Bio 269 Exam 3 -Casotti WCU
1/151
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
152 Terms
Respiration Components
4 Steps from air to cellular level
-breathing air into alveoli, O2 from lungs to vasculature while CO2 from vasculature to lungs
-respiratory diffusion/ External Respiration (across respiratory membrane) by pulmonary capillaries
-bulk transport (movement of gas along pressure gradient) by systemic capillaries
-cellular diffusion/ internal respiration
Dalton's Law
-atmosphere follows this law
-The total pressure of a mixture of gases is the sum of the individual pressures (Ptotal=P1+P2+P3...)
-total = 760 mmHg at sea level, less on top of a mountain
Henry's Law
-gases dissolve in liquid in proportion to their partial pressure
-equilibrium will be reached
-as O2 dissolved in blood, gas changes state of matter
-doesnt take into account solubility
2 Factors affecting gas ability to cross alveolar membrane
-temperature: lower temperature, faster diffusion (not in humans bc maintain constant body temperature)
-Solubility: ability to dissolve in liquid
Order of solubility of gases (highest to lowest)
CO2 > O2 > N2
Does Nitrogen cross membrane?
No because not very soluble
Would we survive with more CO2 in air than O2?
No bc CO2 easily diffused so not enough O2 and we would die
Alveolar Gases
-O2, CO2, N2, H2O (vapor)
-in alveoli at any time, contains more CO2 and H2O than O2
How is there more H2O in our lungs than atmosphere?
We breathe in dry air, when pass by moist surface, picks up H2O particles to prevent drying out alveoli
Where does oxygen diffuse from and to?
alveoli to pulmonary capillaries
Where does carbon dioxide diffuse from and to?
pulmonary capillaries to alveoli
Why is gas different in alveoli than in the air?
-O2 diffuses into blood, Co2 diffuses in opposite direction
-humid air within the lungs
-air in alveoli is a mixture of new and old air (bc not all air is expelled each breath)
How do you maximize new air and minimize old air in alveoli?
By taking a deep breath
4 Circuits in the body
-systemic
-coronary
-pulmonary
**NEW: bronchial circuit**
2 ways humans can alter gas composition in lungs
-increase rate of breathing
-increase depth of breathing
Where is bronchial artery located?
-branches off aorta
-brings oxygenated blood to the tissues of the lungs
Where is the bronchial vein located?
-how deoxygenated blood leaves the tissues of the lungs
-joins the pulmonary vein to return to the heart
Where is blood partly oxygenated? Fully oxygenated?
-partially: most of pulmonary vein, aorta, bronchial artery
-fully: in pulmonary vein directly after the lungs until bronchial vein joins
Partial pressure of O2 and CO2 in atmosphere
pO2: 159mmHg
pCO2: 0.3 mmHg
Partial pressure of O2 and CO2 in alveoli (external respiration)
pO2: 105 mmHg
pCO2: 40mmHg
Partial pressure of O2 and CO2 in left atrium (after alveoli)
pO2: 100mmHg (bc brochial vein joins and deoxygenates some blood)
pCO2: 40 mmHg
Partial pressure of O2 and CO2 in systemic capillaries (internal respiration)
pO2: 40 mmHg
pCO2: 45 mmHg
Partial pressure of O2 and CO2 in right atrium (after systemic capillaries)
pO2: 40 mmHg
pCO2: 45 mmHg
Pressure Gradient: Oxygen
pO2 in deoxygenated blood is 40 mmHg
pO2 in alveoli is 104 mmHg
Pressure Gradient: Carbon Dioxide
pCO2 in deoxygenated blood is 45 mmHg
pCO2 in alveoli is 40 mmHg
How is the same amount of O2 and CO2 exchanged in the alveoli?
Although partial pressure difference are very large, CO2 is 20x more soluble than O2
difference of: pO2 > pCO2
solubility: O2 < CO2
*Cancel each other out*
Importance of Surface Area
-allows for fast diffusion of CO2 and O2 (increased contact of alveoli and pulmonary capillaries)
-human lung: 70m^2
Factors decreasing surface area
-emphysema: membranes of alveoli deteriorate, decreasing surface are
-can result from tumors, increased mucus, smoking for many years
-only 75% surface area remaining, volume stays same
Ventilation
bringing fresh air into the lungs
Perfusion
bringing blood to an organ (aka lungs)
EX: IV w saline is body perfused w fluid
Difference between size of alveoli
Large: high pO2, low pCO2
Small: low pO2, high pCO2
Ventilation-perfusion coupling
-Coupling of the amount of air with the amount of blood supply
-Couple Ventilation (air in alveoli) with perfusion (blood vessels)
-Vasodilate around large alveoli, vasoconstrict around small alveoli
Where does blood bring more dexoygenated blood to: small or large alveoli?
Larger alveoli to oxygenate the deoxygenated blood
How can you bring more deoxygenated blood to larger alveoli?
vasodilate the pulmonary capillaries that go to large alveoli to maximize amount of O2 blood that comes out and vasoconstrict pulmonary capillaries going to the smaller alveoli
What happens to vessels with alveoli that are low ventilated and well perfused
vasoconstriction
What happens to blood vessels with alveoli that are high ventilated but poor perfused
vasodilation
2 Ways O2 is transported in the blood
1. dissolved in plasma (about 15-18 ml/liter of plasma in body)
2. Bound to respiratory pigment, hemoglobin (about 200 ml/liter of plasma)
Structure of hemoglobin
-2 alpha and 2 beta polypeptide chains
-oxyhemoglobin: ratio of O2 to hemoglobin is 4:1
-deoxyhemoglobin: ratio of O2 to hemoglobin is less than 4:1
Percent Saturation
Expresses average saturation of hemoglobin with oxygen
Percent O2 saturation of deoxyhemoglobin leaving capillaries
75%
-ratio of oxygen to hemoglobin is 3:1
Percent O2 saturation of oxyhemoglobin leaving lungs
100%
-ratio of oxygen to hemoglobin is 4:1
O2 affinity for Hb
O2 has a high affinity for Hb, meaning O2 wants to bind to Hb
Factors decreasing O2 affinity for Hb
-increased body temp
-increased pCO2
-decrease in pH (Bohr effect)
-binding to 2, 3 diphosphoglycerate
What causes an increase in 2, 3 diphosphoglycerate
When exercising, RBC energy rate needs to increase, but not enough O2, so use anaerobic respiration, 2, 3 diphosphoglycerate making harder for O2 to attach to hemoglobin
Causes of hypoxia
-anemic: few RBCS less than 45% hematocrit
-Ischemic: impaired or blocked blood circulation
-Histotoxic: body cells unable to use O2 even though enough is being delivered (EX injesting cyanide inhibiting ETC in mitochondria)
-Hypoxemic: reduced arterial pO2 (CO2 poisoning)
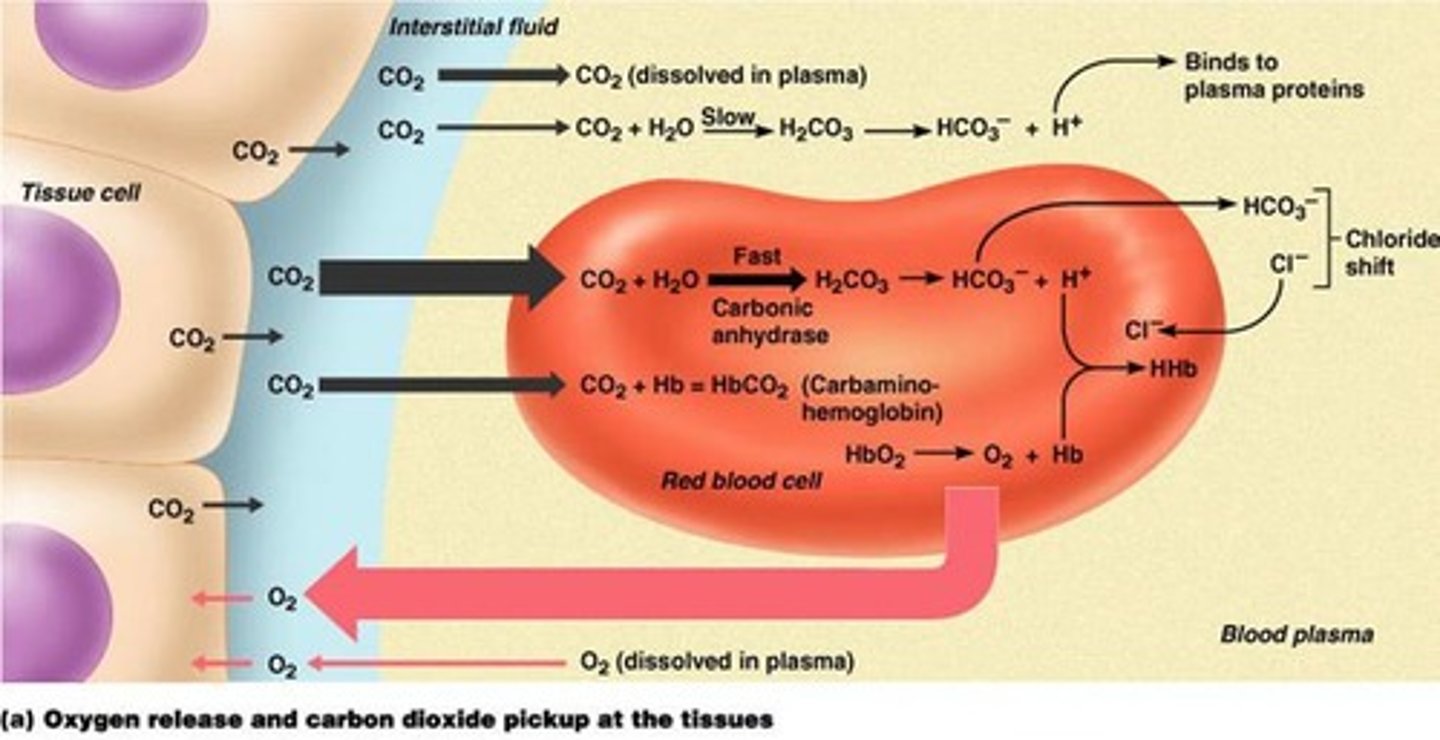
3 ways to transport CO2 in blood
-Dissolved in plasma (7 - 10%)
-Bound to Hb in RBC(20 - 30%)
-converted to Bicarbonate ion in both plasma and RBC(60 - 70%)
CO2 transport from tissue (most to least)
1. FAST, in RBC: CO2 + H2O --carbonic anhydrase--> H2CO3 ---> HCO3- + H+ + Cl-
2. CO2 + Hb ---> HbCO2
3. CO2 dissolved in plasma
4. SLOW, in plasma: CO2 + H2O ---> H2CO3 ---> HCO3 - + H+
Chemical formula for bicarbonate
HCO3-
Chemical formula for carbonic acid
H2CO3
What is the reason for pH decrease in capillaries
carbonic acid production increases
remains in this form until reaches lungs
Formula for carbamino hemoglobin
HbCO2
-meaning at least one molecule fo CO2 attached to hemoglobin
-at the same time, O2 comes off of hemoglobin and goes to tissues and cells of human body
What happens to pH with more CO2 dissolved in blood
decreases (more acidic)
Where does the bicarbonate ion (HCO3-) go once produced inside the RBC? Why?
dissolved into plasma by transport proteins and Cl- dissolves into RBC to stay electrically neutral (CL- isn't an acid or a base so doesn't change pH0
Where does the H+ molecule go once produced in the RBC? Why?
-binds to hemoglobin to make HHb, Hb acts as a buffer
-RBC needs to get rid of H+ so pH can remain stable
Respiration overview
-oxygen utilization varies w activity: @ rest 200ml/min, exercise 6000 ml/min
-importance: breathing increases (rate and depth) due to metabolic demands, regulated by pH of extracellular matrix
What regulates depth and rate of breathing
CO2
Lung Anatomy: Conducting Zone
-trachea
-primary, secondary, tertiary bronchi
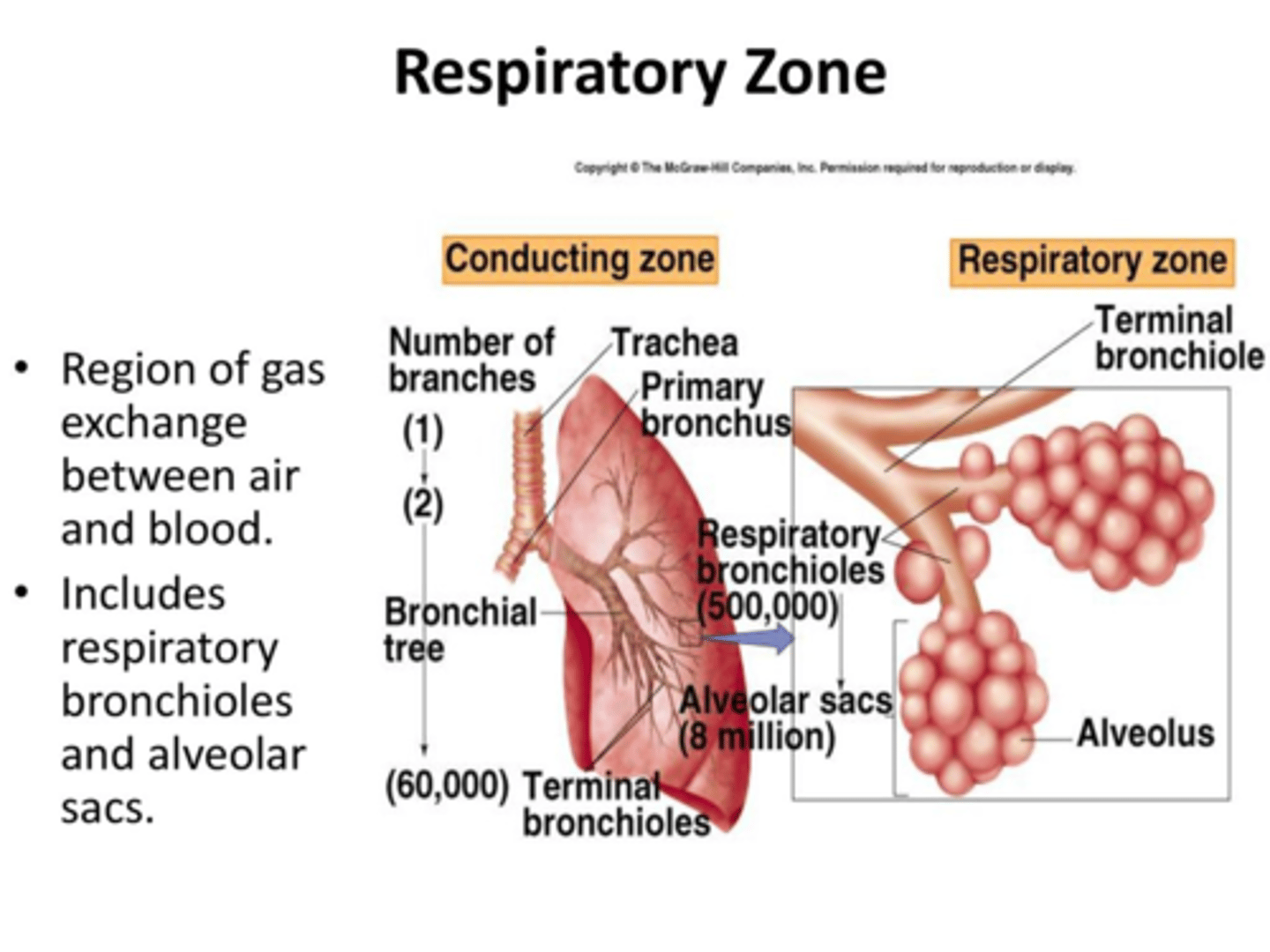
Lung Anatomy: Respiratory Zone
-bronchioles
-alveolar ducts
-alveoli
Function of the conducting zone
-Warm, cleanse and humidify air
-Phonation (vocal cords attached to trachea, secondary function)
-Regulation of air flow (dilation/constriction)
Function of the respiratory zone
gas exchange
2 cell types in respiratory zone
-cell type I: squamous allows for fast diffusion, made of H2O, if they get too close together, they will want to bond and collapse the alveoli
-cell type II: larger, secretes biological detergent called surfactant to break bonds between Type I cells and resist collapsing
Membranes that gases must penetrate
-apical epithelium (alveoli)
-fused basement membrane epithelium and basal endothelium
-apical endothelium (capillary)
Diffusion distances of gases
-shorter is better
-measured in microns
Lung Ventilation: Closed compartment
-head, diaphragm, sternum, ribs, and intercostal muscles
-all surround the lungs creating a closed compartment
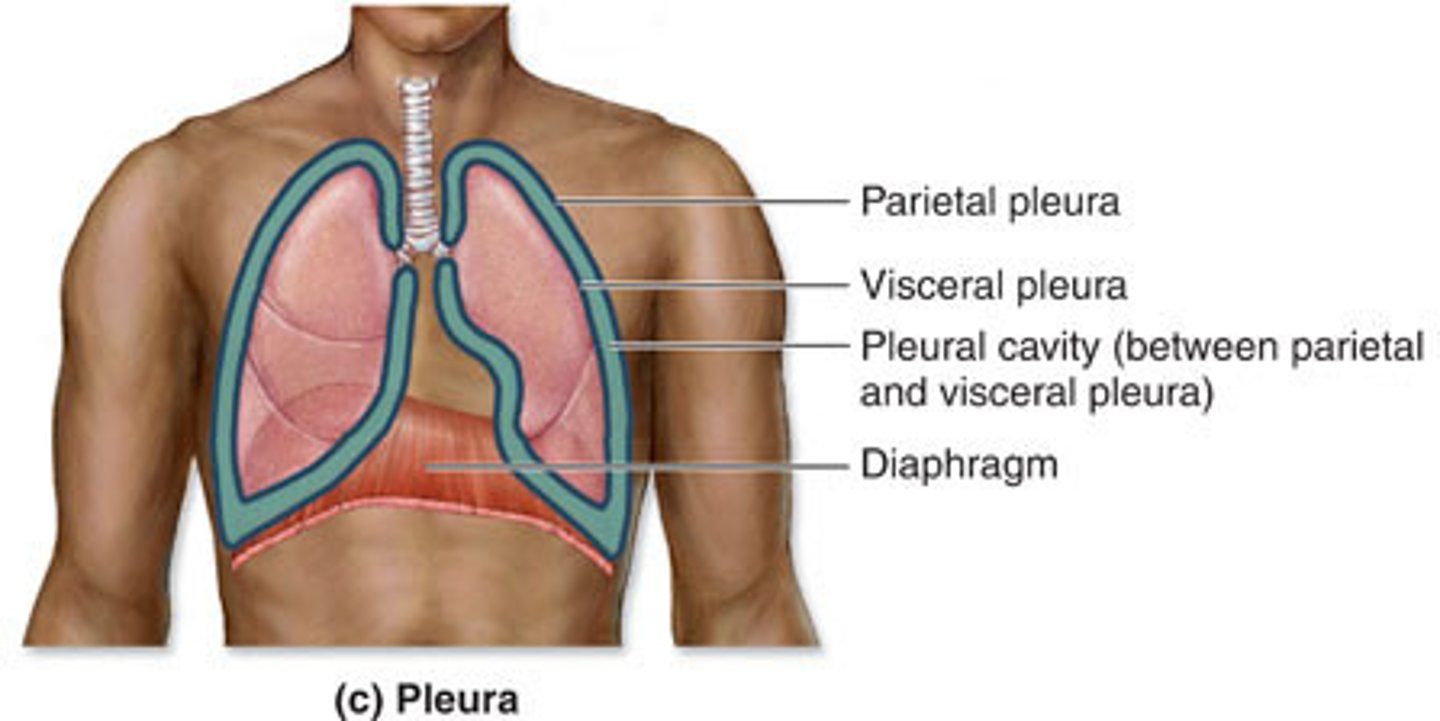
Lung Ventilation: Pleura
-parietal (chest)
-visceral (lungs)
-pleural fluid

How parietal pleura drives visceral pleura
-fluid in between layers allow for them to "stick" and move together
-lungs forced outward, air coming in lungs is drawn inward, pressure in lungs decreases
Ventilation Steps
1. exchange of air between atmosphere and alveoli (bulk flow, high atmospheric pressure to low lung pressure)
2. Exchange of O2 and CO2 between alveoli and lung capillaries by diffusion
3. Transport of gases by blood (bulk flow)
4. Exchange of gases between blood and tissues by diffusion
Bulk Flow
-the movement of a fluid driven by high to low pressure
F = K (ΔP)
K=constant
ΔP=difference between atmospheric pressure and alveolar pressure (bigger ΔP, more air into lungs)
Inspiration
-inhalation
alveolar pressure < 760
Expiration
-exhalation
alveolar pressure > 760
In ventilation, what pressure changes?
Alveolar pressure
2 Cavities in Lungs
-pleural
-pulmonary
Pleural Cavity
space between 2 the pleura
Pulmonary Cavity
air space inside airways (bronchi-alveoli)
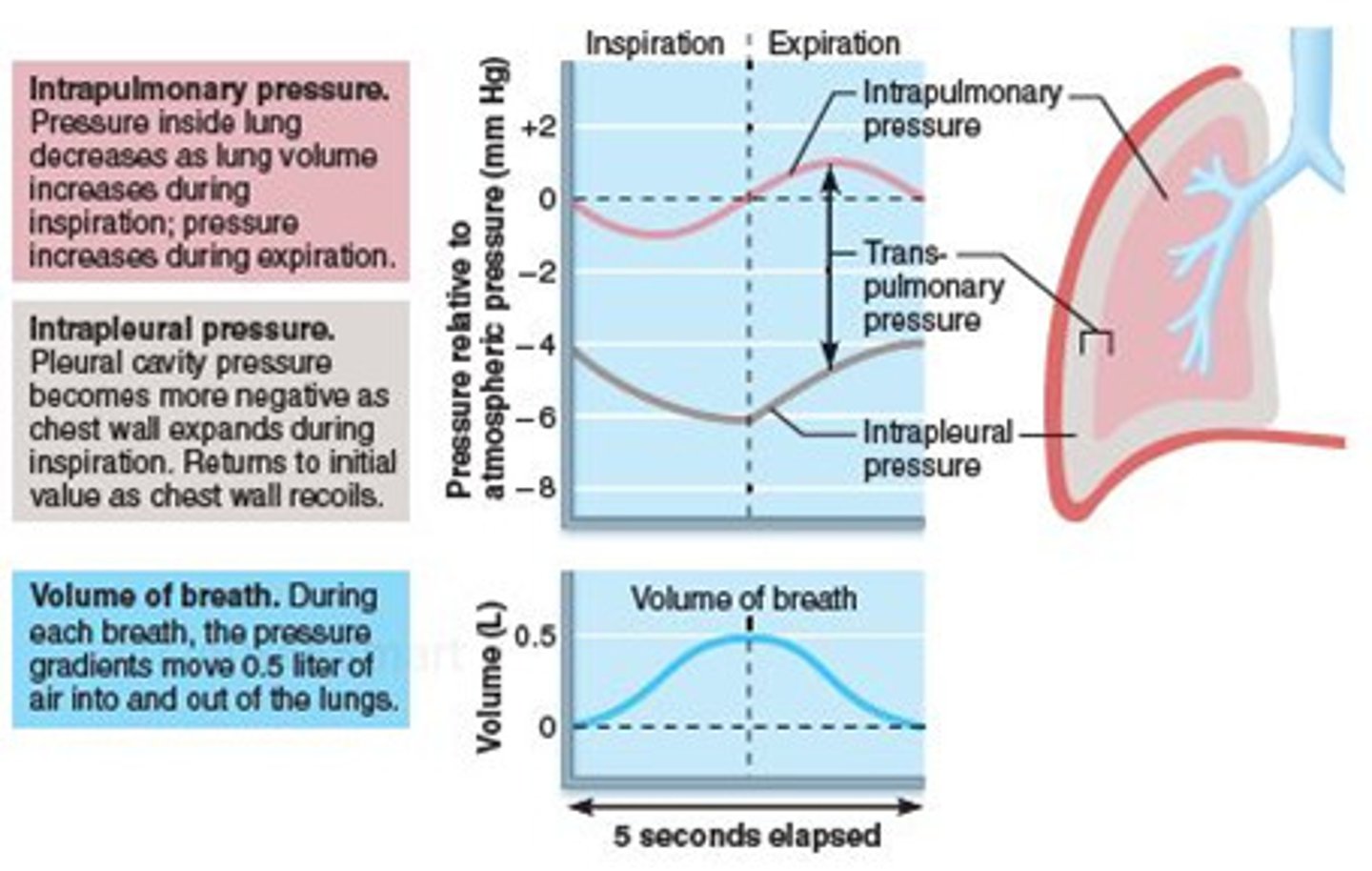
Intrapleural pressure
-pressure within the pleural cavity (fluid)
-we have it bc lung tends to go down to smallest size bc elastic tissue and alveolar fluid (think rubber band)
-chest wall expands and pulls lungs out preventing recoil
Intrapulmonary pressure
pressure of gas inside the alveoli (AKA alveolar pressure)
Inspiration Steps involving pressure
1. Thoracic wall expands
2. Surface tension of fluid causes lungs to be forced out
3. Intrapulmonary pressure decreases, intrapleural pressure decreases
Expiration Steps involving pressure
1. Thoracic wall pushes down on fluid
2. Air pressure in lungs increases (above 760)
3. Intrapulmonary pressure increases, intrapleural pressure increases
Ventilation Graph Steps
1. Beginning inspiration: pressure of gas decreases initially bc volume increases
2. End inspiration: pressure of gas in lungs goes up bc more gas in the lungs
NOW EQUAL PRESSURE 760=760
3. Beginning expiration: gas pressure of alveoli increases bc thoracic wall pushes down on fluid and lungs
4. End expiration: decrease pressure bc more out out of lungs
Air Flow
Flow (F) = ΔP/R
ΔP: change in pressure between atmosphere and alveoli, altered by contraction of inspiratory and expiratory muscles
R: resistance of airways, inversely proportional to the 4th power of the radius
Resistance formula
R= 1/r^4
Lung Complaiance
ΔV/ΔP
ΔV= change in volume
ΔP= change in pressure
-defintion: lungs can change in size rapidly
Athlete's Lung Compliance
-higher than average person
-breathe less times per minute bc theyre bringing in more air w each breath
-lungs are more elastic
-energy saving
Respirometer
-device used to measure extent of respiration
-breathe into tube, upside down container rises and falls, pen draws wave like patterns
Tidal Volume
-normal amount of air breathing in and out
-500ml
Inspiratory Reserve Volume (IRV)
-breathing forcefully in the most air not including tidal volume
-3100ml
Vital Capacity
-forcefully expiring out
-4800ml
IRV+TV+ERV
Expiratory Reserve Volume (ERV)
-volume breathed out that doesn't include tidal volume
-1200ml
Residual Volume (RV)
-air trapped in lungs even after breathing all the way out
-1200ml
Dead Space
-useless air
-about 150ml
-meaning each breath we only bring in ab 350ml of good air
-anatomical dead space: in trachea and bronchioles
-inspired dead space: bad air breathed in
pO2 and pCO2 in "good" and "bad" air
-good air: fresh air, pO2 higher, pCO2 lower
-bad air: dead space air, pO2 lower, pCO2 higher
Alveolar Ventilation
-amount of fresh air breathed into lungs depending on frequency (breaths per minute) and how much air brought in (fresh air tidal volume)
AVR= frequency X tidal volume
-depth is more important
Why do athletes breathe through their nose
increases amount of air brought into lungs and therefore increases O2 being brought in as well
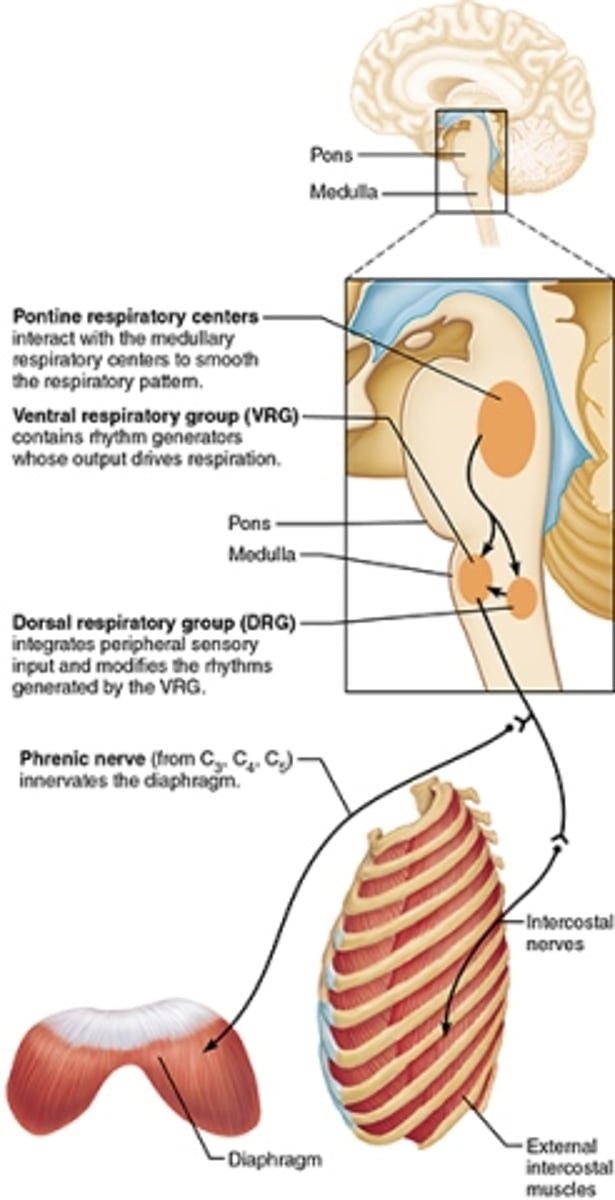
Medullary Respiratory Center
part of the medulla oblongata involved in the neural control of rhythmic breathing
Dorsal Respiratory Group
-a portion in the of the medulla oblongata back of the head where the primary respiratory pacemaker is found
-integrates input info
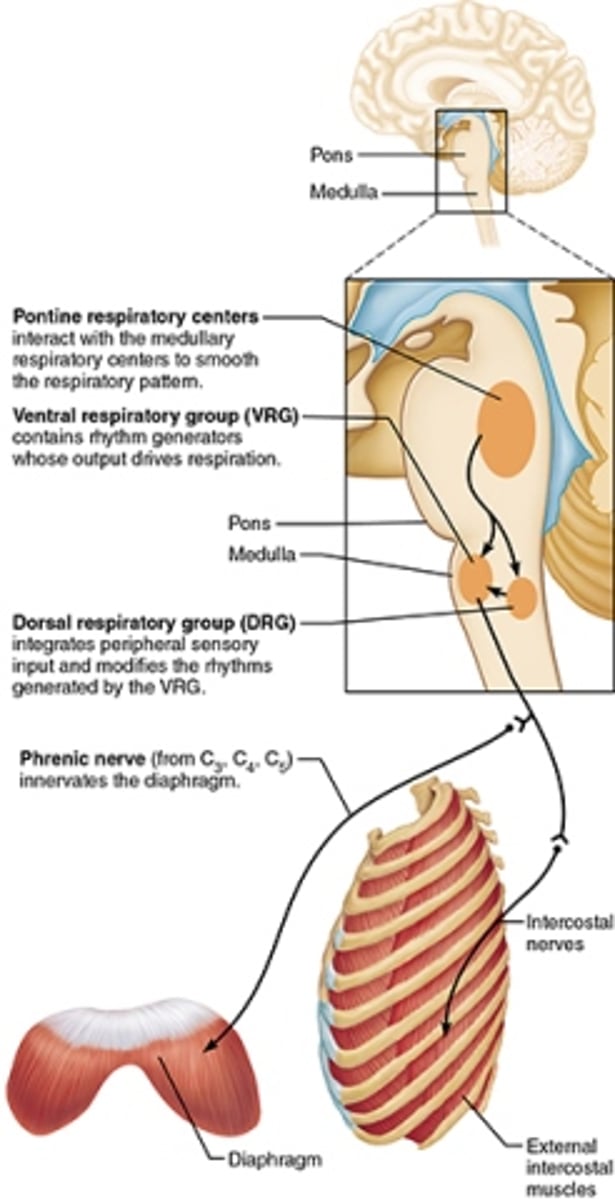
Ventral Respiratory Group
A portion of the medulla oblongata that is responsible for maintaining breathing rhythm
Pontine Respiratory Center
Smooths out breathing and stems into the dorsal and ventral respiratory groups
What muscles contract during expiration
internal intercostal muscles
What muscles contract during inspiration
external intercostals and diaphragm
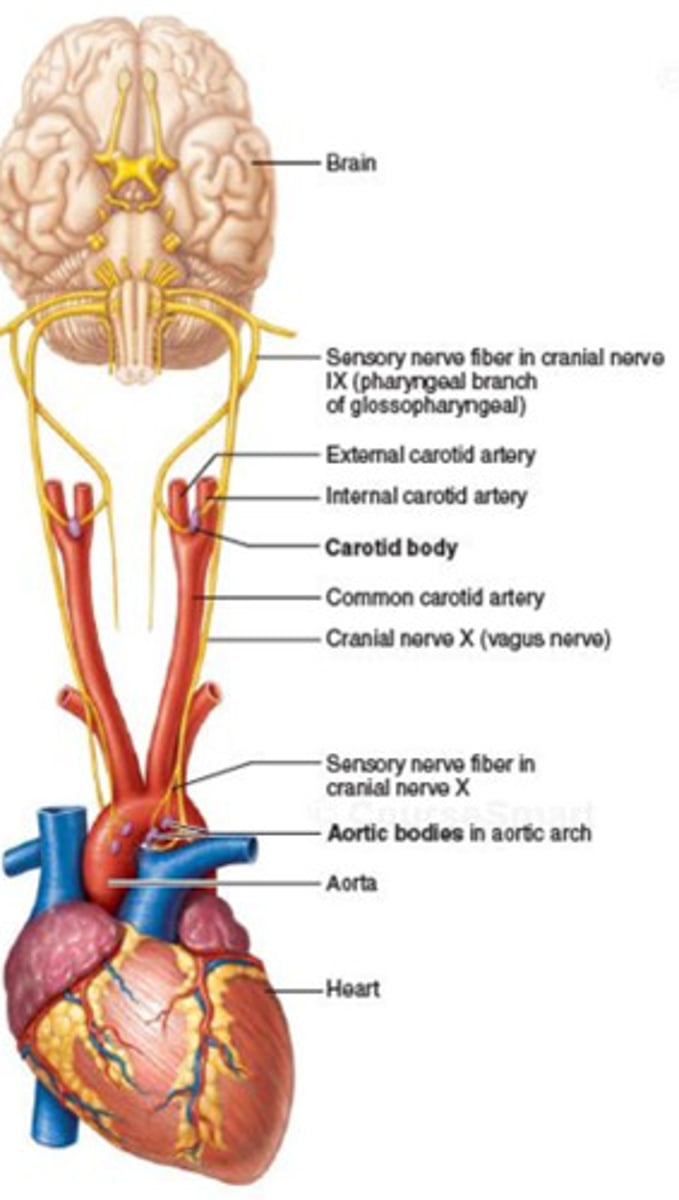
Chemoreceptors
-detect chemical changes in body
-2 Types: Central (brain) and Peripheral (aortic and carotid bodies)