Upper GI Disorders: Treatment of Dyspepsia, Peptic Ulcer Disease and GORD pt 2
1/48
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
49 Terms
3 methods for treating dyspepsia and gastric disorders?
1 neutralisation
2 reduction of acid secretion
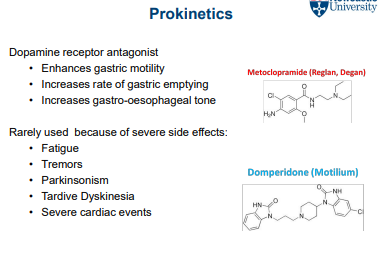
3 prokinetics
Neutralisation examples
antacids
, alginates
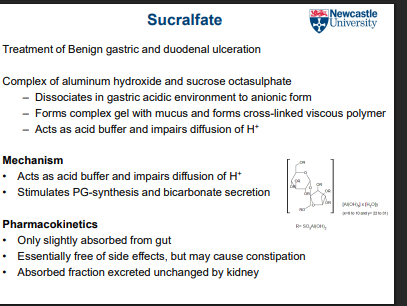
sucralfate (mucosal protectants)
Reduction of acid secretion examples
proton pump inhibitors
Histamine H2 receptor antagonists
What are antacids and how do they work?
They are weak bases (mostly inorganic) that neutralise excess stomach acid and reduce foaming to prevent heartburn.
How quickly do antacids act and how long do they last?
act quickly but provide only short-term relief.
What happens when gastric pH is raised from 1.3 to 1.6?
50% of gastric acid is neutralised.
What happens when gastric pH is raised from 1.3 to 2.3?
90% of gastric acid is neutralised.
Do antacids prevent acid overproduction?
No — they only neutralise acid after it has been produced.
Why are antacids often combined with alginates and anti-foaming agents?
To reduce surface tension of stomach acid, causing bubbles to coalesce and providing defoaming action.
2 types of antacids
-systemic antacids
- non-systemic antacids
Systemic antacids? 3
- short term therapy
- rapid onset
- prolonged use= kidney overload
Non-systemic antacids? 2
- long-term therapy
- most of dose remains in gastrointestinal tract
Examples of non-systemic antacids
rennies,
milk of magnesia,
alka seltzer
What pharmacokinetic and pharmacodynamic interactions can antacids cause?
Binding to other drugs (reducing bioavailability),
chemical inactivation of drugs,
and increased gastric pH reducing drug absorption and excretion.
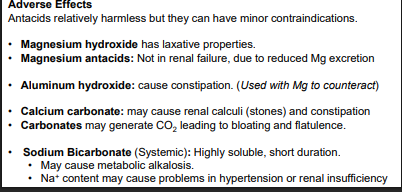
Adverse effects of antacids
-constipation
-diarrhoea
What are alginates and where are they derived from?
Polysaccharides found in the cell walls of brown algae.
What is the main action of alginates in the stomach?
Why are alginates usually combined with antacids?
They form a protective barrier on top of gastric contents.
To enhance protection by neutralising acid while forming a physical barrier.
What components are found in Gaviscon?
A combination of antacids (NaHCO₃, CaCO₃) and alginate.
How does Gaviscon work after ingestion?
It reacts with acid to form a pH ~7 alginic-acid gel “raft” that floats on stomach contents.
What is the purpose of the alginate gel raft formed by Gaviscon?
To impede gastro-oesophageal reflux.
How do proton pump inhibitors (PPIs) reduce stomach acid?
They act on parietal cells—blocking H⁺ (proton) release during HCl production—
thereby inhibiting acid formation rather than neutralising existing acid.
Example of PPIs
- lansoprazole
- omeprazole
- pantoprazole
- esomeprazole
How are proton pump inhibitors (PPIs) absorbed and delivered to their site of action?
They are absorbed from the GI tract and delivered via systemic circulation to the secretory gastric canaliculi.
Why are PPIs enteric coated?
To resist gastric metabolism and allow absorption in the GI tract.
Are PPIs active drugs or prodrugs, and how are they activated?
They are prodrugs — inactive at neutral pH and activated only in strongly acidic conditions.
How do proton pump inhibitors (PPIs) block acid secretion at the molecular level?
Their activated form irreversibly binds to cysteines on active (membrane-inserted) H⁺/K⁺ ATPase proton pumps,
preventing H⁺ movement from partiel cells into the stomach. Pumps in tubulovesicles are not inhibited.
What is the result of PPI action, and how is acid secretion restored?
Achlorhydria — all gastric acid secretion is blocked.
Normal secretion can only resume after new H⁺/K⁺ ATPase pumps are synthesised.
How is omeprazole activated and how does it inhibit acid secretion?
Omeprazole diffuses into parietal cells and accumulates.
In acidic canaliculi (pH <5), it is activated to sulfenic acid,
which irreversibly binds sulfhydryl groups on H⁺/K⁺ ATPase.
The charged molecule is trapped in the cell,can’t diffuse out of partiel cells permanently inactivating the pump
and inhibiting acid production regardless of stimulating factors.
Why is the timing of PPI dosing important?
The drug must be present in plasma at an effective concentration while proton pumps are active.
How often are PPIs usually given, and what limitation exists with this regimen?
Effective orally once daily, but not all proton pumps are inactivated, so nocturnal acid breakthrough (NAB) may occur.
When is full acid-inhibiting effect of PPIs achieved?
Only after repeated dosing.
How common are unwanted effects of PPIs, and what is a concern with long-term use?
: Unwanted effects are uncommon, but long-term treatment may raise concerns.
How does histamine stimulate acid production in the stomach?
Histamine binds to H2 receptors on parietal cells, stimulating acid secretion.
How does gastrin influence histamine levels?
Gastrin stimulates enterochromaffin-like (ECL) cells to release high levels of histamine.
Where are ECL cells and parietal cells located?
They are co-located in the stomach lining.
What role do mast cells play in gastric acid regulation?
Mast cells maintain a steady basal level of histamine throughout the mucosa and increase histamine release during infection.
Which receptor do parietal cells express to respond to histamine?
Histamine H2 receptors.
Examples of H2 receptor blockers
-- cimetidine
- ranitidine
How do Histamine H2 receptor antagonists work?
They act as competitive (reversible) antagonists of H2 receptors on the basolateral membrane of parietal cells.
What effect do H2 receptor antagonists have on gastric acid secretion?
They completely block histamine-mediated acid secretion and reduce secretion
evoked by gastrin and ACh,
effective against both basal and stimulated acid production.
How are H2 receptor antagonists typically administered?
Orally, once or twice daily.
How do Histamine H2 antagonists suppress gastric acid secretion?
By competitively and reversibly blocking parietal cell H2 receptors
How does the potency of H2 antagonists compare to proton pump inhibitors (PPIs)?
They are less potent than PPIs.
What is the incidence of side effects with H2 antagonists?
Less than 3%.
How are H2 antagonists absorbed and how long do therapeutic levels last?
: Rapidly absorbed orally,
peak serum concentration in 1–3 hours,
therapeutic levels maintained up to 12 hours.
What drug interactions are important with H2 antagonists?
• Cimetedine: inhibits hepatic P450s: modulates drug metabolism
• May inhibit absorption of drugs requiring acidic environment for absorption
• SMOKING has been shown to decrease the effectiveness of H2 blockers.
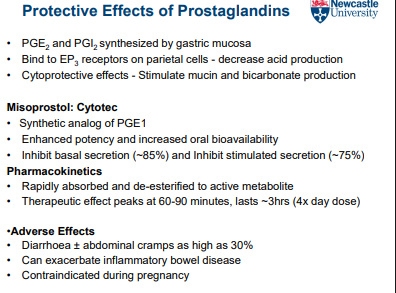
Protective Effects of Prostaglandins