TV4101 - Bovine - Nervous Part 2 - Weaned Calves and Older cattle
1/82
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
83 Terms
Listeriosis
Most common manifestation in AUS?
Prevalence?
Meningo-encephalitis
Sporadic in cattle mainly 2-3yrs
Listeriosis
Pathogenesis?
Soil contaminated feed most important route of infection (many ass. with silage feeding esp with poor fermentation/conserved)
L. Monocytogenes invade oral cavity mm → Trigeminal Nerve (CN V) → Cerebrum
Focal necro with microabscesses → neuritis, meningitis and encephalitis
Listeriosis
CX
Vary based on?
Most common neurological signs?
Location of lesions within cerebrum (which CN affected)
- localised facial paralysis with head tilt towards the affected side
- circling
- ‘propulsive tendency’ → may be found with head forced through a gate or wedged under a feed bunk

Listeriosis
CX
Non-neuro signs?
Mod Pyrexia (Early stages only and gone <96hrs)
Weight loss, dec milk prod, depressed, anorexic

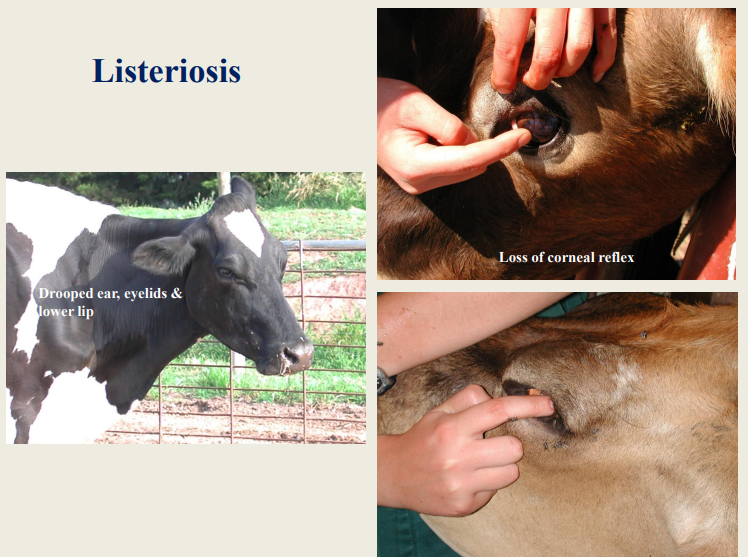
What is this? Describe each
Listeriosis
Left - Head tilt, and circling towards affected side
Right - Unilateral facial paralysis
Several syndromes are associated with L. monocytogenes
infection in cattle - Including?
- uterine infections (abortion)
- meningo-encephalitis
- mastitis (rare)
- septicaemia, and iritis with uveitis


What is this?
Listeriosis
Unilateral facial paralysis
Listeriosis - CX
Infection involving ganglia of the facial nerve (CN VII) signs?
Unilateral facial paralysis, characterised by:
- drooped ear & eyelids (ptosis)
- a flaccid lip
Can lead to loss of both menace response and palpebral reflex → 2ndary exposure keratitis
Listeriosis - CX
Infection involving ganglia of the vestibulocochlear (CN
VIII) nerve signs?
• leads to ataxia, head tilt, and circling
• in later stages, affected cattle become recumbent; may show opisthotonos and torticollis before death

Listeriosis - CX
Other uncommon presentations?
Which nerve is affected?
Involvement of glossopharyngeal nerve (CN IX) may cause stertorous breathing and dysphagia

Listeriosis DX
Main DDX?
- brain stem abscess
- pituitary abscess syndrome (basilar empyema)
- otitis media/interna
- trauma
- less commonly confused diseases include PEM, lead poisoning, nervous ketosis, thrombo-embolic meningo-encephalitis (Histophilus somni infection)
Listeriosis DX
CX for encephalitic form?
Circling, with depression & facial paralysis, is almost
pathognomonic for the encephalitic form of the disease
Listeriosis PM
MS findings?
Lesion location?
Organism isolation?
What is sufficient to confirm Dx?
MS
In cerebrum - Many micro-abscesses or foci of inflam cells (Sufficient to confirm Dx usually)
Lesions usually unilateral
Isolation of causal organism from the brain may require
extended periods of ‘cold enrichment’, and listerial culture
can prove disappointing
Listeriosis Tx
ABs?
Penicillin or aminopenicillins
BID with high dose rates for at least 7 days
Addition, give high dose of penicillin G i/v on first day
Oxytet?
Listeriosis Tx
Supportive therapy?
- NSAID → for the inflammation
- IV fluids & electrolytes → to treat the dehydration & metabolic acidosis
Listeriosis Tx
Rumen aid?
Transfaunation with rumen liquor may promote rumen
function during recovery
Listeriosis - PX
Soil contamination of silage is limited by?
Rolling grass fields at the beginning of the growing season
Listeriosis - PX
We want good silage fermenting.
How do?
- cutting grass at an early growth stage → contains a high fermentable sugar content
- wilting it for 24 hours
- using various silage additives (sugars or organic acids)
- compacting of the silage clamp → expels air
- covering it, making sure it has a tight seal → prevents aerobic bacterial multiplication

What is this?
Botulism

Botulism
Overview?
Ascending motor neuro-paralytic disease caused by ingestion of pre-formed toxins released by Clostridium botulinum bacteria
Botulism
Agent and features?
Cl. botulinum – a large Gram positive rod-shaped bacillus
Very resistant bacterial spores
Endospores germinate (with growth of vegetative cells and toxin production) in anaerobic conditions (rotting carcass, decaying plants, cont canned food)
Botulism
Outbreaks in livestock are
generally divided into two categories, what are they?
1. situations where disease occurs in cattle that develop
osteophagia (bone chewing) or sarcophagia (carrion
eating) → associated with phosphorus deficiency or
protein deficiency, respectively
2. death of a large number of animals in a short period of
time → associated with the ingestion of toxic feed or
water
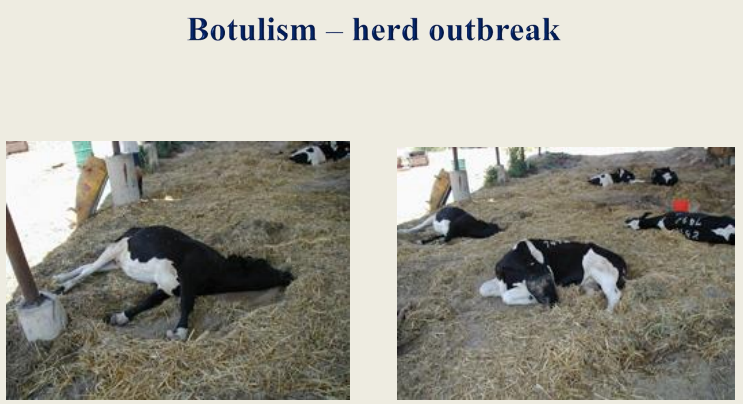
Botulism clinical findings
Oft presented as?
Multiple ‘down cows’ with some evidence of progressive muscular weakness → initial response to Ca treatment (hypocalcaemia), but have relapsed
Botulism clinical findings
Peracute disease – classical intoxication
Features?
• high levels of toxin formed outside of the victim’s body are
ingested in contaminated feed (silage or grain)
• sudden death in previously normal animals → usually with 24 hrs of exposure
Botulism clinical findings
Acute and subacute forms
Features?
Asc para → recumbency
Early classic signs → flaccid paralysis of tongue and muscle ass. with chewing and swallowing (Tongue protruded)
Muscles of jaws and throat are affected before those of limbs; hindquarters before forequarters
Botulism - Toxico-infectious botulism
How it works?
Fatality?
Occurs when?
Cl. botulinum spores in normal GIT from environmental cont
Altered gut conditions → growth of vegetative stage → toxin prod
Death isn’t a certain outcome
Often occurs during droughts or during cases of K deficiency
Botulism CX continued
As the disease progresses?
restlessness, stumbling, knuckling over, shallow abdominal breathing, and constipation
Prog weaker and dehydrated → sternal recumbency
Muscle tone loss in neck and head → head on ground or turned to flank
Skin sensation is retained, and consciousness continues
almost to the end

Botulism DX
Early signs are often confused with?
Post-parturient paresis (‘downer-cow’ syndrome), hypocalcaemia, hypokalaemia, myopathy, organophosphate poisoning, or spinal cord disease
Botulism DX
Tests?
ELISAs, measuring antibody to Type C and D toxins in
serum
Botulism TX
Treatment is only warranted in subacute cases:
- initial objective is the neutralisation of circulating toxin → specific
mono-valent or multi-valent botulinum antitoxin
- feasible, but rarely used in cattle
Botulism PX
• Assess silage and grain stores for risk
• Remove carcases from paddocks and dams
• Supplement with Phosphorous
Botulism Control
Vaccine (best way)
single dose, bivalent (Type C & D) vaccine
→ protects naïve cattle for 2 (SingVac® 2 Year) or 3 years (SingVac® 3Year)
Thrombo-embolic Meningo-encephalitis (TEME)
Agent? What does it do?
Histophilus somni infection; bacteria localize in meninges, brain, muscles and joints
Thrombo-embolic Meningo-encephalitis (TEME)
Prevalence?
Worldwide but oft in US feedlots
1-2 wks after H. somni resp dz episode that is untreated
Thrombo-embolic Meningo-encephalitis (TEME)
Other syndromes associated with H. somni infection include?
- respiratory disease
- reproductive disease & abortion
- myocardial & joint infections
Thrombo-embolic Meningo-encephalitis (TEME)
CX
Positional changes of animal?
Unsteady gait & stance, knuckling of fetlocks, becoming
progressively ataxic
Oft found in lat or sternal recumbency in an
obtunded state (~stupor) with muscle tremors, and sometimes convulsions

Thrombo-embolic Meningo-encephalitis (TEME)
CX
Ocular aspects?
Nystagmus may be present; animals may be blind in one or both eyes
Ocular lesions consist of foci of retinal haemorrhages and
accumulations of exudate → appear as ‘cotton tufts’
Thrombo-embolic Meningo-encephalitis (TEME)
Parameters?
Jts?
Dz characterised by?
Fever (40.5-41.5oC) in the early stages
Joints may be swollen and painful (acute synovitis)
Characterised by acute onset, rapid course, high fatality rate
Thrombo-embolic Meningo-encephalitis (TEME) - PM?
• Fibrinopurulent meningitis
• Red/brown foci of haemorrhage & necrosis
(infarcts) throughout brain & spinal cord → virtually
pathognomonic
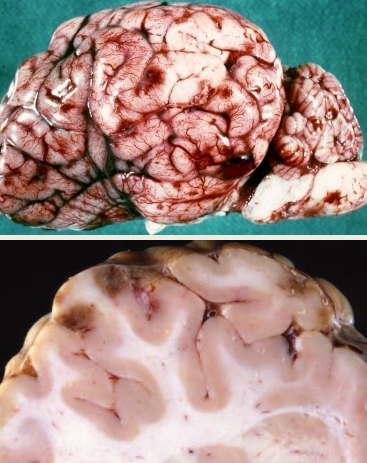
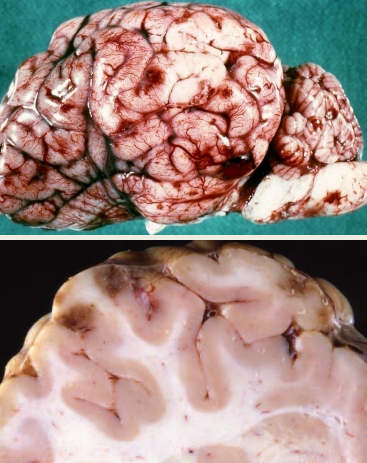
What is this?
TEME
Thrombo-embolic Meningo-encephalitis (TEME) - Management
Treatment should only be initiated in?
Drugs?
The early stages (depression, ataxia, circling), i.e. before cattle become recumbent
Penicillin, florfenicol and oxytetracycline
Thrombo-embolic Meningo-encephalitis (TEME) - Management
Appropriate management and husbandry practices for
prevention of respiratory disease should be put in place
“Can you name some ??”
?
Tetanus
Agent? Features?
Clostridium tetani bacteria that makes toxin with nervous tissue affinity
Stab wounds, deep puncture wounds with tissue damage (→ anaerobic conditions), and those cont with soil/faeces are most likely to lead to tetanus
May be present as a localised wound infection originally
Tetanus
In cattle, most cases are associated with?
Other portal of entry?
Castration, tail docking, dehorning, or uterine infection following abortion/calving
Umbilicus of the newborn calf
Tetanus
Pathogenesis steps?
Bacteria enter wound → anaerobic conditions → germinate in host tissue → mutliply and make tetanus neurotoxin
Neurotoxin spreads → local motor nerves → spinal cord (now cx seen)
Tetanus
Idiopathic tetanus is thought to arise when?
Certain conditions in reticulorumen → small pop of Cl. tetani normally present multiply → make enough toxin to cause dz
Tetanus - CX
Facial Changes?
Anxious, startled expression with bulging eyes, and erect ears
Flared nostrils
Protrusion of the nictitating membrane (not as prominent in cattle c.f. horse)
Drooling saliva

Tetanus - CX
Behaviour changes?
What the earliest signs in general?
Animal is hyperaesthetic → sudden noise or touch induces
spasm
Eating & drinking soon become difficult or impossible →
tetany of masseter muscles (‘lockjaw’)
Earliest sign is a slight muscular stiffness (10-14d PI)
Tetanus - CX
Stance changes?
Head is held lowered, with the neck extended
Animal stands rigidly → has difficulty in walking & turning
Abducted limbs (sawhorse stance)
Tail is held cocked away from the hindquarters, giving a
‘pump handle’ appearance

Tetanus - CX
Other changes?
Final stages?
Slight, but persistent rumen tympany (bloat)
Final stages → lateral recumbency, with severe tetanic
spasms, often accompanied by opisthotonos

Tetanus - TX
Mortality rate of affected, untreated cattle is around?
TX involves 3 steps, what are they?
60%
Neutralisation of the toxin
Prevention of further toxin production
Relaxation of muscle tetany
Tetanus - TX
Neutralisation of the toxin
How to do?
Principle?
Tetanus antitoxin given
Dose varies - 1000-5000 IU/kg BW
Neutralises toxin (only if it hasn’t bound to nerve tissue yet) in early stages of dz
Tetanus - TX
Prevention of further toxin production
How to do?
Local wound treatment, including debridement (controversial)
H2O2 irrigation
Local penicillin
Sys ABs (Penicllin - 30,000 IU/kg BID for 3d → OID until at least 2d after spasms stopped)
Tetanus - TX
3. Relaxation of muscle tetany
How to do?
In addition?
Use of a tranquilliser and/or muscle relaxant (chlorpromazine or acetylpromazine)
acetylpromazine (0.05 mg/kg q8h) ideally
Dec hyperaesthesia AND activates some inhibitory pathways that are refractory to toxin effects
Additional TX
Severe bloat relief via rumen trocar
Cases in single dark deep bedded sheds
Tetanus PX
Active immunisation, using tetanus toxoid (can be carried out at any age)
Long lasting protection
Two vaccinations, 4-6 wks apart
Multi-valent clostridial vaccines usually include a tetanus component

What this?
Nervous coccidiosis
Nervous Coccidiosis
Onset of nervous signs is usually (but not always) proceeded by?
Initial neurological signs include?
Dysentery and tenesmus
- depression
- incoordination
- twitching & hyperaesthesia
Nervous Coccidiosis
As condition worsens?
Recumbent
Periodic head and muscle tremors
Nystagmus
Mouth frothing
Paddling movements
Ventroflexion of head and neck
Opisthotonos

Nervous Coccidiosis
DDX inc?
- polioencephalomalacia
- lead poisoning
- acute meningitis
- salt poisoning
- hypovitaminosis A
- clostridial enterotoxaemia (Cl. perfringens)
Cerebral Babesiosis
May occur from?
CNS are varied, some inc?
Babesia bovis infections
- hyperaesthesia
- nystagmus
- circling
- head pressing
- aggression
- convulsions & paralysis

Cerebral Babesiosis
TX?
No TX, Cerebral babesiosis is almost invariably fatal
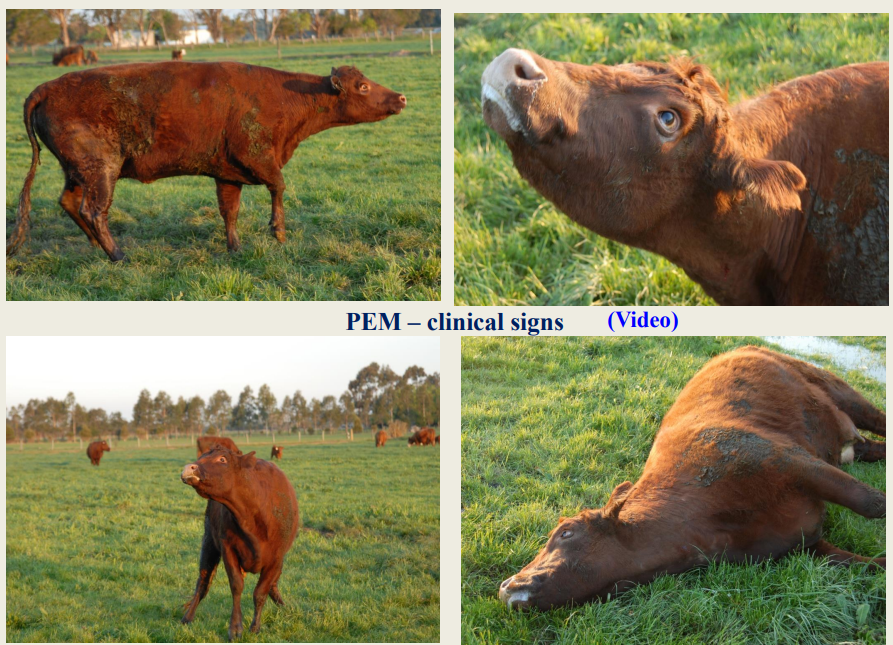
Polioencephalomalacia (PEM)
(Cerebrocortical necrosis)
Descriptive, but non-specific term; PEM refers to?
PEM can be caused by?
In cattle, predominantly a disease of?
Histological lesions of the brain → necrosis of areas in grey matter of the cerebral cortex
thiamine deficiency, lead poisoning, and salt toxicity
Well-fed and thrifty young growing animals
Polioencephalomalacia (PEM)
PEM is usually associated with? (Food aspect) Result?
Grazing lush pastures or feeding of high concentrate rations → Rumen flora changes → Inc pop of organisms that make thiaminase type 1 → thiamine def
Polioencephalomalacia (PEM)
Most PEM cases are associated with a functional deficiency of?
Why is this an issue?
Most common underlying cause of thiamine deficiency is the presence of?
Thiamine (vitamin B1)
Rumen microbial thiamine production needed for
daily vitamin B1 requirements
thiamine is water-soluble → there is no long-term storage
Thiaminases in the rumen
Polioencephalomalacia (PEM)
A cause associated with a drug is? Why?
Feeding of amprolium at high doses above recommended (for control of coccidiosis) → is a thiamine analogue → ass. with thiamine def
Polioencephalomalacia (PEM)
PEM is increasingly associated with ingestion of high X diets? Why? Other features?
High sulphur-containing diets or water sources (or both)
Dec. thiamine at cell level
PEM is distinctly epidemiological in this way
Doesn’t respond or v poorly to thiamine TX
PEM
In the Australasian pastoral farming systems → a change in the diet from X to X is often ass. with PEM
poor, stalky grass to good, lush pasture
PEM - CX
During early stages, there is often?
Behaviour changes?
Brief diarrhoea period b4 nervous signs
Behaviour
Isolate from herd
Dullness
Apparent blindness
Ataxia
Proprioceptive deficits
Hyperaesthetic to tactile and auditory stimuli
Dz progresses → head pressing and bruxism
PEM - CX
Eyes?
Reflexes?
Nystagmus with dorso-medial strabismus of eyeballs
Neurological examination →no menace response, but palpebral response & pupillary light reflex are present → a
centrally-mediated blindness
PEM - CX
Stance changes?
Rumen?
Tremors?
High head carriage and cattle may stagger
Eventually recumbent, combined with opisthotonos & extensor rigidit
Rumen function is maintained → important diagnostic sign
Fine muscle tremors, becoming more severe, then seizures & convulsions develop
W/O TX → convulsing → collapse → death
PEM - DX
DDX?
- lead poisoning
- salt toxicity
- hypovitaminosis A
- listerial encephalitis
- thrombo-embolic meningo-encephalitis
- bacterial meningitis
- hypomagnesaemia
PEM - DX
How to DX?
primarily on history, clinical signs (cx not specific for pem) and
response to intravenous thiamine administration
PEM - PM?
Histolgy?
Brain
Pale, swollen
Cerebral cortex flat and smooth (compressed gyri)
Lesions
Malacia in brain restricted to grey matter esp cerebral cortex
Fluoresce under UV (bright blue-green) sometimes
Histology confirms the presence of cerebrocortical necrosis, mainly affecting the dorsal occipital and parietal regions
PEM - TX
Main tx? Response aspects?
Other ancillary treatments include?
Thiamine HCL
Large initial IV dose (10-15mg/kg)
If response (same dose next 12 hrs then BID for at least 3d)
Favourable response → improved mental status and gait within 12hrs of 1st tx
Improved vision within 48hrs but residual blindness can occur
- IV corticosteroids (dexamethasone, 1-2 mg/kg)
- IV mannitol (1-2 mg/kg in a 20% solution)
Hypovitaminosis A
Young vs Adult?
Calves?
Young animal def → compressed brain and spinal cord
Adult def → night blindness, weight loss and infertility
Calves are born with a low vitamin A status → need colostrum to protect against overt deficiency
Hypovitaminosis A
Vitamin A is formed from its precursor?
Stored where?
Cattle fed a diet devoid of vitamin A will take X b4 showing CX?
β-carotene → present in green feedstuffs
Vitamin A is fat-soluble and stored in liver
Approx 180 days
Hypovitaminosis A - CX
Calves
Eyes?
Eyes
Blind
Dilated, unresponsive pupils
Tapetal bleeding (pupillary oedem and inc CSF psi)
No menace
Excess lacrimation
Hypovitaminosis A - CX
Calves
Neuro signs?
head pressing, convulsions, paralysis and recumbency
Hypovitaminosis A - CX
Adults
Cows?
Placental degeneration → abortion, or birth of dead or weak calves. RFMs are common
Hypovitaminosis A - CX
Adults
Bulls
Degen of the germinative epithelium of the
seminiferous tubules → Dec number of normal
sperm cells
Hypovitaminosis A - TX
Vit A parenteral inj (400IU/kg BW)
Rapid response in animals with inc CSF
Blind cattle (from prolonged papillary oedema and compressed optic nerves) → no response → slaughter
Hypovitaminosis A
Disease is unlikely to occur under year-round grazing
conditions; exceptions include?
- prolonged drought-stricken pastures
- poor-quality preserved feedstuffs
- diets that are high in grain
- continued administration of bloat oils (→ carotene deficiency)
Lead poisoning
Signalment?
Characterized by?
Young, inquisitive calves (usually <5 months of age) mostly - uncommon in adults
Acute encephalopathy following accidental
exposure and ingestion of lead-containing materials