visual fields III
1/46
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
47 Terms
explain what the px is seeing through each eye and how this corresponds with a part of the retina - tells us what part of the visual field is being affected - important concept to understand (everything is inverted)
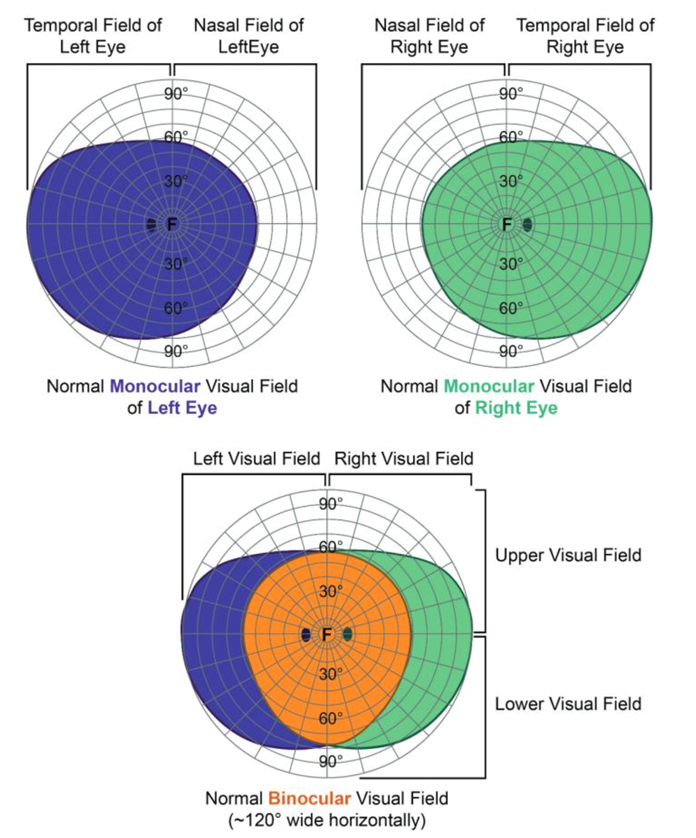
image falls below horizontal midline – falls on superior retina – related to inferior visual field
image falls above horizontal midline – falls on inferior retina – related to superior visual field
image falls in the right visual field/right of vertical midline - image falls on the left side of each retina - RE: nasal retina and LE: temporal retina
image falls in the left visual field/left of vertical midline - image falls on the right side of each retina - RE: temporal retina and LE: nasal retina
Fields cross horizontally
(Right field → left retina; Left field → right retina)Fields flip vertically
(Upper field → lower retina; Lower field → upper retina)
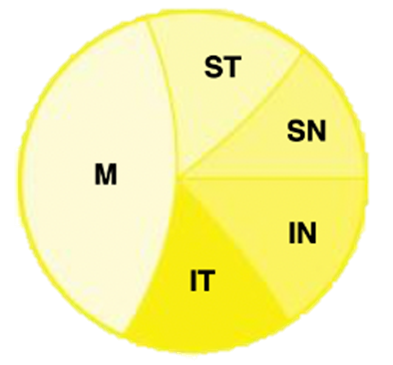
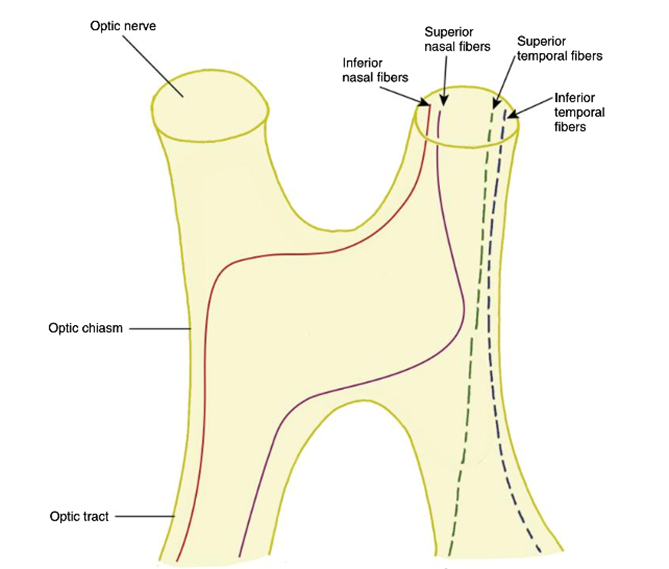
name the fibers within the optic nerve (5)
macular fibers
inferior nasal
superior nasal
inferior temporal
superior temporal
explain the position of the fibers within the optic nerve - once they have entered (3)
Macular fibres move to the centre
The rest of the fibres take up positions as shown (around the centre/around macula fibers)
as we reach the optic chiasm this will be the structure within the optic nerve
explain position of (nasal) fibers in the optic chiasm (4)
Nasal Fibres cross over at the Chiasm - depending on where they are coming from they cross over differently:
Inferior Nasal fibres – cross over at Anterior Chiasm
Superior nasal fibres – cross over at Posterior Chiasm
Notes that they don’t cross in the central chiasm (crossing occurs mainly at edges) - and note that temporal fibers do not cross and continue on the same side (as shown in image)
what is the optic tract and what is it made from
Each optic tract carries information from the same visual field (right or left), made from:
Crossed fibres (from nasal retina of opposite eye)
Uncrossed fibres (from temporal retina of same eye)
So the tract contains both eyes’ information, but only for one side of the visual field.
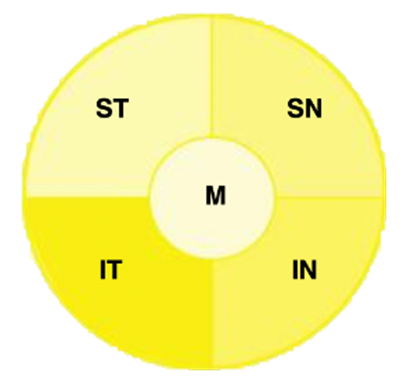
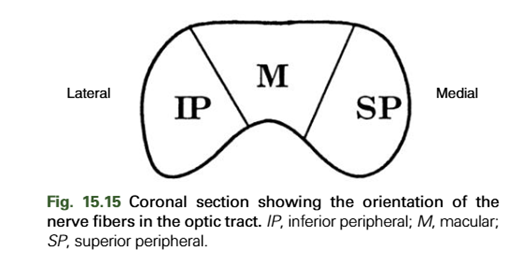
explain the position of the fibers in the optic tract (5)
Macular Fibres – Crossed and uncrossed (come from both eyes) - sit centrally in the tract - macular vision from both eyes is carried in every optic tract
Superior Peripheral Fibers : from the medial (inner) side of the optic tract
the tract contains 2 sources: Ipsilateral Sup-Temp (from the same side - no crossing) + Contralateral Sup-Nasal (from the opposite side - crossed at the chiasm) - corresponds to same part of visual field
Inferior Peripheral: from the lateral (outer) side of the optic tract
the tract contains 2 sources: Ipsilateral Inf-Temp + Contralateral Inf-Nasal - corresponds to same part of visual field
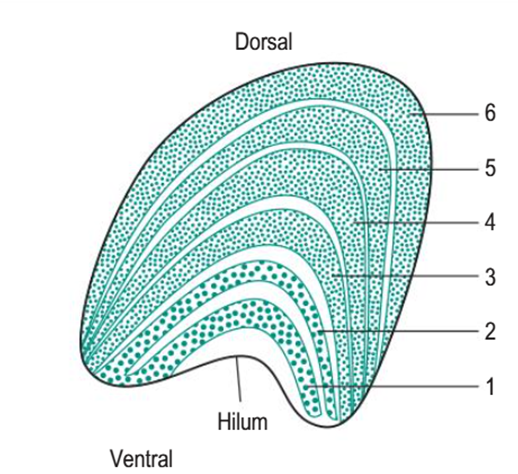
how many layers does the LGN (lateral geniculate nucleus) have
6
what do each of the layers deal with (which fibers)
Layers 1, 4 and 6 deal with:
–Crossed (nasal) fibres
–Contralateral Retina (from opposite side)
Layers 2, 3 and 5 deal with:
–Uncrossed (temporal) fibres
–Ipsilateral Retina (from same side)
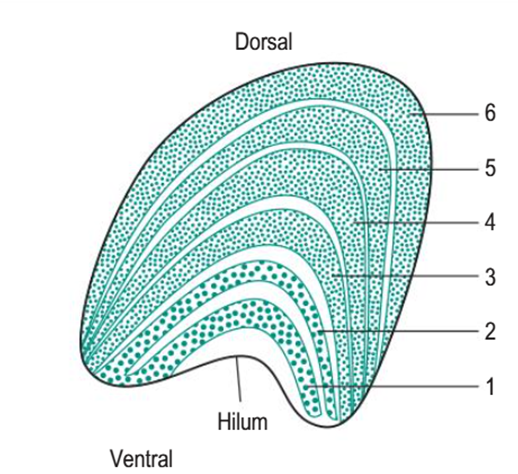
what are the different types of cellular layers and what layers of the LGN do they make up (3)
Magnocellular Layers - layers 1+2
•Magno Cell: larger cells at the bottom of the LGN - contains:
–Retinal Rods
–Magno Ganglion Cells
Parvocellular Layers - layers 3-6
•Parvo cells: smaller cells:
–Retinal Cones - more detail than rods
–Parvo Ganglion Cells
Koniocellular Layers –In between Layers 1-6 (white parts in between all the layers)
•Koniocellular cells:
–Ganglion Cells
»Process Colour - important role in LGN
what are optic radiations
bundles of nerve fibres that carry visual information from the LGN to the primary visual cortex (V1) in the occipital lobe
explain how the inferior optic radiations are formed and the pathway of these inferior radiations (which corresponds to superior visual field)
Fibers leaving lateral LGN - Represent inferior retina - which sees the superior visual field
Inferior Radiations - head to occipital lobe via the temporal lobe
Form Meyer loops along the way - a forward looping pathway
why is the pathway of temporal lobe important
damage to the temporal lobe can lead to a superior quadrantanopia
explain how the superior radiations are formed and their pathway
Fibers leaving medial LGN - represent superior retina - which sees the inferior visual field
Superior Radiations travel through the parietal lobe - these fibers go more directly backwards through the parietal lobe
why is the parietal lobe important
Parietal lobe damage → Inferior quadrantanopia (“pie on the floor”)
describe where the macular fibers are located (3)
Macular fibers situated between superior and inferior fibers - in the middle (think of it like a sandwich)
macula has most detailed central vision - so brain gives it special central position
macular fibers will find their way to the occipital lobe as well
where is the primary visual cortex situated in and what are the 2 main parts of it
The primary visual cortex (V1) is in the occipital lobe
It is split into two main parts:
🔹 Cuneus gyrus → ABOVE the calcarine fissure
🔹 Lingual gyrus → BELOW the calcarine fissure
This division is important because different visual field information goes to each part
the more central vision is - the more posterior in the brain it is processed - fovea will be processed right at the back (star) — and more peripheral part of visual field is dealt with in the anterior part of brain
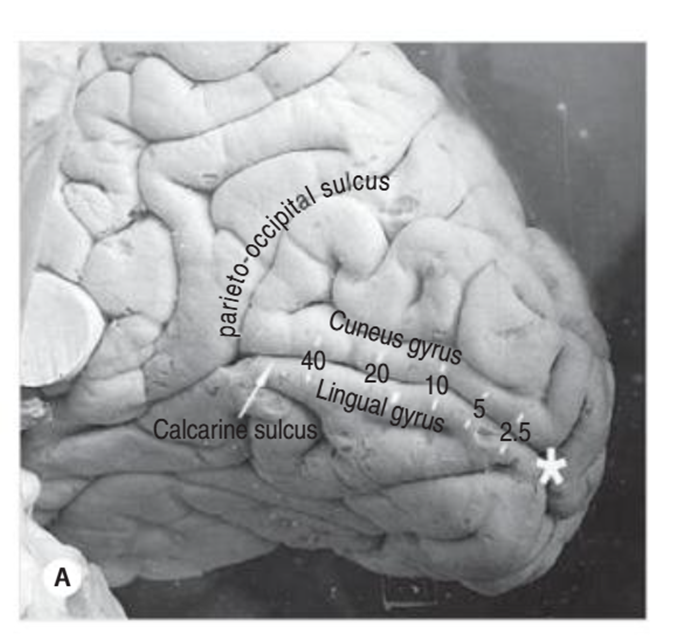
where do the superior radiations end up in the primary visual cortex
end up in the upper half of the of the visual cortex = Cuneus gyrus - ABOVE calcarine fissure
superior optic radiations carry information from the superior retina - which sees the inferior visual field
where do the inferior radiations end up in the primary visual cortex
end up in the lower half of the visual cortex - lingual gyrus - BELOW the calcarine fissure
inferior optic radiations carry information from the inferior retina - sees the superior visual field
what would damage above the calcarine fissure + below the calcarine fissure result in
Damage above the calcarine fissure (Cuneus) → loss in inferior visual field
Damage below (Lingual gyrus) → loss in superior visual field
explain where the macular fibers end up in the primary visual cortex (3)
More posterior the cortex relates more to central vision
Superior Macular fibers - Cuneus Gyrus - above calcarine fissure
Inferior Macular fibers - Lingual Gyrus - below calcarine fissure
define absolute scotoma vs a relative scotoma
absolute scotoma = complete loss of vision in that area of the visual field - expecting 0 in terms of sensitivity/dB
relative scotoma = reduction in vision/sensitivity - hasn’t gone completely black
if a visual defect obeys the horizontal midline - what does this indicate
the problem is retinal - lies in the retina
as retina is organized horizontally - Superior retinal problem → inferior visual field defect / Inferior retinal problem → superior visual field defect
glaucoma, retinal detachment etc.
if a visual defect does not obey the horizontal midline (vertical instead) - what does this indicate
the problem is post-retinal - in the visual pathways/brain - optic nerve, chiasm, radiations etc.
have to treat this as an emergency until proven otherwise - px will feel like they can’t see half (lost half their vision)
example: quadrantanopias, and homonymous hemianopia
lesions of the visual pathway
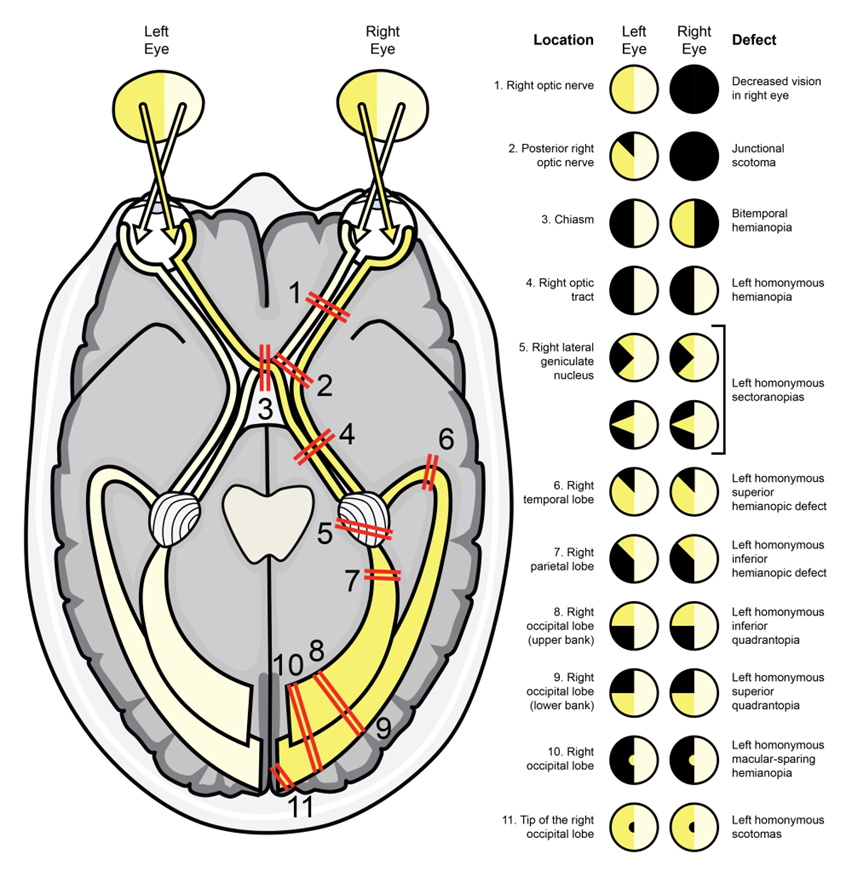
L visual field ends up in R side of the brain // R visual field ends up in L side of the brain
red lines show us what would happen if you had a lesion at that particular point
explain what a junctional scotoma is its effects (3)
affects both eyes to a certain extent - bilateral issue
meningioma compresses on one optic nerve and also the crossing nasal fibers from the other eye (these fibres are just entering the optic nerve from the chiasm)
so one eye gets optic nerve damage and the other eye gets superior temporal field loss
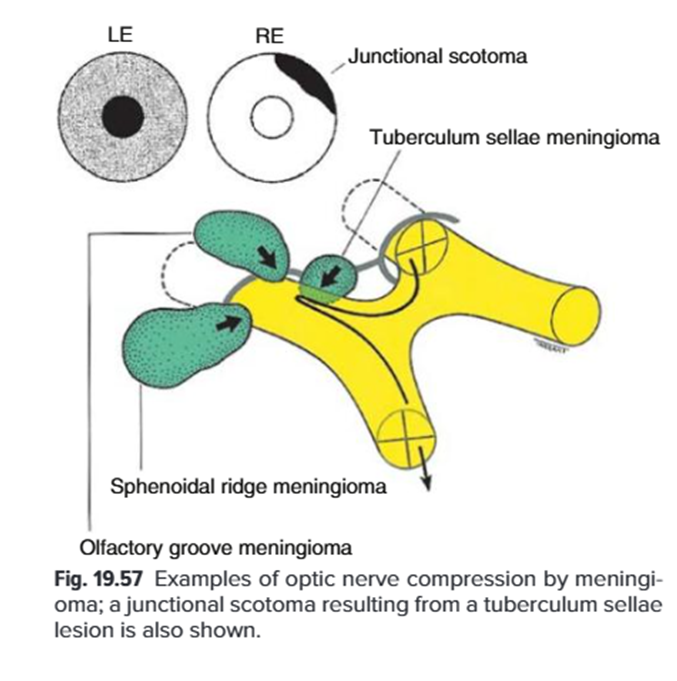
explain WHY a junctional scotoma affects both eyes (3)
due to the crossing inferior nasal retinal fibers - which are contained at the VERY front of the optic chiasm
so if the RE optic nerve was affected = visual field defect in the RE AND it also compresses the left inferior nasal retinal fibers that are crossing the chiasm into the right nerve
these inferior nasal fibers correspond to the superior temporal visual field - which is why the LE will show a superior temporal visual field defect
and vv
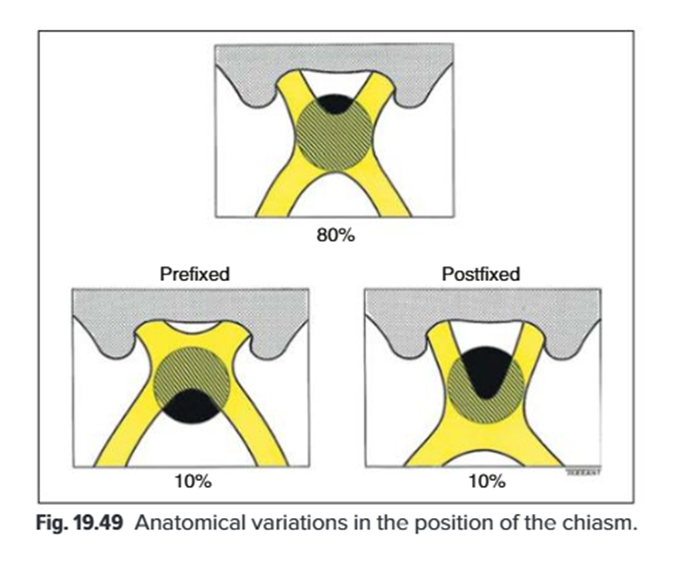
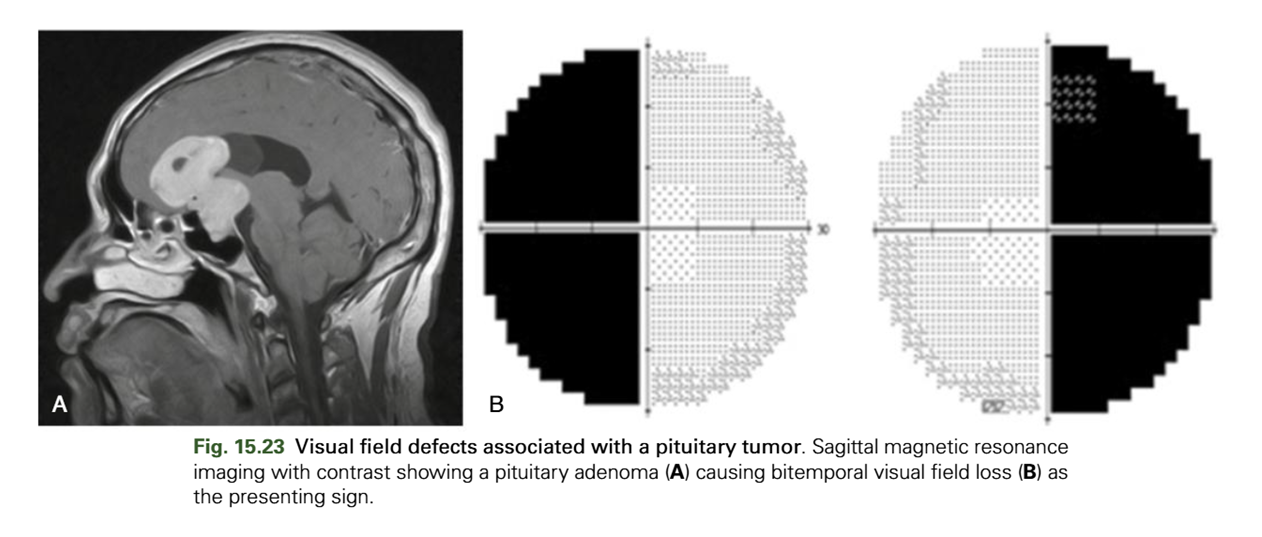
explain how a pituitary tumour affects the optic chiasm (4)
pituitary tumour causes englargment of p gland which is below (inferior) optic chiasm
p gland slightly anterior to OC
inferior nasal fibers cross over at anterior chiasm so will be affected sooner than the superior nasal fibers - affect the superior visual field sooner than the inferior visual field
tumour affects the inferior and superior fibers as the tumour fully grows - end up with a bi- temporal bi-lateral hemianopia
explain the effect of a temporal radiation lesion (4)
affect the temporal lobe - inferior radiations that travel through this part of the brain - which is why the superior visual field is affected
described as a pie in the sky
affects same side of visual field in both eyes (superior left/superior right visual field
macula sparing - doesn’t really affect the centre - it is quite a localised lesion
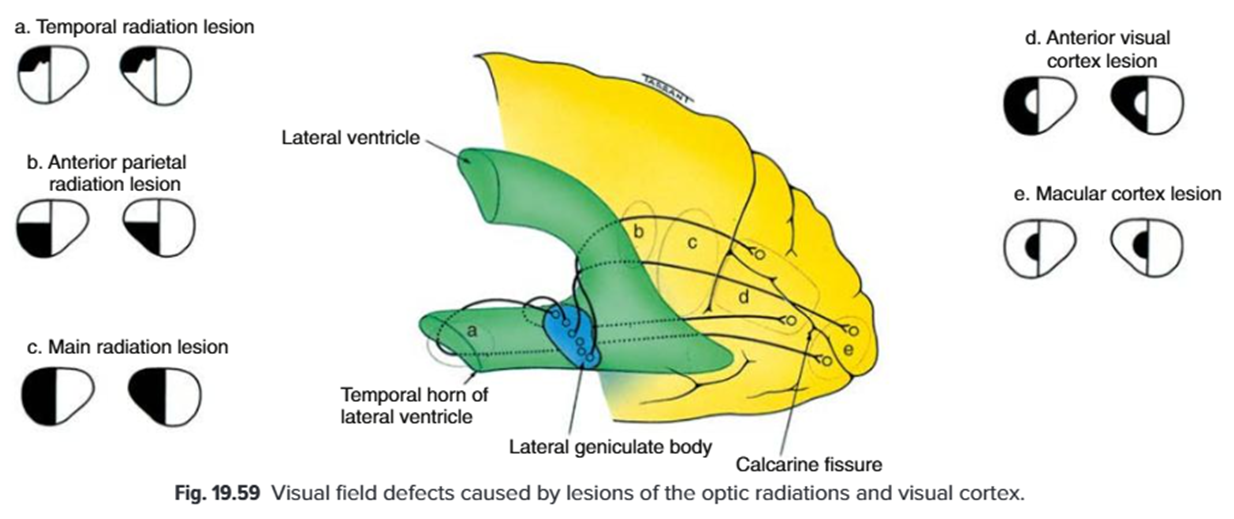
explain the effect of an anterior parietal radiation lesion (4)
affects the inferior visual field (either R or L) - let’s say L for this example
relating to right side of the brain - responsible for processing left visual field and VV
relates to superior retinal nerve fibers - as they travel through the parietal lobe
also affects macular fibers - no macula sparing
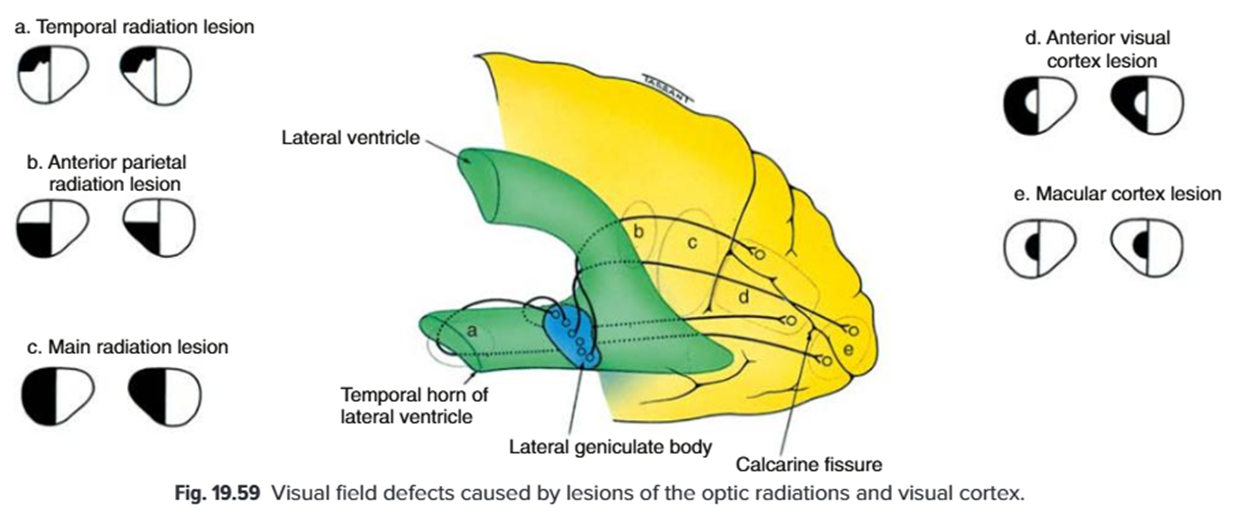
explain the effects of a main radiation lesion
moving further back fibers come together more - combined bundle of superior + inferior fibres traveling together just before reaching the occipital cortex
more congruity - bi lateral homonymous hemianopia
lose superior and inferior visual fields on the SAME SIDE - as optic radiation lesions cause homonymous defects
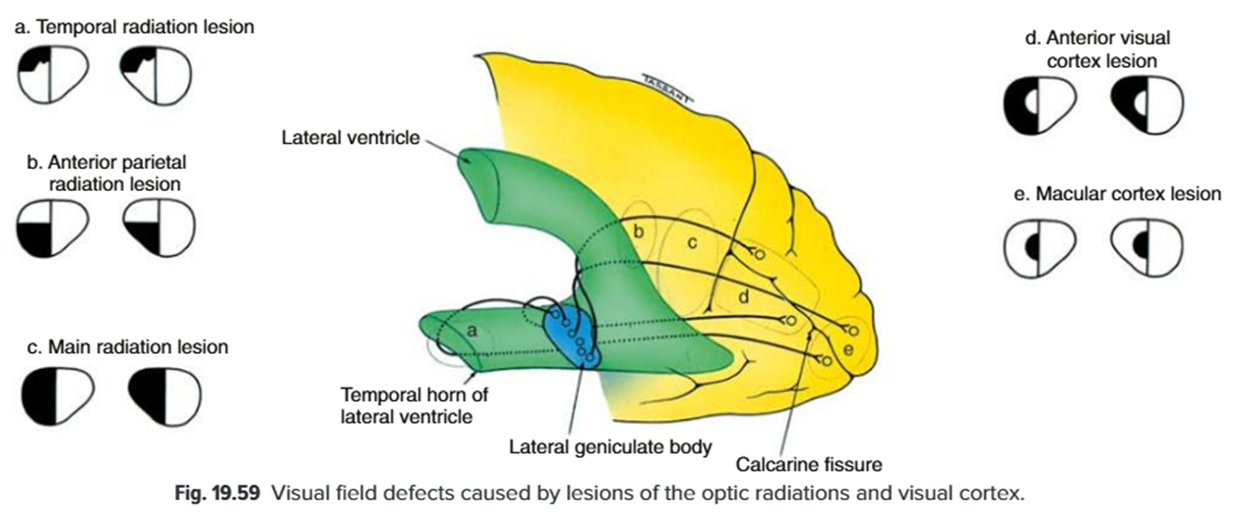
anterior visual cortex lesion
macular sparing - as it is not affecting that part of the brain
bi lateral homonymous hemianopia
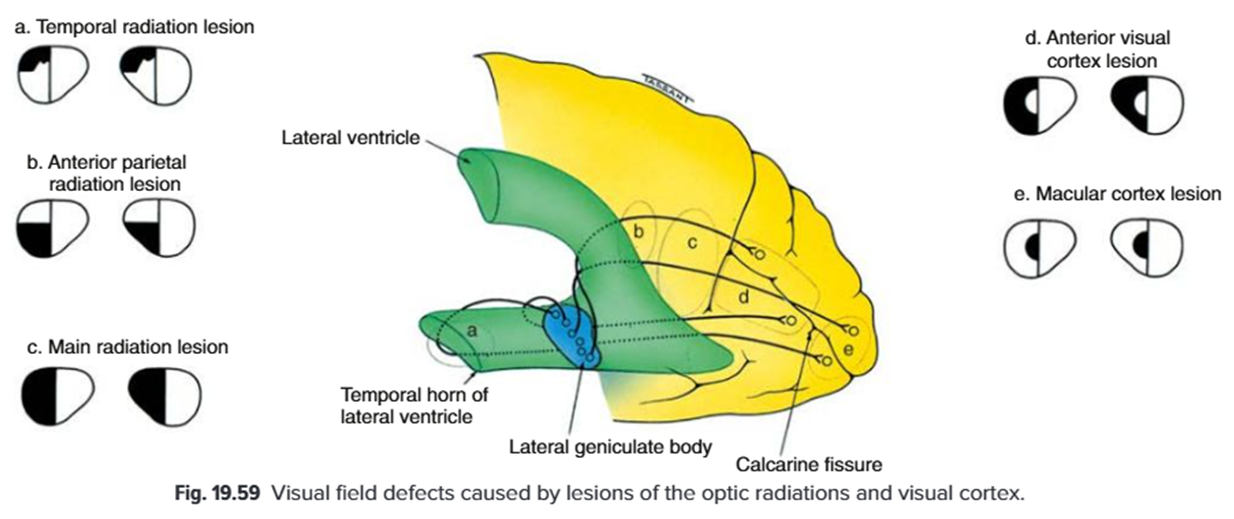
macular cortex lesion
peripheral visual field is fine but affecting the central vision
if affecting right side of the brain - we will get a LEFT central visual defect and VV
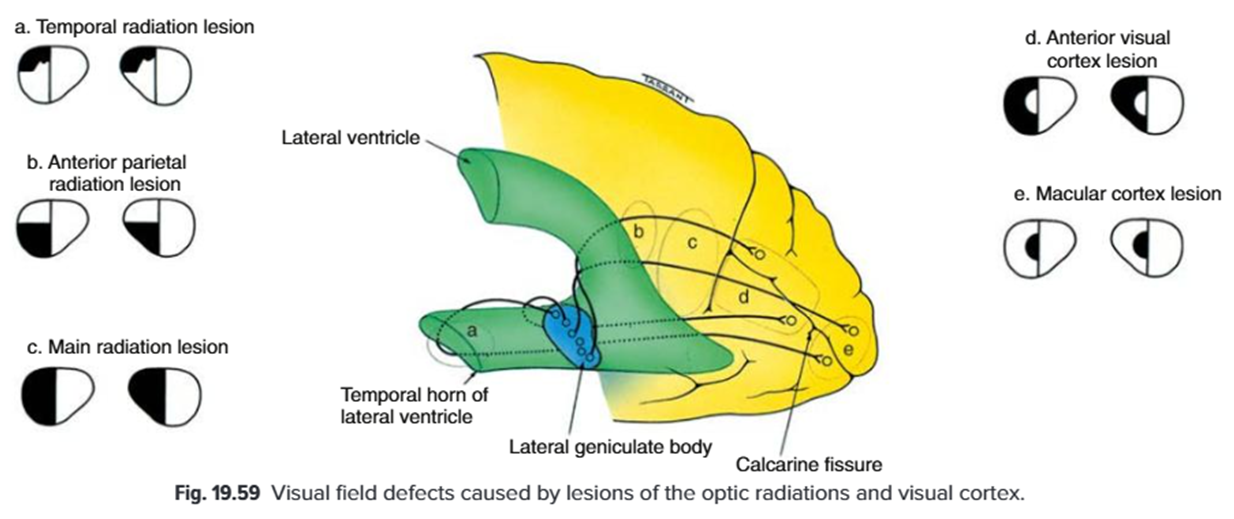
explain the effects of an occipital lobe lesion (4)
vertical midline is obeyed - post-retinal
if affecting R visual field in both eyes - will be affecting L part of brain and VV
affecting superior visual field - so inferior retinal fibers will be affected (lingal gyrus) and VV
R/L homonymous quadrantanopia
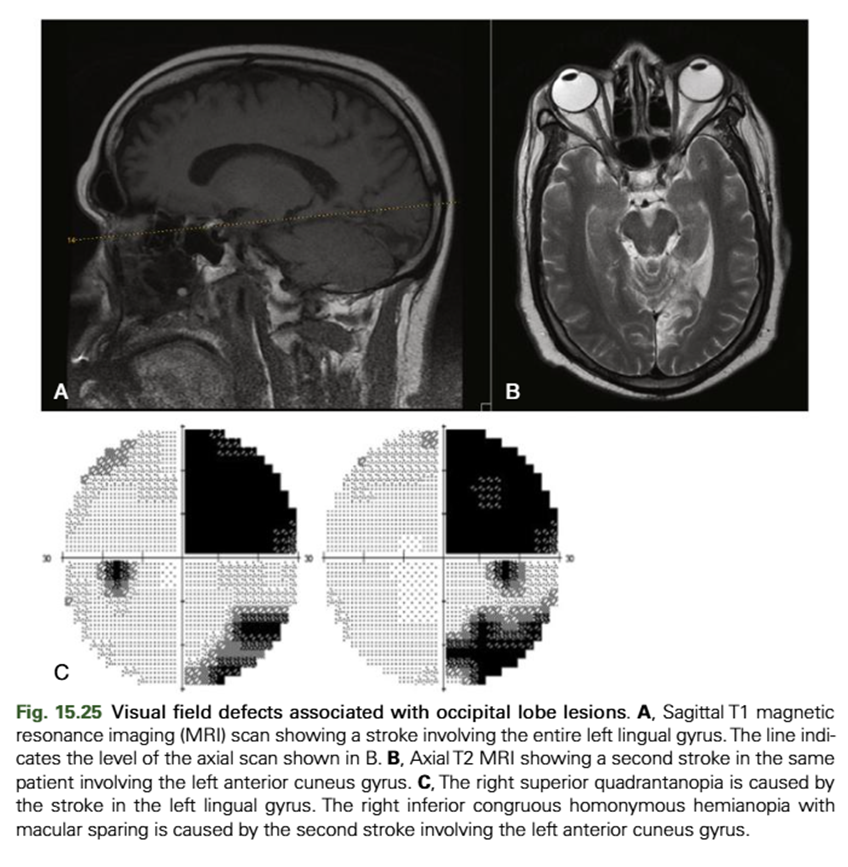
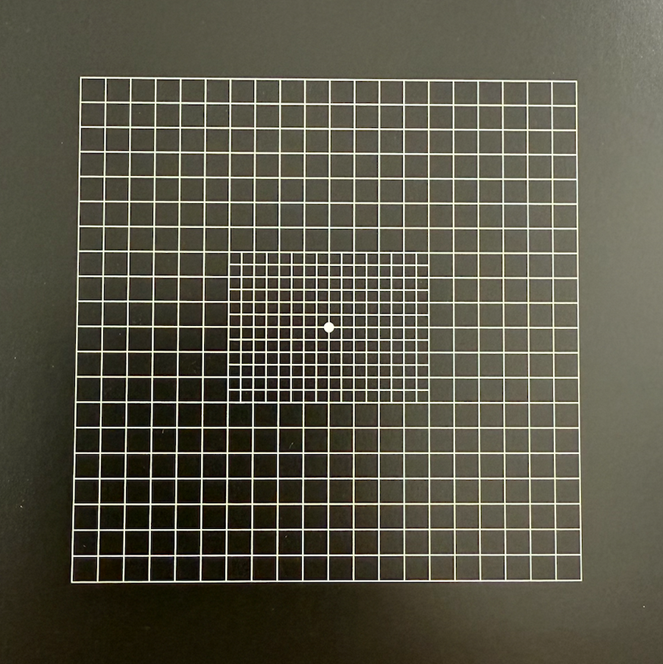
explain the usefulness of the Amsler grid (4)
Useful for a quick assessment of Macular Function : AMD and other acquired macular conditions
Alternative to 10-2
Can be used to self monitor at home - check one eye at a time, once a week - if they notice a change - come back in - if sudden could be dry AMD turning into wet AMD (emergency)
Used to look for scotomas (area of partial/complete vision loss in visual field) and metamorphopsia (visual distortion - straight lines look wavy/bent)
how many different charts does the amsler grid have
7
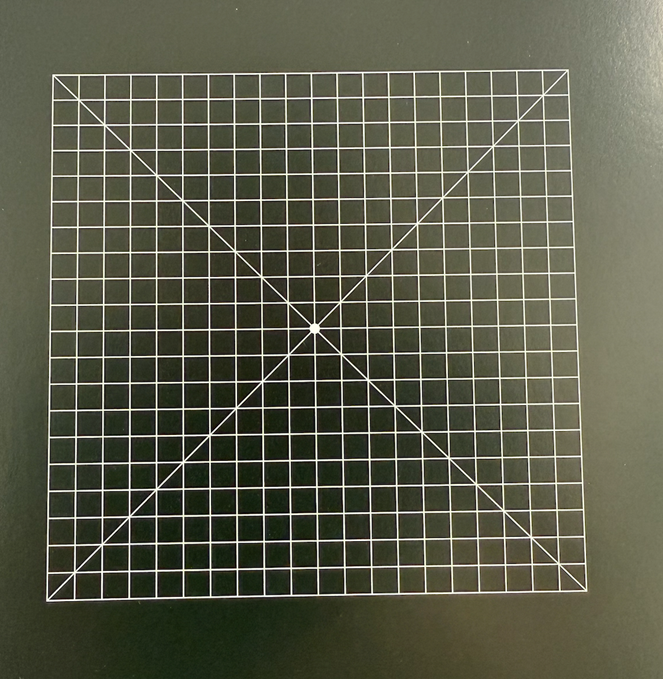
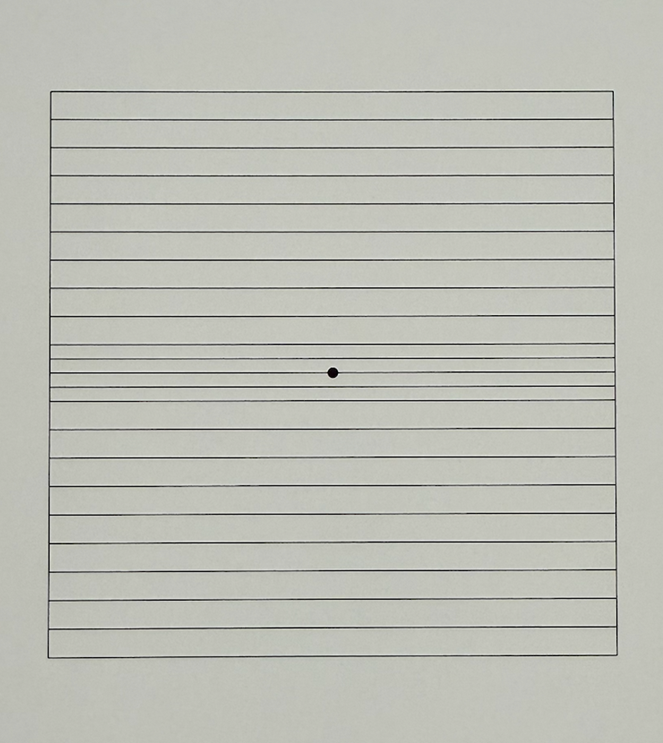
describe chart 1 (5)
•Standard Chart
•5mm squares
•Central white fixation target
•Each square subtends 1 degree when held at 30 cm - 10 deg superior, inferior, temporal and nasal
•White on black more sensitive than black on white - but usually black on white due to printing costs
describe chart 2 (1)
has diagonal lines - assist with fixation (for px who poor central fixation) - for more pronounced cases of AMD where central vision is more affected
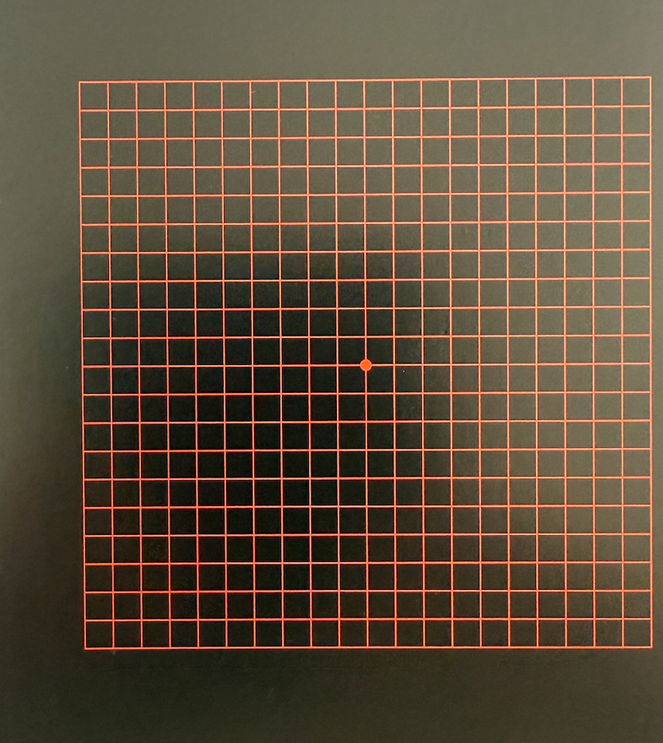
describe chart 3 (2)
•Red grid
•Useful for:
–Toxic Amblyopia (optic nerve becomes damaged due to exposure to certain toxins/drugs - leading to reduced vision) - reduced red colour sensitivity - red grid makes abnormalities easier to notice - detects dysfunction that a standard black/white grid may miss
–Optic Neuritis (inflammation of optic nerve) - loss of red colour sensitivity - early defects easier to detect than standard black/white grid
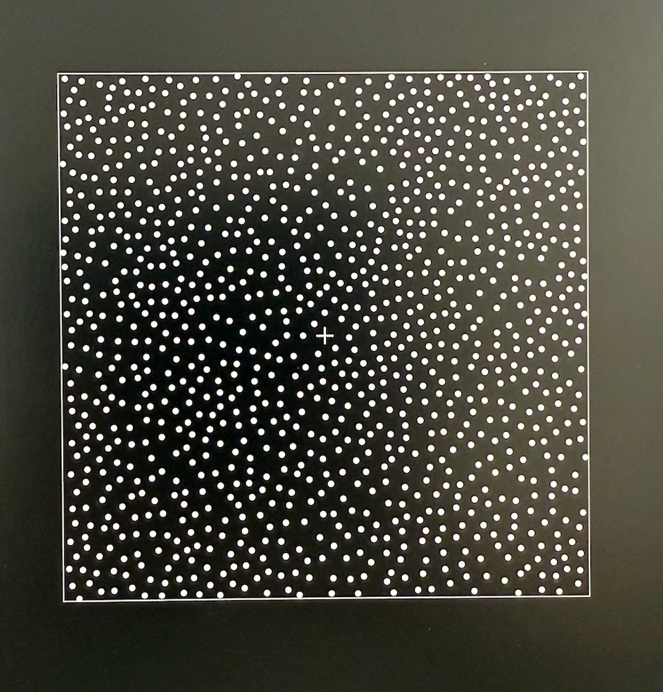
describe chart 4 (3)
•Scattered white dots
•Similar to Chart 1 for relative scotoma detection
•Cannot detect metamorphopsia (which we get if something is pushing the retina forward) - as no lines - no barrel effect
describe chart 5 (2)
•Can be rotated to change orientation of lines
•Investigates metamorphopsia at different meridians
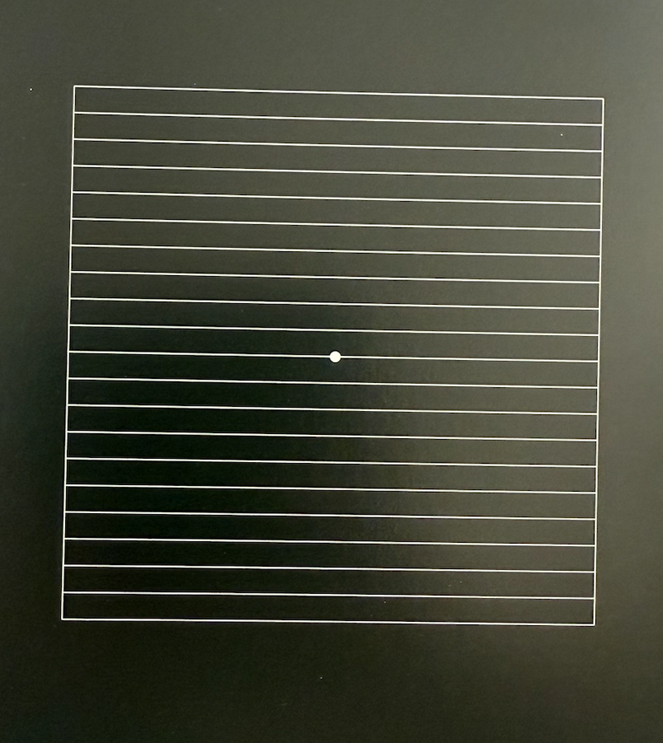
describe chart 6 (3)
•Similar to chart 5
•Black lines on white
Additional lines subtending 0.5 degrees - allows for greater sensitivity
describe chart 7 (2)
•0.5 degrees squares for the central 8 degrees
•Used for more subtle macular disease - early AMD / macular holes (slight central scotoma/distortion)
using chart 1 what is the first question we ask the patient and what do their answers tell us
•Can you see the central white dot?
–“Yes” = no Central Scotoma
–“Yes, but blurry” = Relative Central Scotoma
–“No, can only see it when I look to the side” = Use Chart No. 2 - may be using eccentric fixation - they have an absolute scotoma centrally
using chart 1 what is the second question we ask the patient and what does this tell us
•Can patient see all for sides and corners?
•Determines if large scotoma present.
–E.g. Glaucoma
-need to use a larger test
using chart 1 what is the 3rd question we ask the patient and what does this tell us (3)
•Are any of the square blurred or missing?
blurred = relative scotoma / missing = absolute scotoma
•Chart No. 4 can be helpful here too.
using chart 1 what is the 4th question we ask the patient and what does this tell us (2)
•Are any of the lines wavy or distorted?
•Detects areas of metamorphopsia - record where those areas are
explain the recording of defects from the Amsler grid
•Record defects on the Amsler Recording sheet - draw on sheet where the defect is
is it absolute/relative scotoma
given to px to monitor themselves weekly
•Record: Eye tested / Date of test / Patient’s name