
What further questions would you ask about the patient's medical history?
LP or immunobullous condition (Pemphigus & Pemphigoid) can also cause desquamative gingivitis
What is the likely diagnosis?
Pemphigus
characterised by shallow ulcers or fragile blisters that break open quickly
- an AI disease in which the immune system mistakenly attacks cells in the top layer of the skin (epidermis) & the mucous mems.
- people w/ the disease produce antibodies against desmogleins, proteins that bind skin cells to one another
Pemphigoid
presents with stronger or “tense” blisters that don't open easily
a rare skin condition that causes large, fluid-filled blisters.
could be skin lesions of LP which commonly occur on flexor surfaces of wrists or coincidental dermatological condition
Are the skin lesions related to the oral diagnosis?
- advise on oral hygiene
- avoiding spicy/acidic floods
- avoid tp's w/ SLS
- advise benzydamine HCl oral rinse OTC
How would you manage the patient?
- yes for dentist to r/v & prescribe a topical steroid (eg betamethasone MW)
- referral to OM for further investigations (blood rests & biopsy) & management
Does the patient require referral for her oral lesions and if so why?
- pt could make an appt to see GP regarding their skin lesions (topical steroid cream may be prescribed)
- GP or OM dept may refer to dermatology if req
The patient is concerned about the skin lesions and asks if she needs to be referred for these. What would you advise?
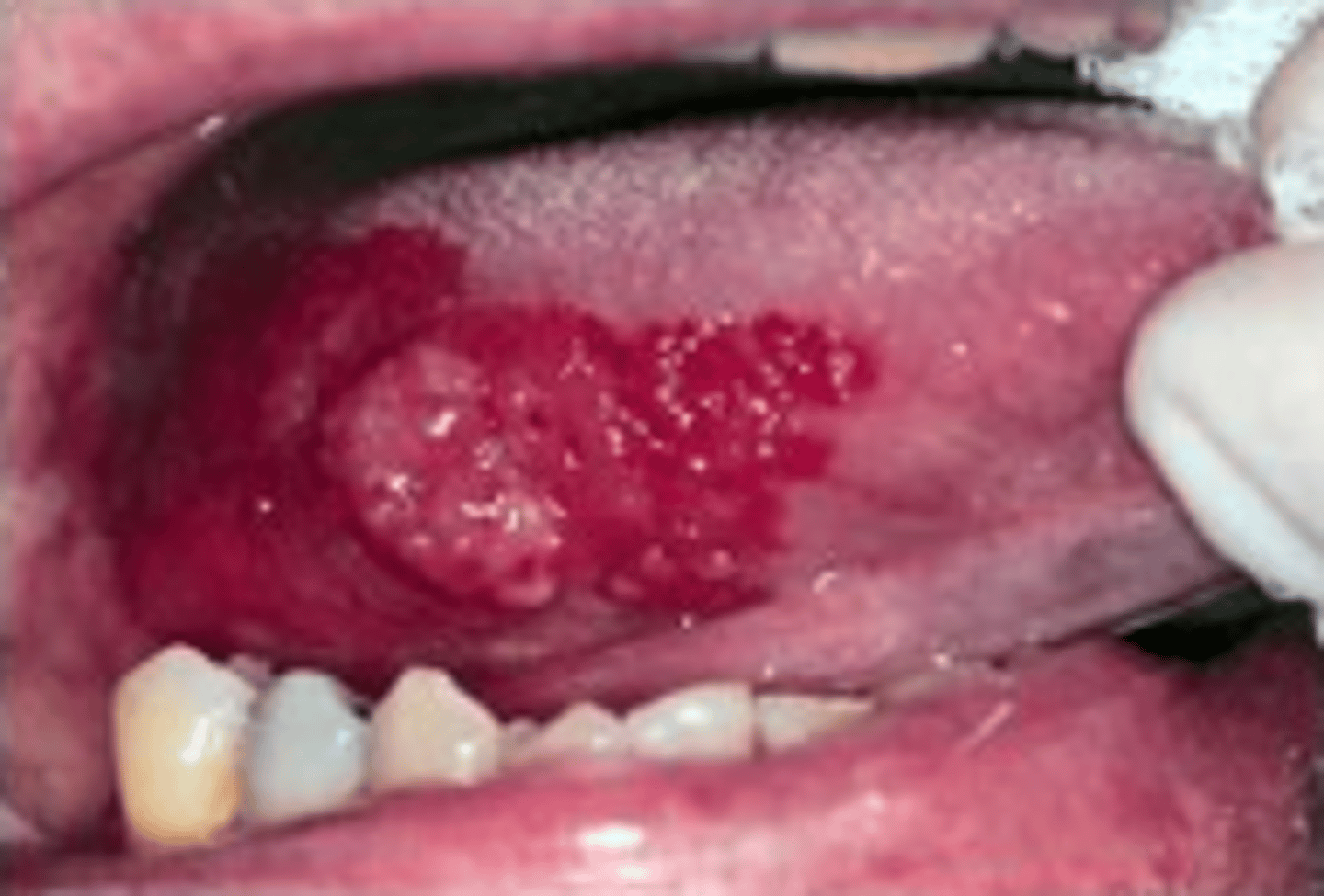
- erythematous/red velvety lesions present on R lateral border of tongue
- approx 5x3cm diameter & extends distally
- well circumscribed w/ an irregular margin
- exophytic/raised area centrally
Describe the appearance of the lesions:
A new patient attends for a replacement of restoration LR4, you notice a red patch on the side of the patient’s tongue which the patient was not aware of.
• 62 year old female
• CO: Nil
• RMH: Hypertension, had surgery for detached retina last year, diverticulitis
• SH: Non-smoker, alcohol 5-6 units/week
• RDH: Irregular attender
• EO: No lymphadenopathy, no asymmetry, no skin lesions, looks generally well
Case 4 background
How long has it been present for? Not sure as she wasn't really aware of it
When was the last time that she visited a dental professional? Many yrs ago
Is it painful? No
Does it bleed? No
Was she a past smoker or heavier drinker in the past? No
What questions would you ask the patient about the lesion?
Erythroplakia (potentially malignant lesion)
What is the likely diagnosis?
- urgent 2 week referral to OM/OS/O&MFS dept
NICE guidelines Dec 2021 state:
- consider an urgent referral for assessment for possible oral cancer by a dentist in ppl who have either:
> lump on lip or in OC or
> red/red & white patch in the OC consistent w/ erythroplakia or erythroleukoplakia
What would your management be?
referral necessary for an urgent biopsy to establish the diagnosis & further management as necessary
Would you refer the patient and if so why?
- imp pt understands they need an urgent referral so that a diagnosis can be made (until then oral cancer cannot be excluded)
- pt should be advised to attend her 2 week referral appt & delay her holiday otherwise the diagnosis & tx will be delayed & this could affect her prognosis
The patient is planning to go on holiday next week to her second home in Spain for a couple of months (post COVID era) and asks if she will still be ok to go?
inflammation of the diverticula (small, bulging pouches that can form in the lining of your digestive system. Most often in the lower part of the LI (colon))
Diverticulitis