Défense against disease
1/58
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
59 Terms
List three major types of cause of disease.
Pathogens (infectious agents like bacteria, viruses, fungi, etc.)
Genetic factors (inherited conditions)
Environmental factors (e.g., exposure to toxins, poor nutrition)
Define pathogen
A microorganism or other agent (such as viruses) that can cause disease in another organism.
A pathogen is an organism or infectious agent that causes disease. It invades a host and disrupts its normal functioning.
List major pathogen types
Bacteria: Unicellular, prokaryotic organisms. Ex: Tuberculosis, cholera.
Viruses: Require living cells to replicate. Ex: COVID-19, influenza.
Fungi: Eukaryotic organisms, some of which cause disease. Examples: Athlete’s foot, ringworm.
Protists: Unicellular, eukaryotic organisms. Ex: Malaria, toxoplasmosis.
Prions: Infectious proteins that cause neurodegenerative diseases. Ex: Bovine spongiform encephalopathy (mad cow disease).
Define “primary defense.”
refers to the body's first line of defense, which prevents pathogens from entering the body, mainly through physical and chemical barriers such as skin and mucous membranes.
The first line of defence by the body is non-specific and prevents the entry of any potential pathogen into the body.
Outline the role of skin in the defence against pathogens.
Skin acts as a physical barrier with layers of dead, keratinized cells in the epidermis.
Constant shedding of outer skin layers removes attached microbes.
Skin secretes sweat and sebum, lowering pH to around 4-5, inhibiting bacterial growth.
Outline the role of sebaceous glands in the defence against pathogens.
Sebaceous glands secrete sebum containing fatty acids and lipids that lower skin pH.
Antimicrobial properties in sebum prevent bacterial and fungal infections.
Sebum contains antimicrobial peptides that directly neutralize harmful microbes.
Outline the role of mucous membranes in the defence against pathogens.
Mucous membranes line internal body cavities such as the respiratory, digestive, and urogenital tracts, secreting mucus that traps pathogens, preventing them from reaching deeper tissues.
Mucus contains the enzyme lysozyme, which breaks down bacterial cell walls, effectively destroying bacteria that come in contact with it.
In the respiratory tract, cilia (tiny hair-like structures) move the mucus, along with trapped pathogens, toward the throat, where it can be expelled by coughing or sneezing, thus physically removing microbes from the body.
State two benefits of blood clotting when skin is cut.
Prevents excessive blood loss.
Blocks the entry of pathogens at the injury site.
Outline two roles of platelets in the blood clotting cascade.
Platelets accumulate at the site of injury and form a plug to seal the wound.
They release clotting factors, triggering the clotting cascade that leads to the formation of a stable clot.
Describe the blood clotting cascade, including the role of platelets, clotting factors, prothrombin, thrombin, fibrinogen and fibrin.
Platelets rush to the injury site, clumping together to form a plug, acting as a physical barrier that immediately reduces bleeding.
Platelets release clotting factors like thromboplastin and calcium ions, initiating the clotting cascade.
Clotting factors activate prothrombin, converting it into thrombin. Thrombin then converts fibrinogen into fibrin.
Fibrin forms a mesh that traps red blood cells and platelets, creating a stable clot that seals the wound and prevents pathogen entry.
Distinguish between innate and adaptive immunity, including the types of cells and timing of response to infection.
FeatureInnate Immune SystemAdaptive Immune System | ||
Timing of Response | Immediate (minutes to hours) | Delayed (days to respond) |
Specificity | Non-specific, same response to all pathogens | Highly specific, targets particular pathogens (e.g., viruses, bacteria) |
Cells Involved | Phagocytes (e.g., macrophages, neutrophils, monocytes) | Lymphocytes (B cells, T cells) |
Memory | No memory, same response each time | Has memory, quicker and stronger response on re-exposure |
Defense Mechanism | Physical barriers (skin, mucous membranes), inflammation, phagocytosis | Antibody production, cytotoxic T cells |
Duration of Response | Short-term, rapid but limited in duration | Long-term, can last years due to immunological memory |
Communication with Other System | Communicates and activates adaptive immune system if unable to eliminate pathogen | Relies on innate system to activate and present pathogens for targeted attack |
Function of phagocytic white blood cells in defence
Phagocytes like neutrophils and macrophages are crucial in the non-specific immune response, targeting a wide range of pathogens.
They recognize pathogens through receptors on their surface, which bind to the pathogen, initiating phagocytosis.
Phagocytes engulf and digest pathogens, eliminating them from the body before they can spread or cause harm.
Process by which a macrophage destroys a pathogen
Recognition and binding: The macrophage identifies the pathogen by binding to it through receptors on its plasma membrane.
Engulfment: The macrophage extends pseudopodia around the pathogen, engulfing it into a vesicle known as a phagosome.
Phagosome maturation: The phagosome fuses with lysosomes, forming a phagolysosome that contains digestive enzymes.
Digestion: The enzymes break down the pathogen’s components, killing it.
Expulsion: The digested materials are either used by the macrophage or expelled from the cell as waste.
What are the professional phagocytes of the body?
macrophage
neutrophils
Monocytes
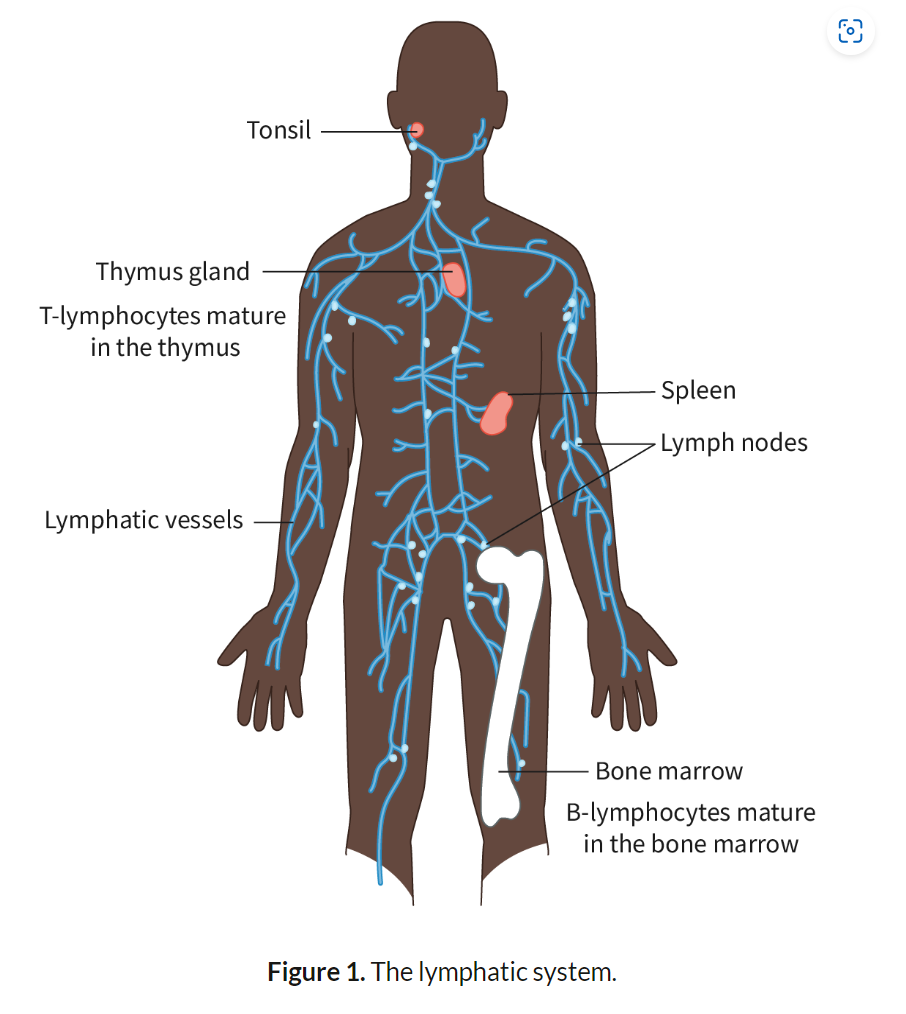
Structure and Function of Lymphocyte Cells
B-Lymphocytes (B-Cells): Develop in the bone marrow. Produce antibodies that bind to specific pathogens. Key role in humoral immunity.
T-Lymphocytes (T-Cells): Mature in the thymus. Two types: Helper T-cells, which activate other immune cells, and Cytotoxic T-cells, which kill infected cells. Involved in cell-mediated immunity.
_______________________________________________________________________
B-Lymphocytes (B-Cells):
B-lymphocytes are a type of white blood cell that develop in the bone marrow and play a critical role in the adaptive immune response.
Once activated by a specific antigen, B-cells differentiate into plasma cells, which are specialized to produce large quantities of antibodies. These antibodies are highly specific and bind to antigens on the pathogen, marking it for destruction by other immune cells or neutralizing its harmful effects.
B-cells are responsible for humoral immunity, which refers to the production of antibodies that circulate in the bloodstream and lymph. Humoral immunity is essential for targeting pathogens in the blood and extracellular fluids.
B-cells also generate memory B-cells after the initial infection, allowing for a faster and more efficient immune response upon future exposures to the same pathogen.
T-Lymphocytes (T-Cells):
T-lymphocytes mature in the thymus and are also involved in the adaptive immune system. T-cells are primarily responsible for cell-mediated immunity, which involves the direct destruction of infected or abnormal cells.
There are two main types of T-cells:
Helper T-cells (CD4+ cells): These cells play a central role in orchestrating the immune response. They activate B-cells, cytotoxic T-cells, and macrophages by releasing signaling molecules called cytokines. Helper T-cells are essential for the initiation and coordination of the immune response.
Cytotoxic T-cells (CD8+ cells): These cells directly attack and kill cells that are infected by viruses or have become cancerous. They recognize infected cells through antigens presented on the cell surface and release enzymes that induce cell death (apoptosis).
Like B-cells, T-cells also form memory T-cells, which remain in the body after an infection and respond rapidly if the same antigen is encountered again, providing long-term immunity.
Interaction Between B- and T-Cells:
Helper T-cells activate B-cells by recognizing the same antigen and secreting cytokines that stimulate B-cells to proliferate and differentiate into plasma cells.
This cooperation between B- and T-cells ensures a coordinated and highly specific immune response tailored to eliminating pathogens effectively.
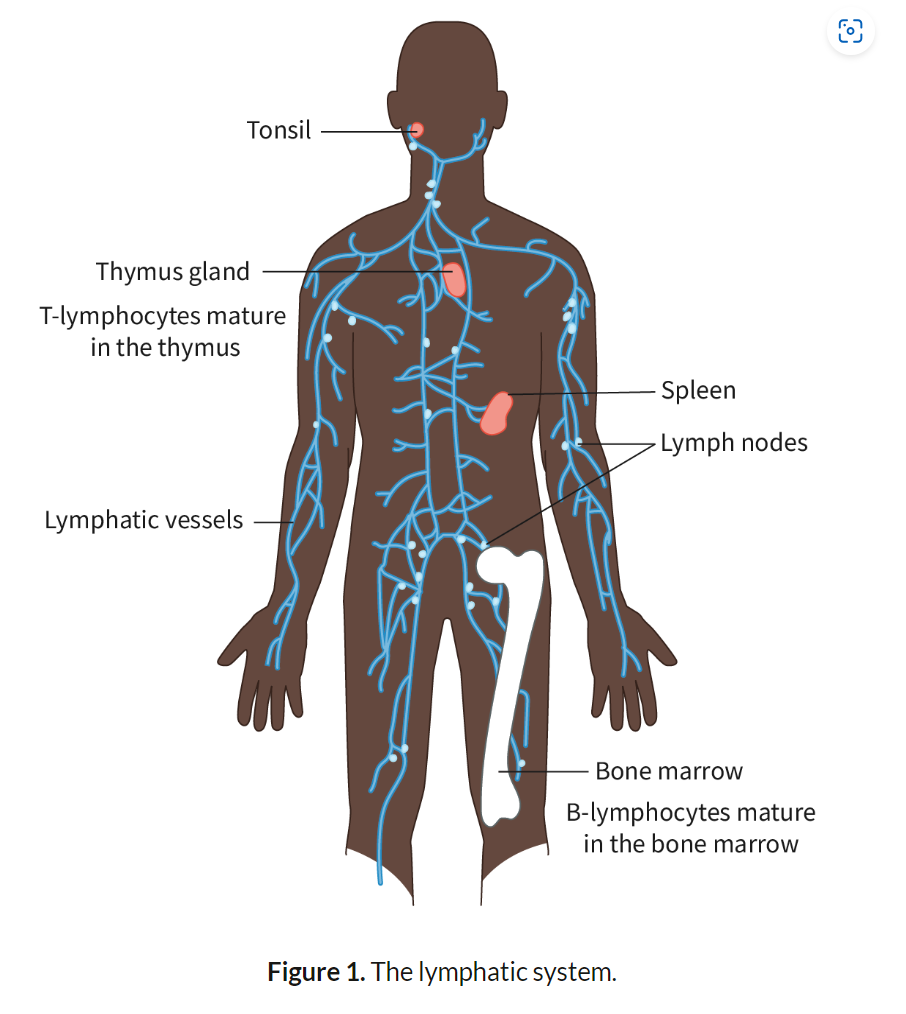
Location of lymphocytes in the body
blood, lymphatic vessels, and secondary lymphoid organs such as lymph nodes, spleen, and tonsils.
Definition of “Specific” in Immune Response:
"Specific" means that lymphocytes recognize and target particular antigens on pathogens, leading to an immune response tailored to that specific pathogen.
Definition of “Antibody”:
Antibodies are Y-shaped proteins produced by B-cells. They bind to specific antigens on pathogens, neutralizing them or marking them for destruction.
Role of Lymphocytes in Producing Antibodies:
B-Cells recognize a specific antigen, become activated, and differentiate into plasma cells, which secrete large amounts of antibodies. These antibodies bind to the antigen and help eliminate the pathogen.
Definition of Antigen:
An antigen is any substance that triggers an immune response by stimulating the production of antibodies. Antigens are usually proteins found on the surface of pathogens.
Antigens are typically proteins, glycoproteins, or lipoproteins found on the surface of pathogens. They are recognized by immune cells due to their unique molecular structure.
Cause and Consequence of Antibody Binding to an Antigen:
Cause: Antibodies bind to antigens due to complementary shapes, like a lock and key, targeting specific pathogens.
Consequence 1 – Neutralization: Antibodies block pathogen entry into host cells by binding to key sites, preventing infection.
Consequence 2 – Opsonization: Antibodies mark pathogens for destruction by phagocytes, making them easier to recognize and engulf.
Consequence 3 – Complement Activation: Antigen-antibody complexes trigger complement system, which punches holes in the pathogen's membrane, leading to membrane attack complexes that destroy pathogens.
Difference Between ABO Blood Antigens:
Blood groups are determined by the presence of specific antigens on the surface of red blood cells:
Group A: Has A antigens.
Group B: Has B antigens.
Group AB: Has both A and B antigens.
Group O: Has no A or B antigens.
Consequence of Mismatched Blood Transfusions:
When incompatible blood is transfused, the recipient’s antibodies bind to the donor’s RBC antigens, leading to agglutination (clumping of RBCs) - clumping blocks blood vessels and disrupts normal blood flow.
and hemolysis (rupturing of RBCs) releasing hemoglobin into the bloodstream. Free hemoglobin can damage organs, particularly the kidneys, leading to kidney failure, shock, and in severe cases, death.
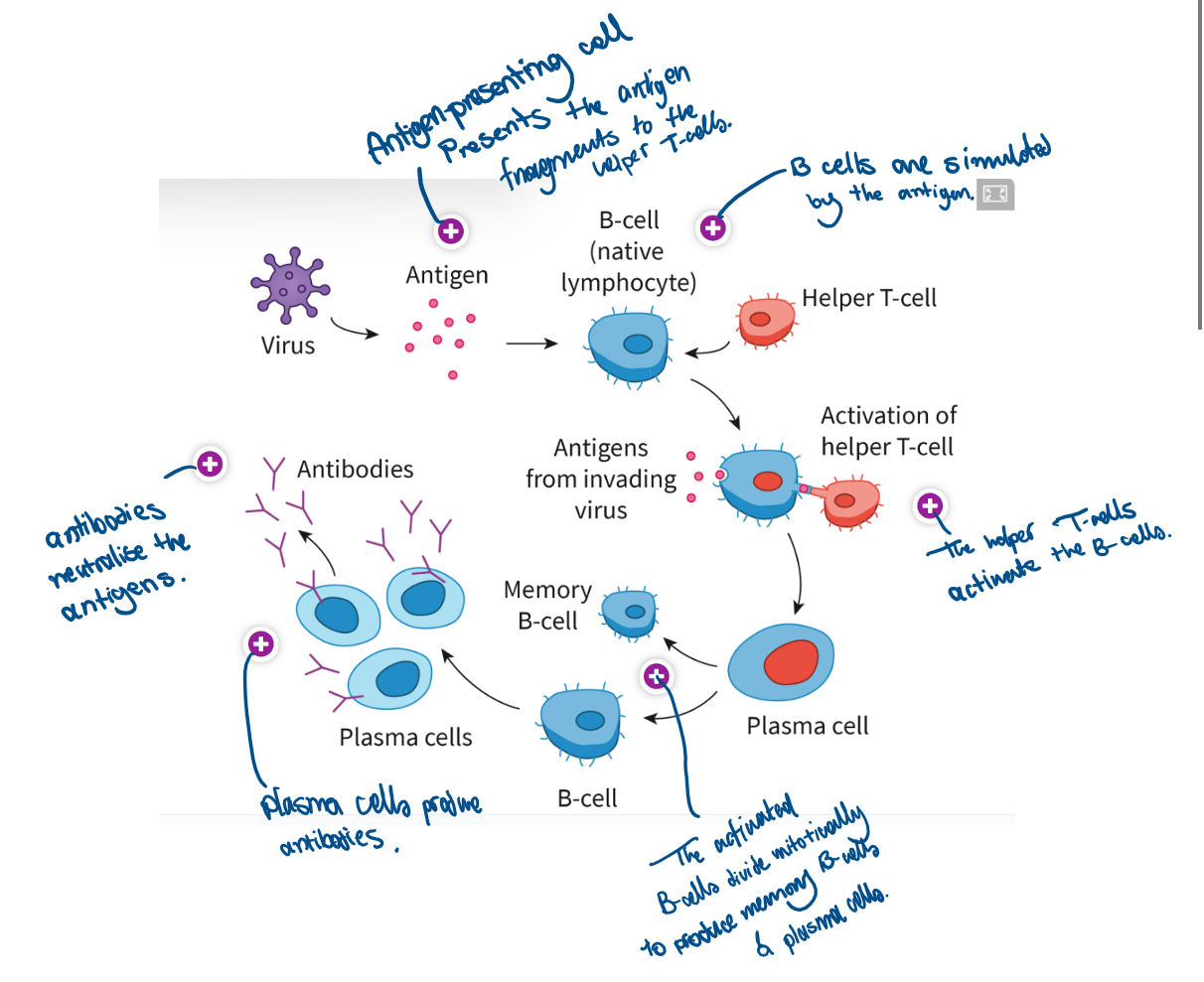
Describe activation of helper T lymphocytes by a macrophage
Phagocytes that digest a pathogen retain fragments of it. Antigen-presenting cells present the fragments to specific helper T-cells, thereby activating the latter.
What happens once a T-cell is activated?
results in an increase in the number of helper T-cells that recognise the same antigen
activates the B-cells specific to the same antigen
activates cytotoxic T-cells specific to the same antigen.
What does the activation of B-cells depend on?
-when the receptor present on the surface of a B-cell recognises and binds to a specific antigen.
-the stimulation by an activated helper T-cell that recognises the same antigen.
Outline the role of the helper T lymphocytes in the activation of B lymphocytes
Activated helper T-cells release cytokines that stimulate specific B-cells. Helper T-cells also interact with B-cells directly by binding to the same antigen, ensuring activation.
B-cells secrete antibodies only after activation by helper T-cells through antigen recognition and cytokine signaling.
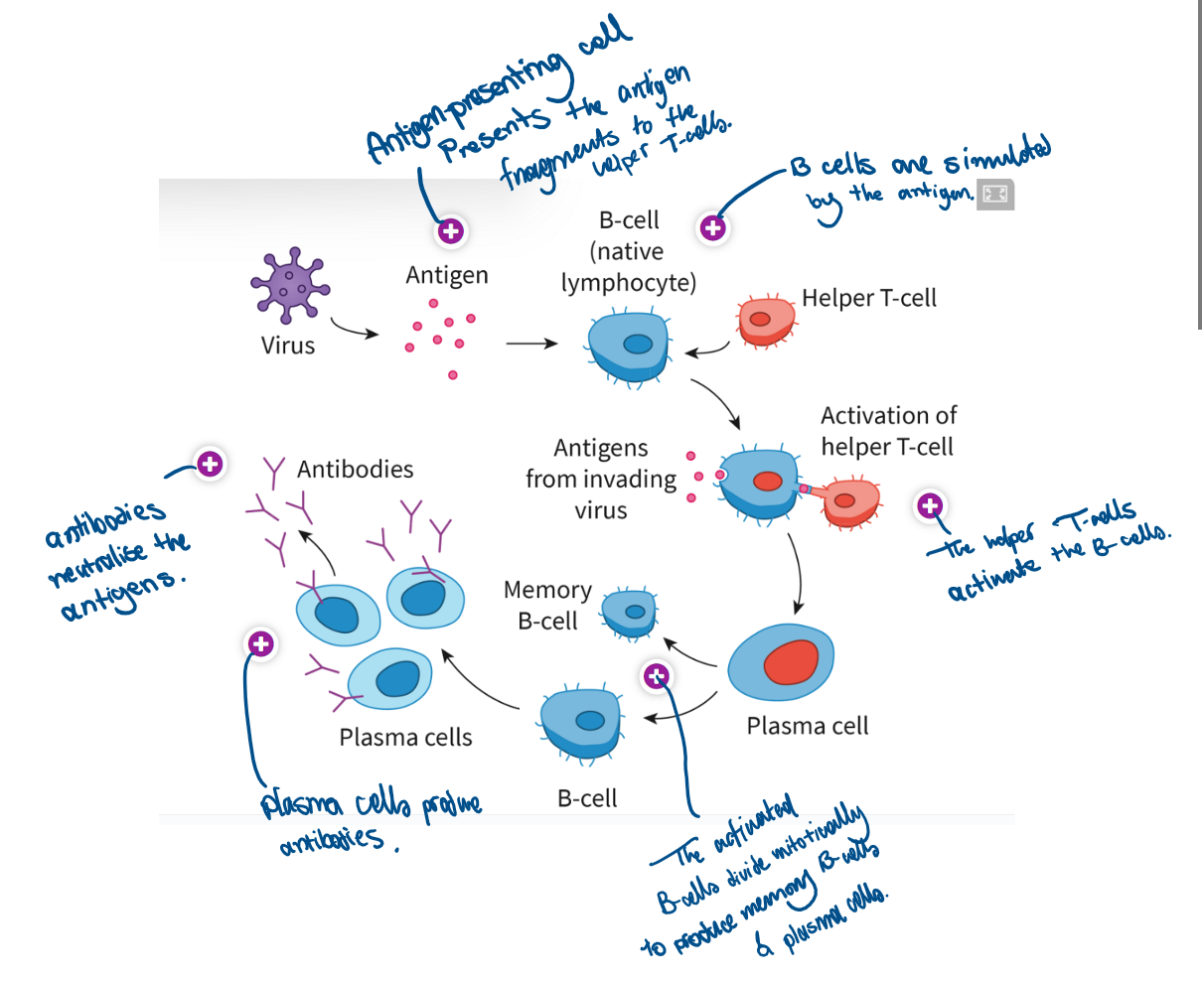
Describe clonal selection of plasma B cells
Only the B-cells with receptors specific to the antigen are selected to multiply. These cells undergo repeated mitosis to form identical clones.
Plasma B-cells produce antibodies only after maturation and differentiation to enhance their capacity for large-scale protein synthesis.
Define immunity
Immunity is the body’s ability to resist infection due to the presence of memory cells, which enable a rapid and specific immune response to previously encountered pathogens.
Outline the role of memory B cells in maintaining immunity
Memory B-cells persist in the bloodstream and lymph nodes after an initial infection. They "remember" the antigen and quickly differentiate into plasma cells upon reinfection, producing antibodies more efficiently.
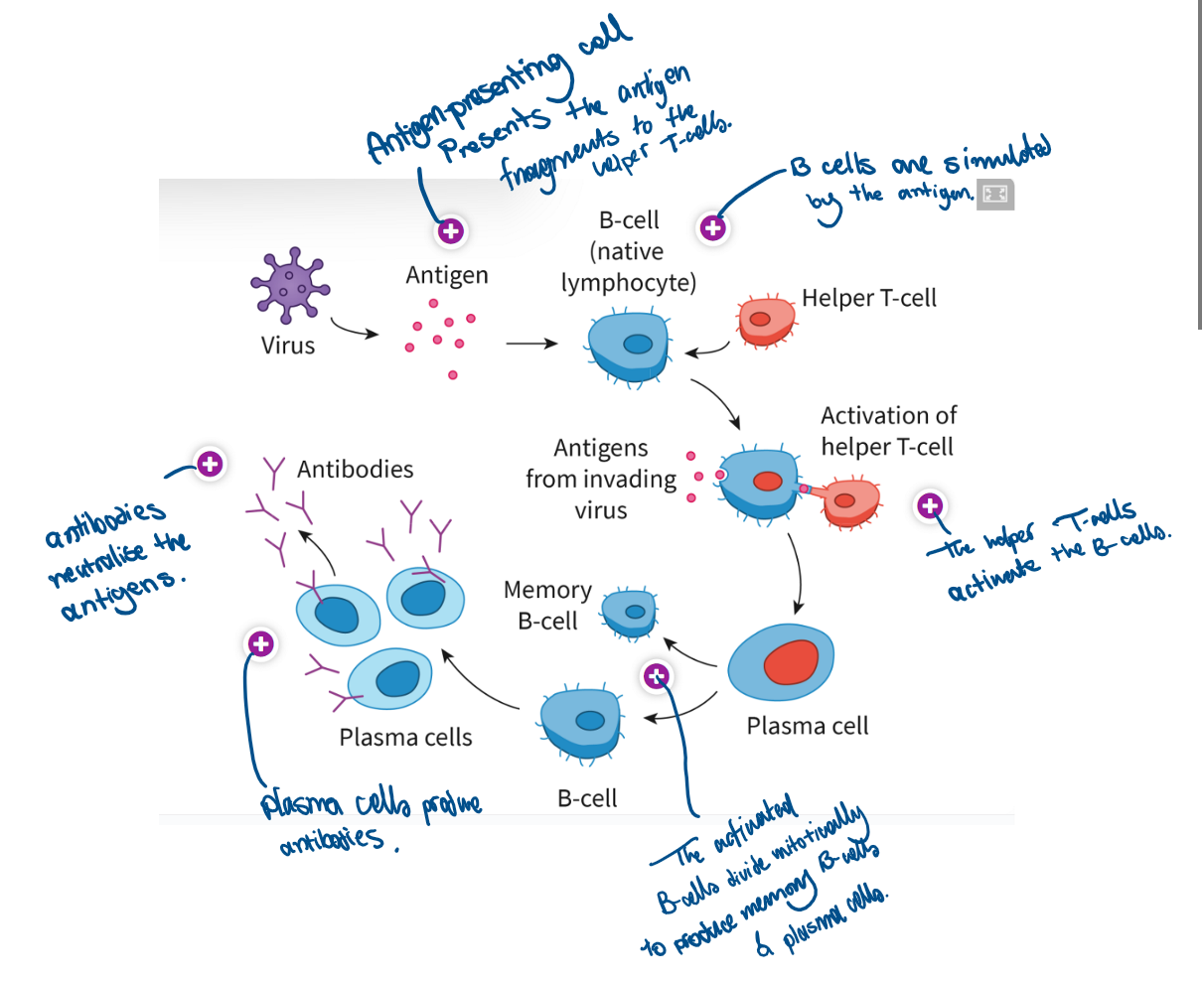
Compare the primary and secondary immune responses to specific pathogens.
Feature | Primary Immune Response | Secondary Immune Response |
Magnitude | Smaller response; fewer antibodies produced. | Larger response; significantly more antibodies produced. |
Speed | Slower; takes days to weeks to develop. | Faster; begins within hours due to memory cells. |
Duration | Shorter-lasting immunity. | Longer-lasting immunity; sustained by memory cells. 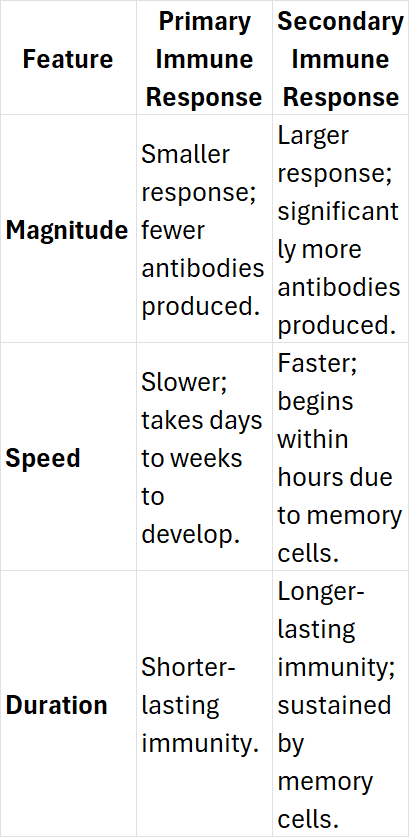 |
What are plasma cells?
B-cells that produce antibodies
Mechanisms of HIV transmissions
Sexual intercourse with an infected person (via vaginal fluids or semen).
Transfusion of infected blood.
Sharing needles or syringes.
From mother to child during childbirth or breastfeeding.
Describe the consequences of HIV on the immune system
HIV targets helper T-cells (CD4+ T-cells), critical for activating B-cells and cytotoxic T-cells.
Viral replication in T-cells leads to cell lysis, reducing helper T-cell count.
A weakened immune system makes the individual vulnerable to opportunistic infections.
The immune response is progressively impaired, culminating in AIDS.
Outline the relationship between HIV and AIDS
HIV is the causative agent of AIDS (Acquired Immunodeficiency Syndrome).
HIV attacks the immune system, specifically the helper T-cells, which weakens the body’s ability to fight infections.
Over time, as the number of helper T-cells decreases, the individual becomes vulnerable to severe infections and certain cancers, a condition known as AIDS.
The transition from HIV to AIDS occurs when the immune system is significantly impaired, and the individual becomes highly susceptible to opportunistic infection
The different stages of HIV
Stage 1
Acute HIV infection is the initial stage where the HIV multiplies and destroys the helper T-cells. During this period, the level of HIV in the blood is high, which increases the risk of transmission.
Stage 2
Chronic HIV infection is the stage where the HIV multiplication drops to low levels. Individuals in this stage may not have obvious symptoms. This stage could last for several years.
Stage 3
At the final stage, the body cannot fight opportunistic infections. The individuals suffer from a range of conditions affecting different organ systems due to the progressive weakening of the immune system, leading to the term, ‘acquired immuno-deficiency syndrome’ or AIDS.
What’s a retrovirus and example of retrovirus
A retrovirus is a virus that has RNA as its genetic material. On infection, reverse transcription occurs and the RNA is converted to DNA.
Outline the natural function of antibiotics when secreted from saprotrophic fungi
Antibiotics are naturally produced by saprotrophic fungi to compete for resources by inhibiting or killing other microorganisms that could be harmful or take up nutrients. This gives the fungi a competitive advantage in their environment.
Antibiotic: A substance that can kill or inhibit the growth of certain bacteria.
Outline the function of antibiotics when used in medical treatment.
Antibiotics are used in medicine to treat bacterial infections by either inhibiting bacterial growth (bacteriostatic) or killing bacteria directly (bactericidal). They target specific bacterial structures, such as cell walls or protein synthesis machinery, which are not present in human cells.
State why antibiotics fail to control viral infections.
Antibiotics are ineffective against viral infections because viruses do not have cellular structures that antibiotics can target. Viruses hijack host cells for replication and lack the independent metabolic processes that antibiotics typically disrupt in bacteria.
Describe how natural selection leads to the development of antibiotic resistance in bacteria.
When bacteria are exposed to antibiotics, some bacteria may have genetic mutations that give them resistance, such as the ability to pump out the drug or break it down. These bacteria survive the treatment and reproduce, passing on the resistant traits to offspring, gradually increasing the population of resistant bacteria.
Discuss the medical cause and consequences of evolution of antibiotic resistance
The overuse and misuse of antibiotics (e.g., incorrect prescriptions or incomplete courses of treatment) accelerate the development of resistance. This makes infections harder to treat, resulting in longer hospital stays, higher healthcare costs, and increasing mortality rates due to multidrug-resistant (MDR) bacteria
Outline the major routes of pathogen transmission.
Pathogens can be transmitted from animals to humans through direct contact (e.g., bites, scratches), indirect contact (e.g., contaminated food or water), or vector organisms (e.g., mosquitoes transmitting viruses like Japanese encephalitis).
Outline the reason why most infectious agents are species-specific.
Most infectious agents are species-specific due to differences in host cell receptors, immune systems, and cellular environments.
Pathogens are adapted to infect particular species where they can effectively replicate and thrive.
Define zoonosis.
A zoonosis is an infectious disease that can be transmitted from non-human animals to humans, typically involving pathogens like viruses, bacteria, or parasites that have reservoirs in animal species.
Mycobacterium tuberculosis, the causative agent of tuberculosis, can be transmitted from cattle to humans through contaminated dairy products
List two reasons that will lead to an increase in the appearance of zoonotic diseases in humans.
Increased human-wildlife interaction due to habitat encroachment
global travel and trade, which facilitate the spread of zoonotic diseases across regions and species.
Definition of Immunization
Immunization is the process by which an individual becomes protected from a specific infectious disease, either through vaccination (introduction of a vaccine) or by naturally acquiring immunity after a previous infection.
Life attenuated Vaccines
vaccines contain weakened forms of the live pathogen.
They stimulate a strong immune response because the pathogen is still capable of replicating but cannot cause disease.
Example: Oral polio vaccine.
Inactivated Vaccines
killed or inactivated versions of the pathogen. They can be safer but often require boosters.
Example: Inactivated polio vaccine (IPV).
DNA Vaccines:
Utilize plasmids (genetic material) from the pathogen to trigger the immune system. Example: Zydus Lifesciences’s COVID-19 vaccine.
RNA Vaccines:
Introduce messenger RNA (mRNA) that codes for an antigen, stimulating an immune response without using the pathogen itself.
Example: Pfizer and Moderna COVID-19 vaccines.
Principle of Vaccination
Vaccines work by mimicking an infection. This prompts the immune system to respond by producing memory B-cells that "remember" the pathogen.
Primary Immune Response: Occurs when the body encounters the antigen for the first time. This response is slower as the immune system learns to recognize the pathogen.
Secondary Immune Response: If the body encounters the same pathogen again, memory B-cells quickly recognize and respond, often neutralizing the pathogen faster and more effectively.
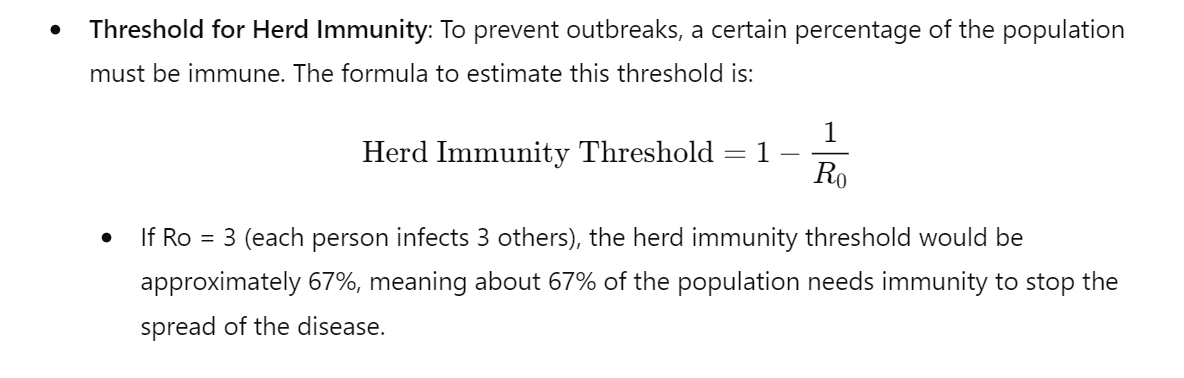
Herd Immunity
Refers to the immunity of a population, which occurs when a large proportion of individuals are immune to a particular disease (either through vaccination or prior infection).
This reduces the overall spread of the disease and protects those who are not immune, such as the immunocompromised, babies, and the elderly.
Explain how Herd Immunity Limits Disease Transmission
When enough people in a community are immune, the spread of the pathogen slows down, making it harder for the disease to spread to vulnerable individuals. This is critical in protecting those who cannot be vaccinated.
Define Ro (Basic Reproduction Number):
Ro represents the average number of secondary infections produced by an infected individual in a fully susceptible population.
Given an Ro value, estimate the percentage of people in a population who must be immune to reach herd immunity.
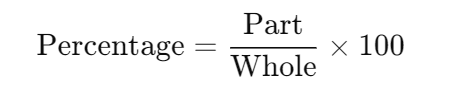
Expressing One Number as a Percentage of Anothe
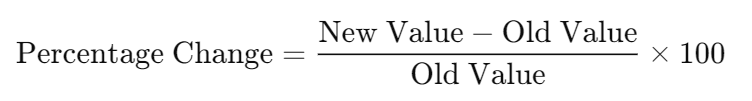
Percentage Change:
Percentage Difference: