CC10 Antimicrobial Modes of action & mechanisms of resistance
1/42
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
43 Terms
What are the requirements for antimicrobial activity
Adsorbs to cell surface
Passage into cell
Interacts with specific target e.g. ribosome/nucleoid
Disinfectant mode of action
Has a specific mode of action
multiple cellular targets
e.g.
oxidation
crosslinking
coagulation
disruption of structures
Describe oxidation
Disruption and breakage of chemical bonds in macromolecule
How does oxidation break bonds through DNA/RNA
Strand breakage, binding to DNA or RNA
Disrupts transcription, translation and replication
e.g. peroxide penetrates spores and reacts with DNA
How does oxidation occur through fatty acids
Reaction and degradation of unsaturated fatty acids in cell membranes
Disrupts membrane
Leakage of cytoplasmic contents
How does oxidation occur through disulfide bonds
Modification of S-S bonds
loss of protein structure
Disrupts enzyme function and results in cell death
Describe X-linking and coagulation
Interactions between macromolecules
such as clumping
leads to loss of function
X linking
Aldehydes cause the cross linking of lysine residues to other amino acids
This change in protein structure can cause protein aggregation (exposure of hydrophobic residues)
Cross linking of DNA/RNA/PROTEINS/PEPTIDOGLYCAN
Describe coagulation
Occurs due to macromolecule denaturation
Can lead to coagulation and precipitation
Chlorohexidine
Phenols
Ethanol
QAC’s
What is precipitation
disruption of cytoplasm, lipid membranes
Describe the mode of action for disruption of cellular structures
Disruption of functional structures
for example cell wall and cytoplasmic membrane
How does this disruption occur with reference to ions
+VE ions have affinity for -VE microbial membranes
Disrupts proton motive force
Disrupts cell-membrane associated activities e.g. energy generation
What is the proton motive force
A gradient of electrochemical charge across a membrane
Movement of protons across a membrane
Cells cannot function without
How can heavy metals disrupt cellular structures
Directly bind to and damage lipid membrane
Indirectly bind by charge to LPS (lipopolysacchride)
Describe the effect of concentration
At low concentrations:
reversible enzyme inhibition
permeability changes
structural damage
leakage
At high concentrations:
Autolysis
Lysis
Cytoplasm coagulation
Describe the effect of increasing exposure time
Short time:
Bacteriostatic
Inability to repair
Long time:
Bactericidal- LETHAL
Biocides and cellular targets
Different biocides can target different cellular target
Can have multiple targets e.g. bacteria, fungi, viruses, protozoa, helmets
Outer membrane targets
Agents: QACs, Mercury (Hg), Silver ions (Ag+), EDTA.
Effect: Disrupts the outer membrane.
Cell wall targets
Agents: Low concentration of phenol, formaldehyde, hypochlorite, EDTA.
Effect: Damages the cell wall.
Cytosol targets
Agents: Aldehyde, phenols, biguanides, QAC.
Effect: Causes coagulation of cellular contents.
Ribosome targets
Agents: Oxidizing agents, peroxygen.
Effect: Damages ribosomes, impacting protein synthesis.
Protein targets
Agents: Alcohols.
Effect: Denatures proteins.
Coagulation in Cytoplasm targets
Agents: High concentration chlorhexidine, phenol, mercury (Hg) salts.
Effect: Leads to protein coagulation.
Membrane Proton Motive Force targets
Agents: Parabens, phenols.
Effect: Disrupts proton motive force, impacting energy production
Membrane Permeability targets
Agents: Cetrimide, chlorhexidine, phenol, ethanol.
Effect: Increases permeability, damaging the cell membrane.
Membrane associated activity targets
Membrane ATPase: Chlorhexidine disrupts ATP synthesis.
Electron Transport System: Hexachlorophane interferes with electron transport.
Enzymes with -SH Groups: Mercury and silver disrupt these enzymes.
Nucleic acid targets
Agents: Aldehyde, peroxygen, biguanides, phenols, QACs.
Effect: Damages DNA/RNA, preventing replication and transcription.
What are the 5 mechanisms of resistance
Intrinsic/innate resistance : A natural chromosomal encoded property
Extrinsic/acquired resistance: organism becomes resistant
Phenotypic resistance: Response to mode of growth- reversible
Genetic resistance: Mutation or genetic transfer- irreversible
Co-resistance: multiple resistance genes
What factors affect innate resistance
Composition of outer layer
Efflux pumps
What are efflux pumps
Antimicrobial pumped out of cell via pumps in the cell wall
So the agent doesn’t reach optimum concentration
What are the types of efflux pumps
Chromosomal encoded pumps
which contributes a natural low level of resistance at all times
What is a biocide
a chemical, mixture, or microorganism that controls harmful organisms in a way that's not purely physical or mechanical
List the 3 mechanisms of innate resistance to biocides
physical barrier to protection e.g. spores, waxy fatty acids, outer membrane, peptidoglycan
Decreased accumulation of biocide through efflux pumps, degradation
Absence of target/ metabolic pathway
What are the two types of acquired phenotypic resistance
intracellular bacteria: A parasite inside protozoa, isolated = more resistant
Biofilms: Physical barrier, cell-cell communication, 3D community, increased genetic exchange
What are the 2 acquired genetic resistance mechnaisms
Chromosomal mutation/gene transfer
Efflux
How do mutations affect resistance
Changes proteins, fatty acids, phospholipids
Changes O-chain lengths of LPS
Changes number and size of porins
Modifies target
alters metabolic pathway
Increases efflux
ALL CAN DECREASE EFFICACY OF ANTIMICROBIAL AGENT
How can Efflux affect
Creates widespread resistance of multiple solvents, detergents, antibiotics
Controlled by Multiple antibiotic resistance operon
mar A - activator
mar - repressor
How can we increase efficiency of pump
inactivate mar R
over express mar R
This up regulation can be produced by mutation
Describe multi-drug resistant plasmids
Different plasmids code for different resistance
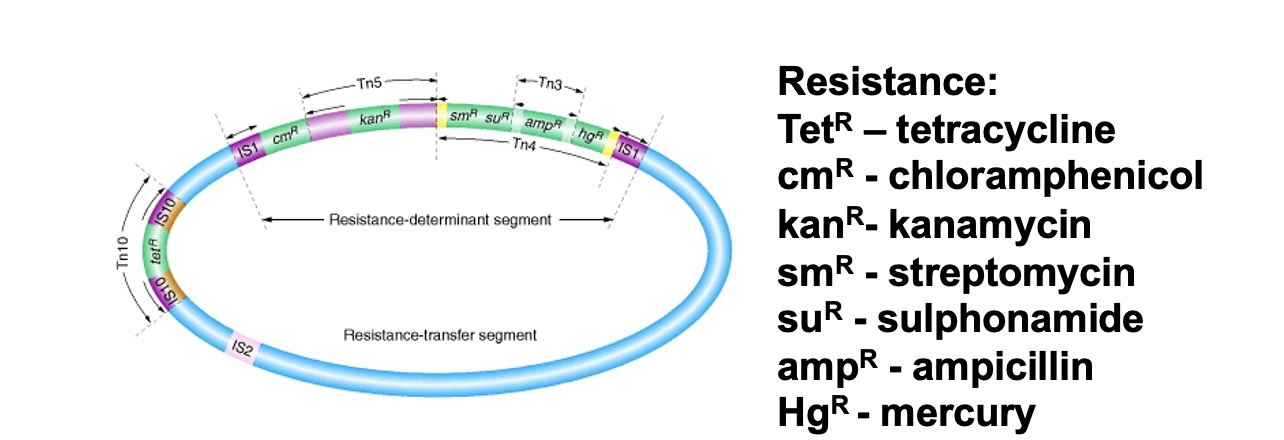
Co-resistance
Selecting resistance for one antimicrobial selects resistance for every compound encoded by plasmid e.g. both antibiotics and biocides
How can we reduce development of resistance
What is meant by the ‘Chain of infection’
Infectious agent
Reservoir
Portal of exit: the way the infectious agent leaves the reservoir
Mode of transmission
Portal of entry
Susceptible host (any person in healthcare)
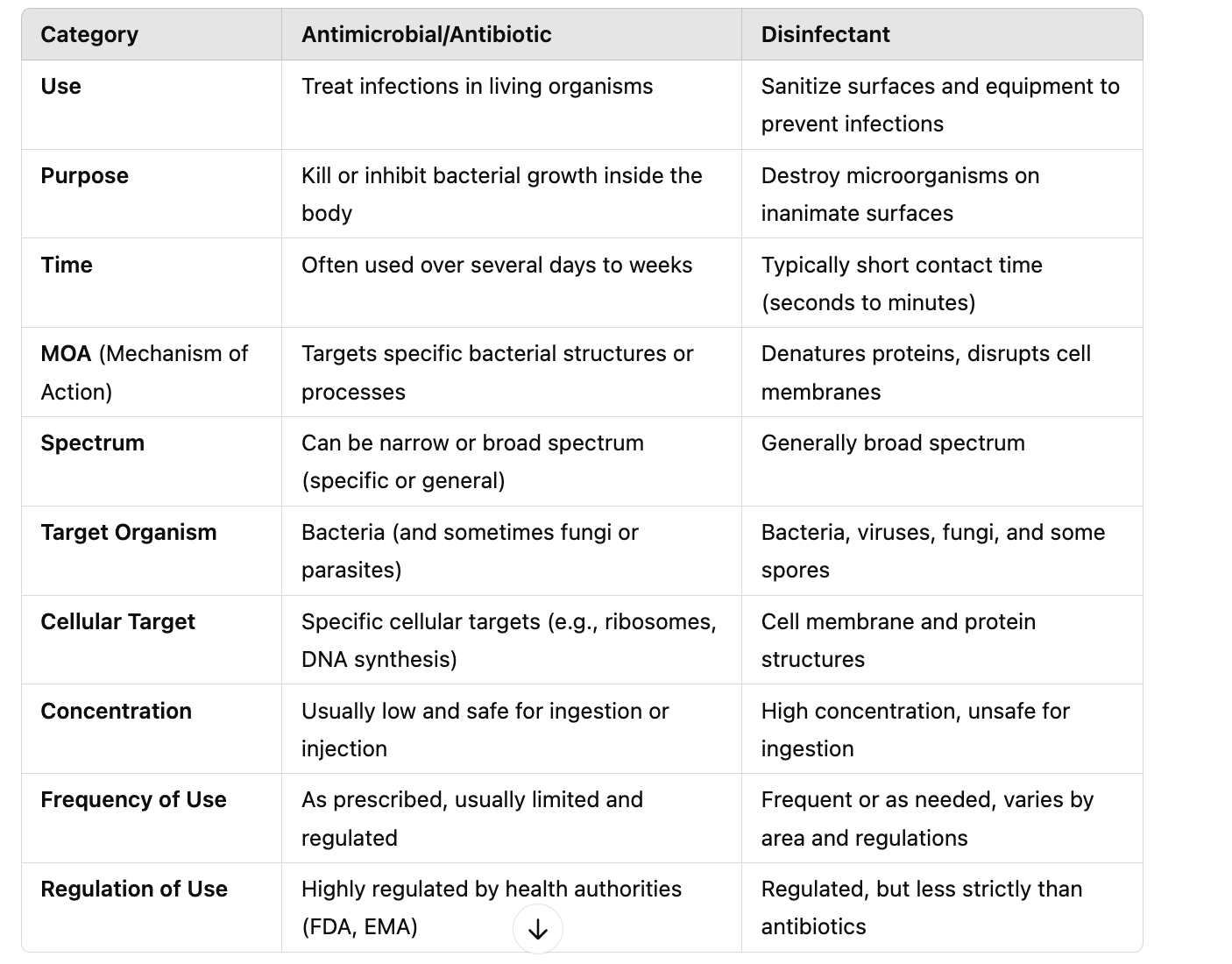
Disinfectant vs antimicrobial