Review and important info
1/78
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
79 Terms
what is Delirium
Psychosis caused by Medical issues
when a pt becomes temporaily confused, disoriented and not able to think or remeber clearly
rapid onsent, related to a seroius underlyaing condition
what are risk factors for deliruim
Older age
Preexisting MiND(Mild Neurocognitive Disorder) or MND(Major Neurocognitive Disorder)( dementia)
recent surgey
what are commen causes of deliruim
Dehydration
Electrolyte imbalances
Infection (UTIs, pneumonia, etc.)
Dementias and other neurocognitive disorders
Hospitalization, especially intensive care
Intoxication or withdrawal from alcohol or drugs
Organ failure: esp kidney or liver
Medications, such as sedatives, opioids, anesthesia, antihistamines, anticholinergics
Metabolic disorders, such as diabetic ketoacidosis (DKA)
Severe pain
Sleep deprivation
what are some s/s of delirum
Changes in alertness (usually more alert in the morning, less at night)
Changing levels of consciousness
Confusion
Disorganized thinking or talking in a way that doesn’t make sense
Disrupted sleep patterns or sleepiness
Emotional changes: anger, agitation, depression, irritability, or overexcitement
Psychosis: hallucinations and delusions
Incontinence
Memory problems, especially with short-term memory
Trouble concentrating
What are some importnat notes about treating someone with deliruim
treat the underlaying conidtion
ensure sfaty and use supportive measures like nutriction and pain managment
Use clocks and calendars within view
Invite family members to spend time in the room
Ensure clients are wearing hearing aids and glasses
Allow for undisrupted sleep when possible
Encourage clients up and out of bed when possible
Control pain (unless the pain medication is causing the psychosis)
Administer prescribed medications to distressed clients at risk to themselves or to others, such as haloperidol (note that sedation can worsen delirium symptoms)
Avoid the use of restraints if possible
what is Delirum Tremens
most severe condition caused by withdrawal from alcohol. It is a life-threatening condition that requires immediate and rigorous medical attention.
usually occur one to three days after the last drink if the individual suddenly stops drinking. The duration of DTs is typically three to seven day
willl have s/s like tremor, N/V, hallucinations, seizures
treat with benzos and supportive therapy
What is the most common cause of delirium in an older adult?
urinary tract infection (UTI)
what is dementia
The decline in cognitive ability is gradual, progressive, and irreversible beyond normal aging. The symptoms progress slowly, and the onset is described as vague and insidious.
Individuals with dementia/Major NCD lose the ability to think, take care of themselves, remember things, and control their emotions.
Dementia affects an individual’s cognition with a decline in at least one of the following domains:
◦ Executive function
◦ Complex attention
◦ Language
◦ Learning and Memory
◦ Perceptual-Motor
◦ Social cognition
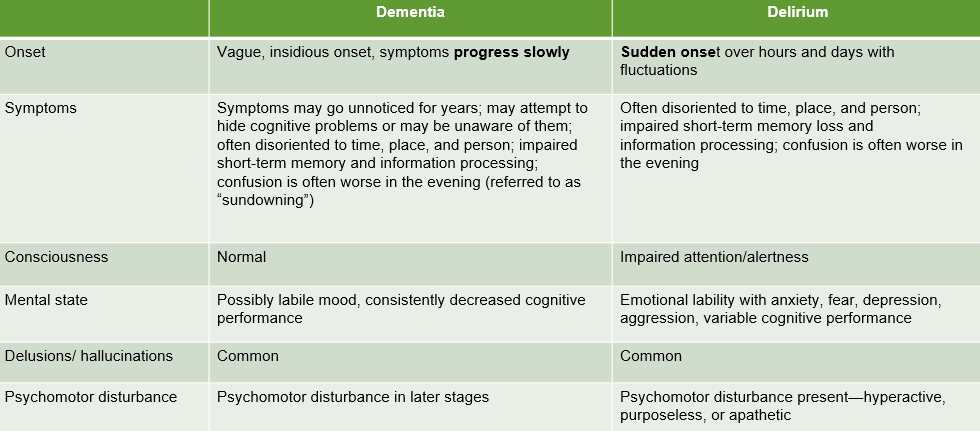
What are the main differences between delirium and dementia?
dementia is slow and delium is a fast onset from an underlaying condition
When a patient presents as combative and confused in the emergency room, should the patient be prescribed psychotropics or medically cleared first?
medical clearance must be completed first to rule out immediate life-threatening conditions before assuming a primary psychiatric disorder and initiating psychotropic medication.
What type of neurocognitive disorder (NCD) causes atrophy in the cortex of the brain?
Alzheimer disease is the most common form of dementia (Major Neurocognitive Disorder).
what is Alzheimer disease
the most common form of dementia and is categorized as a subtype of Major Neurocognitive Disorder (Major NCD).
The cognitive decline associated with Alzheimer disease is progressive and gradual.
Causes Atrophy in the cortex and involves the deposits of amyloid plaques and neurofibrillary tangles in the neurons, leading to the degeneration of neurons. The presence of amyloid plaques is found upon autopsy. PET scans may also reveal the buildup of amyloid plaques and tau proteins in clients with the disease.
Treatment Goals: slow the progression of the disease.
Medications foucsed on Slowing Disease Progression, Treating Cognitive Symptoms (Memory and Thinking), and Treating Noncognitive Symptoms (Behavioral and Psychological)
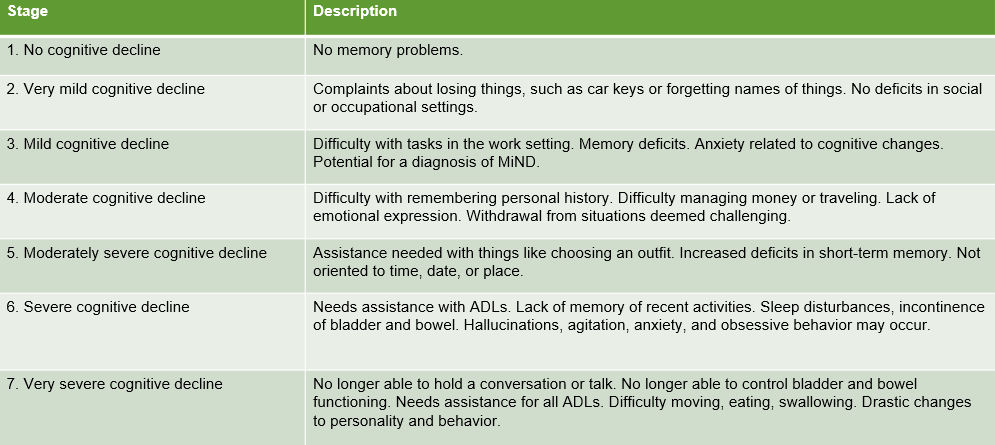
What are the stages and behavior of dementia (mild, moderate, severe cognitive impairment)?
What medication is prescribed for managing agitation associated with dementia?
Brexpiprazole (Rexulti).
Brexpiprazole (Rexulti) is classified for treating noncognitive symptoms (behavioral and psychological).
side effects: increased risk of death in older adults with dementia-related psychosis. Furthermore, Rexulti is not approved for the treatment of people with dementia-related psychosis without agitation
What interventions can enhance patients’ psychosocial functioning for modifiable risk factors related to dementia?
Encouraging the individual to remain socially active.
Encouraging the individual to pursue treatment for depression and anxiety.
Encouraging the individual to do daily activities that will work the brain—crossword puzzles, playing cards, and learning something new.
what are some medical and nutrictional interventions that may delay cognitive decline
Checking blood pressure routinely to ensure that blood pressure remains within a healthy range. This could include the purchase of an at-home electronic blood pressure cuff for an individual who already has some cardiovascular concerns.
Checking that cholesterol and blood glucose levels are within normal ranges—hypercholesterolemia and diabetes are known to increase the risk for dementia.
Teaching individuals about the importance of eating a nutritious diet to maintain a healthy weight/BMI.
What is Huntington’s Disease
a genetic mutation that causes a neurocognitive disorder.
Major Neurocognitive Disorder (Major NCD). It is also identified as an irreversible cause of neurocognitive disorders.
Huntington disease is characterized as a genetic mutation that results in the building blocks of protein repeating more times than they should normally do. The disease attacks the neurons in the brain, causing them to die.
Associated with symptoms such as difficulty with speaking, swallowing, eating, and chorea (involuntary, jerky movements that can make a person appear clumsy or fall easily).
Can cause Depressive disorder due to another medical condition. Furthermore, it is included among the other factors that raise the risk of developing schizophrenia
What is Lewy Body dementia
a subtype of Major Neurocognitive Disorder (Major NCD).
LBD involves the insoluble deposits of alpha-synuclein protein that damage the brain. These protein deposits are known as Lewy bodies.
Lewy Body dementia and Parkinson disease both involve these Lewy bodies. Because LBD shares many symptoms with Parkinson disease, it can often be difficult to diagnose LBD from Parkinson disease.
The disease gained public attention when comedian Robin Williams developed a Major NCD called Lewy body dementia, which ultimately led him to take his own life.
What is Vascular dementia
a neurocognitive disorder that stems from injuries to the brain caused by ischemia.
This injury occurs due to conditions, such as a stroke, that block blood flow to the brain and subsequently lead to permanent neuron death.
What medications is used to treat mild to severe dementia?(7)
Aducanumab(aduhelm)
Lecanemab( leqembi)
Donepezil(aricept)
galantamine(Razadyne)
Rivastigmine(exelon)
Memantine(Namenda)
Memantine + Donepezil(namzaric)
What are common examples of first-generation antipsychotics?
Chlorpromazine (Thorazine)
Fluphenazine
Haloperidol (Haldol)
Thioridazine
Trifluoperazine
How should depot antipsychotics be administered, and what are the nursing responsibilities involved in this process?
Depot antipsychotics are injectable forms of certain medications, including first-generation antipsychotics and second-generation antipsychotics
Route: Depot antipsychotics are administered via the intramuscular (IM) injection route, which makes them long-acting.
These depot forms are used for clients who struggle with nonadherence to medication. They are typically administered every two to six months.
Nursing Responsibilities in the Process
Supporting Treatment Adherence and Monitoring:Nurses have a vital role in advocating for treatment adherence and wathing for any side effects
Providing Education and Support:
Nurses must provide client and family education.
Education should cover:
The client's illness.
Side effects and adverse events of medications.
Relapse prevention.
Ensuring Safety and Collaboration:
What are the various types of delusions(5)
Persecutory (or Paranoid)
Grandiose
Somatic
Erotomaniac
Jealous
what are Persecutory (or Paranoid) delusions
The central theme is that people are out to get the individual. The person believes they are being watched, harassed, or obstructed.
Patients may present as irritable, aggressive, guarded, suspicious, or isolating. They may also socially isolate and live just for the wrongs done to them. In extreme cases, they may involve the legal system to get justice for the wrongs they believe have been done
what are Grandiose delusions
The individual believes they have done something great or are someone extraordinary. They believe they have great wealth, power, or influence.
Patients with delusional disorder (grandiose type) are rare and may have a comorbidity of psychosis or mood process. (Behavioral details are limited in the sources).
what are Somatic delusions
The delusions involve health, bodily functions, or undiagnosed disease. Onset is either acute or gradual. They typically seek mental healthcare for the supposed physical issue.
Patients with somatic delusions may experience unremitting symptoms and may be referred to as a consultant by medical or dental clinics. This type of delusion is a common comorbidity with depression, anxiety, substance abuse, and personality disorders. Patients may bring samples of their hair or skin for extensive testing for infestation. The sources also mention a specific patient behavior: formication, which is a hallucination that bugs are crawling on the skin
what are Erotomaniac delusions
The individual has thoughts of an idealized love between themselves and another individual, usually a celebrity or someone they have never met. They believe the celebrity harbors true feelings for them.
Behaviors include stalking or assaultive actions. Stalking behaviors commonly lead to arrests, probations, home relocations by the celebrities, and restraining orders. Individuals with this delusion are described as vulnerable, isolated, sexually repressed, and exhibiting poor social skills
what are Jealous delusions
The individual believes their partner or spouse is cheating on them or will cheat despite evidence to the contrary.
Jealous delusions can give rise to homicidal or suicidal acting out
what are Referential delusions
Beliefs that ordinary events carry a hidden message meant specifically for them
what are Nihilistic delusions
Beliefs related to the nonexistence of the self, life, the world, or the concept of meaning, or that something catastrophic will happen
what are Non-Bizarre vs. Bizarre Delusions
Bizarre delusions involve fixed false beliefs that are not possible in this world, such as believing an alien has implanted a chip in the person's head.
Non-bizarre delusions involve fixed false beliefs containing content that is plausible but inconsistent with evidence, such as believing one is under constant police surveillance. Delusional disorder is characterized by having one or more non-bizarre delusions lasting for at least one mont
what are Hallucinations
an alteration of perception of sensory experiences without actual external stimuli.
They are classified as positive symptoms of schizophrenia spectrum disorders.
Hallucinations can be categorized by the five senses. The individual experiencing the hallucination may or may not react or respond to what they perceive
What are the different types of hallucinations(5)
Auditory Hallucinations
Visual Hallucinations
Tactile Hallucinations
Gustatory Hallucinations
Olfactory Hallucinations
what are Auditory Hallucinations
An altered perception of hearing in the absence of external stimuli. These can include single or multiple noises, music, or murmuring.
Patients may report hearing voices in their head. A subset, command auditory hallucinations, directs the individual to do things, including commit violence toward self or others
what are Visual Hallucinations
A false sensory experience that is seen.
Patients may describe seeing people, things, or flashes of light
what are Tactile Hallucinations
False sensory perceptions involving the sense of touch.
A specific type is formication, which is the hallucination that bugs are crawling on the skin. Patients may peel, pick, or scratch their skin
what are Gustatory Hallucinations
False perception involving taste.
Patients typically report strange or unpleasant tastes
what are Olfactory Hallucinations
False sensory experience involving the sense of smell. This is also referred to as phantosmia.
Patients typically report strange or unpleasant odors
What is neuroleptic malignant syndrome (NMS), and what are its symptoms?
a severe, life-threatening reaction that is a common side effect associated with the use of antipsychotic medications.
NMS usually occurs two weeks after the initiation of antipsychotic treatment or following a change in dosage.
The block of dopamine in the nigrostriatal pathway caused by antipsychotics can lead to movement disorders and critical side effects like neuroleptic malignant disturbance.
NMS is characterized by a distinct cluster of severe symptoms:
High Fever: A high fever, typically ranging from 102 to 104 degrees Fahrenheit.
Muscle Rigidity: Muscle rigidity.
Autonomic Instability/Vital Sign Changes: Irregular pulse, tachycardia, tachypnea, confusion, and hypertension.
Altered Consciousness: Confusion.
Other Physical Symptoms: Diaphoresis (sweating)
What nursing responsibilities should be considered when caring for a patient with NMS?
Immediate Action and Treatment Cessation:
The primary treatment involves the removal of the offending agent (the antipsychotic medication).
Treatment necessitates immediate and rigorous medical attention.
Cardiovascular Monitoring and Supportive Care:
Maintain cardiovascular status through monitoring. NMS symptoms include irregular pulse, tachycardia, tachypnea, confusion, and hypertension.
Provide supportive care.
Maintain IV fluids
Ensure mechanical respiration if needed.
Managing Critical Symptoms (Fever and Rigidity):
NMS is characterized by a high fever (102 to 104 degrees Fahrenheit) and muscle rigidity.
Manage hyperthermia by using cooling blankets.
Administer dantrolene for muscle rigidity.
Administer benzodiazepines for agitation.
For moderate to severe symptoms, bromocriptine/amantadine may be used.
Laboratory and Physical Monitoring:
Monitor for elevated CK (creatine kinase) levels.
The condition also presents with diaphoresis (sweating).
NMS is a critical potential side effect associated with the block of dopamine caused by antipsychotic medications
What medication will the doctor prescribe for a patient with schizoaffective disorder who is transitioning to a second-generation antipsychotic?
When a patient with schizoaffective disorder is transitioning to a second-generation (atypical) antipsychotic, the doctor will typically prescribe a medication that targets both psychotic and mood symptoms, since schizoaffective disorder includes features of schizophrenia and mood disturbances (either depression or mania).
Common Second-Generation Antipsychotics Used:
Risperidone (Risperdal) – Often chosen for its effectiveness on both positive (hallucinations, delusions) and negative (flat affect, social withdrawal) symptoms.
Paliperidone (Invega) – FDA-approved specifically for schizoaffective disorder and available in both oral and long-acting injectable forms.
Olanzapine (Zyprexa) – Effective for mood stabilization and psychosis but requires monitoring for metabolic side effects.
Quetiapine (Seroquel) – Useful for patients with significant depressive features or sleep disturbances.
Aripiprazole (Abilify) – Has partial dopamine agonist activity, often chosen for patients needing fewer metabolic side effects and more mood stabilization.
Lurasidone (Latuda) – Also effective for mood symptoms, especially depressive episodes.
What is a significant side effect associated with clozapine (Clozaril), and what nursing responsibilities should be taken into account?
Agranulocytosis is a severe and potentially life-threatening decrease in white blood cells (WBC) and absolute neutrophil count (ANC). It is listed as a specific risk associated with Clozapine (Clozaril).
Nursing Responsibilities and Interventions
Because agranulocytosis poses a critical health risk, nursing interventions are mandatory and strict:
Monitoring Blood Counts: The nurse must assess and document white blood cell count and absolute neutrophil count both at the initiation of treatment and during treatment.
REMS Protocol Adherence: This monitoring must be performed according to the REMS protocol with Clozaril clients.
Communication: Nurses are responsible for communicating findings with the provider.
Other Side Effects and Monitoring (General Antipsychotic Responsibilities)
As Clozapine is an SGA, nurses must also monitor for a range of other side effects common to this class, which require specific nursing interventions:
Side Effect | Nursing Responsibilities/Interventions |
Metabolic Side Effects (Metabolic Syndrome) | Assess weight and BMI before and during regular intervals. Assess fasting glucose and lipids with provider orders. Educate the client on a healthy diet and exercise. |
Gastrointestinal Issues (e.g., Constipation) | Encourage hydration, a high fiber diet, and increase in physical activity if not contraindicated. |
ECG Changes | Assess and document ECG findings before initiation and during treatment. Educate the client about notifying the care team regarding symptoms like palpitations, dizziness, weakness, or shortness of breath. |
Extrapyramidal Side Effects (EPS) (e.g., Dystonia, Akathisia, Pseudoparkinsonism) | Although Clozapine carries a lowered incidence of EPS compared to first-generation antipsychotics, monitoring is required. Nurses must assess and document the onset and location of symptoms and administer medications if ordered to mitigate EPS. |
Sedation | Assess and document sedation and the risk for falls. Implement fall-risk protocols. Educate the client not to operate heavy machinery while taking sedating medications. |
What is schizophrenia
severe mental illness and distrubance involving a collection of cognitive, affective and behavioral symptoms
what is loose assciation
When a client switches from one unrelated topic to another
“I like hotdogs. Come take a look at my houseboat.
what is Circumstantial thinking
When a person delays getting to the point of a conversation, providing random, tedious, and unnecessary details
When asked about their day, the client provides all the tiny details of everything they did that day.
What is Tangentiality
Occurs when a person answers a question with indirectly related or unrelated information but never gets to the point of the topic
“I have a date tonight. Do you like dates? I think that all fruit is necessary for good fiber intake. I need to use the restroom.”
what is concrete thinking
A literal interpretation of ideas or environmental stimuli with a lack of abstract thinking, such as being unable to understand metaphors or analogies
A client who is asked to shower takes their clothes off immediately regardless of where they are.
what is Neologism
Making up new words that have no meaning to others but make sense to the individual
“I have moxyplams for my tadonxses.”
what is word salad
The random connection of words without logic
Cab Abu use eat too oh hi.
what is Clang associations
Connecting words according to sound
Cat bat mat sap lap.
what is Mutism
The inability to speak
The client does not respond when asked a question.
what is perseverating
When someone repeatedly uses the exact words, phrases, and ideas when communicating
A client references the same person over and over again during a session.
what is Echolaila
The repetition of words that one hears from another person
A client is asked to sit down for dinner and responds, “Dinner, dinner, dinner, I want to go to dinner, dinner, dinner.”
What is echopraxia
The imitation of the movement of others
The client mimics the movement of the nurse with whatever they do with their body position or limbs.
what is catatonia
An abnormality of movement and behaviors
The client is found lying stiff in bed.
what is Negativism
Resistance to movement and instructions
The client does not move or respond when another client asks them to.
what is stupor
A complete lack of response
The client is conscious but not interacting at all.
what is Catatonic excitement( Pyschomotor agitiation)
Excessive and stereotypic movements
The client is pacing, rocking, and grimacing.
what is Waxy Flexibility
When a client allows their limbs to be placed in any position for long periods
The nurse puts the client’s hand up in a stop position, and the client does not move it at all.
How can we differentiate between positive and negative symptoms of schizophrenia?
based on whether the symptoms represent an addition of abnormal experiences or behaviors (positive) or a subtraction or "taking away" of normal functions or expressions (negative).
1. Positive Symptoms of Schizophrenia
Positive symptoms are active symptoms that include changes to behaviors or thought content, consisting of distorted thoughts and perceptions. They are described as being "added" to the person.
Category | Specific Positive Symptoms |
Distorted Thoughts (Delusions) | Persecutory, Referential, Grandiose, Somatic, Religious, Erotomaniac, Nihilistic, Disordered thought. |
Altered Perceptions (Hallucinations) | Auditory (hearing voices), Visual, Tactile (formication), Gustatory, Olfactory. |
Disorganized Thinking/Speech | Loose associations, Circumstantial thinking, Tangentiality, Concrete thinking, Disordered Speech, Echolalia, Echopraxia. |
Disordered Behavior | Aggression, Stereotypy, Catatonic excitement. |
2. Negative Symptoms of Schizophrenia
Negative symptoms are described as a "take away" from a person's personality, involving the subtraction or lessening of normal functions. This includes diminished or inappropriate affect and anhedonia.
Category | Specific Negative Symptoms |
Affective and Emotional | Affective flattening, Decreased eye contact, Inappropriate affect, Lack of emotional expression. |
Behavioral Deficits | Avolition (decrease or absence of motivation), Anergia (inability to feel pleasure or lack of energy), Apathy, Disordered movement, Negativism, Decreased response to social interaction. |
Speech Deficits (Alogia) | Poverty of speech (or poverty of content), Mutism, Alogia. |
what are the postivtive symptoms of schiophrenia
Delusions
Hallucinations
Disordered thought
Loose associations
Circumstantial thinking
Tangentiality
Concrete thinking
Disordered Speech
Echolalia
Echopraxia
Disordered behavior
Aggression
Stereotypy
Catatonic excitement
what are negative symptoms of schizophernia
Affective
Affective flattening
Decreased eye contact
Inappropriate affect
Disordered movement
Negativism
Avolition
Anergia
Disordered speech
Poverty of speech
Mutism
Alogia
Disordered behavior
Apathy
Decreased response to social interaction
what are cognitive symptoms of schizophrenia
Slow thinking
Difficulty understanding
Poor concentrating
Difficulty with memory
Disorganized thoughts
Difficulty with vigilance
Difficulty with reason
Difficulty with problem-solving
What is Bipolar disorder
fluctuating periods of intense mood states. It is characterized by the presence of both depression and mania, or hypomania.
The disturbances in mood are intense, persistent, and interfere significantly with daily life, having severe repercussions on physical health, interpersonal and Treatment
fluctuate between mania and depression
Describe the symptoms associated with bipolar disorder
1. Manic/Hypomanic Episodes (Elevated Symptoms)
Mania is a condition in which a person’s mood is abnormally elevated and is accompanied by high energy or activity.
Hypomania is a milder form of mania that typically does not cause significant impairment in social or occupational functioning.
Symptoms characterizing a manic episode include:
• Elevated mood.
• Increased energy/activity.
• Decreased need for sleep.
• Pressured speech (rapid speech).
• Talkativeness.
• Flight of ideas.
• Distractibility.
• Increased goal-directed activity.
• Increase in risky behaviors.
• A person's mood is abnormally elevated and accompanied by high energy or activity.
• Mania symptoms involve a high degree of happiness or euphoria called elation.
2. Depressive Episodes (Low Symptoms)
The depressive phase of bipolar disorder includes symptoms similar to Major Depressive Disorder (MDD).
Symptoms characterizing a depressive episode include:
• Depressed mood (feelings of sadness).
• Loss of interest/Anhedonia (lack of pleasure in activities once enjoyable).
• Decreased energy/motivation.
• Guilt.
• Decreased or increased appetite.
• Insomnia or hypersomnia.
• Suicidal thoughts/ideation..
Should the nurse be cautious in how they inquire about suicidality to avoid pushing clients toward making a plan? Why or why not?
No , b/c the nurse's responsibility is to delve deeper into the individual’s suicidal ideation, including the existence of a plan, a means, and a timeline, as these factors significantly correlate with imminent risk.
By asking directly, nurses can gather the information needed to:
Gauge the immediacy and severity of the risk.
Determine the appropriate level of intervention or treatment required, which may include hospitalization or close monitoring.
Develop a comprehensive safety plan (which involves risk assessment, close monitoring, and environmental modifications such as removing sharp objects)
Are men or women at a higher risk of attempting suicide? What are the reasons for this?
Risk of Attempting Suicide: Women are at a higher risk of attempting suicide.
Depression is more prevalent in women (1 in 3 lifetime risk) compared to men (1 in 5 lifetime risk).
more likely to use methods that are less immediately lethal (like ingestion of toxic substances or overdose of medications as a method of suicide, while men commonly use hanging, drug overdose, or firearms)
Risk of Death by Suicide (Completion): Men die by suicide four times as often as females. Men generally use methods like firearms, hanging, and drug overdose
Outline the necessary interventions in suicide precautions
Lethality Assessment: Perform a structured risk evaluation to gauge the immediacy and severity of the risk.
Direct Inquiry: The nurse must never be reluctant to ask if the client is contemplating suicide or if they have a plan. If a plan exists, inquire about the method, time, and means to implement protective precautions.
Safety Environment: Implement a comprehensive safety plan. This includes removing items that could be used for self-harm (e.g., sharp objects).
Monitoring: Implement close monitoring (which may include continuous 1:1 observation). Monitor client responses for warning signs of self-harm or increasing emotional distress.
Medication Safety: Ensure prescribed medications are carefully selected (with a lower risk of lethality in case of overdose).
Communication: Establish a therapeutic relationship. Do not argue with the client about suicidal ideation. Instead, distract or redirect the client to reality-based activities
What is the nursing priority for a patient who has been newly prescribed an antidepressant and is showing rapid improvement in mood?
Priority Action: The immediate nursing priority is vigilant monitoring for an increased risk of suicide and self-harm.
Reason for Risk (The Critical Period): The client may experience an increase in energy and activity from the antidepressant before their suicidal ideation decreases. This shift provides the motivation to act on existing suicidal thoughts or plans.
Key Safety Interventions (The Nurse Must Do)
Assessment: Conduct a lethality assessment. You must never be reluctant to ask if the client is contemplating suicide or if they have a plan
Plan Inquiry: If a plan exists, inquire directly about the method, time, and means (weapons/drugs) to determine the severity of risk and implement protective precautions.
Monitoring and Environment: Initiate or maintain close monitoring. Implement a comprehensive safety plan and remove items that could be used for self-harm (e.g., sharp objects).
Medication Check: Ensure the client is not hoarding or storing up medications for the purpose of self-harm.
What ECT
a medical procedure that involves the passage of a controlled electric current through the brain, intentionally inducing a brief seizure.
This procedure is performed while the client is anesthetized. The controlled electric current causes a rapid increase in neurotransmitters, thereby alleviating depressive symptoms
what are the indciations for ECT
ECT is typically reserved for cases where other forms of treatment have been unsuccessful or immediate, powerful intervention is required:
Treatment-Resistant Depression: ECT is used for clients who do not respond adequately to traditional treatments such as pharmacotherapy and psychotherapy.
Bipolar Disorder: It can be an essential part of treatment in some cases of bipolar disorder.
Severe Depression: ECT may be considered for clients exhibiting acute suicidal ideation or behavior due to its rapid onset of action. Unlike pharmacological therapy, ECT often produces a significant reduction in depressive symptoms and suicidality within a week or two after a single session.
Catatonia: ECT is listed as an evidence-based treatment for catatonia (which can occur in the context of schizophrenia spectrum disorder, depression, or bipolar disorder)
what are the contraindications for ECT
People takeing:
Antipsychotics (Dopaminergic-blocking medications): Antipsychotics are contraindicated in patients with malignant catatonia. Since ECT is a first-line treatment for catatonia, any existing antipsychotic medication should be managed appropriately.
Dopaminergic-blocking medications should be avoided in malignant catatonia
What are the nursing responsibilities associated with ECT
1. Safety and Pre-Procedure:
Since ECT may be used for clients with acute suicidal risk, the nurse's general responsibilities include implementing the comprehensive safety plan, which involves risk assessment, close monitoring, and environmental modifications.
2. Monitoring During Treatment (Especially for Catatonia):
If ECT is used to treat catatonia (especially malignant catatonia), the nurse's responsibilities include monitoring vital signs, fluid intake and output, cardiopulmonary status, and nutrition.
The nurse must monitor patients with malignant catatonia for severe physical symptoms such as hyperthermia, hypertension, and lethal arrhythmias.
3. Physical Care (Immobility Management):
For patients with limited movement (common in catatonia, which is treated with ECT), nurses should monitor for skin integrity to decrease the incidence of pressure ulcers.
4. Careful Assessment:
Prior to and during treatments like ECT, nurses are generally responsible for careful assessment and quality assurance of care provided by health-care professionals.
5. Treatment Effectiveness Monitoring:
Unlike antidepressant medication, the depressive symptoms and suicidality resulting from ECT can produce a significant reduction within a week or two after a single session, making continuous assessment of efficacy critical.
What is Persistent Depressive disorder(PDD)
formerly known as dysthymia, is a type of depressive disorder characterized by its chronic nature and milder symptom severity compared to Major Depressive Disorder (MDD).
It is characterized by a steady, low-grade depressive mood. The symptoms are generally described as less severe than MDD.
The low-grade depressive mood must be long-lasting, for at least two years.
While symptoms are chronic, there may be periods of improvement involved, but these periods must last no longer than two months.
Although the symptoms are not as intense as MDD, PDD can still pose a significant challenge in daily functioning and well-being.
Treatment: Antidepressants, specifically SSRIs and Serotonin and SNRIs, are found to frequently treat PDD
What is Premenstrual Dysphoric Disorder (PMDD)
PMDD is categorized as a type of depression or mood disturbance.
It occurs specifically during the week before the onset of menstruation.
marked by prominent mood changes, including mood swings, irritability, and anxiety.
Symptoms typically subside around the onset of menstruation
What is Major Depressive Disorder (MDD)
MDD is one of the most common mood disorders recognized by the DSM-5. It is often referred to clinically simply as "depression".
MDD involves disturbances in a person's emotional state that are intense, long-lasting, and persistent, interfering significantly with daily life and having severe repercussions on physical health, interpersonal relationships, and overall quality of life.
For a diagnosis of MDD, a client must experience at least five or more specific symptoms (including depressed mood and/or loss of interest or pleasure). These symptoms must be present most of the day, nearly every day, for at least two weeks.
The symptoms must also cause significant distress or impairment in social, occupational, or other important areas of functioning
Explain the differences between Persistent Depressive Disorder (PDD), Premenstrual Dysphoric Disorder (PMDD), and Major Depressive Disorder (MDD).
Disorder | Key Difference (Duration/Timing) | Severity/Nature |
Major Depressive Disorder (MDD) | Characterized by distinct episodes lasting at least two weeks. | Symptoms are intense and cause significant distress or impairment. |
Persistent Depressive Disorder (PDD) (formerly Dysthymia) | Chronic depression characterized by long-lasting symptoms for at least two years. Periods of improvement must last no longer than two months. | Symptoms are less severe than MDD (a steady, low-grade depressive mood). |
Premenstrual Dysphoric Disorder (PMDD) | Cyclical timing: occurs specifically during the week before the onset of menstruation. | Marked by severe mood disturbances, including mood swings, irritability, and anxiety. Symptoms subside around the onset of menstruation |
What is the most commonly prescribed medication for MDD?
SSRIs and SNRIs are the types of antidepressants found to be effective and have tolerable side effects.
• Pharmacotherapy, primarily using antidepressant medications, is considered an essential component in managing mood disorders like MDD
Is hopelessness a critical factor in assessing suicidal risk? Why?
Yes, hopelessness is a critical factor in assessing suicidal risk.
Hopelessness is considered a factor that heightens the risk of suicide among individuals with mental health problems. It is critical because of its profound psychological effect on the individual:
View of Suicide as Escape: Feelings of hopelessness, along with worthlessness and a persistent sense of overwhelmed despair that often accompany depression, can lead individuals to perceive suicide as the only viable option to escape their pain.
Symptom of Underlying Disorder: Hopelessness is a recognized symptom of Major Depressive Disorder (MDD). In adults, feelings of guilt or hopelessness are described as classic symptoms of depression.
Lethality Assessment Component: While the structured evaluation of risk (lethality assessment) focuses heavily on immediate danger signals like the presence of a detailed plan and the availability of means (weapons/drugs), hopelessness contributes significantly to the overall risk profile that necessitates these protective precautions