OPP 3 - Peripheral Nerve Entrapment (Lect. & Lab)
1/25
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
26 Terms
General Nerve compression MOI
Brief compression primarily affects myelinated fibers, and classically spares unmyelinated fibers (except in cases of severe acute compression). Acute compression compromises axoplasmic flow which can reduce membrane excitability. Chronic compression affects both myelinated and unmyelinated fibers and can produce segmental demyelination in the former, and if the insult persists, axolysis and wallerian degeneration will occur in both types. The issue of ischemia is more controversial.
Some contend that simultaneous venous stasis at the site of compression can produce ischemia which can lead to edema outside the axonal sheath which may further exacerbate the ischemia. Eventually, fibrosis, neuroma formation, and progressive neuropathy can occur.
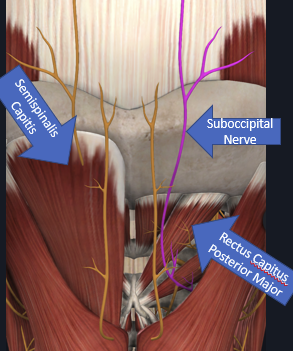
Occipital nerve entrapment
A sensory branch of C2
Entrapment presents as occipital neuralgia: pain in the occiput usually with a trigger point near the superior nuchal line. Pressure here reproduces pain radiating up along back of head towards vertex.
More common in women.
ddx:
headache (may mimic migraine or part of tension HA)
myofascial pain: pain widely separated from trigger point
rare: vertebrobasilar disease, cervical spondylosis, chiari malformation
Possible causes of occipital nerve entrapment
trauma
direct trauma (including iatrogenic placement of suture through the nerve during surgical procedures, e.g. in closing a posterior fossa craniectomy)
following traumatic cervical extension which may crush the C2 root and ganglion between the C1 arch and C2 lamina
fractures of the upper cervical spine”
atlanto-axial subluxation (AAS) (e.g. in rheumatoid arthritis) or arthrosis
entrapment by hypertrophic C1–2 ligament
neuromas
arthritis of the C2–3 zygapophyseal joint
Occipital N entrap Tx
For idiopathic occipital neuralgia: available evidence is from small, retrospective, case series studies and is insufficient to conclude that either local injection or surgery are effective.
Nerve blocks at trigger points with steroids and local anesthetics provide only temporary relief. ex: greater occipital N
usually point at near superior nuchal line, may also block @ point where N. emerges from dorsal neck muscles
Surgical procedures such as nerve root decompression or neurectomy may provide effective pain relief for some patients; however, patient-selection criteria for these procedures have not been defined, and recurrence is common. In idiopathic cases with no neurologic deficit, the condition is usually self limited.
ex: C2 nerve root decompress b/t C1 & C2; in cases of AAS, decompress and atlanto-axial fusion may work
Surgical tx’s for idiopathic occipital neuralgia
release of the nerve within the trapezius muscle. Immediate results: relief in 46%, improvement in 36%. Only 56% reported improvement at 14.5 mos
intradural division of the C2 dorsal route via a posterior intradural approach
occipital neurectomy: relief only occurs in ≈ 50%, and recurrence, usually within a year, is common
Median Nerve neuropathy
C5-T1 nerve roots
Purely motor anterior interosseous nerve which supplies all but 2 muscles of finger and wrist flexion
+ phalens, reverse phalens, tinel’s, and opponens pollicus
2 most common entrapment sites:
wrist @ transverse carpal lig (carpal tunnel syndrome)
Upper forearm @ pronator teres muscle
struther’s ligament
anatomical variant, bridges SCP to medial epicondyle
pronator teres syndrome
From direct trauma or repeated pronation with tight hand-grip.
Nocturnal exacerbation is absent. Pain in palm distinguishes this from carpal tunnel syndrome (CTS)
pain is distal and moves proximal
Carpal Tunnel Syndrome (CTS)
onset over months to years
usually as result of repetitive activity, frequent grasping, ulnar deviation, direct pressure over carpal tunnel, and vibrating hand tools.
systemic causes: pregnant, diabetes, RA
most common compression neuropathy
sx: tingling in the hand, worse at night and with elevation of hands
PE: decreased pinprick in digits 1–3 and the radial half of 4, +Tinels/Phalens/Reverse Phalens, Electrodiagnostics —> Prolonged NCV on EMG
tx: mild —> NSAIDs + neutral positioning
severe —> surgical nerve decompression
Ulnar Nerve Entrapment sites
C7, C8 and T1 nerve roots.
Second most prevalent entrapment neuropathy
Potential sites of compression:
above elbow by the arcade of Struthers
at the elbow in the ulnar groove process.
under the aponeurosis between the heads of the flexor carpi ulnaris
Guyon’s canal Etiologies: structural, mechanical or idiopathic.
May also be due to chronic subluxation out of the ulnar groove
@ elbow = numb in palm AND backside of hand
@ wrist = numb in palm only
Ulnar nerve entrapment sx
Motor/sensory findings include:
Wasting of the interossei
most evident in the first dorsal interosseous (in the thumb web space)
Wartenberg’s sign: one of the earliest findings of ulnar nerve entrapment
abducted little finger due to weakness of the third palmar interosseous muscle--patient may complain that the little finger doesn’t make it in when they reach into their pocket
Sensory findings involving the little finger and ulnar half of the ring finger. Sensory loss over the ulnar side of the dorsum of the hand.
This will be spared in ulnar nerve entrapment at the wrist (dorsal ulnar cutaneous nerve branches proximal to the wrist) Injury above elbow
Meralgia Paresthetica
compression of the lateral femoral cutaneous nerve (L2 and L3 nerve roots) - Erupts medial to ASIS and below inguinal ligament
risk factors: obesity, tight belt/scrub strings
Signs and Symptoms
Burning dysesthesias of lateral thigh
Increased/altered sensation of touch and clothing
Pts may constantly rub lateral thigh
Symptoms to not go past the knee
Disc herniation patterns of pain/numbess
pain —> proximal (thigh, arm)
numbness —> distal (shin, forearm)
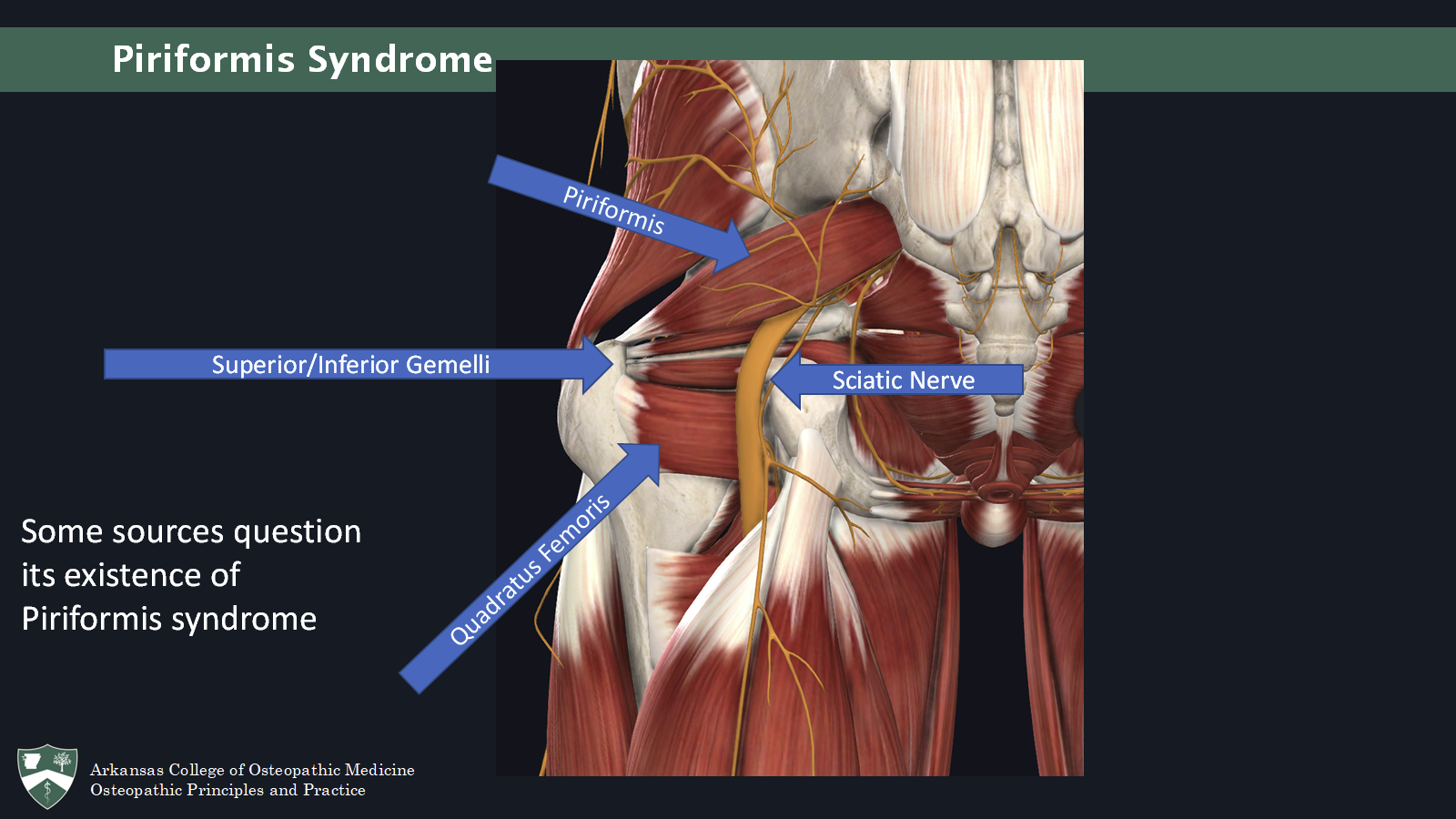
Piriformis syndrome
More common in women
Pain in the gluteal region that travels down
Increases with sitting longer than 15-20 minutes and improves with ambulation
Contralateral SI pain
Parasthesias in posterior thigh and/or foot
Signs:
Ipsilateral leg externally rotated
Ipsilateral leg short
Tenderness in the greater sciatic notch with/without palpable mass
Reproducible with active contraction or passive stretch
Straight leg raise may be positive
In most cases: sacrum is anteriorly rotated to contralat. side
Tx: OMM (ME, CS- peeing dog, HVLA, artic, Still, consider sacrum/pelvis)
untreated can result in chronic pain, parasthesias, or weakness
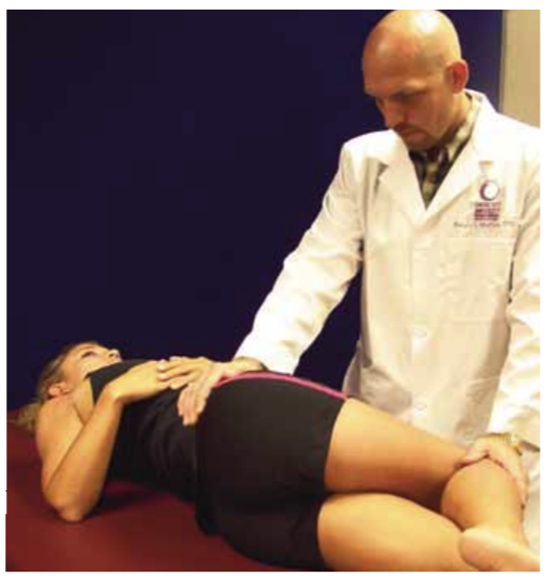
Piriformis Syndrome - FADIR test
Patient in lateral recumbent position
Affected side up
Hip flexed to 60 degrees
Knee flexed to 60-90 degrees
Examiner induces internal rotation and
Adduction of the hip
Downward pressure on the knee
Piriformis Syndrome - Piriformis Sign
While patient is supine
Ipsilateral external rotation of the lower extremity
Piriformis Syndrome - Lesegue Sign (seated straight leg raise)
“worthless” lol
Piriformis Syndrome - Freiberg’s sign
Patient supine
Thigh extended
Passive internal rotation of the leg
Positive if pain is reproduced
Piriformis Syndrome - Pace’s sign
Patient seated
Patient attempts to abduct the thighs against resistance
Positive if pain is reproduced
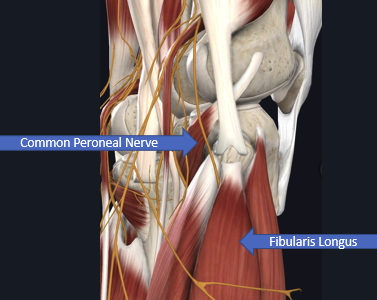
Fibular nerve/Common peroneal nerve compression
may be seen w/ knee or fibular fx’s, also assoc with crossing legs while seated
sx: parasthesias of lat lower leg/dorsum of foot, may have painful dysesthesia
signs: weakness of dorsiflexors, + tinnel’s at some point along nerve course (ex tarsal tunnel), may have prolonged NCV on EMG
tx: OMM for fib head, surgical decompression
ddx: must differentiate from L5 radiculopathy, consider diabetic neuropathy if “painless footdrop”
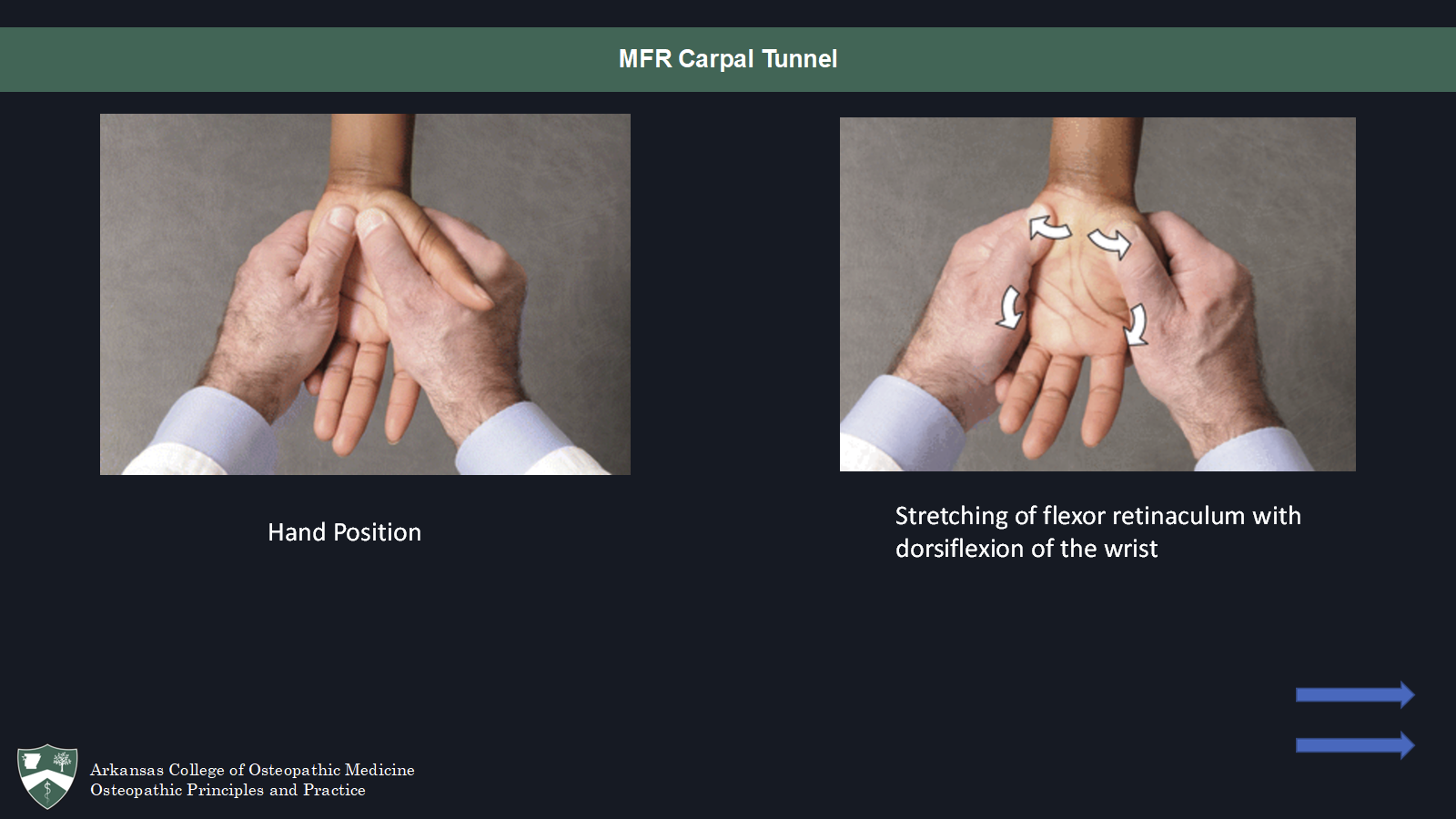
Carpal tunnal - myofascial release (MFR)
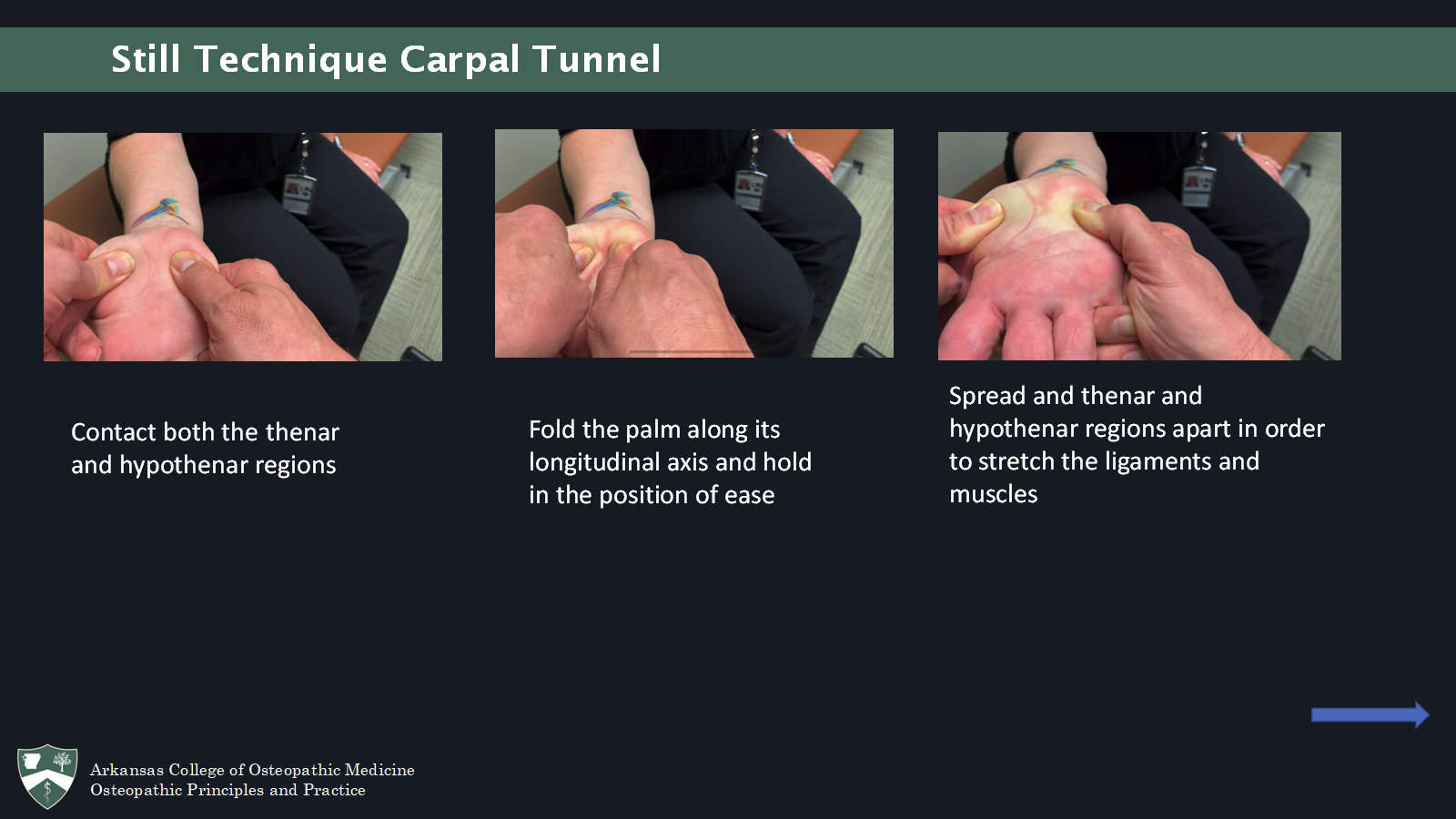
Carpal tunnel - Still’s technique
carpal tunnel - BLT
dorsiflex and ulnar deviate
hold hand like MFR but flipped (thumbs on dorsum, fingers on their palm) and begin w/ them pronated, end with them supinated, dorsiflexing, and ulnar deviated
O/A & A/A
dx and tx
note: make sure to dx A/A while standing
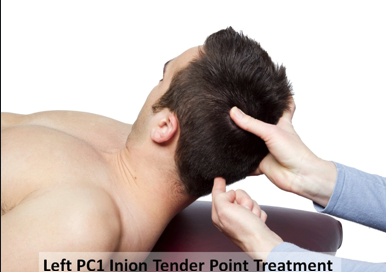
PC1 inion - counterstrain (FStRa)
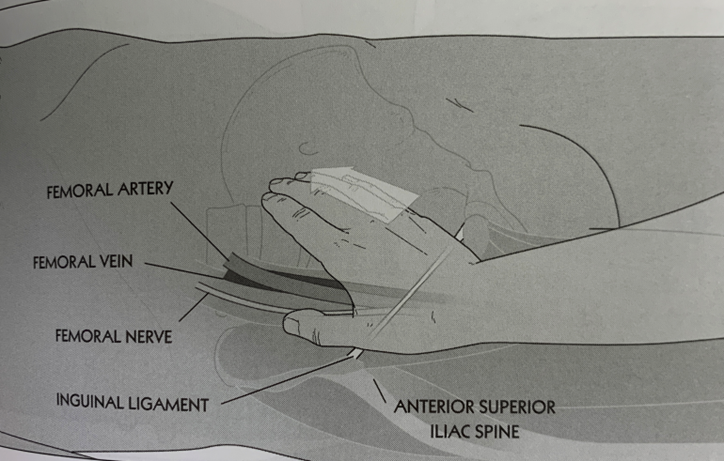
Inguinal Ligament - Articular release
Position – Supine
Contact the middle of the inguinal ligament with the hypothenar eminence. Force is in a superior, medial and posterior direction.
Maintain a steady pressure until a release is felt.