Breast
1/67
Earn XP
Description and Tags
Chapter 21 page. 643 - DONE
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
68 Terms
Female sex
• Increasing age
• Family history of breast cancer
• Personal history of breast cancer
• First-degree relative (mother, sister, daughter)
• Premenopausal breast cancer
• Multiple affected first- and second-degree relatives
• Associated cancers (ovarian, colon, prostate)
• Biopsy-proven atypical proliferative lesions
• Lobular neoplasia (lobular carcinoma in situ)
• Atypical epithelial hyperplasia
• Prolonged estrogen effect
• Early menarche
• Late menopause
• Nulliparity
• Late first pregnancy
Risk Factors for Breast Cancer
Breast Cancer Facts
👩⚕ 1 in ____ American women will develop breast cancer.
🎯 It's the most common cancer among U.S. women.
⚠ It's the 2nd leading cause of cancer death in women aged 40–59.
🧬 Lifetime risk is around 12%.
8
🥇 Mammography = gold standard
📈 But sonography is gaining ground, especially:
In younger women
🧱 With dense breast tissue
🤰 During pregnancy/lactation
🖼 Mammogram vs. Sonogram
Palpable lump in women under 30 or during pregnancy
❓ Questionable mammogram results
🧪 Check on breast implants
🧱 Dense breast tissue
📆 Monitor benign lumps over time
🧫 Check lymph nodes in armpit
🧭 Guide procedures like biopsies
🎯 Help with planning radiation therapy
👨⚕ Evaluate male breasts
🚫 If mammogram isn't possible or recommended
✅ Top 10 Reasons for Breast Ultrasound
A ______________ is an X-ray picture of the breast.
It’s used to look for signs of breast cancer — even before you feel a lump.
🛠 How it works:
👉 Your breast is gently pressed between two plates (yes, it can feel a little squishy 😅).
📷 An X-ray machine takes images from different angles.
👨⚕ A doctor (radiologist) looks at the images to check for anything unusual.
🎯 Why it's important:
🕵♀️ Finds cancer early, sometimes years before symptoms show.
📅 Usually done every 1–2 years starting at age 40–50, depending on your risk factors.
Mammogram
🍼 Main Job of the Breast
The primary function of the female breast is to produce milk to feed a baby (👶) — this process is called lactation.
🧬 How Milk is Made & Moved
🧃 Milk is made in the acini (tiny milk-making sacs).
🚚 Then, it's carried through ducts to the nipple.
👩🔬 Two Important Cell Types
Luminal cells 🧪 → Make the milk.
Myoepithelial cells 💪 → Squeeze to help push milk out.
🧱 What's Inside the Breast?
🧈 Fat (for shape)
🧵 Ligaments (for support)
🧬 Glandular tissue (makes milk)
🛣 Ducts (carry the milk)
📍 Many breast problems (like lumps or cancer) start in the ducts.
🔁 Hormone Effects
The breast changes with:
📆 Menstrual cycle
🤰 Pregnancy
🤱 Lactation (breastfeeding)
🧒 Breast Development
Starts before your first period (🩸) and continues until around age 16.
Estrogen helps the duct system grow.
🤰 During Pregnancy
👶 The breast prepares to make milk:
Estrogen, progesterone, prolactin work together.
🧪 Prolactin (from the pituitary gland) makes the acini produce milk.
🚫 Milk is held off by high progesterone during pregnancy.
👶 After Birth
🧸 Placenta is expelled → progesterone drops.
🍼 Milk production starts.
👶 Baby suckling triggers:
🧠 Oxytocin (from the brain) → helps squeeze milk out.
📈 More prolactin → makes more milk!
🛡 Fun Fact
Full breast development (during lactation) may lower the risk of breast cancer a little.
🧼 What Is the Breast, Really?
It’s a modified sweat gland 😅 located in the upper chest area (anterior chest wall).
Imaging Note
Dense or milk-filled breasts = 📷 harder to see on a mammogram.
That’s why they usually wait 6+ months after breastfeeding ends to do one.
Physiology of the breast
🧭 Where the Breast Is Located
🧍♀ Breast tissue sits between:
2nd–3rd rib (superiorly)
6th–7th rib cartilage (inferiorly)
Sternum (middle)
Side/armpit (anterior axillary line)
👉 Some breast tissue extends into the armpit — this is called the axillary tail or tail of Spence.
🔘 Surface Structures
👶 Nipple (center)
🟤 Areola (pigmented area around nipple)
🧬 Some people may have:
Extra breast tissue (ectopic)
Extra nipples (accessory)
These often form along the milk line (from armpit to groin)
📸 Ultrasound View: 3 Main Layers
Subcutaneous layer (just under the skin)
Mammary/glandular layer (milk-producing part)
Retromammary layer (deepest layer, near chest muscle)
🧈 Fat & Tissue Appearance
🟡 Fat = hypoechoic (dark on ultrasound)
⚪ Ducts, glands, ligaments = echogenic (bright)
🏗 Mammary/Glandular Layer (Main Milk-Making Part)
Has 15–20 lobes → like spokes on a wheel
Most lobes are in the upper outer quadrant (🔍 why most tumors are found there)
Each lobe branches into:
🌿 Lobules
🍇 Acini (milk glands)
Acini + ducts = TDLUs (Terminal Ductal Lobular Units)
🔍 This is where most breast diseases start
🧵 Supportive Structures
Tissue between lobes = stroma (connective + fat)
🕸 Cooper’s ligaments:
Connect everything like a web
Help keep breast shape
Show up as bright lines on ultrasound
💻 How Everything Looks on Ultrasound
📍 Skin line, nipple, and retromammary layer = bright echoes
🧼 Areola = slightly darker than nipple/skin
🌫 Nipple = mixed bright/dark with shadowing
⚖ Echo Patterns Matter
Less fat = brighter image (more fibrous tissue)
More fat = mix of dark + bright areas
🔍 Important to tell normal fat from abnormal lumps
🧱 Retromammary Layer
Looks like the subcutaneous layer
Lies just above the chest muscles
💪 Chest Muscles (Behind the Breast)
Pectoralis major
Under the breast, attaches from sternum/clavicle to the upper arm
Forms the front border of the armpit
Pectoralis minor
Lies deeper, connects ribs 3–5 to shoulder blade
🔍 Why Check the Whole Breast?
Even though most problems happen in the glandular tissue, it's important to:
Scan all the way to the chest wall
Make sure nothing is missed behind or around the breast
🧠 Breast Anatomy & How It Looks on Ultrasound
🧍♀ Everyone’s Breast Tissue Is Different
🔄 Breast size & shape changes with:
📆 Menstrual cycle
🤰 Pregnancy
🤱 Breastfeeding
🧓 Menopause
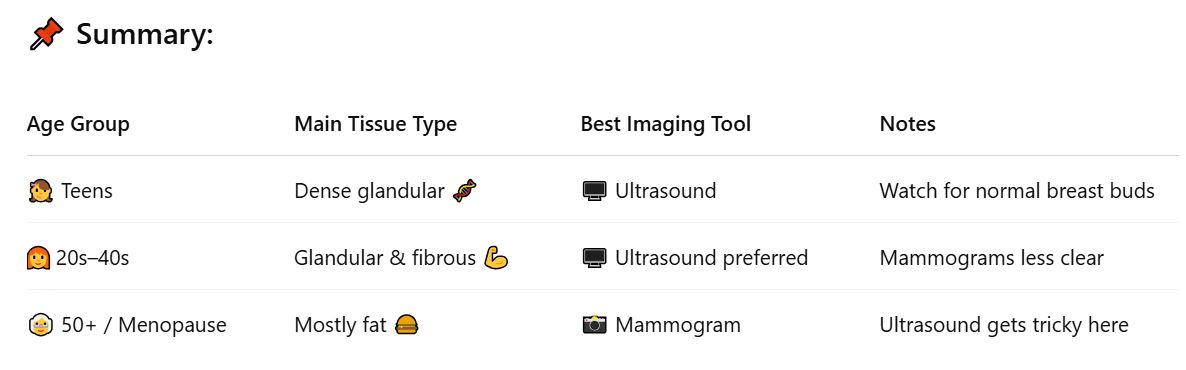
🧒 Young Women (Under 30)
💪 Mostly fibrous tissue → appears dense & bright on imaging (especially ultrasound)
⚠ Common “lump” = breast bud behind nipple (totally normal during puberty, not a tumor!)
📸 Ultrasound is the go-to imaging method for women under 30
👩🦰 Reproductive Age (20s–40s)
🧬 Breasts have distinct mammary layers due to active glandular tissue
📷 Mammograms are less useful in younger women with dense breasts
💻 Ultrasound is usually better for clear imaging in this group
🧓 Older Women & Menopause
🧠 Involution happens:
Glandular tissue dies (🧬➡💀)
Slowly replaced by fatty tissue (🍔)
🧓 After menopause:
Glands shrink (ducts atrophy)
Breast becomes mostly fat
All layers look darker (hypoechoic) on ultrasound
📷 Imaging Tips
💻 Fatty breasts = hard to see clearly with ultrasound
📸 BUT fatty breasts = easy to image on mammograms
🧬 Parenchymal Patterns = How Breast Tissue Looks Inside
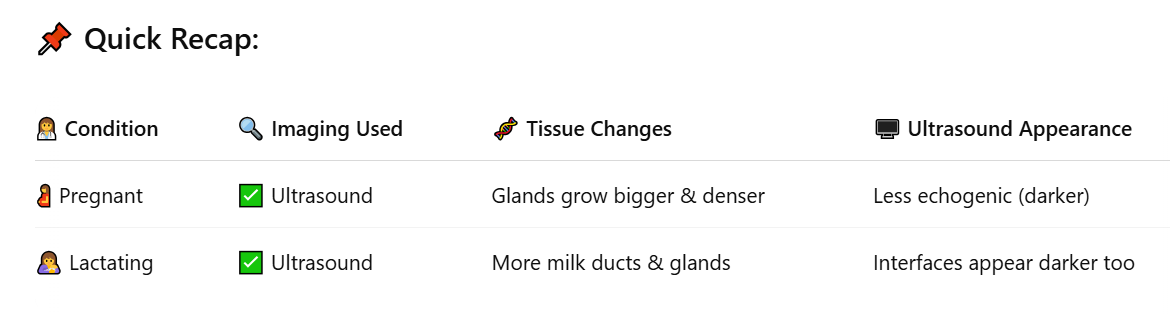
💻 Ultrasound is the MVP
For pregnant or breastfeeding women, sonography (ultrasound) is the #1 tool for breast imaging
📷 (Mammograms are usually avoided during pregnancy)
🔬 What Happens to the Breast?
🧬 Glandular tissue grows a lot (in both size and density)
⬆ This causes the breast to look less echogenic on ultrasound (meaning it's darker, less reflective)
🤰🤱 Breast Imaging During Pregnancy & Breastfeeding
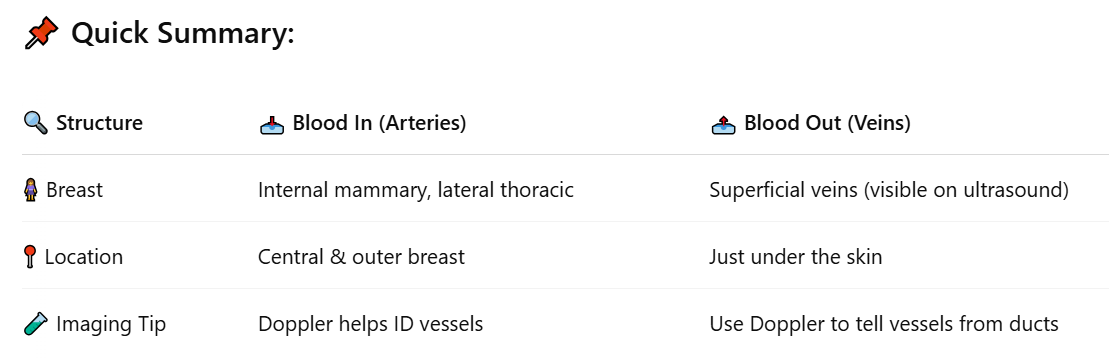
🩸 Arterial Supply = Blood To the Breast
💡 Main arteries:
Internal mammary artery → supplies central & inner breast (🔴 over half the breast!)
Lateral thoracic artery → supplies upper outer quadrant
➕ Other contributing arteries (smaller role):
Intercostal arteries
🧢 Subcapsular arteries
💪 Thoracodorsal arteries
🔄 Venous Drainage = Blood Out of the Breast
🩻 Veins follow arteries in deeper parts of the breast
💧Main drainage = superficial veins (close to the skin)
These can often be seen on ultrasound
May appear enlarged in:
⚠ Superior vena cava syndrome
🧵 Chronic venous clots (e.g. in subclavian vein)
💉 Dialysis patients with AV shunts
❓ Duct vs. Vessel?
👀 If you're unsure whether a black tube on ultrasound is:
A 🥛 dilated duct
OR a 🩸 blood vessel
✅ Use Color Doppler or vascular imaging to tell the difference (vessels show blood flow)
❤ Blood Flow to the Breast (Vascular Supply)
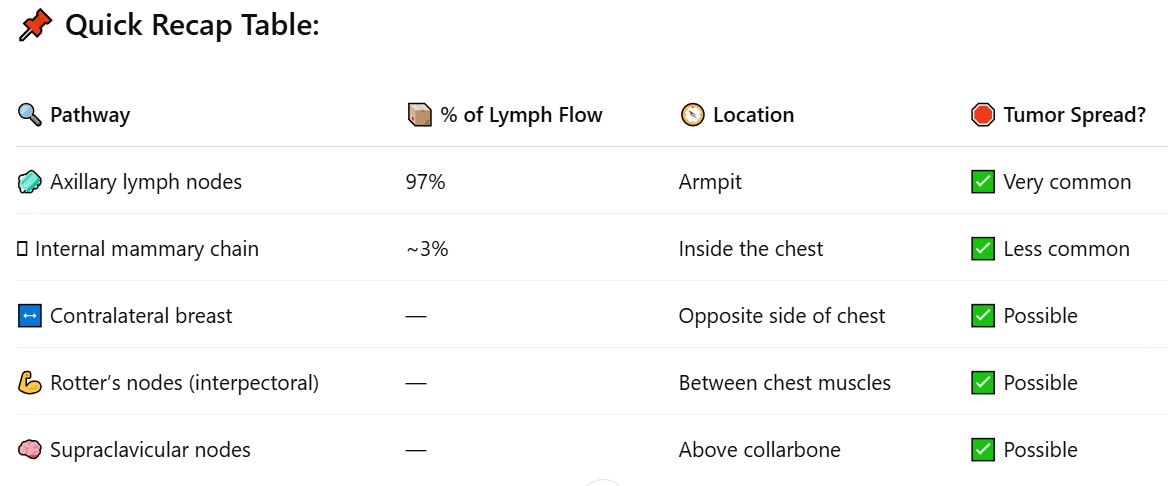
🔁 How Lymph Moves
Lymph = clear fluid that helps clean tissues & fight infection
🚫 Lymph vessels have no valves → fluid flows one way only:
➡ Superficial nodes → deep nodes
📍 Main Drainage Path
🧼 Most of the lymph (about 97%) drains to the axillary lymph nodes (in the armpit area)
🧪 Only about 3% drains to the internal mammary chain (inside the chest)
🛣 Lymph Flow Pathway
Starts in intramammary & deep nodes
Flows outward (centrifugally) ➡ toward:
🛑 Axillary lymph nodes (main route)
🛑 Internal mammary chain (small role)
⚠ Tumor Spread
Most breast tumors spread through the axillary nodes
But some can also spread to:
Internal mammary nodes (in chest)
↔ Across the midline to the opposite breast
💪 Interpectoral (Rotter’s) nodes (between chest muscles)
🧠 Supraclavicular nodes (above the collarbone)
🌊 Lymphatic Drainage = How Waste & Immune Fluid Leaves the Breast
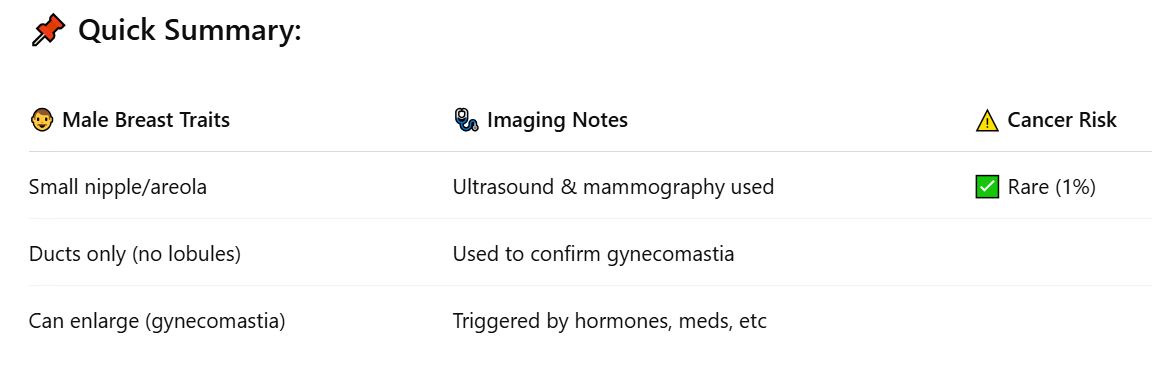
🔘 Anatomy Basics
👨🦱 Male nipple and areola = small
🔬 Male breasts have:
✅ Ducts under the nipple
❌ No lobules or acini (no milk-making parts)
📈 What Can Happen?
📉 Normally, duct tissue stays small
⚠ Sometimes it grows (hypertrophies) due to:
🔄 Hormonal changes (puberty, aging)
🧪 Certain diseases
💊 Medications
💥 This condition = Gynecomastia
📸 Imaging (mammogram & ultrasound) is used to:
Confirm it’s benign
✅ Rule out cancer
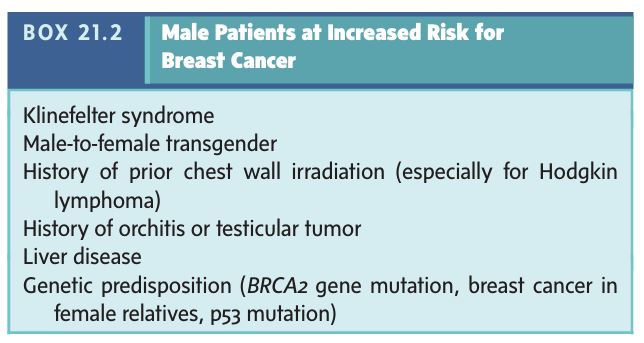
🎗 Male Breast Cancer
❗Rare, but it does happen
🇺🇸 ~1,300 new cases/year in the U.S.
📊 That’s about 1% of the number in women
The Male Breast
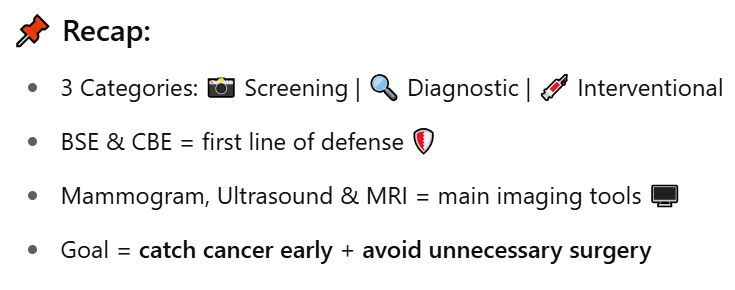
🧠 Breast Evaluation = 3 Main Categories
🔍 Breast Cancer Screening
→ Routine checks to catch cancer early
Tools: 👩⚕Physical exam + 📸 Mammography🧪 Diagnostic Interrogation
→ "Problem-solving" imaging when there's a symptom, lump, or concern
Tools: 💻 Ultrasound, 📸 Mammogram, 🧲 MRI💉 Interventional Breast Procedures
→ Taking tissue samples or placing markers
Purpose: Confirm diagnosis with histology or guide treatment
🎗 Why Screening Matters
🆙 Breast cancer cases are increasing worldwide
🚨 It’s now the #1 cancer killer in women (more than lung cancer)
🎯 Goal: Catch cancer early = most curable stage
✅ Screening = Detecting BOTH Cancer and Benign Lesions
🎗 Finding cancer early = lifesaving
⚖ Identifying non-cancerous lumps avoids unnecessary surgery and scarring
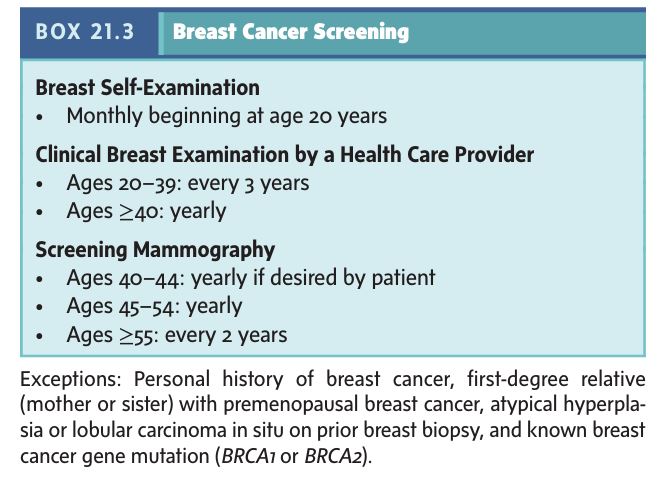
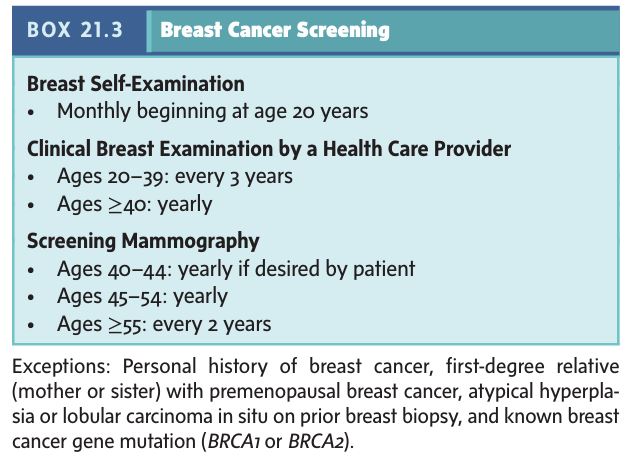
🧍♀ American Cancer Society Recommendations
🔄 Activity | 📅 When to Start | 📌 Frequency & Notes |
|---|---|---|
👋 Breast Self-Exam (BSE) | Age 20+ | Monthly, at the end of your period |
👩⚕ Clinical Breast Exam (CBE) | Age 20+ | Regularly by a doctor or nurse |
🧠 Fun Fact: 70% of breast cancers are found by feeling a lump during BSE or CBE!
Breast Evaluation
🖼
🟢 Recommended to start yearly at age 40
📸 Still the gold standard for breast cancer screening
✅ Detects cancer earlier than analog methods
🧠 Now done with digital mammography:
Better contrast
Image zoom/editing
Easier storage
No issue with breast size
🔍 3D Mammography (Tomosynthesis)
🆕 Newer tech = 3D breast images
📈 Improves detection, especially in:
🧑 Younger women
💪 Dense breasts (less fatty)
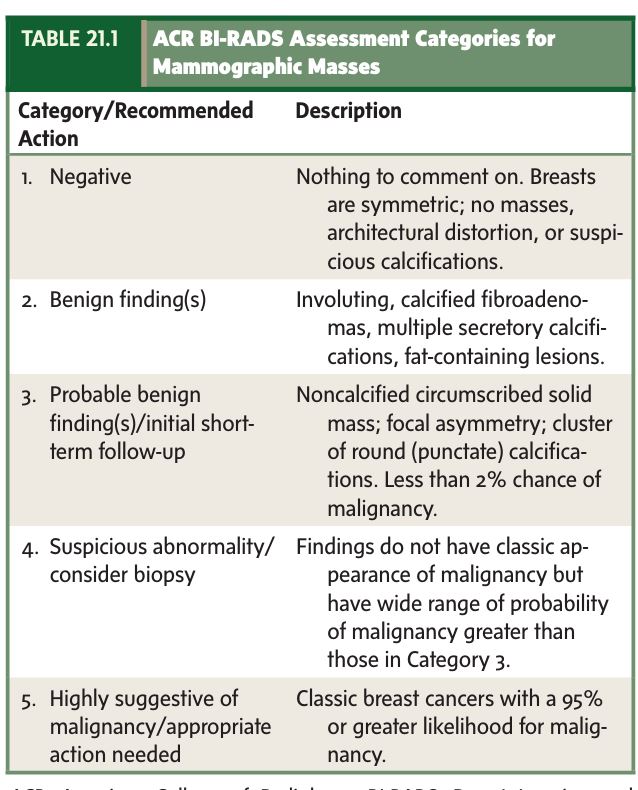
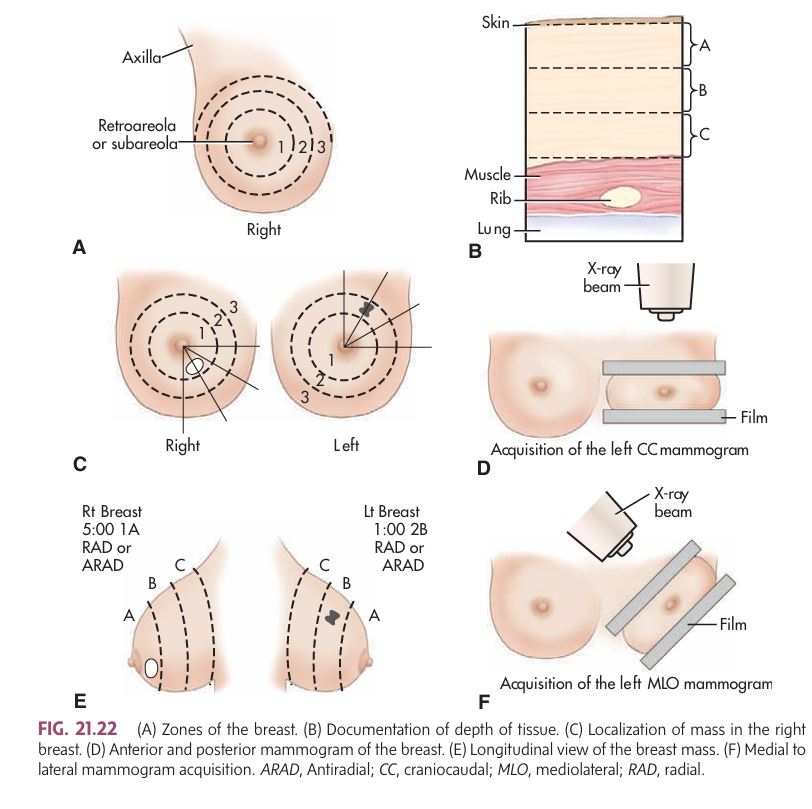
🗂 BI-RADS System
Created by the American College of Radiology (ACR)
📋 Standardized way to describe and rate breast findings
🔢 BI-RADS = includes categories for malignancy risk
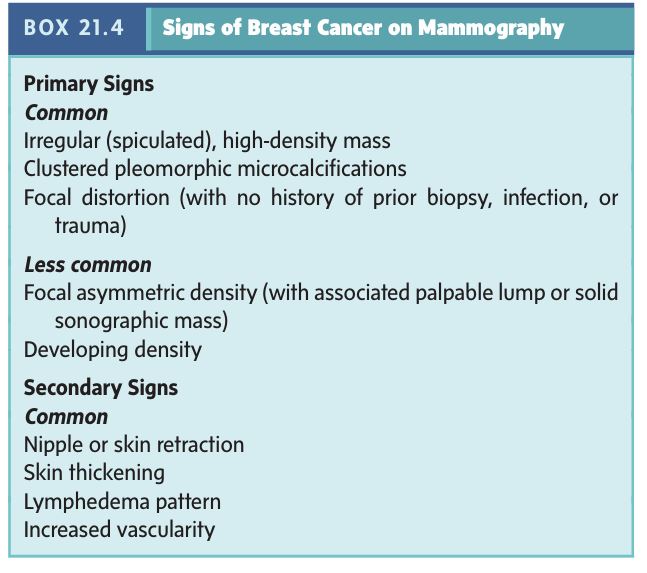
📸 Signs of cancer (see Box 21.4 in your text) can include:
Microcalcifications
Focal distortions
Masses
🩺 Diagnostic Interrogation (aka Problem-Solving Imaging)
Used when:
🤔 A lump or symptom is found by BSE or CBE
☎ A patient is recalled after an abnormal screening mammogram
✅ Involves:
🖼 Special mammogram views
🧪 Often paired with ultrasound (in ~1/3 of cases)
⚠ Challenges in Certain Patients
Some mammograms are harder to interpret due to:
🧱 Dense breast tissue
🫧 Breast implants
🧵 Scar tissue (from surgery or biopsy)
☢ Radiation or post-treatment changes
👉 Scars can look like cancer! Distortion = tough to evaluate
🤝 Ultrasound as a Helpful Partner
Used as an adjunct, not a replacement
📉 Ultrasound struggles with:
⚡ Microcalcifications
🔺 Subtle tissue distortion
👍 But it’s super helpful in:
Young patients
High-risk individuals
Cases with unclear mammogram findings (see Box 21.5)
🔬 Tissue Diagnosis Options
Used when:
😨 The patient is high-risk
📏 The mass is larger
🙅♀ The patient doesn’t want to wait for follow-up
🧪 Options include:
💉 Fine-needle aspiration (FNA)
🧵 Core needle biopsy
🌀 Vacuum-assisted biopsy
🪓 Surgical excisional biopsy
Screening Mammography

🎯 Goal: Properly classify any breast lesion based on how suspicious it is for cancer.
👩⚕ Decision-making depends on:
Imaging results (📸, 💻)
Clinical signs (palpable lump, nipple changes, etc.)
Patient’s age and risk factors
🧍♀ Clinical Assessment
🔍 Look for signs/symptoms of possible breast cancer:
Lump
Pain
Nipple discharge
Skin changes
🧪 If symptoms are present ➡ Diagnostic imaging is done
🧘 If no symptoms ➡ Regular screening mammogram first
🕵♀️ Diagnostic Breast Interrogation
Used when:
🖐 Lump is found during BSE or CBE
📞 Patient is called back after an abnormal mammogram
🔍 Includes:
Extra detailed mammogram views
🧪 In ~⅓ of cases, an ultrasound is added to help clarify things
💉 Interventional Breast Procedures
Used when imaging isn’t clear:
Ex: Mass looks benign but not a simple cyst
👉 Must confirm if it's solid or fluid-filled
🛠 Techniques include:
💧 Cyst aspiration: fluid = likely benign cyst
💉 Fine-needle aspiration (FNA): checks for cancer cells
🧵 Core needle biopsy: removes small tissue for testing
🧲 Wire localization: guides surgeons before biopsy
☢ Tracer injection: maps lymph nodes before surgery (sentinel node mapping)
🧩 Tricky Case: Lump with Normal Imaging
Imaging shows nothing but the patient feels a lump
Step 1: Monitor through at least one menstrual cycle
⏳ Most times, the lump goes away → fibrocystic change = benign
Step 2: If the lump stays or grows → surgical biopsy 🔍
🎯 Targeted vs. Whole Breast Scans
🔎 Targeted Scan | 🧭 Whole Breast Scan |
|---|---|
Scan just the area of concern | Scan the entire breast |
More specific and cost-effective | Can find unrelated issues (but more false-positives) |
Less likely to cause unnecessary worry | Best done with automated breast scanners |
🔁 Example: Mass seen in upper inner right breast ➡ Only that area gets scanned with ultrasound.
🩺 Breast Evaluation Overview
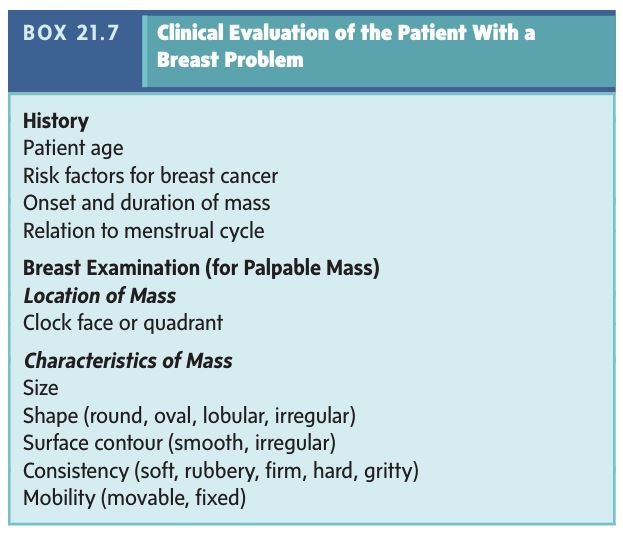
📋 What Info Do We Need Before the Exam?
✅ Patient's age
✅ Risk factors (like family history)
✅ Symptoms (like a lump or pain)
✅ Any breast surgeries or injuries 🚑
✅ Where the lump is (if there is one)
👀 What Should the Sonographer Look For?
During the scan or even just looking at the breast:
⚠ Skin issues like redness, thickening, or a dimpled (peau d’orange) appearance
⚠ Nipple changes: retraction (pulling inward), crusting, or unusual discharge
⚠ Scars, bruises, or inflammation
📸 When Is Ultrasound Used First?
Ultrasound is often the first imaging choice when:
👧 The patient is under 30 years old
🤰 She is pregnant or breastfeeding
💉 Has breast implants
🩻 A mammogram is hard to interpret
🛏 Patient Positioning During the Scan:
Lay on your back with your arm up over your head
Slightly roll to the opposite side for better imaging
If needed, other positions can be used (like upright) to help find a lump
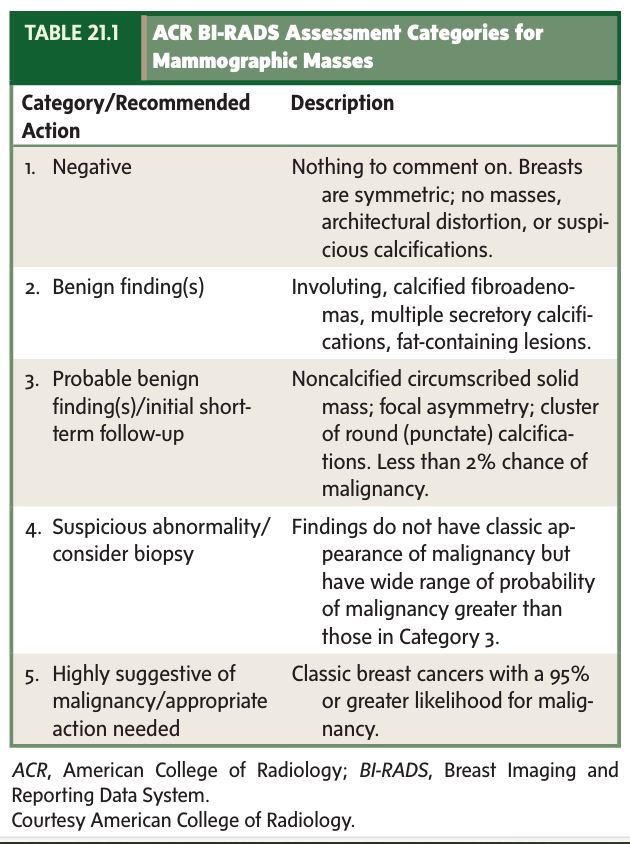
🧭 How the Scan Is Done:
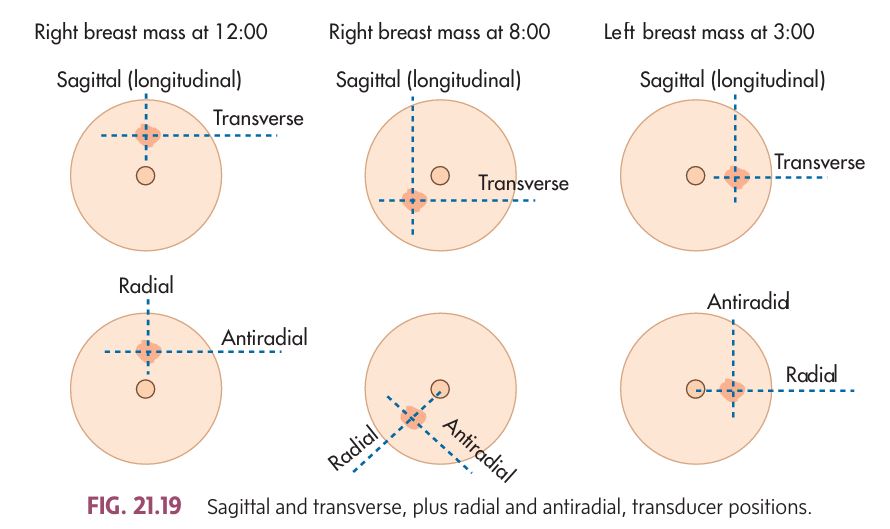
The tech uses a probe (transducer) and scans in 2 planes:
📍 Sagittal/Transverse (up/down and side-to-side)
📍 OR Radial/Antiradial (like spokes on a wheel, toward/away from the nipple)
💡 Use high-frequency settings for best image quality
They’ll record any masses in 3D measurements (length × width × height)
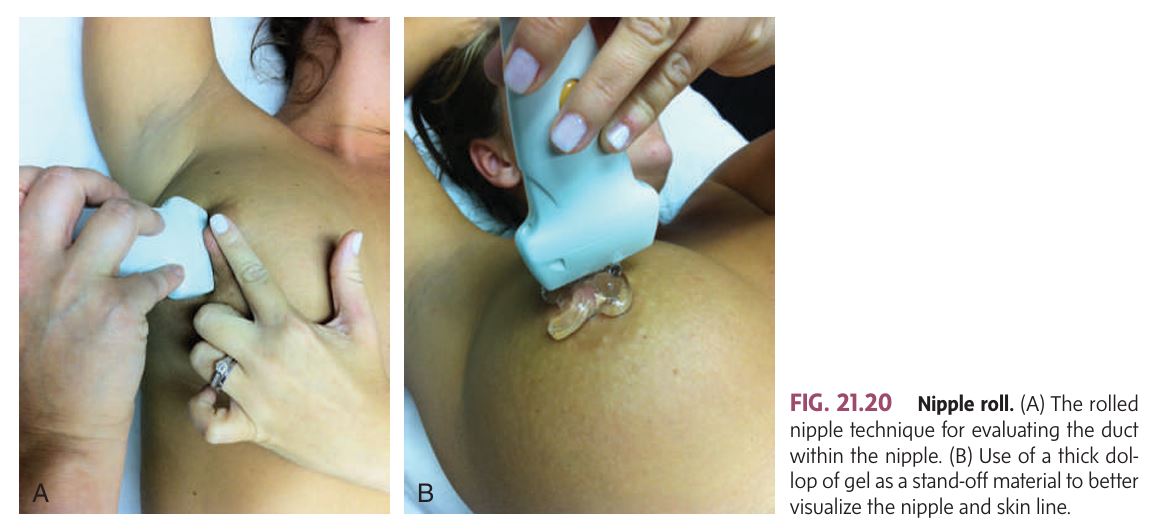
👃 Nipple & Skin Scanning Tips:
To scan behind the nipple, they may use the rolled nipple technique ➡ gently roll the nipple aside with a finger and the probe
If it's hard to see the top skin layer, they might use:
💦 A big blob of gel
🧽 A standoff pad (but not too thick, or image quality drops)
Sonographic Evaluation of the Breast
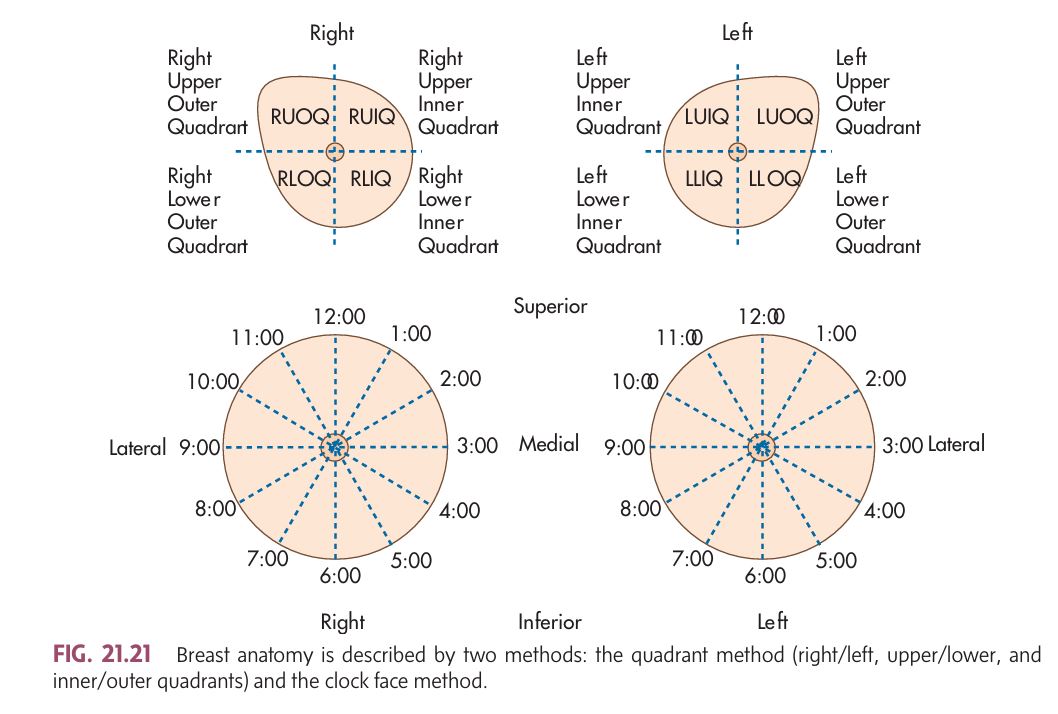
Sonographers need to label (annotate) images correctly to show where a lump or abnormality is found. There are 3 common systems used for this:
🕒 1. Clock Face Method
Think of the breast like a clock.
The nipple = center of the clock.
Every location is marked based on time ⏰:
🕛 12 o'clock is straight up from the nipple.
🕒 3 o'clock is:
Right medial breast
Left lateral breast
🕕 6 o'clock is straight down.
🕘 9 o'clock is:
Right lateral
Left medial
The scan is done radially, like the hands of a clock 📍.
🔲 2. Quadrant Method
Divide the breast into four parts:
✅ Upper Outer (UOQ)
✅ Upper Inner (UIQ)
✅ Lower Outer (LOQ)
✅ Lower Inner (LIQ)
You can scan in:
🔹 Longitudinal/Transverse
🔹 Radial/Antiradial
🔢🔠 3. 123-ABC Method (for Precise Location)
Used with the clock or quadrant method:
🔢 "123" = Distance from the nipple:
1 = Closest to the nipple
2 = Mid-breast
3 = Peripheral (far from nipple)
🔠 "ABC" = Depth of the mass:
A = Subcutaneous (just under the skin)
B = Mammary layer (glandular zone)
C = Retromammary layer (deepest, near the chest wall)
🧠 Example:
Lt. 2:00 3C = Left breast, 2:00 position, far from nipple, deep near the chest wall.
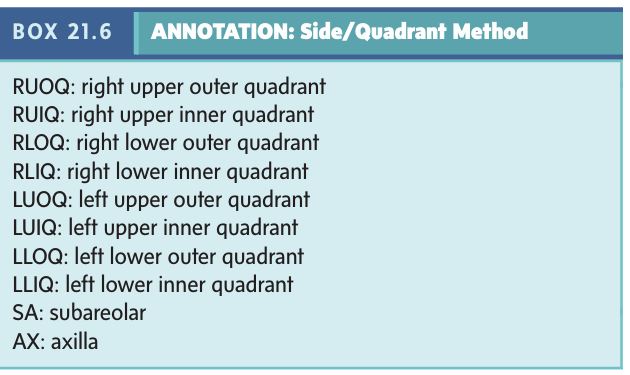
🔁 RAD vs. AR
RAD (Radial) = Scan follows the ducts toward nipple
AR (Antiradial) = Scan is across the ducts
🎯 Important because cancers often grow along ducts, so radial orientation helps catch them early.
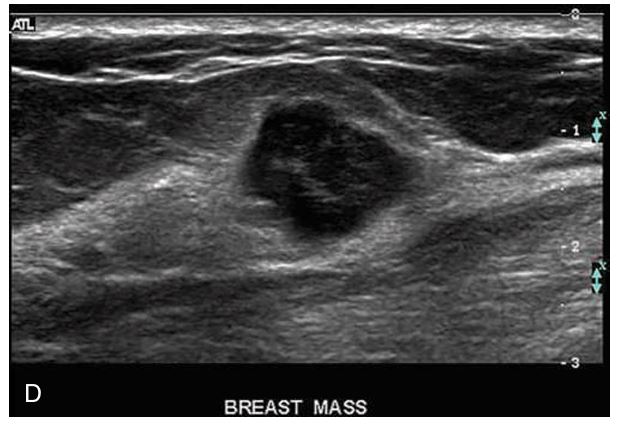
🧪 Characterizing a Solid Breast Mass
Sonography helps figure out whether a mass is probably benign or probably malignant. But 🛑 it's not a substitute for biopsy if results are unclear.
🧠 What to look at:
📏 Margins – are they smooth or jagged?
🔷 Shape – round, oval, or irregular?
↕ Orientation – wider than tall? Or taller than wide (riskier)?
🌫 Echo pattern – is the mass darker (hypoechoic), mixed, etc.?
🌀 Mobility & compressibility – does it move or squish with pressure?
💉 Vascularity – is there blood flow inside?
Methods BREAST scanning
🧠 What it is:
The ACR developed a standardized form for describing breast findings on ultrasound—similar to how BI-RADS is used for mammograms.
👉 BI-RADS stands for Breast Imaging Reporting and Data System.
✅ Purpose:
To make sure everyone uses the same terms when describing breast masses.
🔎 This helps ensure accurate diagnosis of breast disease and specific types of lesions.
📂 How the ACR Form Works:
It separates breast disease into two main categories:
1⃣ Mass
A mass is something that takes up space (has 3 dimensions).
It is described by its form and structure (called morphology).
These are broken down into primary and secondary features (see Table 21.3 in your text).
You also check if it moves or can be compressed (using dynamic maneuvers).
2⃣ Architectural Distortion
This refers to abnormal tissue structure without a clear mass.
It means the tissue looks distorted or pulled, not in its normal pattern.
🔬 Extra Tools to Use:
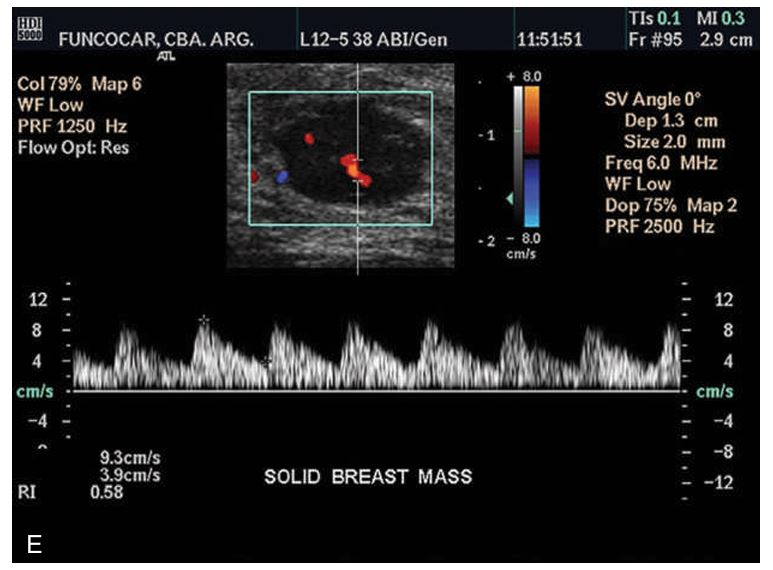
When possible, use color Doppler to see if blood flow is present or absent in the mass.
Blood flow can help show if a mass might be benign or malignant.
📋 American College of Radiology (ACR) Sonography Descriptive Form
Benign (non-cancerous) breast conditions are common, and some of the most frequent ones include:
✅ Cysts
✅ Fibrocystic Dysplasia
✅ Fibroadenoma
✅ Intraductal Papilloma
✅ Ductal Ectasia
👩⚕ What factors are considered when a lump is found?
When a dominant mass (a lump that stands out) is felt, doctors consider:
🔹 The patient’s age
🔹 The characteristics of the mass (how it feels, moves, etc.)
🔹 The patient’s medical history
📊 Age & Common Conditions:
👩 Younger Women:
More likely to have fibrocystic dysplasia or fibroadenomas
👵 Older/Postmenopausal Women:
More likely to have intraductal papillomas or ductal ectasia
🧪 Pathology of the Breast
Common Symptoms of Breast Disease:
Pain – may or may not be associated with a lump.
Palpable Mass – a noticeable lump or mass.
Nipple Discharge – can occur spontaneously or be induced.
Skin Changes – including dimpling, ulceration, and nipple retraction.
Key Points:
Benign conditions (non-cancerous) often cause pain, a mass, and/or nipple discharge.
Malignant conditions (cancerous) are more likely to cause skin dimpling, ulceration, and nipple retraction.
Benign vs. Malignant Tumors:
Benign Tumors (e.g., fibroadenomas):
Feel rubbery and mobile (can be moved easily).
Have well-defined borders.
Malignant Tumors (cancerous):
Feel hard, often like stone, and have irregular borders.
May have a gritty texture.
Soft Tumors:
Typically represent a lipoma (fatty tissue).
Cystic Masses:
Like a water balloon, well-defined but less mobile than fibroadenomas.
Form part of the breast parenchyma (tissue), whereas fibroadenomas are enclosed by a capsule.
📏 Characteristics of Benign Solid Masses:
Smooth margins or mildly lobulated (rounded).
Lobulations in benign fibroadenomas are generally:
Large, rounded, and no more than three lobulations.
Growth Pattern:
Benign lesions tend to grow along the normal tissue planes of the breast (which are horizontally oriented).
These lesions are wider than tall and grow parallel to the chest wall.
🩺 Clinical Evaluation of Breast Disease
Common in: Women aged 35 to 55, especially those peri-menopausal.
Symptoms:
HX of palpable lump(s) that change size with the menstrual cycle.
Pain, especially when the cyst is growing.
Tenderness
Causes: Cysts are dilated ducts filled with secretions. They may result from internal or external factors.
Postmenopausal Changes: Cysts may resolve after menopause, but hormone replacement therapy (HRT), blood pressure meds, steroids, or digitalis can cause cyst formation in postmenopausal women.
Small Cysts: May persist from one cycle to the next.
Appearance: Cysts are often round or oval (long axis towards the nipple), smooth, and soft. Some may become firm or tender under tension.
Treatment: Small, simple cysts in low-risk patients are usually followed with imaging for monitoring.
Breast Cysts
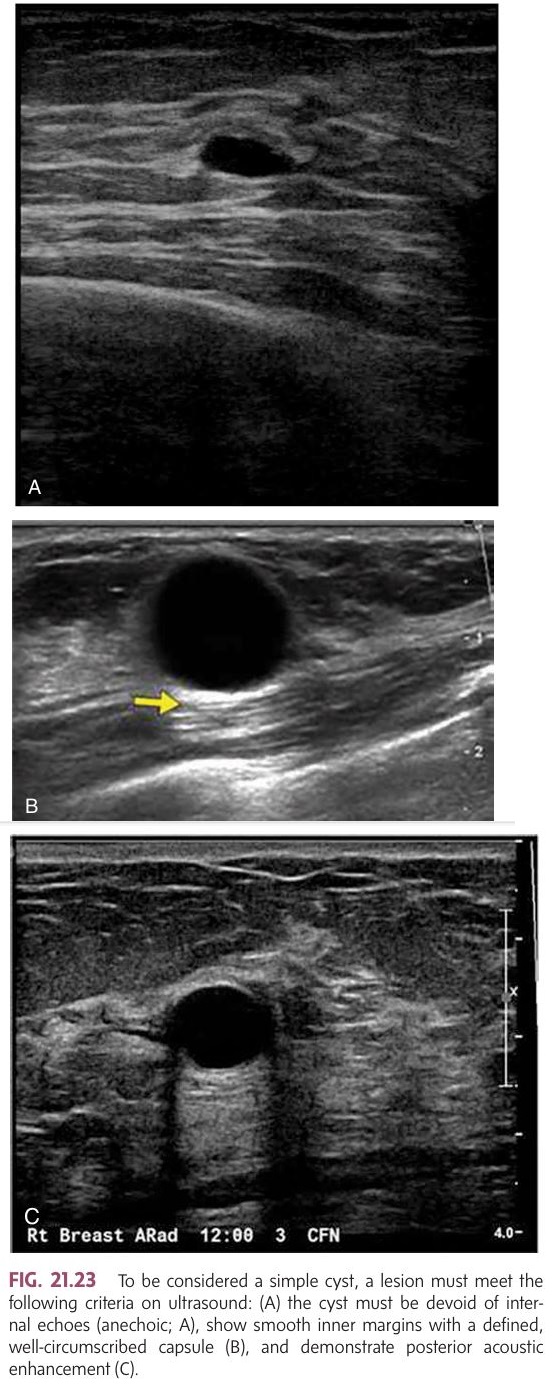
Simple Cyst pics
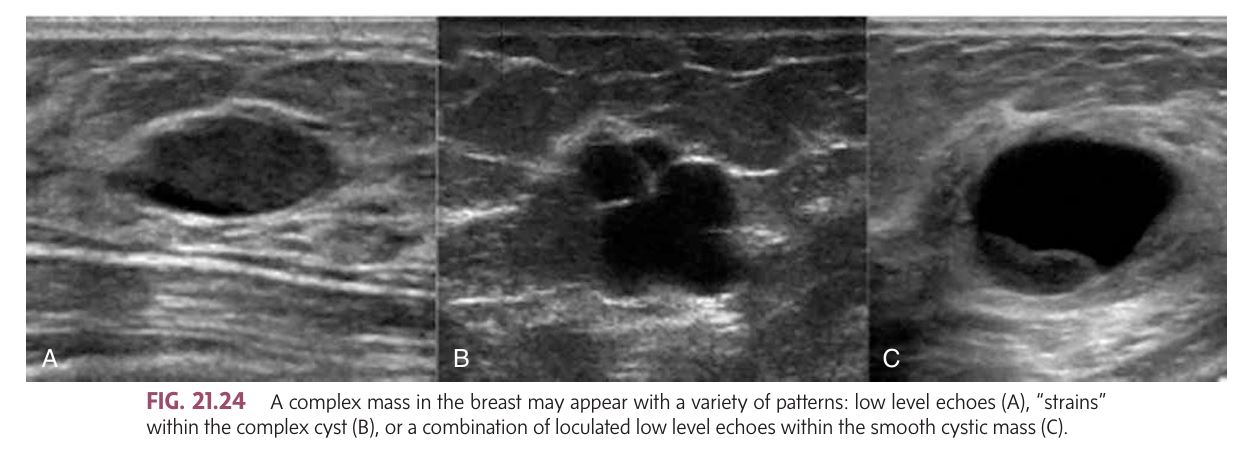
Complex cyst pics
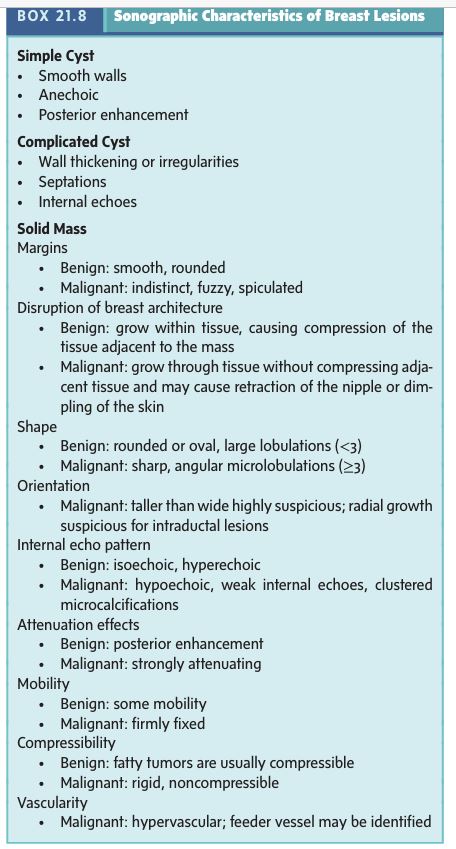
Simple Cysts:
Criteria on Ultrasound:
Anechoic (no internal echoes).
Smooth inner margins with a well-circumscribed capsule.
Posterior acoustic enhancement (shows clearer tissue behind the cyst).
Benign: No further work-up usually required.
Complex Cysts:
Features include:
Internal echoes, wall irregularities, nodularity, septations, or shadowing.
May appear solid unless layers or floating crystals are visible.
Requires aspiration or biopsy to confirm if benign.
Inflammation Signs: Fluid-debris levels, wall thickening, or blood flow seen in the wall.
Subcutaneous Cysts (e.g., epidermal or sebaceous cysts): Contain keratin or sebum, often due to blocked glands or follicles, and may result from trauma.
Types of Cysts
Most common cause of breast masses in premenopausal women.
Symptoms:
Pain (mastodynia), especially premenstrual.
Swollen, heavy breasts.
Dark brown or green nipple discharge.
Discomfort under the arms.
Both breasts are often equally affected.
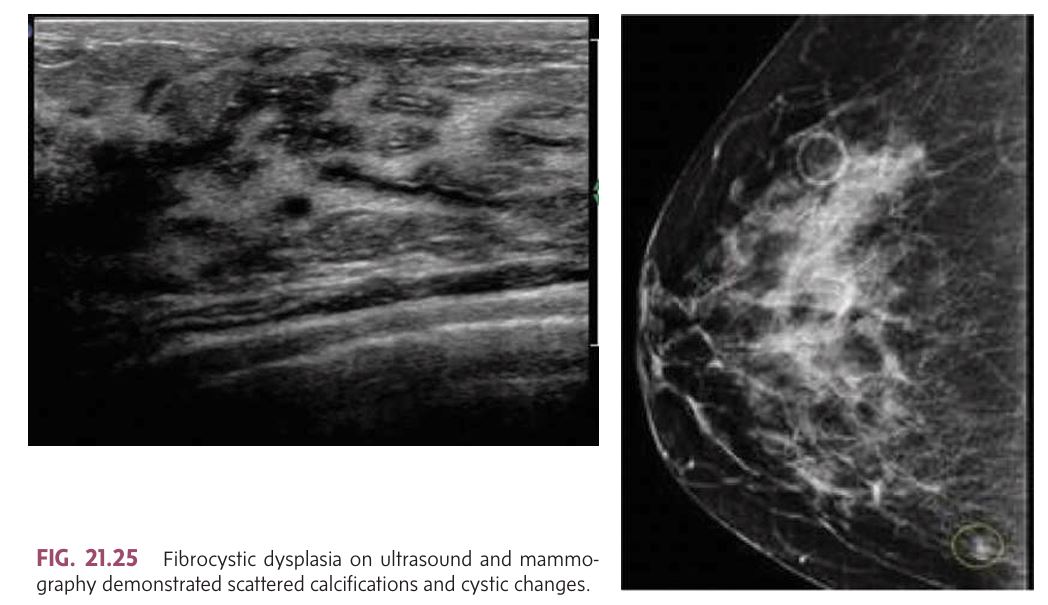
Imaging Findings:
Mammogram: Diffuse benign microcalcifications and round masses.
Ultrasound: Scattered calcifications and cystic changes (simple, complicated, or clustered cysts).
Stages of Fibrocystic Changes:
Mastodynia (Pain) – Occurs in younger women, usually before menstruation.
Adenosis – Common in women aged 25 to 40; can cause painful, lumpy breasts and nipple discharge.
Late-stage Cystic Disease – In women aged 35-55, presents with larger cysts, increased pain, and palpable lumps.
Pathology: Includes apocrine metaplasia, fibrosis, epithelial ductal hyperplasia, and sclerosing adenosis. It's important that biopsy findings correlate with imaging and clinical symptoms.
Fibrocystic Dysplasia/Fibrocystic Changes
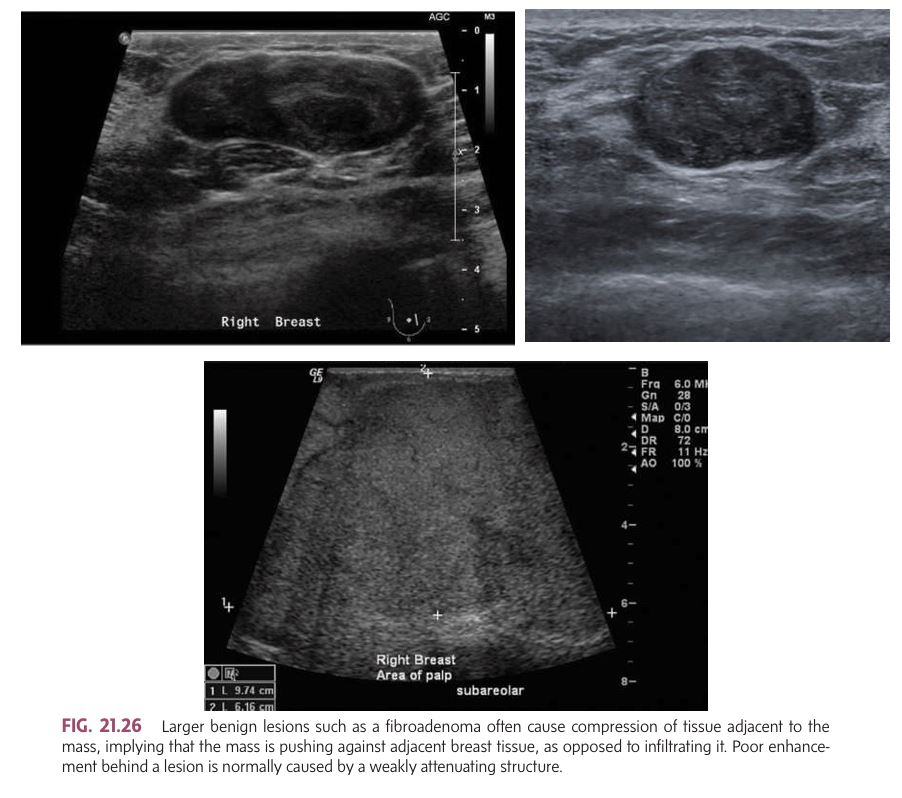
Most common benign breast tumor in women aged 15-40.
Characteristics:
Firm, rubbery, mobile, clearly separate from surrounding tissue.
Round/oval, smooth or lobulated.
Doesn't usually cause pain (mastodynia) and doesn't change size with the menstrual cycle.
Grows slowly but may rapidly increase in size with hemorrhage (bleeding inside the tumor).
If tumor grows more than 20% in 6 months, further investigation is needed (may suggest phyllodes tumor).
Sonographic Features:
Smooth, rounded margins and low-level homogeneous internal echoes.
Intermediate posterior enhancement (clearer behind the mass).
May appear hypoechoic (darker) compared to breast fat but can sometimes be hyperechoic (brighter).
Larger fibroadenomas may compress surrounding tissue.
Fibroadenoma (Benign Tumor)
Seen in adolescent girls (ages 10-20).
These tumors can grow very large and may have dilated veins.
Treatment usually involves needle biopsy followed by surgical excision.
Giant (Juvenile) Fibroadenoma
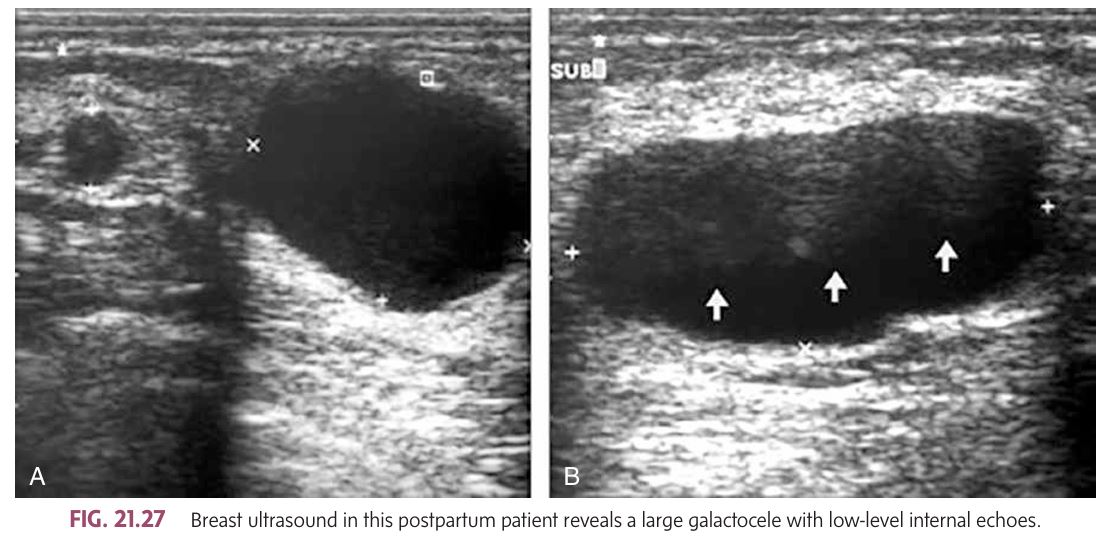
Most common mass during pregnancy/lactation: Fibroadenomas.
Reason for growth: Increased hormone levels during pregnancy and lactation can cause fibroadenomas to enlarge rapidly.
Note: The hormonal surge can also affect breast cancers, which might be diagnosed later than in non-pregnant women.
Other Breast Issues During Pregnancy/Lactation:
Mastitis
Abscesses
Cysts
Galactoceles (milk-filled cysts).
Galactocele Appearance: May appear as a complex cyst on mammography or ultrasound, or sometimes show a fat-fluid level.
Treatment: Cysts (including galactoceles) can be aspirated under ultrasound guidance.
Pregnant and/or Lactating Patient: Benign Breast Masses
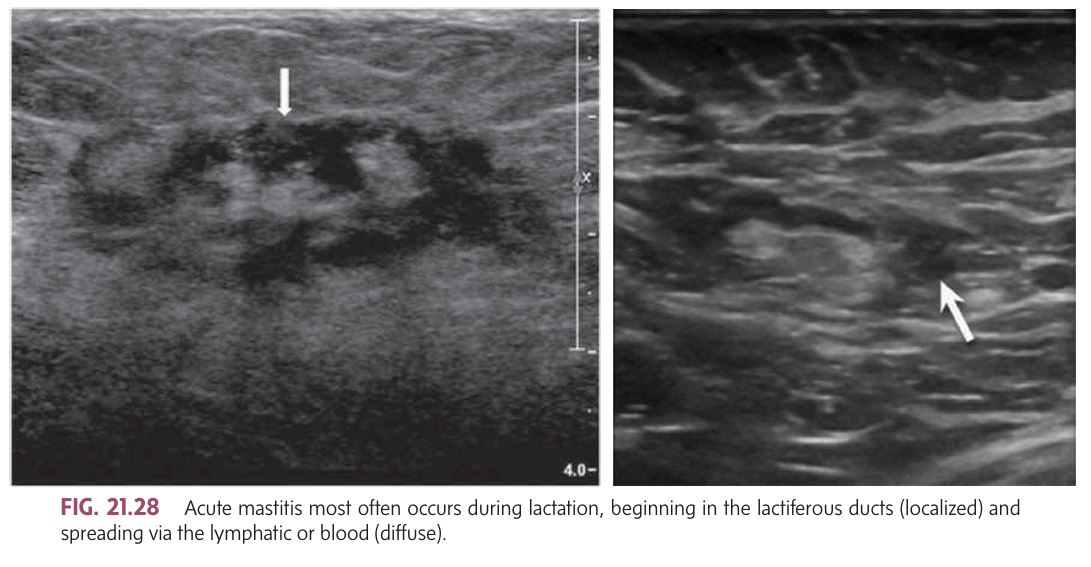
Mastitis:
Types:
Puerperal Mastitis (Most common acute type during lactation).
Periductal Mastitis (Noninfectious, seen in perimenopausal and menopausal women).
Granulomatous Mastitis (Caused by trauma, foreign bodies, infections, or autoimmune disorders).
Acute Mastitis:
Causes: Infection, trauma, or mechanical obstruction in milk ducts.
Symptoms: Enlarged, reddened, tender breast, often in a localized area.
Common in lactating women:
If the galactocele (milk cyst) becomes infected, it can lead to mastitis and potentially form an abscess.
If a galactocele persists, it may turn into a lipid or oil cyst.
Treatment:
Initially antibiotics.
After inflammation decreases, breast imaging (mammogram or ultrasound) can rule out inflammatory breast cancer.
Chronic Mastitis:
Cause: Chronic inflammation of the glandular tissue, often due to intraductal secretions forced into periductal connective tissue.
Symptoms: Nipple discharge, possible nipple retraction, and subareolar thickening (no dominant mass).
Ultrasound appearance: Mixed, diffuse echo pattern with sound absorption.
Mastitis
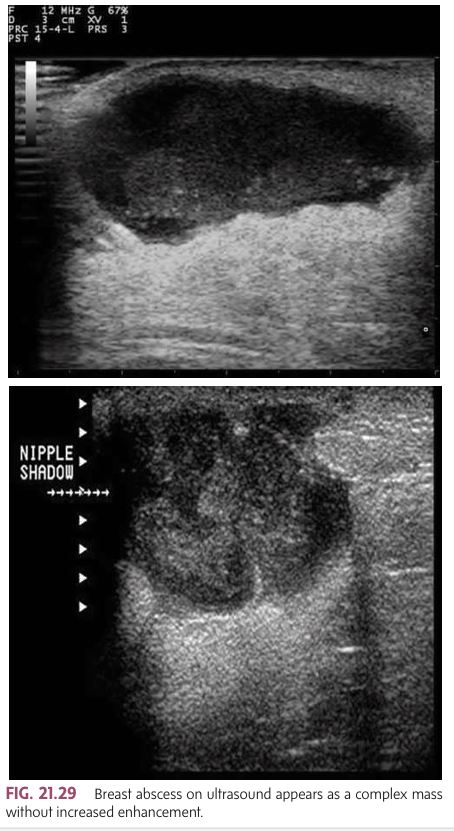
Because obstructed ducts are prone to infection, acute mastitis can develop into a ______
Cause: Bacteria entering through cracked nipples or skin wounds, leading to infection.
most often found in the subareolar area.
Symptoms:
Pain, swelling, redness, and possibly fever.
Swollen, painful axillary nodes.
Sonographic Features:
Acute abscesses: Poorly defined borders.
Mature abscesses: Well encapsulated with sharp borders.
Ultrasound: Diffuse, mottled breast appearance, irregular margins, posterior enhancement, and low-level internal echoes.
If associated with mastitis, skin thickening is almost always present, and edema leads to diffusely increased echogenicity of the breast tissue.
Doppler imaging: Can show increased vascularity (hyperemia), which helps distinguish an abscess from other lesions like hematomas.
Breast Abscess
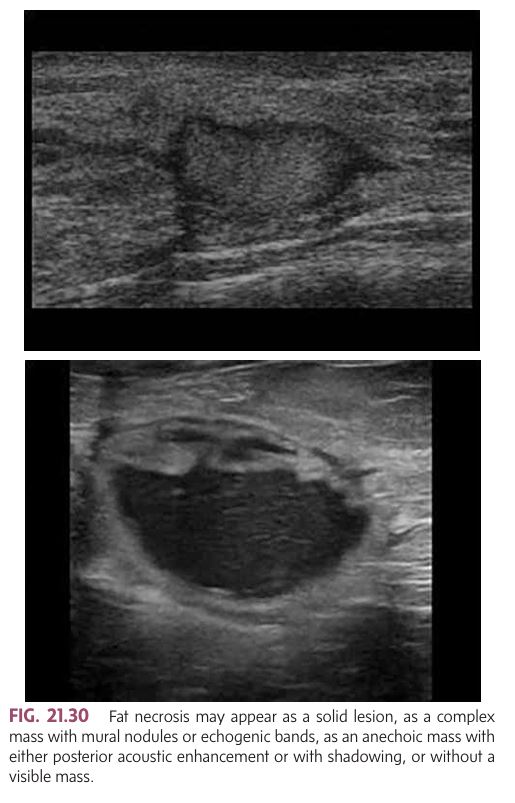
Injury to breast fat may cause a common benign inflammatory process.
Cause: Trauma, surgery, radiation, or inflammatory conditions (e.g., plasma cell mastitis, cancer).
More common in older women.
Clinical Appearance: Spherical, superficial nodule that may have calcified necrosis.
Deep Fat Necrosis: May cause skin retraction and mimic breast carcinoma.
Benign Characteristics:
Limited mobility or may "roll away" when palpated.
Compression with ultrasound transducer may change its shape (suggesting benign nature).
Sonographic Appearance of Fat Necrosis:
Varied appearance:
Solid lesion.
Complex mass with mural nodules or echogenic bands.
Anechoic mass (may show posterior acoustic enhancement or shadowing).
May not show a visible mass.
Despite its variable appearance, fat necrosis is distinct from the rest of the breast tissue and usually benign.
Fat Necrosis
Cause: Occurs due to trauma or may develop spontaneously in patients on anticoagulants (like coumadin or heparin) or those with bleeding disorders (e.g., leukemia, thrombocytopenia, hemophilia).
Trauma sources: Seat belt or airbag injuries in automobile accidents, invasive procedures (biopsy, cyst aspiration, surgery).
Breast Hematoma

Seroma: (most common) Collection of serous fluid (watery portion of blood).
Lymphocele: Collection of lymph fluid.
Common after surgery or trauma.
Sonographic Appearance: Difficult to differentiate between seroma and lymphocele on ultrasound
Seroma/Lymphocele

Definition: A benign tumor consisting entirely of fatty tissue. Sometimes, a fibroadenolipoma has additional fibrous and glandular elements.
Occurrence: More common in middle-aged or menopausal women.
Clinical Features:
on palpation, a large, soft, poorly demarcated mass
No skin thinning or fixation.
Sonographic Findings:
Smooth walls.
Hypoechoic to surrounding tissues.
May show posterior enhancement.
Compressible and soft to touch.
Difficult to distinguish in a fatty breast (may look similar to normal fat tissue on ultrasound).
Lipoma
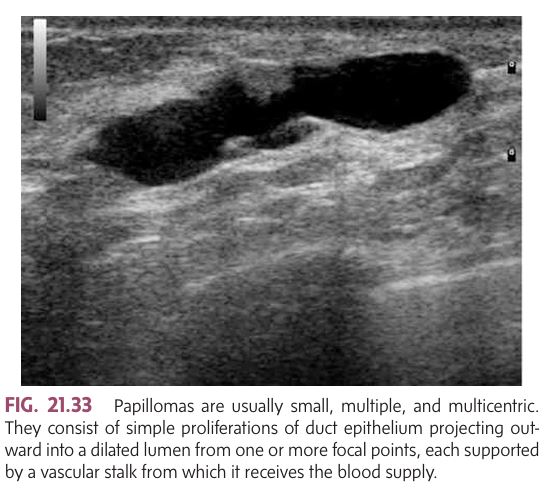
Definition: A small, benign tumor that grows within the acini (milk ducts) of the breast.
Common Age Range: 35 to 55 years.
Symptom: Spontaneous nipple discharge from a single duct. When discharge is abundant, it is often preceded by a feeling of fullness or pain in the areola/nipple area, which is relieved once the fluid is expelled.
Sonographic Findings:
small, Multiple and multicentric papillomas.
Raspberry-like appearance on mammogram, aiding in correlation between mammogram and ultrasound.
Tumors are often supported by a vascular stalk.
Can cause the duct to fill with blood or serum if trauma ruptures the stalk.
Can be palpable if large.
Papillomas often appear linear, resembling a terminal duct.
Intraductal Papilloma
Cause: Associated with disorders of collagen metabolism, especially in premenopausal Type 1 diabetic women.
Risk: These women are prone to developing benign fibrosis in the breast.
Sonographic Findings:
Highly echogenic mass that is well-circumscribed but lacks a capsule.
Most commonly located in the upper outer quadrant of the breast.
Can resemble breast cancer on imaging techniques, causing difficulty in distinguishing it from malignancy.
Prognosis:
Generally benign and does not lead to malignancy.
The condition is not cancerous but requires differentiation from other breast masses.
Diabetic Mastopathy
Overview:
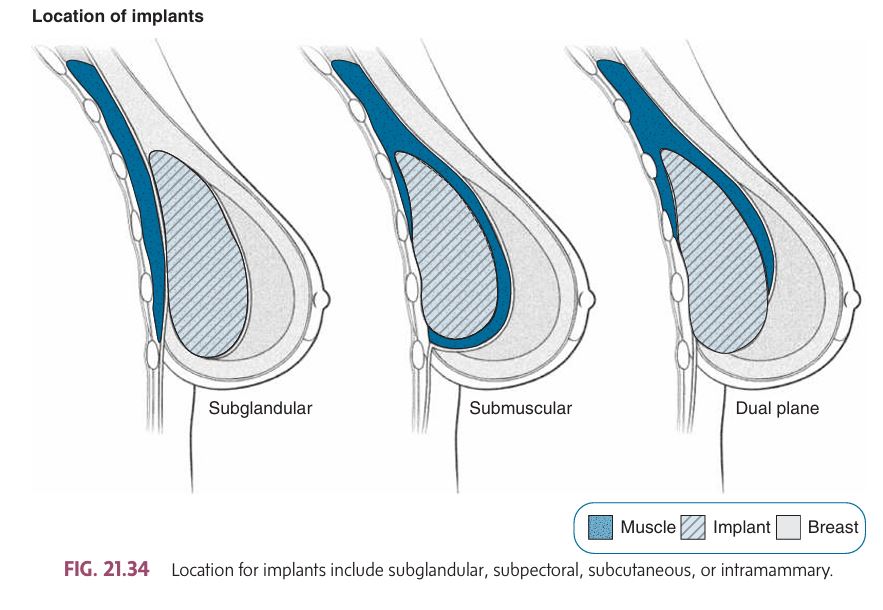
Breast implants can be used for cosmetic purposes or for reconstruction after mastectomy, to correct congenital amastia or hypoplasia, or to address breast asymmetry or defects.
Silicone gel-filled and saline implants are the most common types. Implants can be placed in various locations: subglandular, subpectoral, subcutaneous, or intramammary.
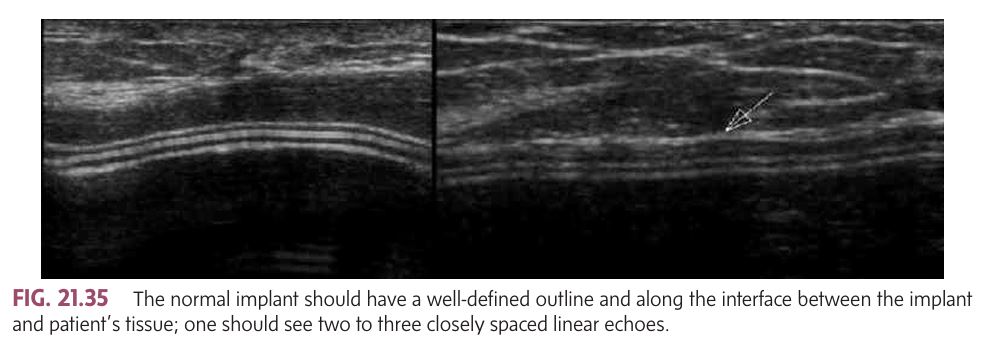
Normal Sonographic Findings:
Well-defined outline of the implant.
Two or three closely spaced linear echoes (representing the anterior and posterior surfaces of the shell and the fibrous capsule).
Saline implants and tissue expanders: May show a port or valve along the anterior surface, usually located beneath the subareolar area.
A peripheral or radial fold extending from the implant wall is common.
Breast Augmentation and Implant Complications:
Acute Complications (early, soon after implantation):
Pain/tenderness.
Loss of nipple sensation.
Hematoma.
Abscess.
Seroma.
Chronic Complications (may develop years later):
Capsular fibrosis/contracture: The fibrous capsule around the implant hardens and tightens, which can distort the shape of the breast.
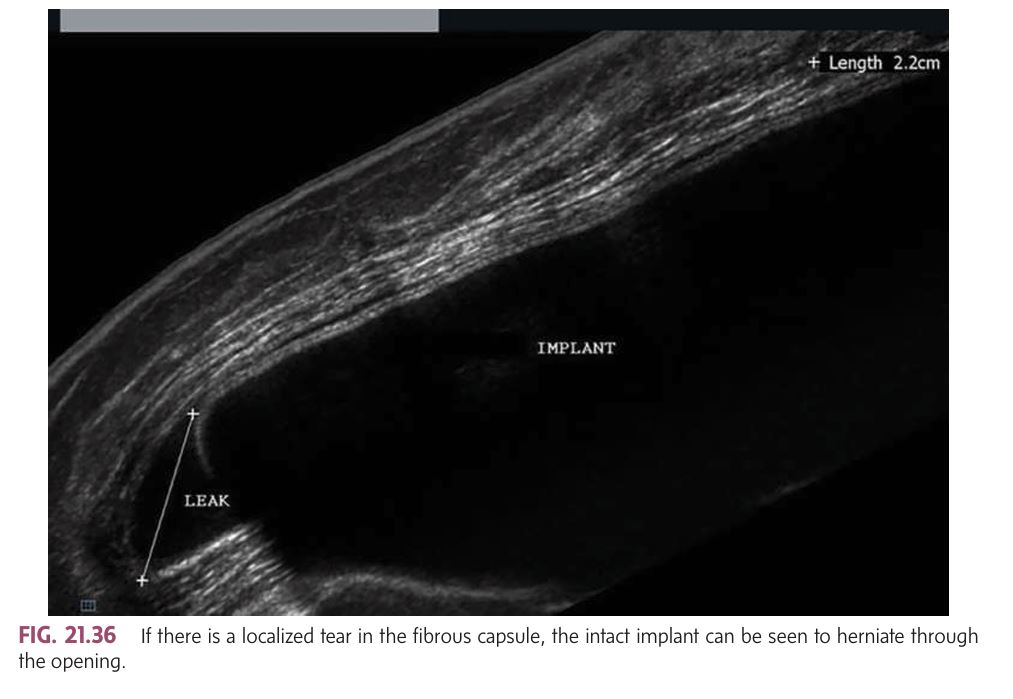
Herniation: A tear in the fibrous capsule may cause the implant to protrude or move (palpable and identifiable via sonography or MRI).
Migration: The implant moves from its original position.
Rupture (Intracapsular or Extracapsular): The most common complication, especially with silicone implants.
Silicone granuloma: When silicone leaks into the surrounding tissue, forming a localized inflammatory response.
Chronic infection: This can result in prolonged inflammation or damage.
Complications of Breast Implants
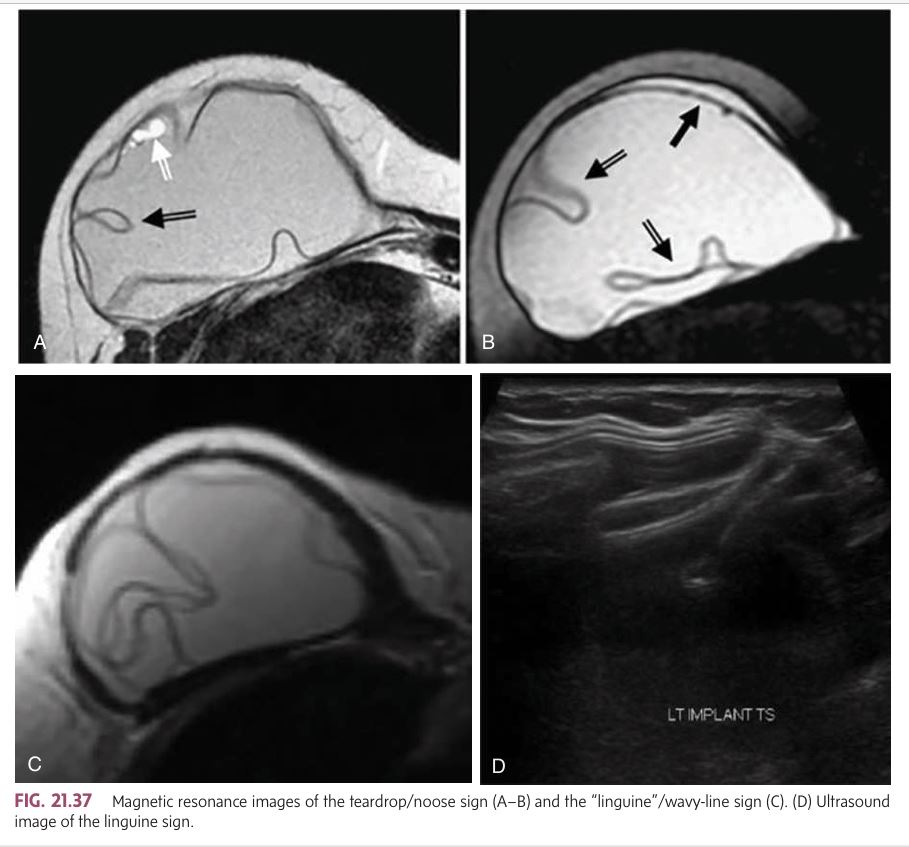
intracapsular silicone rupture include the _____ on MRI
“linguine”/wavy-line sign and the teardrop/ noose sign
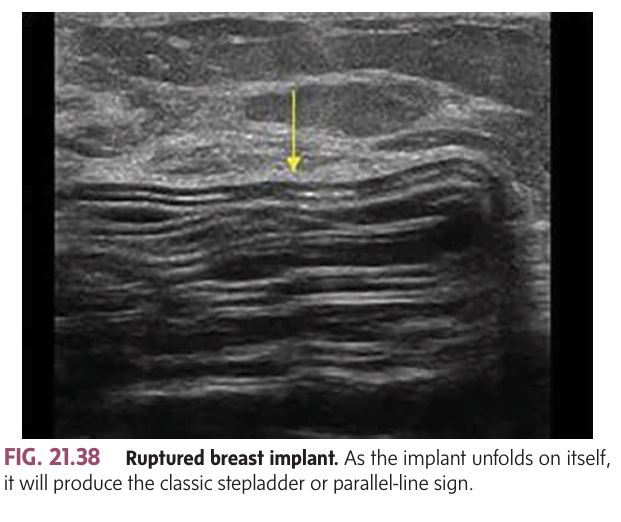
Intracapsular Rupture : As the implant folds on itself, it will produce the
classic stepladder or parallel-line sign
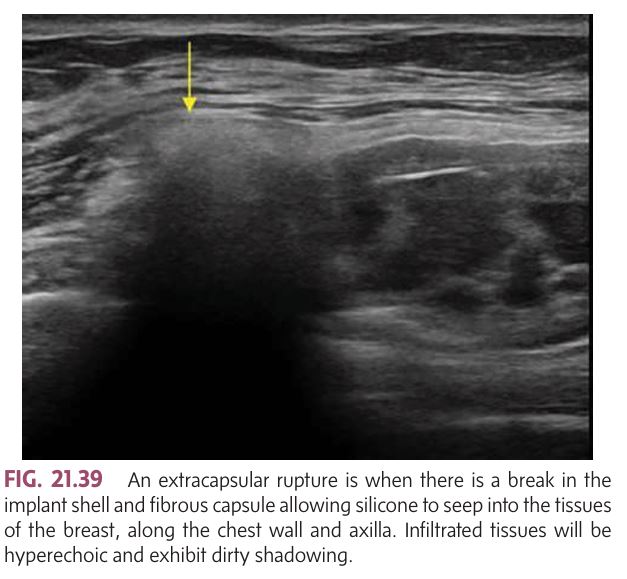
Extracapsular Rupture: The most classic sonographic appearance is the ________ or echogenic noise. Infiltrated tissues will be hyperechoic and exhibit dirty shadowing
“snowstorm” sign
Capsular Contracture:
What Happens: A fibrous capsule forms around the implant (normal post-implantation), but in some cases, it becomes thickened and tightens, leading to a distortion of the implant shape.
Sonographic Findings: The fibrous capsule measures >1.5 mm, and capsular calcifications may develop over time. Herniation may occur due to a tear in the capsule, allowing the implant to protrude.
Best Imaging Modality: MRI is considered the most effective for assessing the integrity of the implant, especially identifying double-lumen implant failures.
Implant Rupture:
Types:
Intracapsular rupture: The silicone gel leaks out of the implant but remains contained within the fibrous capsule.
Extracapsular rupture: The silicone escapes the fibrous capsule and spreads into surrounding tissues.
Common Risk Factors: Implant age (especially silicone implants between 11-15 years old) and trauma.
Effects:
Intracapsular rupture: May result in granuloma formation and inflammatory reactions, leading to autoimmune responses.
Saline implant rupture: Results in deflation, causing visible breast asymmetry, but is absorbed by the body without long-term harm.
Sonographic Findings for Implant Rupture: Intracapsular Rupture:
Classic Sonographic Signs:
Stepladder sign: Appears as a series of parallel lines inside the implant, indicating collapse or folding of the implant.
Echogenic silicone gel: May appear more echogenic due to mixing with bodily fluids, proteins, and salts. This appearance is not always reliable because substances used at implantation (like saline or antibiotics) may cause this effect as well.
Extracapsular Rupture:
Classic Sonographic Appearance:
Snowstorm sign (also known as echogenic noise): Silicone leaks into surrounding tissues, causing them to appear hyperechoic (brighter) and show dirty shadowing.
Silicone may migrate along the chest wall and into the axilla.
MRI for Rupture Detection:
Intracapsular Rupture: MRI can reveal the "linguine" sign (collapsed elastomer shell suspended in silicone) and teardrop sign (gel trapped in the fold of the implant).
Extracapsular Rupture: MRI can also detect the presence of silicone in adjacent lymph nodes, and granulomas will appear hypointense on T1 and hyperintense on T2 weighted images, especially with silicone suppression.
Key Complications:
1. Margins:
Irregular or ill-defined margins are common for malignant masses.
Fremitus technique: Have the patient hum while using power Doppler to identify mass boundaries 👂💨. This helps with:
Confirming the presence of a mass.
Differentiating between masses and locating them.
Identifying multifocal or isoechoic masses 🔍
2. Spiculation (Finger-like extensions) 🌿🦋:
Malignant masses often show spiculated margins which look like small lines radiating from the mass.
This is highly suspicious for cancer 🧐.
3. Shape 📐:
Angular margins and microlobulations (1-2 mm lobes) are associated with malignancy.
Microlobulations tend to be sharper and more numerous than those in fibroadenomas 🔺🔍.
4. Orientation 🔄:
Vertical orientation: If the mass is taller than wide, it's highly suspicious for malignancy. This is known as "taller than wide" 📏🔝.
5. Internal Echo Pattern 🎶:
A hypoechoic solid mass (darker on the ultrasound) is more suspicious for malignancy.
It can show weak internal echoes and cause dense posterior shadowing 🚫👀.
6. Attenuation Effects 💨:
Posterior shadowing suggests malignancy, while edge shadowing can be seen in benign masses. Look for dense attenuation 🎯.
7. Microcalcifications 💎:
These are suspicious for malignancy, although they are better detected via mammography 📸 than ultrasound.
8. Mobility 🚫:
Malignant masses are usually rigid and fixed in position 🛑.
9. Compressibility 🏋♀️:
Malignant lesions are noncompressible (i.e., hard to squish) 💪.
10. Vascularity 🩸:
Increased vascularity (seen with Doppler ultrasound) is a red flag. Tumors may have feeder vessels that are highly suspicious for malignancy 🚨.
Sonographic Characteristics of Malignant Breast Masses 🩺💡
Malignant tumors are aggressive and tend to grow through tissue via finger-like extensions termed _______
they are highly suspicious for malignancy
appear as small lines that radiate outward from the surface of a mass
typically alternating hypoechoic and hyperechoic lines.
Spiculation

________ are associated with malignancy as are microlobulations (very small 1- to 2-mm lobulations)
Sharp angular margins

If a mass measures longer in the anteroposterior dimension (height) than in the transverse or sagittal plane (width), it has a vertical orientation, is usually described as ________ and is highly suspicious for malignancy
“taller than wide”
A solid lesion that is markedly ________ relative to the normal breast parenchyma is more suspicious for malignancy
hypoechoic
Shadowing behind a solid breast mass is another suspicious sonographic sign for malignancy because malignant tumors tend to be _________
highly attenuating
malignant masses often demonstrate ________ vascularity within the lesion and often have a feeder vessel
increased
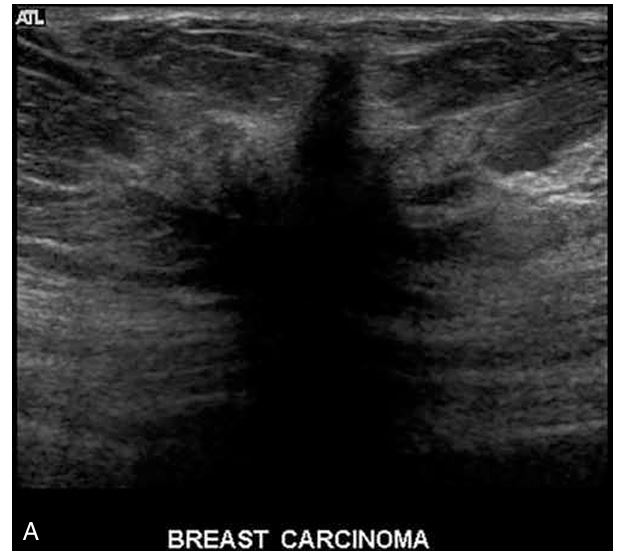
The most common type of breast cancer, accounting for nearly 85% of breast cancers.
IDC begins in the milk ducts but invades the surrounding fatty tissue of the breast and can metastasize via the bloodstream or lymphatic system.
There are different grades of IDC, ranging from low-grade (non-comedo) to high-grade (comedo).
Atypical ductal hyperplasia is considered a precursor.
Signs & Symptoms:
A palpable mass may be felt.
Nipple retraction or skin changes may occur.
Bloody or clear nipple discharge.
Pain or discomfort in the breast area.
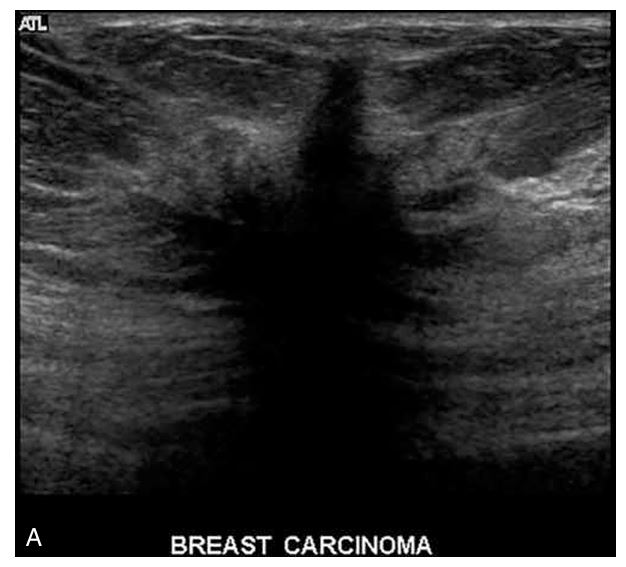
Sonographic Features:
Often presents as an irregular mass with poorly defined borders.
Ducts are enlarged and may be filled with a "cottage cheese-like" material containing calcifications (comedocarcinoma).
May show posterior shadowing due to fibrosis.
A heterogenous internal echo pattern may be seen.
Prognosis:
Prognosis is generally worse than for non-invasive forms due to the potential for metastasis.
Non-comedo types have a better prognosis compared to comedo types.
Invasive Ductal Carcinoma (IDC) 🚨
Description:
A type of intraductal carcinoma filled with yellow, paste-like necrotic material (comedones).
Forms:
Invasive and noninvasive types exist
Signs & Symptoms:
May have no clinical findings
Clear nipple discharge more common than bloody
May cause pain or a crawling sensation
With early invasion: minimal thickening may be felt
With progression: nipple retraction, dominant mass, fixation
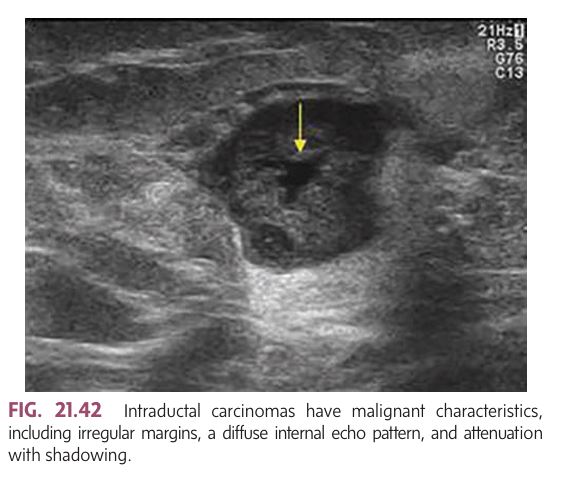
Mammographic/Sonographic Findings:
Microcalcifications commonly seen
Malignant features:
Irregular margins
Diffuse internal echoes
Shadowing/attenuation
Other Notes:
Other DCIS types include intracystic papillary carcinoma and Paget disease
Comedocarcinoma 🧨
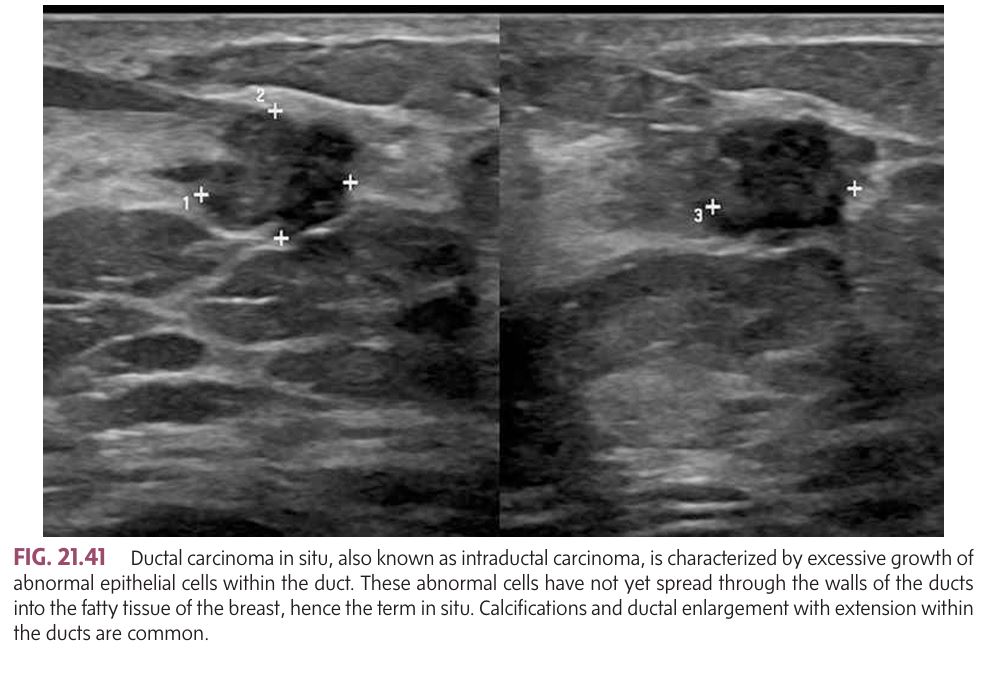
Also known as intraductal carcinoma and is the most common noninvasive breast malignancy.
Description: Non-invasive; cancer cells are confined to the ducts and haven't spread to surrounding tissue.
Signs & Symptoms:
Asymptomatic in many cases.
Nipple discharge (may be bloody).
Some cases may cause a palpable mass.
Imaging Findings:
Microcalcifications (small white specks on mammography).
Ductal enlargement on imaging.
Grading: Can be classified as low, intermediate, or high nuclear grade; higher grades are more aggressive.
Ductal Carcinoma In Situ (DCIS) 🏫
Not a true cancer — considered a precancerous growth starting in the lobule with low malignant potential.
Features:
Confined to lobules
Does not invade through the lobular wall
No distinct mass, making it difficult to detect on mammography or sonography
Indicates increased risk of future invasive breast cancer
Lobular Carcinoma in Situ (LCIS) 🧬
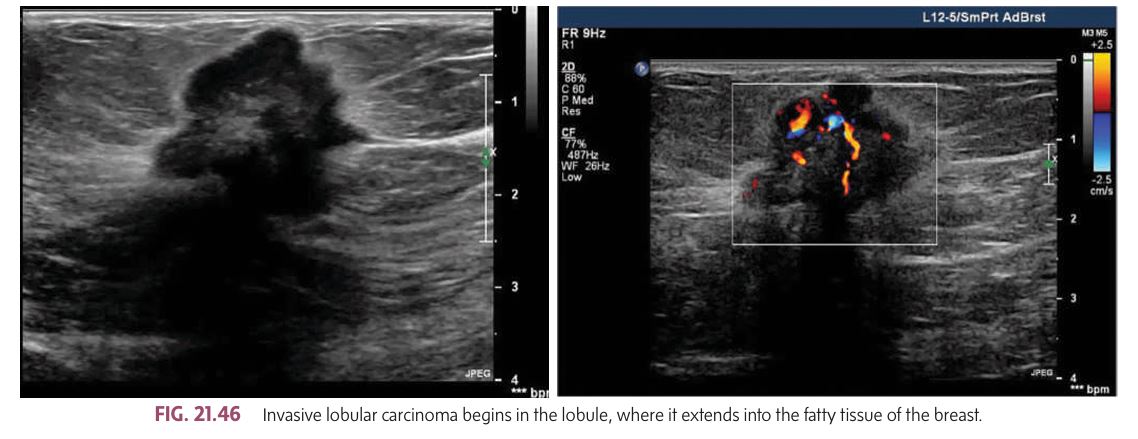
Second most common type of invasive tumor, accounting for 10% to 15% of all breast cancers.
begins in the lobule of the breast and extends into the fatty tissue.
Similar to invasive ductal carcinoma (IDC), ____ has the potential to metastasize and spread to other parts of the body.
Signs & Symptoms:
often be bilateral (affecting both breasts), multicentric (in multiple areas within the same breast), or multifocal (in multiple distinct locations).
Compared to IDC, this tends to have a more diffuse and less well-defined presentation.
Prognosis:
poorer prognosis compared to invasive ductal carcinoma.
However, when the cancer remains localized to the breast, treated patients can have a 75% survival rate after 10 years.
represent 10% to 12% of all breast cancers.
Associated Tumors:
More favorable forms of include medullary, intracystic papillary, papillary, colloid, and tubular carcinomas.
Invasive Lobular Carcinoma (ILC) 🔀
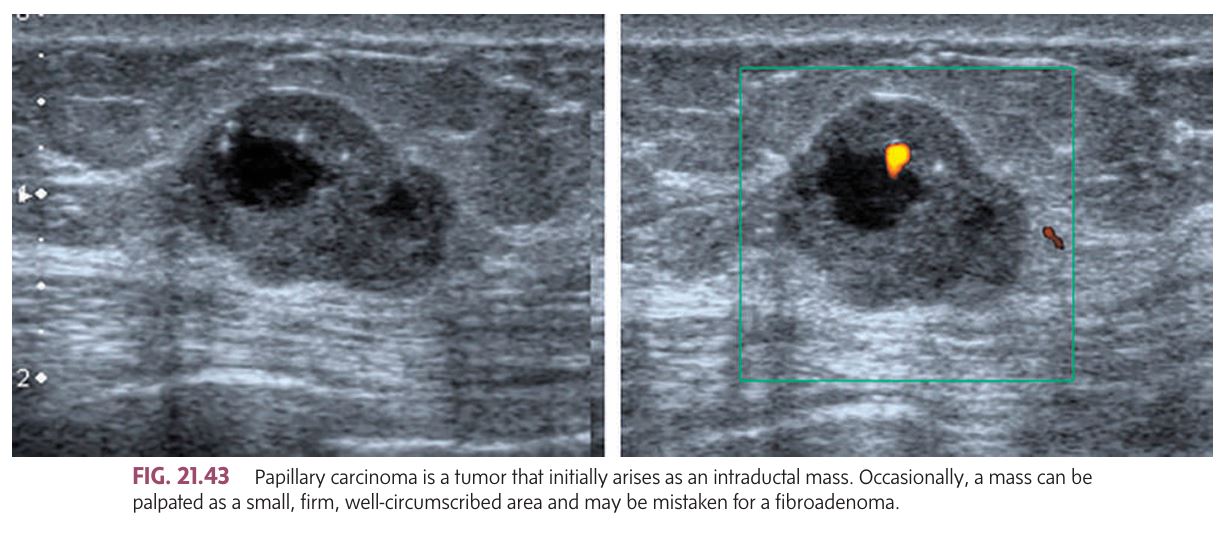
A tumor that initially arises as an intraductal mass; may also present as an intracystic tumor (rare). Early stage is noninvasive and may develop from a benign ductal papilloma. Associated with little fibrotic reaction.
Signs & Symptoms:
Earliest sign: bloody nipple discharge
Sometimes a small, firm, well-circumscribed mass (may mimic fibroadenoma)
May show blue or red discoloration under the skin with central ulceration
A diffusely nodular skin appearance may indicate multiple intraductal papillary carcinomas
In advanced intracystic form, mass may become poorly circumscribed
Mammographic Findings:
Microcalcifications
Clustered nodules in a single quadrant
Other Notes:
Malignant lesions extend >1.5 cm into a duct and its branches
Prognosis is more favorable than other types
Papillary Carcinoma 🌸
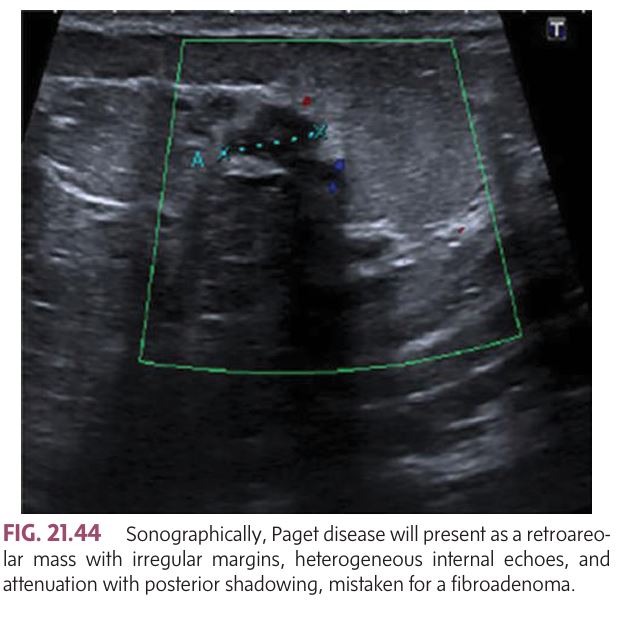
This is a relatively rare tumor and it typically occurs in women over 50 years of age.
Description:A rare tumor that arises in the retroareolar ducts and grows towards the nipple, spreading into the intraepidermal region of the nipple and areola.
Characterized by a rash-like appearance, which may be confused with melanoma.
Signs & Symptoms:
Ulceration, enlargement, or deformity of the nipple and areola.
Rash-like appearance, often mistaken for a benign inflammatory eczematous condition.
Palpatory findings may not always be present.
Sonographic Features:
Retroareolar mass with irregular margins.
Heterogeneous internal echoes.
Attenuation with posterior shadowing.
Paget Disease 💥
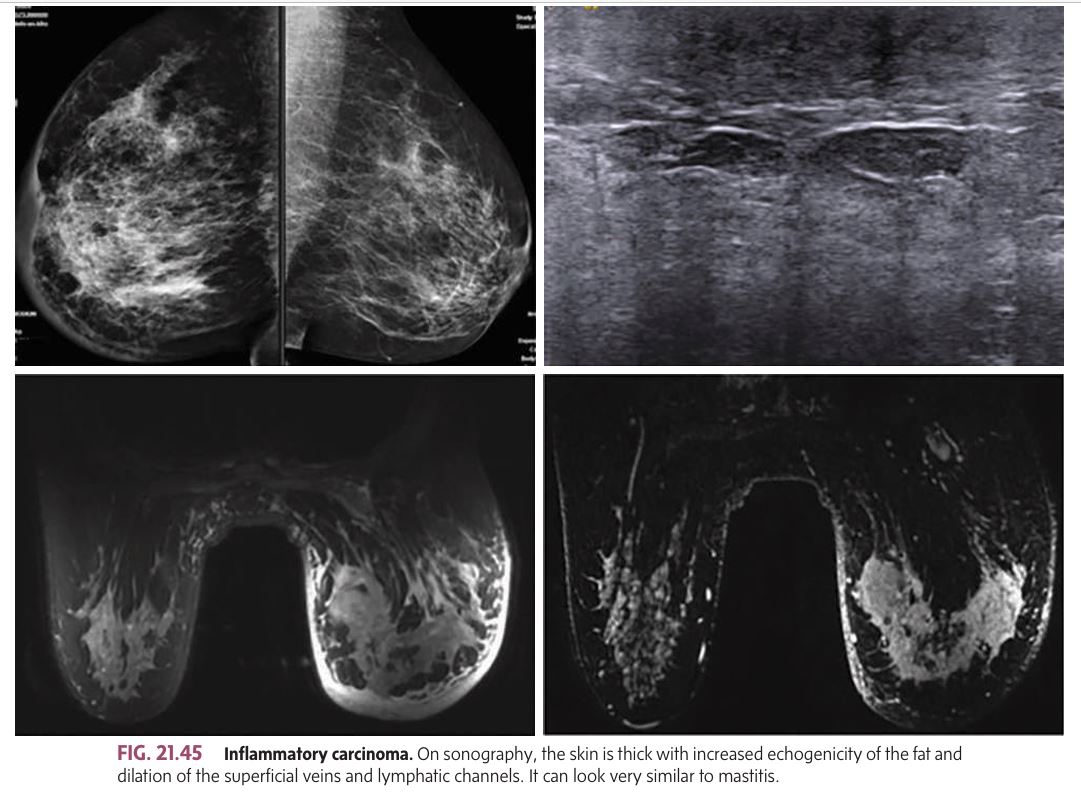
A rare, highly malignant cancer that blocks lymphatic channels in the skin, causing rapid metastasis and poor prognosis.
Signs & Symptoms:
Red, swollen breast
Peau d’orange (orange peel texture) in 1/3 of cases
Skin is warm/feverish, breast is hard
Enlarged axillary lymph nodes
Sonographic Features:
Thickened skin with increased echogenicity of the fat.
Dilation of superficial veins and lymphatic channels.
May resemble mastitis, making it difficult to distinguish without biopsy.
Prognosis:
Poor, due to rapid and diffuse metastasis.
Inflammatory Carcinoma 🩸
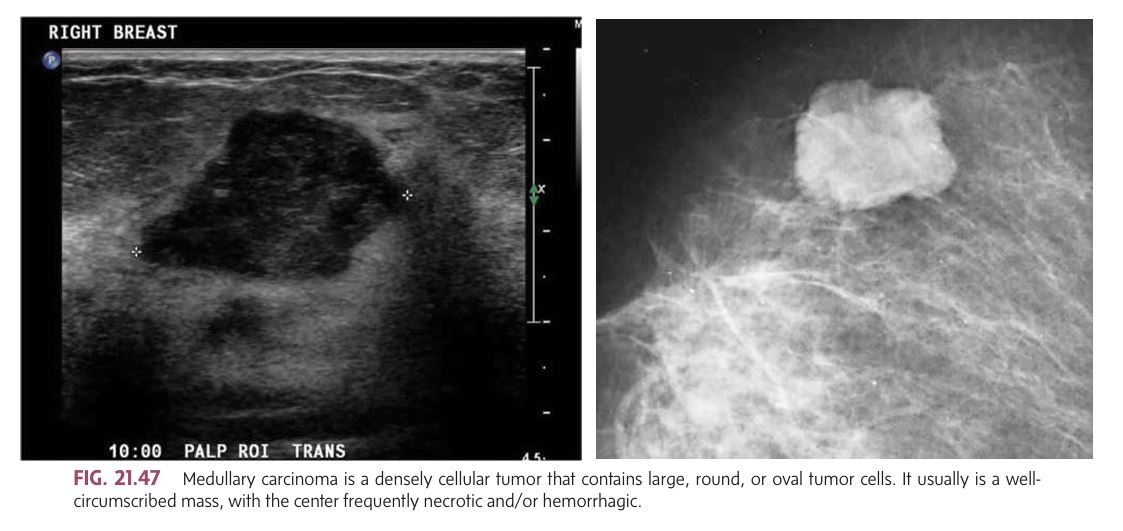
A rare and densely cellular tumor with large, round, or oval tumor cells. It is typically well-circumscribed and often features a necrotic or hemorrhagic center.
majority of cases occurring in women younger than 50 years.
are relatively rare, accounting for less than 5% of breast cancers.
Signs & Symptoms:
Well-circumscribed, mobile, non-tender mass.
Often large and smoothly lobulated.
Mild compressibility.
Discoloration of the overlying skin.
Bilateral occurrence is more frequent than other breast cancers.
Sonographic Features:
Well-defined mass with smooth margins.
Possible central necrosis or hemorrhage.
May resemble a fibroadenoma but grows rapidly.
Prognosis:
Good prognosis due to low incidence of lymph node involvement.
Medullary Carcinoma 🧠
An uncommon, well-differentiated subtype of invasive ductal carcinoma, typically less than 2 cm in size.
Demographics:
Most commonly seen in women around 50 years old
Prognosis:
Favorable outcome
Low recurrence and low metastasis rate
Death is rare
Signs & Characteristics:
Poorly circumscribed margins
Hard consistency
Tubular Carcinoma 🛠
A pathological subtype of invasive ductal carcinoma with dense fibrosis and possible focal calcifications.
Signs & Symptoms:
Very firm, nonmovable nodular mass
Often shows fixation, skin flattening, and nipple retraction
Retraction caused by shortening of Cooper’s ligaments
May involve entire breast or become fixed to thoracic wall
Bloody discharge is rare
Note:
Often lacks specific histologic pattern, so may be classified as ductal carcinoma not otherwise specified
Scirrhous Carcinoma 🏰
A rare type of ductal carcinoma primarily affecting women over 75 years old. The tumor cells produce a gelatinous (mucinous) material that fills lactiferous ducts or stromal tissue, giving the mass a soft consistency.
Signs & Characteristics:
Soft-feeling mass upon palpation
More common in elderly patients
Sonographic Features:
Smooth margins
Posterior enhancement
“Salt and pepper” echotexture
Colloid (Mucinous) Carcinoma 🍬
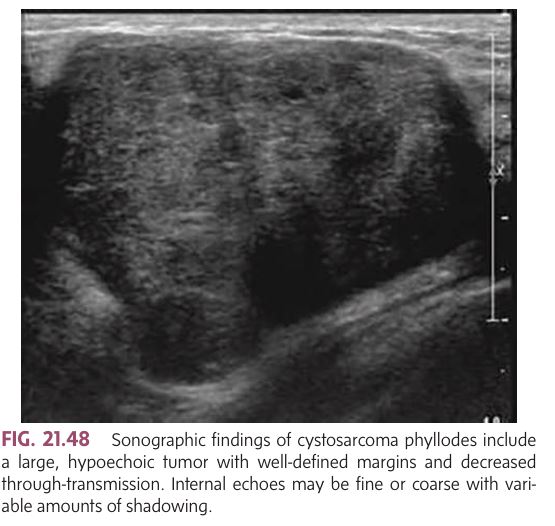
A rare breast tumor with malignant potential, accounting for less than 1% of all breast neoplasms. Considered the malignant counterpart to fibroadenoma, it is the most frequent breast sarcoma. Typically found in women aged 45–50 and usually unilateral.
Signs & Characteristics:
May begin as a longstanding small mass that suddenly grows rapidly
Initially firm, mobile, and well-delineated (resembles fibroadenoma)
As it enlarges:
May become lobulated or irregular
Skin changes due to pressure
Ulceration, infection, or abscess may develop
Does not adhere to surrounding tissues or muscle (no skin dimpling or fixation)
Sonographic Features:
Large, hypoechoic mass
Well-defined margins
Decreased through-transmission
Internal echoes may be fine or coarse, with variable shadowing.
Cystosarcoma Phyllodes 🌸
________ the breast is rarely primary, typically being lymphomatous invasion from non-Hodgkin lymphoma.
Signs & Characteristics:
Enlarged nodes within the breast and axillary region
Hypoechoic, round or oval masses
Homogeneous texture
Posterior enhancement
Sonographic Features:
Diffuse infiltration may present similarly to inflammatory carcinoma
Biopsy is required to differentiate lymphoma from inflammatory carcinoma, leukemic infiltration, or other nodular masses of the breast
Lymphoma 🦠
Primary breast cancer is most likely to spread first to the lymph nodes and then to bone, lung, brain, and liver.
Bone metastases are the most common distant site for breast cancer metastasis.
Metastatic lesions in the breast are rare, but they often arise from the contralateral breast or other extramammary primaries.
Common Extramammary Primaries:
Melanoma (most common)
Lung cancer
Ovarian cancer
Sarcoma
Gastrointestinal tract cancers
Common Hematologic Primaries:
Lymphoma
Leukemia
Metastatic Disease 🌍
🧪 1. Preoperative Needle Wire Localization 🧷
Purpose: Accurately localize non-palpable breast lesions pre-surgery.
Ultrasound advantage:
Quick, efficient, and ideal for complex locations (near implants or chest wall).
Used before surgical excision.
2. Large-Core Needle Biopsy 💉
Purpose: Obtain core samples from solid masses.
Benefits:
Faster, more comfortable, and cost-effective than stereotactic biopsy.
Best for ultrasound-visible lesions.
❌ Not ideal for clustered pleomorphic microcalcifications (better seen on mammography).
Ultrasound-Guided Interventional Procedures
🖼 3. Ductography / Galactography 🥛
Used for: Evaluating nipple discharge in nonpregnant/nonlactating patients.
Common cause of discharge: Benign papilloma.
Discharge types: Clear, bloody, yellow, brown, black.
Contraindications: ❌ Mastitis, abscess, pregnancy, lactation.
4. Magnetic Resonance Imaging (MRI) 🧲
Most sensitive method for breast cancer detection.
Used for:
Multifocal/multicentric disease 🔍
Treatment response 💊
Pre-op staging 🎭
Uses contrast: Gadolinium ➡ Tumors enhance quickly & wash out.
Rim enhancement = Strong suspicion of malignancy 🔴
✅ Best soft-tissue contrast & multiplanar imaging.
⚠ Limitations/Contraindications:
Not widely available in all regions 🌍
Expensive 💸
Contraindicated in:
Patients with pacemakers, metal joints ⚙
Uncontrolled claustrophobia 😰
5. SPECT (Single Photon Emission Computed Tomography) ☢
Purpose: Tracks radioactive material to locate cancer cells or map blood flow.
Injected agent: Radioisotope.
Advantage:
More sensitive than planar imaging in obese patients.
Used for sentinel node detection and mapping.
6. Sentinel Node Procedure / Lymphoscintigraphy 🧭
Goal: Identify first lymph node ("sentinel node") receiving drainage from a tumor.
Agent: Blue dye and/or Technetium-99m radioisotope.
"Hot spot" indicates sentinel node for biopsy.
✅ If negative → 95–100% accurate in ruling out axillary metastasis.
✨ Replaces full axillary lymph node dissection (ALND) to avoid:
Lymphedema, nerve damage, or shoulder mobility loss.
Other Imaging Modalities
🧬7. Automated Breast Ultrasound (ABUS) 🤖
Purpose: Standardize imaging & reduce operator dependency.
Ideal for: Dense breast tissue and small lesion detection.
Technology:
Volumetric scan + 3D multiplanar reconstruction 🧩
Water path system + compression for better imaging.
✅ Improves reproducibility and early detection.
8. Breast Elastography 🌈
Evaluates: Stiffness and size of breast lesions.
Malignant tumors:
Appear stiffer than benign ones
Often larger on elastography than B-mode due to desmoplastic response.
Color coded (e.g., red = soft, blue = hard) for easy interpretation.
✅ Increases specificity, sensitivity, and accuracy of ultrasound.
Emerging Sonographic Technologies
🔍 Breast Ultrasound Evaluation Overview 📚 Anatomy & Tissue Characteristics
The breast has three layers (from skin to chest wall):
Subcutaneous layer
Mammary (glandular) layer
Retromammary layer
Fatty tissue = Hypoechoic
Ducts, glands, Cooper’s ligaments = Echogenic
TDLUs (Terminal Duct Lobular Units): Basic functional unit; surrounded by connective tissue.
Cooper’s ligaments: Echogenic connective tissue septa anchoring breast structures to skin.
Lymphatic drainage: Primarily to axillary lymph nodes.
Primary function: Fluid transport.
🩺 Breast Imaging Categories
Screening: Physical exam + mammography
Diagnostic Interrogation: Follow-up and problem solving
Interventional: Biopsy and localization
🎯 Goals of Breast Evaluation
Properly classify lesions by malignancy risk
Begin with distinguishing cystic vs. solid lesions
📊 Sonographic Features of Lesions ✅ Benign Features
Smooth, rounded margins
“Wider than tall” (parallel to chest wall)
Compressible and may shift with palpation
Isoechoic or hyperechoic to fat
Limited vascularity
Well-defined, mobile, rubbery (e.g., fibroadenoma)
⚠ Malignant Features
Irregular, spiculated margins
“Taller than wide” (vertical growth)
Hypoechoic
Non-compressible, stone-hard, gritty
Posterior shadowing
Infiltrates planes → skin dimpling, nipple retraction
Microcalcifications
Intratumoral vessels seen on Doppler
Skin ulceration or nipple inversion (late signs)
💡 Lesion Classifications 🔹 Cysts
May be simple, complicated, or complex
Complex cysts (e.g., with septations, mural nodules, internal echoes) may need aspiration/biopsy
🔹 Solid Masses
Fibroadenomas: Most common in teenagers
Most solid lesions don’t enhance (except fibroadenomas)
🚨 Clinical Symptoms of Concern
Palpable mass
Nipple discharge (spontaneous or induced)
Pain (less commonly associated with cancer)
Skin dimpling, ulceration, nipple retraction (red flags for malignancy)
KEY PEARLS