Chapter 21: Acute Respiratory Disorders
1/29
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
30 Terms
Chapter 21: Acute Respiratory Disorders
Airway structures allow air entry for oxygenation and tissue perfusion
Nursing priority in acute respiratory disorders: maintain a patent airway (promotes oxygenation)
Older adults are at higher risk due to:
Decreased pulmonary reserves
Decreased lung elasticity
Thickened alveoli
Increased susceptibility to infection
Common acute respiratory disorders:
Rhinitis
Sinusitis
Influenza
COVID-19
Pneumonia
Health Promotion and Disease Prevention
Perform hand hygiene (prevents transmission of bacteria and viruses)
Encourage immunizations:
Influenza and pneumonia vaccines
Especially for young children, older adults, chronically ill, and immunocompromised clients
Limit exposure to airborne allergens (prevents hypersensitivity reactions)
Promote smoking cessation (reduces airway inflammation and infection risk)
Acute Respiratory Disorders Risk Factors
Extreme age (very young or advanced age)
Recent exposure to viral, bacterial, or influenza infections
Lack of current immunizations (influenza, pneumonia)
Exposure to:
Plant pollen
Molds
Animal dander
Foods
Medications
Environmental contaminants
Tobacco smoke
Substance use:
Alcohol
Cocaine
Chronic lung disease:
Asthma
Emphysema
Immunocompromised status
Presence of a foreign body
Conditions increasing aspiration risk:
Dysphagia
Impaired ability to mobilize secretions:
Decreased level of consciousness
Immobility
Recent abdominal or thoracic surgery
Inactivity and immobility
Rhinitis
Inflammation of the nasal mucosa and often the sinus mucosa
Causes:
Infection (viral or bacterial)
Allergens
Prevalence: affects ~10–30% of the global population annually
Commonly coexists with asthma and allergies
Classification:
Acute
Chronic
Nonallergic
Allergic (seasonal or perennial)
Types
Viral (common cold)
Caused by viruses
Spread via respiratory droplets (sneezing, coughing) or direct contact
Allergic
Allergen exposure triggers histamine and mediator release from WBCs
Mediators bind to blood vessel receptors → capillary leakage
Results in local edema and swelling
Rhinitis Expected Findings
Excessive nasal drainage and congestion
Rhinorrhea (runny nose)
Purulent nasal discharge
Sneezing and pruritus of nose, throat, and ears
Itchy, watery eyes
Sore, dry throat
Red, inflamed, swollen nasal mucosa
Low-grade fever, fatigue, cough (viral)
Diagnostic testing:
Allergy testing to identify triggers
Rhinitis Care
Encourage rest (8–10 hr/day)
Encourage increased fluids (≥2,000 mL/day) (thins secretions)
Use home humidifier or inhale steam from hot shower (moistens airways)
Teach proper tissue disposal and cough etiquette (limits transmission)
Recommend saline nasal sprays (soothe mucosa, loosen secretions)
Warm saltwater gargles (relieve sore throat)
Reinforce hand hygiene (prevents spread)
Therapeutic Management
Depends on underlying cause (viral vs allergic vs bacterial)
Rhinitis Meds
Antihistamines (block histamine effects)
Example: brompheniramine/pseudoephedrine
Leukotriene inhibitors
Example: montelukast
Mast cell stabilizers
Example: cromolyn
Older adults: monitor for vertigo, hypertension, urinary retention
Decongestants
Example: phenylephrine
Vasoconstriction reduces edema
Use only 3–4 days (prevents rebound congestion)
Expectorants
Example: guaifenesin (promotes mucus clearance)
Intranasal glucocorticoid sprays
Most effective for prevention and treatment of seasonal and perennial rhinitis
Antipyretics
For fever
Antibiotics/antimicrobials
Only if bacterial infection is identified
Client Education
Perform frequent hand hygiene (reduces transmission)
Limit exposure to others during acute symptoms (protects vulnerable populations)
Avoid known allergens (foods, medications, environmental triggers)
Complementary therapies:
Echinacea, vitamin C, zinc may reduce severity and duration (limited evidence)
Sinusitis
Inflammation of the mucous membranes of one or more sinuses
Most commonly affects maxillary and frontal sinuses
Mucosal swelling blocks drainage of secretions → infection risk
Often follows rhinitis
Associated factors:
Deviated nasal septum
Nasal polyps
Inhaled air pollutants or cocaine
Facial trauma
Dental infections
Loss of immune function
Common causative organisms:
Viral
Streptococcus pneumoniae
Haemophilus influenzae
Diplococcus
Bacteroides
Sinusitis Expected Findings
Nasal congestion
Headache
Facial pressure or pain (worse when bending forward)
Cough
Bloody or purulent nasal drainage
Tenderness on palpation of:
Forehead
Orbital areas
Facial areas
Fever patterns:
Low-grade fever (viral)
High-grade fever (bacterial)
Sinusitis Exams
Diagnostic Procedures
CT scan or sinus x-rays to confirm diagnosis (supports clinical findings)
Endoscopic sinus lavage or surgery may be used to relieve obstruction and promote drainage
Sinusitis Care
Encourage steam humidification (reduces congestion)
Promote sinus irrigation and saline nasal sprays (improves drainage)
Apply hot and wet packs to sinuses (relieves pain and pressure)
Teach increased fluid intake and adequate rest (thins secretions)
Discourage air travel, swimming, and diving (prevents pressure changes)
Encourage tobacco cessation in all forms (reduces mucosal irritation)
Instruct on proper technique for sinus irrigation and nasal spray use
Therapeutic Procedures
Repair of deviated nasal septum
Surgical excision of nasal polyps
Client Education
Sinus irrigation and saline sprays can relieve congestion and reduce antibiotic use
Report severe symptoms immediately:
Severe headache
Neck stiffness (nuchal rigidity)
High fever
(may indicate complications)
Sinusitis Meds
Nasal decongestants (reduce mucosal swelling)
Example: phenylephrine
Broad-spectrum antibiotics
Example: amoxicillin
Use limited to confirmed bacterial infection
Pain relief
NSAIDs
Acetaminophen
Aspirin
Client Education
Start OTC decongestants at first signs of sinusitis
Avoid use longer than 3 to 4 days (prevents rebound congestion)
Sinusitis Complications
Meningitis or encephalitis (pathogens enter bloodstream from sinuses)
Mucocele formation (cyst in paranasal sinus)
A nurse in a clinic is assessing a client who has sinusitis. Which of the following techniques should the nurse use to identify manifestations of this disorder?
a
Percussion of posterior lobes of lungs
b
Auscultation of the trachea
c
Inspection of the conjunctiva
d
Palpation of the orbital areas
d Palpation of the orbital areas
A client who has sinusitis may report tenderness when the orbital, frontal, and facial areas are palpated.
Influenza
Acute, highly contagious viral respiratory infection
Occurs seasonally as epidemics, most often in fall and winter
Affects children and adults of all ages
Caused by several virus families that vary yearly
Adults are contagious:
24 hr before symptoms appear
Up to 5 days after symptom onset
Pandemic Influenza
Originates in animals or birds with mutation allowing human transmission
High potential for global spread
Examples:
H1N1 (swine flu)
H5N1 (avian flu)
Influenza Expected Findings
Severe headache and myalgias
Chills
Fatigue and weakness
Fever
Cough
Severe diarrhea and cough (avian flu)
Hypoxia (avian flu) (impaired gas exchange)
Influenza Exams
Diagnostic Procedures
Viral cultures and lab tests available
CDC recommends testing only if results will guide treatment decisions
Influenza Care
Maintain droplet and contact precautions for hospitalized clients with pandemic influenza (prevents transmission)
Provide saline gargles (relieves throat irritation)
Monitor hydration status, intake, and output (prevents dehydration)
Administer IV fluids as prescribed
Monitor respiratory status closely (early detection of hypoxia)
Interprofessional Care
Consult respiratory therapy for respiratory support
Notify community health officials of outbreaks
Coordinate with state and federal public health agencies during pandemics for containment and prevention measures
Client Education
Obtain yearly influenza vaccination when available
Perform frequent hand hygiene and follow cough etiquette (limits spread)
Avoid crowds and close personal contact during outbreaks
If symptomatic:
Increase fluid intake
Rest
Stay home from work or school
Avoid travel to areas with identified pandemic influenza
Follow public health announcements and early warning systems during pandemics
Influenza Meds
Antivirals
Examples:
Amantadine
Rimantadine
Ribavirin
Oseltamivir
Zanamivir
Peramivir
Antivirals shorten illness duration when started early
Oral zanamivir and oral oseltamivir commonly used
During pandemics, antivirals may be distributed broadly
Client Education
Start antiviral therapy within 24 to 48 hr of symptom onset (maximizes effectiveness)
Influenza Vaccines
Quadrivalent or trivalent vaccines prepared annually based on predicted strains
Annual vaccination recommended for everyone ≥6 months of age
High-risk groups requiring vaccination:
History of pneumonia
Chronic medical conditions
Adults >65 years
Pregnant women
Health care workers
H1N1 vaccine available for general population
H5N1 vaccine stockpiled for pandemic use
Influenza Complications
Pneumonia
Higher risk in older adults
Higher risk in debilitated or immunocompromised clients
A nurse is teaching a group of clients about influenza. Which of the following client statements indicates an understanding of the teaching?
a
“I should wash my hands after blowing my nose to prevent spreading the virus.”
b
“I need to avoid drinking fluids if I develop symptoms.”
c
“I need a flu shot every 2 years because of the different flu strains.”
d
“I should cover my mouth with my hand when I sneeze.”
a
“I should wash my hands after blowing my nose to prevent spreading the virus.”
Pneumonia
Inflammatory lung process with excess fluid in alveoli
Caused by:
Infectious organisms
Aspiration of irritants (fluid or foreign body)
Inflammation of lung parenchyma → edema and exudate filling alveoli (impaired gas exchange)
Can be:
Primary disease
Complication of another illness (common after influenza)
High-risk populations:
Infants and young children
Older adults
Immunocompromised clients
Immobility is a major contributing factor
Types of Pneumonia
Community-Acquired Pneumonia (CAP)
Most common
Often a complication of influenza
Health Care–Associated Pneumonia (HCAP)
Higher mortality
More antibiotic resistance
Acquired 24–48 hr after exposure
Associated with non-hospital admission and health care contact
Hospital-Acquired Pneumonia (HAP)
Occurs >48 hr after hospital admission
Ventilator-Associated Pneumonia (VAP)
Occurs >48 hr after intubation
Types of Pneumonia
Community-Acquired Pneumonia (CAP)
Most common
Often a complication of influenza
Health Care–Associated Pneumonia (HCAP)
Higher mortality
More antibiotic resistance
Acquired 24–48 hr after exposure
Associated with non-hospital admission and health care contact
Hospital-Acquired Pneumonia (HAP)
Occurs >48 hr after hospital admission
Ventilator-Associated Pneumonia (VAP)
Occurs >48 hr after intubation
Pneumonia Expected Findings
Anxiety
Fatigue
Weakness
Chest discomfort from coughing
Confusion from hypoxia (most common sign in older adults)
Physical Assessment
Fever and chills
Flushed face
Diaphoresis
Shortness of breath or dyspnea
Tachypnea
Sharp pleuritic chest pain
Productive cough
Yellow-tinged sputum
Purulent, blood-tinged, or rust-colored sputum (may be absent)
Crackles and wheezes
Dullness to percussion over consolidated areas
Decreased oxygen saturation (normal 95%–100%)
Pneumonia Exams
Sputum Culture and Sensitivity
Obtain specimen before antibiotics
Suction specimen if client cannot cough
Older adults may have weak cough and difficulty expectorating
CBC
Elevated WBC count (may be absent in older adults)
ABGs
Hypoxemia
PaO₂ <80 mm Hg
Blood Cultures
Rule out bacteremia
Electrolytes
Signs of dehydration:
Elevated BUN
Hypernatremia
Diagnostic Procedures
Chest X-Ray
Shows lung consolidation
May be negative early in disease
Important in older adults due to vague early symptoms
Pulse Oximetry
Usually <95% in pneumonia
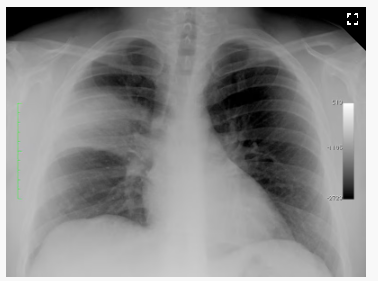
Pneumonia (Image)
Pneumonia Care
Position to maximize ventilation:
High-Fowler’s (≈90%) if not contraindicated
Encourage coughing or suctioning (clears secretions)
Administer prescribed breathing treatments and medications
Administer oxygen therapy
Monitor skin integrity around oxygen devices
Encourage incentive spirometry (prevents alveolar collapse)
Structure activity with rest periods
Promote nutrition and hydration:
Increased work of breathing increases caloric needs
Adequate nutrition reduces secondary infection risk
Fluids 2–3 L/day unless contraindicated (thins secretions)
Provide rest for dyspneic clients
Reassure clients experiencing respiratory distress
Interprofessional Care
Respiratory therapy:
Inhalers
Breathing treatments
Suctioning
Nutrition services for weight changes
Rehabilitation services for prolonged weakness and activity intolerance
Client Education
Complete all prescribed medications
Rest as needed
Maintain hand hygiene
Avoid crowded areas during recovery
Recovery may take time
Obtain influenza and pneumonia vaccines
Stop tobacco use if applicable
Pneumonia Meds
Antibiotics
Used to destroy infectious pathogens
Common classes:
Penicillins
Cephalosporins
Often started IV, then switched to oral
Obtain cultures before first dose
Begin antibiotics after specimen collection
Nursing Actions
Monitor for frequent stools
Monitor kidney function, especially in older adults
Client Education
Take antibiotics as prescribed
Some penicillins should be taken:
With food
Or 1 hr before or 2 hr after meals (specific agent dependent)
Bronchodilators
Reduce bronchospasm and airway irritation
Short-acting beta₂ agonists
Albuterol (rapid relief)
Anticholinergics
Ipratropium (blocks parasympathetic response)
Methylxanthines
Theophylline (narrow therapeutic range)
Nursing Actions
Monitor theophylline levels (toxicity risk)
Tachycardia, nausea, diarrhea
Monitor for tremors and tachycardia with albuterol
Monitor for dry mouth, palpitations, headache, blurred vision with ipratropium
Client Education
Suck on hard candy for dry mouth (ipratropium)
Increase fluid intake unless contraindicated
Anti-Inflammatories
Reduce airway inflammation
Glucocorticoids
Fluticasone
Prednisone
Monitor for:
Immunosuppression
Fluid retention
Hyperglycemia
Hypokalemia
Poor wound healing
Nursing Actions
Monitor immunity status
Monitor blood glucose
Monitor weight and edema
Assess mouth and throat for aphthous ulcers
Client Education
Take steroids with food
Do not stop steroids abruptly
Report black, tarry stools
Increase fluid intake
Pneumonia
Atelectasis
Alveolar collapse from inflammation and edema
Increased hypoxemia risk
Findings:
Dyspnea
Hypoxemia
Diminished or absent breath sounds
Chest x-ray shows density
Bacteremia (Sepsis)
Pathogens enter bloodstream from lungs
Acute Respiratory Distress Syndrome (ARDS)
Persistent hypoxemia despite oxygen therapy
Reduced lung volume and elasticity
Worsening dyspnea with noncardiac pulmonary edema
Chest x-ray: ground-glass appearance
ABGs:
Hypercapnia
Decreased oxygen saturation despite oxygen therapy
A nurse is monitoring a group of clients for increased risk for developing pneumonia. Which of the following clients should the nurse expect to be at risk?
Select all that apply.
a
Client who has dysphagia
b
Client who has AIDS
c
Client who was vaccinated for pneumococcus and influenza 6 months ago
d
Client who is postoperative and has received local anesthesia
e
Client who has a closed head injury and is receiving mechanical ventilation
f
Client who has myasthenia gravis
a
Client who has dysphagia
b
Client who has AIDS
e
Client who has a closed head injury and is receiving mechanical ventilation
f
Client who has myasthenia gravis
A nurse is assessing a client who, upon awakening, was disoriented to person, place, and time. The client reports chills and chest pain that is worse upon inspiration. Which of the following actions is the nursing priority?
a
Obtain baseline vital signs and oxygen saturation.
b
Obtain a sputum culture.
c
Obtain a complete history from the client.
d
Informed client about recommended pneumococcal vaccine.
a
Obtain baseline vital signs and oxygen saturation.