Chapter 17: Endocrine System
1/112
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
113 Terms
What are endocrine glands?
Endocrine glands are ductless glands that secrete hormones directly into the interstitial fluid, which then diffuses into the bloodstream to reach target cells throughout the body, eliciting widespread and long-lasting effects.
What are exocrine glands?
Exocrine glands are glands that secrete their products (e.g., sweat, saliva, digestive enzymes) through ducts onto epithelial surfaces or into body cavities, rather than directly into the bloodstream. Their effects are typically localized.
How does nervous signaling differ from endocrine signaling in terms of speed and duration?
Nervous signaling uses rapid electrical impulses and chemical neurotransmitters for fast, short-term, and highly localized responses. In contrast, endocrine signaling involves hormones transported via the bloodstream, resulting in slower onset, but generally longer-lasting and more widespread effects throughout the body.
What is a hormone?
A hormone is a chemical messenger molecule secreted from an endocrine gland or specialized cell into the extracellular fluid. It travels primarily through the blood circulatory system and binds to specific protein receptors on or within target cells, triggering a particular physiological response.
Describe the characteristics of lipid-soluble hormones.
Lipid-soluble hormones are hydrophobic, meaning they do not dissolve well in blood plasma and require transport proteins for circulation. Due to their lipid-soluble nature, they can readily diffuse across the lipid bilayer of the cell membrane to bind to specific receptors located in the cytoplasm or nucleus of target cells.
Provide examples of lipid-soluble hormones.
Key examples of lipid-soluble hormones include all steroid hormones (derived from cholesterol, such as cortisol, aldosterone, estrogen, progesterone, and testosterone), thyroid hormones (T3 and T4), and nitric oxide (a gas that acts as a local hormone).
Describe the characteristics of water-soluble hormones.
Water-soluble hormones are hydrophilic, meaning they dissolve easily in blood plasma and typically circulate freely without the need for plasma transport proteins. They cannot directly pass through the lipid bilayer of the cell membrane and therefore bind to specific protein receptors located on the external surface of the target cell membrane, initiating a signal transduction pathway involving second messengers.
Provide examples of water-soluble hormones.
Examples of water-soluble hormones include most amine hormones (e.g., catecholamines like epinephrine and norepinephrine; melatonin), all peptide hormones (short chains of amino acids), and all protein hormones (longer polypeptide chains).
What are amine hormones?
Amine hormones are a class of hormones derived from a single amino acid, often modified. Examples include catecholamines (epinephrine, norepinephrine, and dopamine), which are derived from tyrosine, and melatonin, derived from tryptophan. Thyroid hormones (T3 and T4) are also amine hormones, but due to their lipid-like structure, they are lipid-soluble.
What are peptide hormones?
Peptide hormones are short chains of amino acids, typically ranging from 3 to 49 amino acids in length. They are water-soluble and serve as chemical messengers in various physiological processes. Examples include antidiuretic hormone (ADH) and oxytocin.
What are protein hormones?
Protein hormones are longer polypeptide chains, typically composed of 50 to 200 or more amino acids, often with complex three-dimensional structures. They are water-soluble and exert widespread effects on target cells. Examples include human growth hormone (hGH) and insulin.
Explain the role of cAMP as a second messenger in hormone signaling.
Cyclic AMP (cAMP) is a crucial intracellular second messenger in the signaling pathway of many water-soluble hormones. When a hormone binds to its cell surface receptor, it activates an enzyme called adenylyl cyclase, which converts ATP into cAMP. cAMP then activates protein kinases, initiating a cascade of phosphorylation events that lead to the cell's specific response.
How is cAMP inactivated, and what is the significance of this process?
cAMP is rapidly inactivated by the enzyme phosphodiesterase, which converts it into inactive 5'-AMP. This rapid degradation is essential for ensuring that the cellular response to a hormone is transient and can be quickly terminated once the hormone signal is removed, allowing for precise control of cellular activity.
Describe the anatomical and functional relationship of the Hypothalamic-pituitary axis.
The Hypothalamic-pituitary axis is a principal neuroendocrine control system that regulates numerous body functions. The hypothalamus produces releasing and inhibiting hormones that control the anterior pituitary's secretion, and it also synthesizes hormones (oxytocin and ADH) that are stored and released by the posterior pituitary, illustrating a direct functional link between the nervous and endocrine systems.
What is the Hypophyseal portal system, and what is its significance?
The hypophyseal portal system is a specialized capillary network that directly connects the hypothalamus to the anterior pituitary gland. This direct vascular link allows hypothalamic releasing and inhibiting hormones to quickly reach the anterior pituitary cells in high concentrations, regulating their hormone secretion without being diluted in the systemic circulation.
What is Human Growth Hormone (hGH), and what are its main functions?
Human Growth Hormone (hGH), also known as somatotropin, is a protein hormone secreted by the anterior pituitary gland. Its primary functions include promoting the growth of all body tissues, especially bone and muscle, by stimulating protein synthesis, cell division, and cellular uptake of amino acids. hGH also enhances lipolysis and reduces glucose uptake by cells, and stimulates the liver to produce insulin-like growth factors (IGFs) which mediate many of its growth-promoting effects.
What is Thyroid-Stimulating Hormone (TSH), and what is its role?
Thyroid-Stimulating Hormone (TSH), also known as thyrotropin, is a glycoprotein hormone secreted by the anterior pituitary gland. Its main role is to stimulate the thyroid gland to synthesize and release thyroid hormones (T3 and T4), which are critical regulators of metabolism.
What is Follicle-Stimulating Hormone (FSH), and what is its function in males and females?
Follicle-Stimulating Hormone (FSH) is a gonadotropin secreted by the anterior pituitary gland. In females, it stimulates the development of ovarian follicles and the secretion of estrogens. In males, FSH stimulates spermatogenesis (sperm production) in the seminiferous tubules of the testes.
What is Luteinizing Hormone (LH), and what is its function in males and females?
Luteinizing Hormone (LH) is a gonadotropin secreted by the anterior pituitary gland. In females, it triggers ovulation of a mature egg and stimulates the formation of the corpus luteum, which secretes progesterone and estrogen. In males, LH stimulates the interstitial cells (Leydig cells) of the testes to produce and secrete testosterone and other androgens.
What is Prolactin (PRL), and what is its primary function?
Prolactin (PRL) is a protein hormone secreted by the anterior pituitary gland. Its primary function is to promote milk production by the mammary glands following childbirth. While its most prominent role is in lactation, prolactin also influences reproductive function and immune responses in both males and females.
What is Adrenocorticotropic Hormone (ACTH), and what does it target?
Adrenocorticotropic Hormone (ACTH), also known as corticotropin, is a polypeptide hormone secreted by the anterior pituitary gland. Its main target is the adrenal cortex, where it stimulates the synthesis and secretion of glucocorticoid hormones, particularly cortisol, which play vital roles in the stress response and metabolism.
What is Oxytocin (OT), and what are its key physiological roles?
Oxytocin (OT) is a peptide hormone synthesized in the hypothalamus and released from the posterior pituitary gland. Its key physiological roles include stimulating strong uterine contractions during labor and promoting milk ejection (the 'let-down' reflex) from the mammary glands during breastfeeding. Oxytocin also plays a role in social bonding and parental behaviors.
What is Antidiuretic Hormone (ADH), and what are its main effects?
Antidiuretic Hormone (ADH), also known as vasopressin, is a peptide hormone synthesized in the hypothalamus and released from the posterior pituitary gland. Its main effects are to promote water reabsorption by the kidneys, thereby decreasing urine output and conserving body water, and in higher concentrations, to cause vasoconstriction, which helps to increase arterial blood pressure.
Describe the main functions of Thyroid Hormones (T3 and T4).
Thyroid hormones (triiodothyronine, T3, and thyroxine, T4) are lipid-soluble amine hormones secreted by the thyroid gland. They are crucial regulators of the body's basal metabolic rate (BMR), influencing caloric expenditure and heat production. They also play essential roles in regulating protein synthesis, promoting normal growth and development of the nervous, skeletal, and muscular systems, and enhancing the effects of catecholamines.
What is Calcitonin, and what is its role in calcium homeostasis?
Calcitonin is a peptide hormone secreted by the parafollicular cells (C cells) of the thyroid gland. Its primary role in calcium homeostasis is to lower high blood calcium (Ca^{2+}) levels. It achieves this by inhibiting the activity of osteoclasts (cells that break down bone), thereby decreasing bone resorption and promoting the deposition of calcium into bone tissue, helping to preserve bone mass.
What is Parathyroid Hormone (PTH), and how does it regulate calcium?
Parathyroid Hormone (PTH) is a peptide hormone secreted by the parathyroid glands. It is the most important regulator of blood calcium (Ca^{2+}) levels, acting to increase them when they fall below normal. PTH increases blood calcium by: \n1. Stimulating osteoclast activity to release Ca^{2+} from bone matrix. \n2. Increasing Ca^{2+} reabsorption from the kidneys back into the blood. \n3. Promoting the kidneys to synthesize calcitriol, which enhances dietary Ca^{2+} and phosphate absorption from the gastrointestinal tract. PTH secretion is regulated by a strict negative feedback loop based on blood Ca^{2+} concentrations.
What is Calcitriol (1,25-dihydroxyvitamin D), and what is its main function?
Calcitriol (1,25-dihydroxyvitamin D) is the active form of vitamin D. It is primarily produced by the kidneys in response to parathyroid hormone (PTH). Its main function is to significantly enhance the absorption of dietary calcium and phosphate from the gastrointestinal tract into the blood, thereby increasing blood calcium levels in coordination with PTH.
What is Aldosterone, and what is its role in electrolyte and fluid balance?
Aldosterone is a mineralocorticoid steroid hormone secreted by the adrenal cortex. It plays a critical role in regulating electrolyte balance, specifically by increasing the reabsorption of sodium (Na^{+}) ions and water back into the blood by the kidneys, and promoting the excretion of potassium (K^{+}) and hydrogen (H^{+}) ions in the urine. This action contributes significantly to the regulation of blood volume and blood pressure.
What are Glucocorticoids (e.g., Cortisol), and what are their primary functions?
Glucocorticoids, such as cortisol, are steroid hormones secreted by the adrenal cortex. They have diverse and vital functions including: \n1. Regulating metabolism by increasing blood glucose levels (gluconeogenesis), promoting the breakdown of proteins and lipids. \n2. Helping the body adapt to stress by ensuring sufficient energy supply. \n3. Suppressing inflammatory and immune responses. \n4. Maintaining blood pressure by enhancing the effects of other vasoconstrictors.
What are Adrenal Androgens, and what roles do they play?
Adrenal androgens are weak masculinizing steroid hormones (e.g., dehydroepiandrosterone, DHEA) produced by the adrenal cortex. In females, they contribute to libido and are converted into estrogens in other body tissues, especially after menopause. In males, their effects are usually masked by the much greater quantities of androgens produced by the testes, but they contribute to prepubertal development.
What is Epinephrine, and what is its role in the stress response?
Epinephrine (adrenaline) is an amine hormone secreted by the adrenal medulla. It is a key mediator of the 'fight-or-flight' response during acute stress. Its effects include increasing heart rate and contractility, dilating airways, increasing blood glucose levels (glycogenolysis and gluconeogenesis), and redirecting blood flow to skeletal muscles, preparing the body for immediate action.
What is Norepinephrine (from the adrenal medulla), and how does it contribute to the stress response?
Norepinephrine (noradrenaline) is an amine hormone secreted by the adrenal medulla alongside epinephrine. It also contributes significantly to the 'fight-or-flight' response, primarily by causing widespread vasoconstriction, which leads to increased peripheral resistance and elevated blood pressure, and by increasing the force of heart contractions.
What is Melatonin, and what is its main function?
Melatonin is an amine hormone primarily secreted by the pineal gland. Its production and release are stimulated by darkness and inhibited by light, establishing a clear circadian rhythm. Its main function is to help regulate the body's sleep-wake cycle (circadian rhythms) and promote feelings of sleepiness.
Describe the endocrine functions of the Pancreas.
The endocrine function of the pancreas is performed by the pancreatic islets (islets of Langerhans). These specialized cell clusters contain alpha cells, which secrete glucagon to raise blood glucose, and beta cells, which secrete insulin to lower blood glucose, thereby regulating metabolic homeostasis.
Describe the exocrine functions of the Pancreas.
The exocrine function of the pancreas is carried out by the acinar cells, which synthesize and secrete a pancreatic juice rich in digestive enzymes (e.g., amylase for carbohydrates, lipase for fats, proteases for proteins) and bicarbonate. These secretions are delivered via ducts to the duodenum to aid in the chemical digestion of food.
What is Insulin, and how does it regulate blood glucose?
Insulin is a protein hormone secreted by the beta cells of the pancreatic islets. Its primary function is to lower elevated blood glucose levels. It achieves this by promoting the uptake of glucose by target cells (especially muscle and adipose tissue), stimulating the conversion of glucose into glycogen (glycogenesis) for storage in the liver and muscles, and promoting protein and fat synthesis.
What is Glucagon, and how does it regulate blood glucose?
Glucagon is a protein hormone secreted by the alpha cells of the pancreatic islets. Its primary function is to raise low blood glucose levels (hypoglycemia). It acts mainly on the liver to stimulate the breakdown of stored glycogen into glucose (glycogenolysis) and the synthesis of new glucose from non-carbohydrate sources (gluconeogenesis), releasing glucose into the bloodstream.
What is the primary hormone of the Testes, and what are its key functions?
The primary hormone produced by the testes is testosterone, a steroid androgen hormone. It drives the development and maturation of male reproductive organs, promotes spermatogenesis (sperm production), and stimulates the development and maintenance of male secondary sex characteristics (e.g., facial hair, deepened voice, increased muscle mass). The testes also produce inhibin, which inhibits FSH secretion.
Name the primary hormones produced by the Ovaries and their functions.
The ovaries produce several key steroid hormones: \n1. Estrogen: Responsible for the development of female secondary sex characteristics and regulates the female reproductive cycle, including uterine lining growth. \n2. Progesterone: Works with estrogen to regulate the menstrual cycle, maintain pregnancy by preparing the uterus, and develop mammary glands for milk production. \n3. Inhibin: A protein hormone that selectively inhibits the secretion of Follicle-Stimulating Hormone (FSH) from the anterior pituitary, helping to regulate gamete production.
What are secondary endocrine organs, and why are they important?
Secondary endocrine organs are organs that are not traditionally considered primary endocrine glands, but they nonetheless produce and secrete hormones as part of their broader physiological roles. They are important because they contribute significantly to the overall endocrine regulation of the body, often integrating with other organ systems.
Provide examples of secondary endocrine organs and the hormones they produce.
Examples of important secondary endocrine organs and their hormones include: \n- Kidneys: Produce Erythropoietin (EPO), Renin, and Calcitriol. \n- Adipose tissue: Produces Leptin and Adiponectin. \n- Heart: Produces Atrial Natriuretic Peptide (ANP). \n- Gastrointestinal tract: Produces numerous hormones such as gastrin, secretin, cholecystokinin, and ghrelin. \n- Thymus: Produces thymosins.
What is Renin, and what is its role particularly from the kidneys?
Renin is an enzyme secreted by the juxtaglomerular cells of the kidneys, primarily in response to decreased blood pressure, reduced blood volume, or low sodium levels. Renin initiates the Renin-Angiotensin-Aldosterone System (RAAS), leading to the production of angiotensin II and aldosterone, which together act to increase blood pressure and fluid volume.
What is Erythropoietin (EPO), and what is its main function?
Erythropoietin (EPO) is a glycoprotein hormone primarily secreted by the kidneys (and liver to a lesser extent), especially in response to hypoxia (low blood oxygen levels). Its main function is to stimulate erythropoiesis, the production of red blood cells in the red bone marrow, thereby increasing the oxygen-carrying capacity of the blood.
What is Leptin, and what is its role in metabolism?
Leptin is a protein hormone produced predominantly by adipose (fat) tissue. It acts on receptors in the hypothalamus of the brain to signal satiety, thereby decreasing appetite and promoting an increase in energy expenditure. Leptin plays an important role in long-term energy balance and body weight regulation.
What is Adiponectin, and what are its beneficial metabolic effects?
Adiponectin is a protein hormone secreted by adipose tissue. Its beneficial metabolic effects include enhancing insulin sensitivity in target tissues like muscle and liver, promoting fatty acid oxidation, and exerting anti-inflammatory properties. Higher levels of adiponectin are generally associated with better metabolic health.
What is Growth Hormone-Releasing Hormone (GHRH)?
Growth Hormone-Releasing Hormone (GHRH), also known as somatocrinin, is a peptide hormone produced by the hypothalamus. Its function is to stimulate the somatotroph cells of the anterior pituitary gland to synthesize and secrete Human Growth Hormone (hGH).
What is Thyrotropin-Releasing Hormone (TRH)?
Thyrotropin-Releasing Hormone (TRH) is a small peptide hormone produced by the hypothalamus. Its primary function is to stimulate the thyrotroph cells of the anterior pituitary gland to synthesize and secrete Thyroid-Stimulating Hormone (TSH). TRH also stimulates prolactin (PRL) release.
What is Corticotropin-Releasing Hormone (CRH)?
Corticotropin-Releasing Hormone (CRH) is a peptide hormone produced by the hypothalamus. Its function is to stimulate the corticotroph cells of the anterior pituitary gland to synthesize and secrete Adrenocorticotropic Hormone (ACTH), thereby initiating the stress response pathway.
What is Prolactin-Releasing Hormone (PRH)?
Prolactin-Releasing Hormone (PRH) is a hypothalamic hormone that stimulates the lactotroph cells of the anterior pituitary gland to secrete Prolactin (PRL). While not as clearly defined as other releasing hormones, several factors, including TRH, can act as PRH.
What are the structures of the endocrine system?(10)
Hypothalamus
Pituitary gland
Pineal gland
Thyroid gland
Parathyroid gland
Thymus
Adrenal Glands
Pancreas
Ovaries
Testes
Thyroid gland location
anterior to the upper part of the trachea near the larynx.
Thyroid hormones function
to maintain a proper metabolic rate, contribute to growth, and help minimi
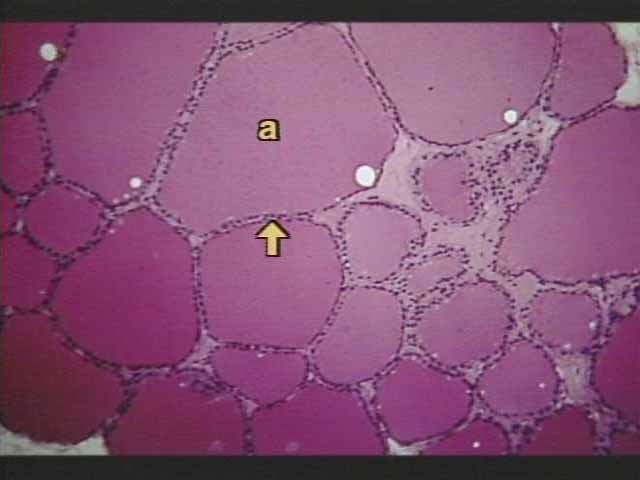
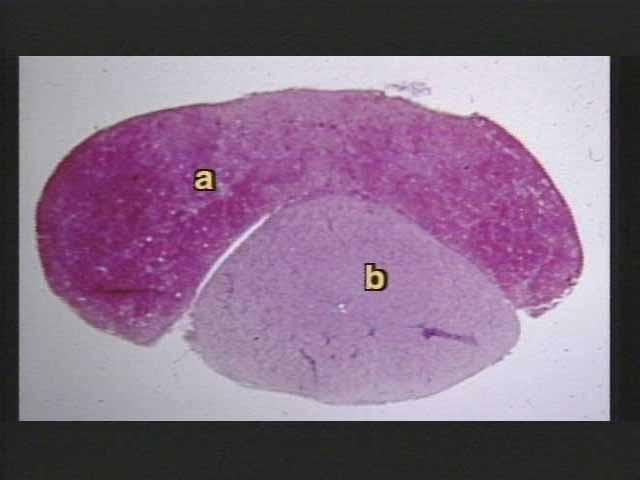
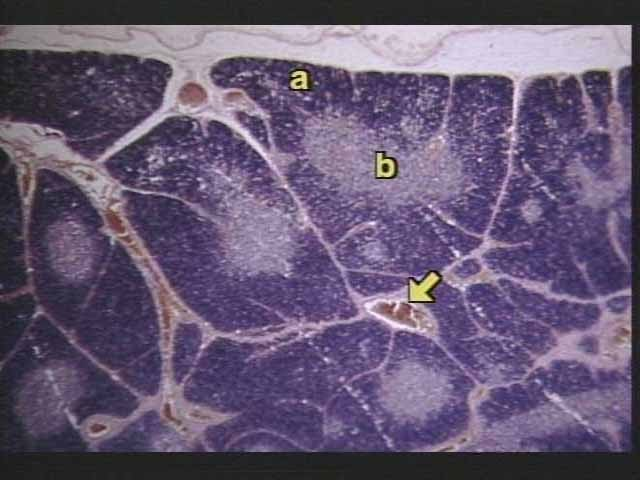
What is the structure labeled ‘a’?
thyroid tissue with thyroid follicles
What is the structure the arrow is pointing to?
follicular cells enclosing colloid.
The thyroid gland is divided into
right and left lobes
the right and left lobes of the thyroid are joined by
a thin band called the isthmus
hollow balls of cells called thyroid follicles are filled with a protein substance called
colloid - which stores thyroid hormones
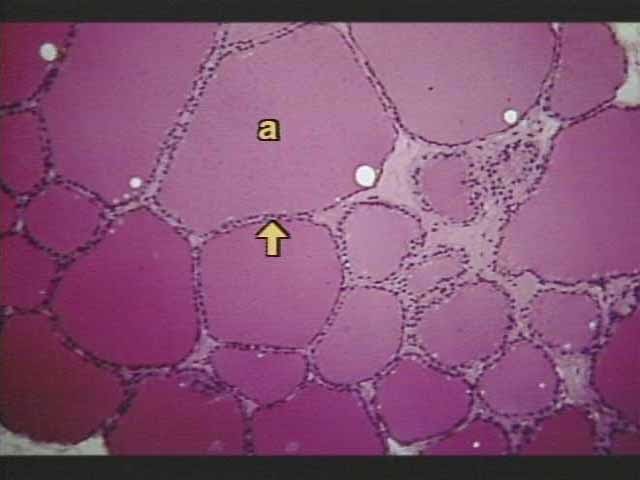
What is this image?
colloid filled follicles and follicle cells
Where are the parathyroid gland located?
They are 4 small glands on the dorsal surface of the thyroid.
Parathyroid function
Regulation of calcium levels in the blood
Adrenal glands location
Pair of endocrine glands on top of each kidney that produce hormones like adrenaline and cortisol.
Adrenal gland structures
outer adrenal cortex and adrenal medulla
The adrenal cortex has how many sublayers? What do they secrete?
3 - mineral corticoids, gluc
the inner adrenal medulla secretes
adrenalin and noradrenalin during alarm reactions
which adrenal structure is innervated?
the adrenal medulla
outermost layer of the adrenal cortex is called - and produces
zona glomerulosa - mineralocorticoids such as aldosterone.
name of middle layer of adrenal cortex
zona fasciculata - produces glucocorticoids such as cortisol.
deepest layer of adrenal cortex - secretes what?
zona reticularis - gonadocorticoids
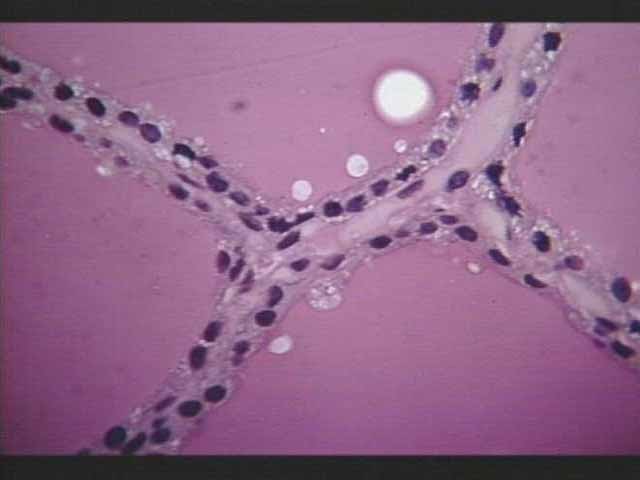
What does this image depict?
light micrograph of adrenal glands
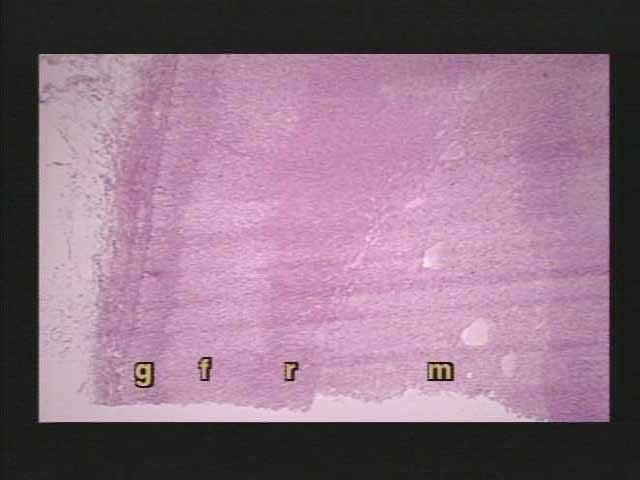
What do the letters g-f-r-m label here?
g. zona glomerulosa
f. zona fasci
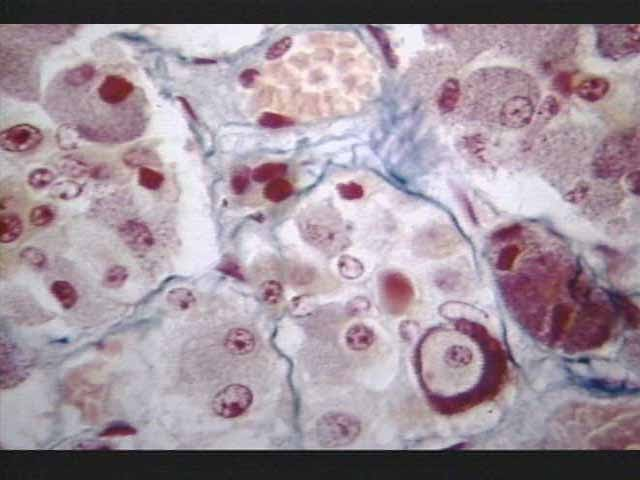
chromaffin cells
modified neurons in the adrenal medulla that secrete catecholamines
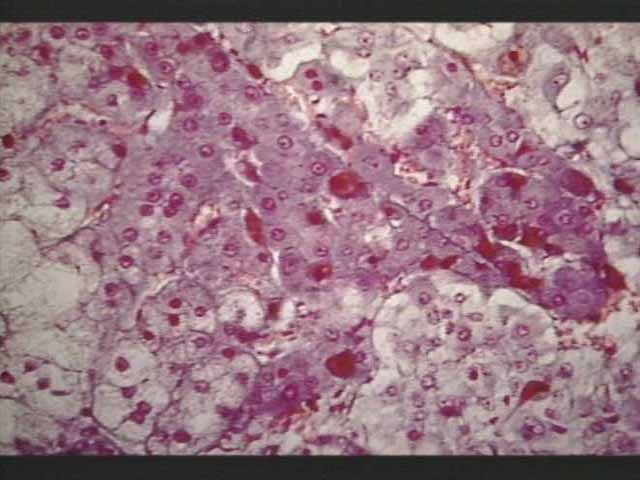
What does this image depict?
Chromaffin cells in the adrenal medulla
Where is the pituitary gland located?
the sella turcica of the sphenoid bone and is attached to the base of the hypothalamus by a stalk-like infundibulum.
The pituitary gland is attached to the hypothalamus by what strcuture?
the infundibulum
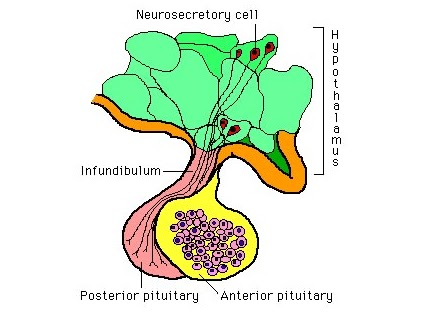
The pituitary is divided structurally and functionally into
a large anterior lobe and a smaller posterior lobe
The pituitary gland controls (master gland)
various hormonal functions, including growth, metabolism, and reproduction.
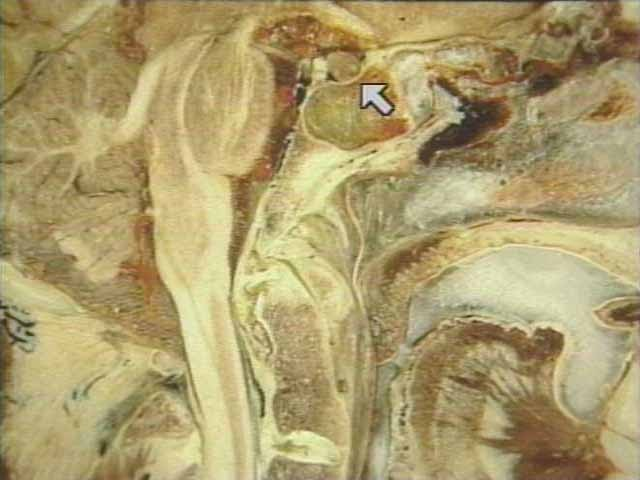
What is depicted in this photo?
Pituitary gland (arrow)
What is this photo?
Anterior (a) Posterior(b) lobes of the pituitary gland
What is this?
Magnified view of the anterior pituitary, showing the variety of cell types that compose the pituitary.
What is the islets of langerhans?
isolated clumps of endocrine cells surrounded by exocrine tissue in the pancreas
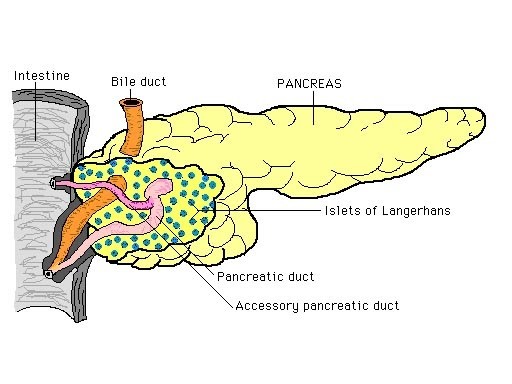
The solid yellow portion represents
the exocrine gland of the pancreas
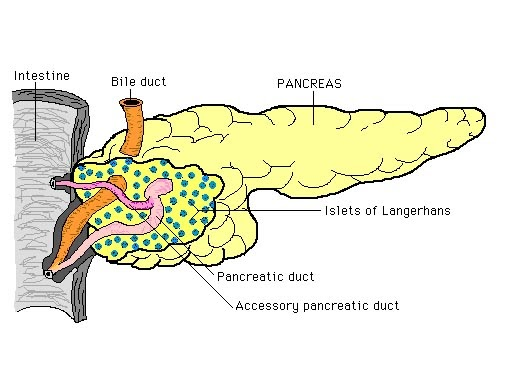
The dotted portion represents
the endocrine portion (islets of langerhans)
The exocrine portion of the pancreas secretes
pancreatic juice into the duodenum to help with digestion
the islets secrete
glucagon and insulin, which regulate blood sugar levels.
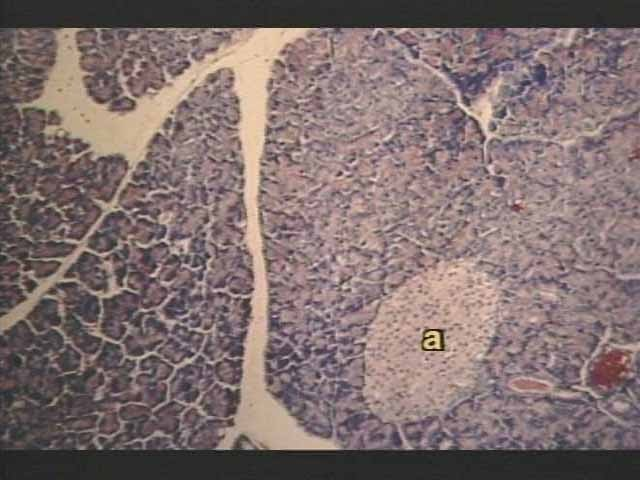
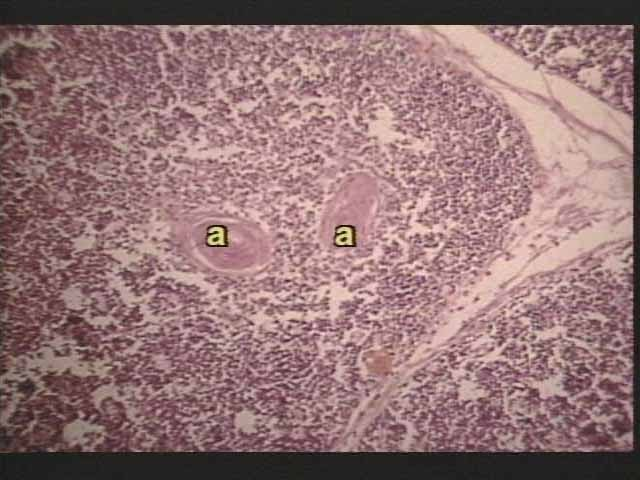
What is this?
Pancreas with Islets of Langerhans (a)
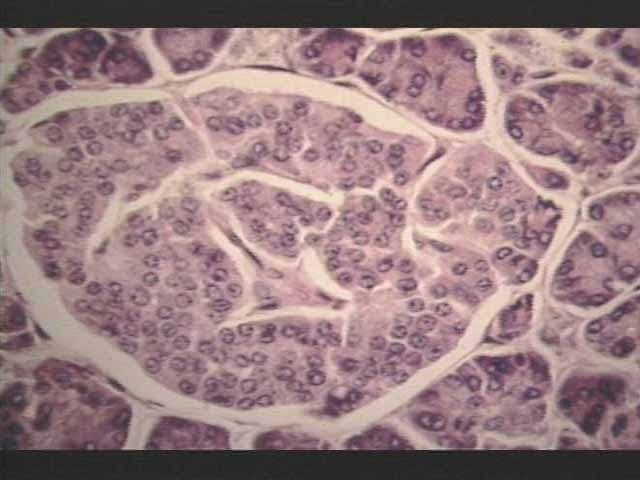
What is this?
Close up view of Islets of Langerhans
Thymus gland location
in the upper portion of the mediastinum, posterior to the sternum and between the lungs
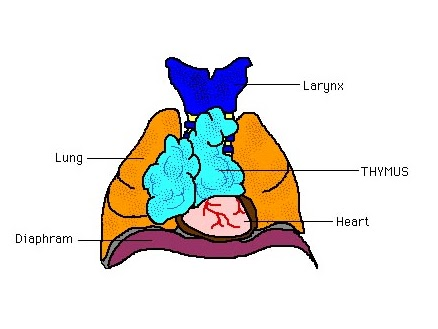
The thymus reaches maximum size during
childhood and then quickly atrophies
Thymus function
build resistance to disease
They thymus are made up of
lobules of thymus tissue which has a cortex and medulla
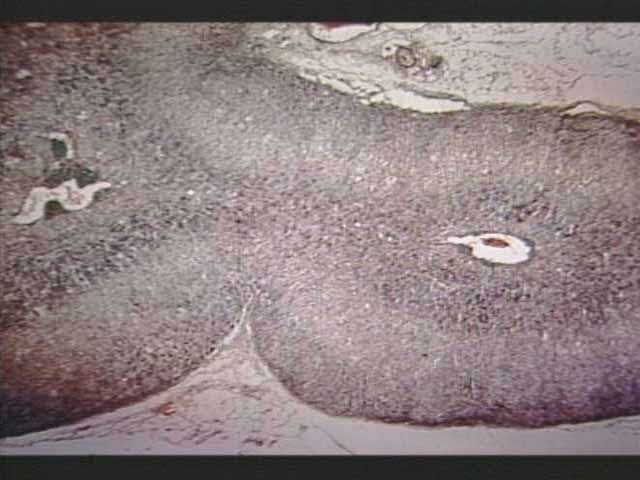
What is pictured?
The cortex (a) and medulla (b) of a thymic lobule
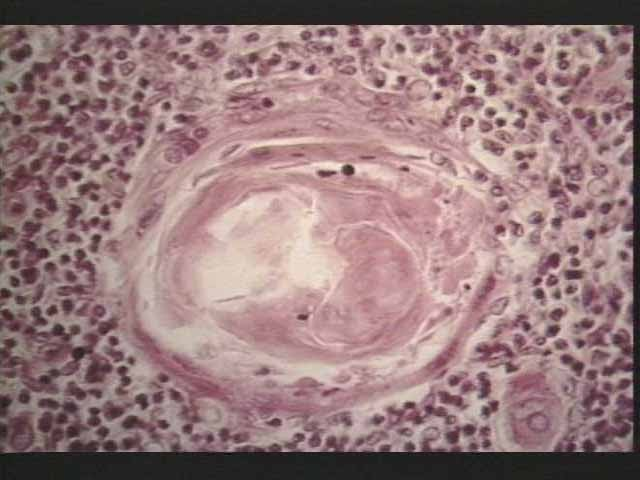
Whats this?
Close up of Hassall’s corpuslce
Hassalls corpuscle
structures within the thymus that play a role in T cell development and thymic regulation, often appearing as round formations in the thymic medulla.
Whats this
Close up of a thymic lobule with Hassalls’ corpuscles
Pineal gland
A small endocrine gland in the brain that produces melatonin, which regulates sleep-wake cycles.
The pineal gland is composed of
supportive neuroglia cells and secretory cells
Where is the pineal gland located?
The pineal gland is located near the center of the brain, between the two hemispheres, nestled in a groove where the two halves of the thalamus join.
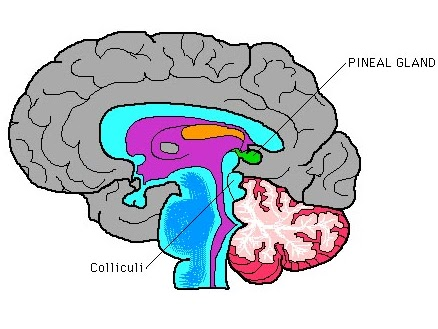
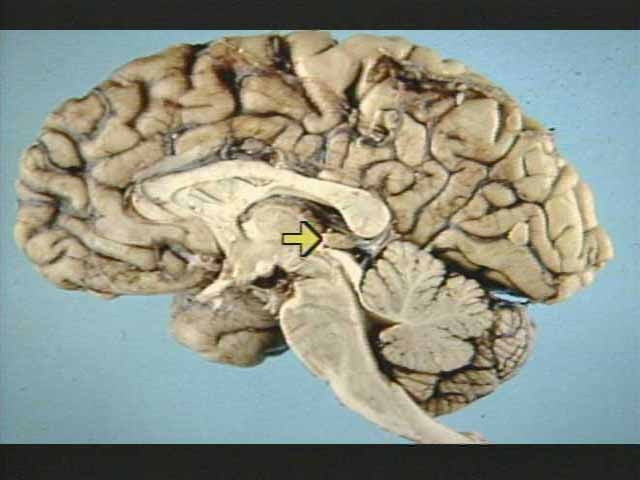
What is this arrow pointing to?
the pineal gland
Pancreas location
upper abdomen, behind the stomach and is situated in the curve of the duodenum, extending across the back of the abdomen.
The pancreas is comprised of
pancreatic ducts