RESPIRATORY SYSTEM
1/61
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
62 Terms
RESPIRATORY SYSTEM
Consists of nose, pharynx, larynx, trachea, bronchi, and lungs.
Functional Division of the Respi System
divided into the conducting zone and respiratory zone.
Structural division of the respi system
divided into the upper and lower respiratory system
Upper respiratory system
Nose, nasal cavity, pharynx, and associated structures
Lower respiratory system
larynx, trachea, bronchi, lungs
Conducting zone
Consists of a series of interconnecting cavities and tubes both outside and within the lungs.
These include the nose, nasal cavity, pharynx, larynx, trachea, bronchi, bronchioles, and terminal bronchioles;
their function is to filter, warm, and moisten air and conduct it into the lungs.
Respiratory Zone
Consists of tubes and tissues within the lungs where gas exchange occurs.
These include the respiratory bronchioles, alveolar ducts, alveolar sacs, and alveoli, and are the main sites of gas exchange between air and blood
Provides for gas exchange: intake of O2 for delivery to body cells and removal of CO2 produced by body cells
Helps regulate blood pH
Contains receptors for the sense of smell, filters inspired air, produces vocal sounds (phonation), and excretes small amounts of water and heat.
What are the functions of the respiratory system?
Nose
Consists of a visible external portion and an internal portion inside the skull called the nasal cavity.
The external nose is the portion of the nose visible on the face and consists of a supporting framework of bone and hyaline cartilage covered with muscle and skin and lined by a mucous membrane.
Pharynx
Throat
Funnel-shaped tube that starts at the internal nares and extends to the level of the cricoid cartilage, the most inferior cartilage of the larynx
Larynx
Voice box
Short passageway that connects the laryngopharynx with the trachea.
It lies in the midline of the neck anterior to the esophagus and the fourth through sixth cervical vertebrae
Trachea
Located anterior to the esophagus and extends from the larynx to the superior border of the fifth thoracic vertebra
Divides into right and left primary bronchi
Bronchi
Superior border of 5th thoracic vertebra
Divides into right and left primary bronchus
Divides into lobar bronchi
Continues to branch into the segmental bronchi
Divides into bronchioles then into terminal bronchioles
Alveoli
Cup-shaped out-pouching lined by simple squamous epithelium and supported by a thin elastic basement membrane
An alveolar sac consists of two or more alveoli that share a common opening
Pulmonary ventilation
External (pulmonary) respiration
Internal (tissue) respiration
What are the basic steps of respiration?
Pulmonary ventilation
Moving air in and out of lungs
External (pulmonary) respiration
Gas exchange between alveoli and blood
Pulmonary capillary blood gains O2 and loses CO2.
Internal (tissue) respiration
Gas exchange between blood and cells
Blood loses O2 and gains CO2
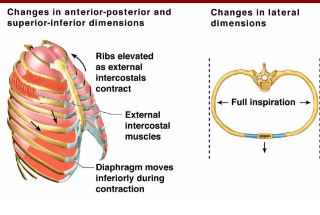
Inhalation
Inspiration/ Breathing in
For air to flow into the lungs, the pressure inside the alveoli must become lower than the atmospheric pressure.
Increases size of lungs
Primary: Diaphragm, External Intercostal
Accessory: Scalenes, SCM, Upper Trapezius, Pectoralis Major/Minor
Exhalation
Expiration/ Breathing out
The pressure in the lungs is greater than the pressure of the atmosphere
Normal exhalation during quiet breathing, unlike inhalation, is a process because no muscular contractions are involved
Results from elastic recoil of the chest wall and lungs
Primary: Passive recoil
Accessory: Abdominalis, Internal intercostals
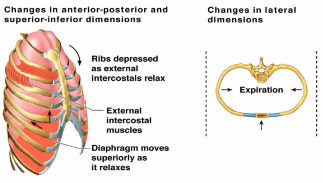
THORACIC CAGE MECHANISM
Movement of the ribcage
Pump Handle Motion
Sternum and Ribs 1-6
Superior/anterior (inhalation)
Inferior/posterior (exhalation)
Bucket Handle Motion:
Ribs 7-10
lateral/superior (inhalation)
medial/inferior (exhalation)
Caliper motion
Ribs 8-12
lateral (inhalation)
medial (exhalation)
surface tension of alveolar fluid
compliance of the lungs
airway resistance
What are the factors affecting pulmonary ventilation?
Surface tension of Alveolar Fluid
Coats the luminal surface of alveoli and exerts a force known as surface tension.
Compliance of the Lungs
How much effort is required to stretch the lungs and chest wall
High = expand easily
Low = resist expansion
Airway Resistance
Rate of airflow through the airways depends on both the pressure difference and the resistance
Tidal Volume
Volume of air inspired or expired with each normal breath
about 500 milliliters in the adult male
Inspiratory reserve volume
extra volume of air that can be inspired over and above the normal tidal volume when the person inspires with full force;
about 3000 ml
Expiratory reserve volume
Maximum extra volume of air that can be expired by forceful expiration after the end of a normal tidal expiration;
about 1100 ml
Residual volume
volume of air remaining in the lungs after the most forceful expiration
about 1200 ml
Inspiratory capacity
Amount of air a person can breathe in, beginning at the normal expiratory level and distending the lungs to the maximum amount
about 3500 ml
Functional residual capacity
Air that remains in the lungs at the end of normal expiration
about 2300 ml
Vital Capacity
Maximum amount of air a person can expel from the lungs after first filling the lungs to their maximum extent and then expiring to the maximum extent
about 4600 ml
Total lung capacity
maximum volume to which the lungs can be expanded with the greatest possible effort
about 5800 ml
Pleural pressure
“Intrapleural pressure”
the pressure of the fluid in the thin space between the lung pleura and the chest wall pleura.
This is normally a slight suction, which means a slightly negative pressure.
The normal pleural pressure at the beginning of inspiration is about -5 centimeters of water,which is the amount of suction required to hold the lungs open to their resting level.
Alveolar pressure
Intrapulmonic pressure”
the pressure of the air inside the lung alveoli.
When the glottis is open and no air is flowing into or out of the lungs, the pressures in all parts of the respiratory tree, all the way to the alveoli, are equal to atmospheric pressure, which is considered to be zero reference pressure in the airways that is, 0 centimeters water pressure.
Transpulmonary pressure
the difference between the alveolar pressure and the pleural pressure
measure of the elastic forces in the lungs that tend to collapse the lungs at each instant of respiration, called the recoil pressure.
OXYGEN TRANSPORT
Transported from the lungs to peripheral tissues by the hemoglobin that is densely packed in our red blood cells.
RELATIONSHIP BETWEEN HEMOGLOBIN AND O2 PARTIAL PRESSURE
The more oxygen partial pressure (PO2), the more oxygen combines with Hemoglobin (Hb).
Dissolved CO2
The smallest percentage about 7% is dissolved in blood plasma. On reaching the lungs, it diffuses into alveolar air and is exhaled.
Carbamino compounds
A somewhat higher percentage, about 23%, combines with the amino groups of amino acids and proteins in the blood to form carbamino compounds
Bicarbonate ions
The greatest percentage of CO2– about 70%- is transported in blood plasma as bicarbonate ions.
CO2 diffuses into systemic capillaries and enters red blood cells, it reacts with water in the presence of the enzyme carbonic anhydrase to form carbonic acid, which dissociates into H+ and HCO3
Dorsal root ganglion
previously known as “inspiratory area”
For inspiration
Location: Dorsal Medulla (Nucleus Tractus Solitarius)
Responsible for inspiratory ramp signal
2 seconds on
3 seconds off
Ventral root ganglion
formerly known as “expiratory area”
for expiration and inspiration, but its mainly for expiration
Location: Ventrolateral Medulla
PONTINE RESPIRATORY GROUP
Pneumotaxic center
Apneustic Center
Pneumotaxic center
limits inspiration by switching off the inspiratory ramp signal
Location: Upper pons
Controls rate and depth of breathing
Controls inspiratory time
Apneustic Center
Prolongs inspiration by preventing the switching off the inspiratory ramp signal
Location: Lower pons
Limbic system stimulation
anticipation of activity or emotional anxiety may stimulate the limbic system, which then sends excitatory input to the DRG, increasing the rate and depth of breathing
Temperature
Body ____ ↑ = Rate of breathing ↑
Body _____ ↓ = Rate of breathing ↓
A sudden cold stimulus causes temporary apnea, an absence of breathing.
Pain
A sudden, severe ___ brings about brief apnea, but prolonged somatic___ increases breathing rate.
Visceral ___ may slow the rate of breathing
Stretching the anal sphincter muscle
Increases the breathing rate and is sometimes used to stimulate respiration in a newborn baby or a person who has stopped breathing.
Irritation of airways
Physical or chemical irritation of the pharynx or larynx brings about an immediate cessation of breathing followed by coughing or sneezing.
Blood pressure
The carotid and aortic baroreceptors that detect changes in blood pressure have a small effect on breathing.
A sudden rise in _______ decreases the breathing rate, and a drop in _________ increases the breathing rate.
Chest symmetry- Upper lobes
Thumbs: sternal notch
Fingers: Above the clavicle
Chest symmetry- Right Middle Lobe and Lingula
Thumbs: Xiphoid process
FIngers: Lateral ribs
Chest symmetry- lower lobes
Thumbs: Lower thoracic spine
Fingers: Lateral ribs
HEART RATE
Resting _____= lowest amount of blood you need because you’re not exercising
normally 60-100 bpm
BLOOD PRESSURE
Measurement of pressure in an artery at the peak of systole and during diastole and is measured in mmHg
Normal: 120/80 mmHg
PULSE RATE
Number of heartbeats per minute.
Resting pulse rate = 60-80bpm
RESPIRATORY RATE
Number of breaths per minute
Number of movements indicative of inspiration and expiration per unit time
Count the number of themes the chest rises or falls per minute