(pt 2) exam #1 - immunohematology (cls 544)
1/54
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
55 Terms
history of the ABO blood group system
1901: Discovered by Dr. Karl Landsteiner
Noted three different patterns agglutination named A, B, C
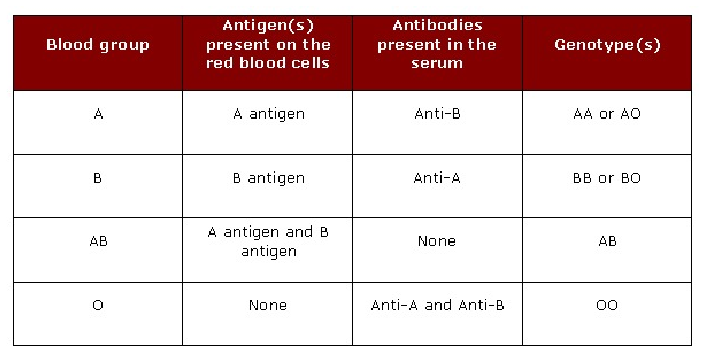
ABO blood group system
most important of all blood groups in transfusion medicine
blood group system in which people have antibodies in their blood to antigens that are absent from their RBCs without any prior exposure (transfusion or pregnancy)
Due to these antibodies, transfusion of incompatible ABO type may result in immediate lysis of donor RBCs
Anti-A/B antibodies are IgM
Transfusion of ABO-incompatible RBC units remains the leading cause of immediate hemolytic transfusion reaction (HTR) and HTR-related deaths reported by the FDA
After TRALI and TACO
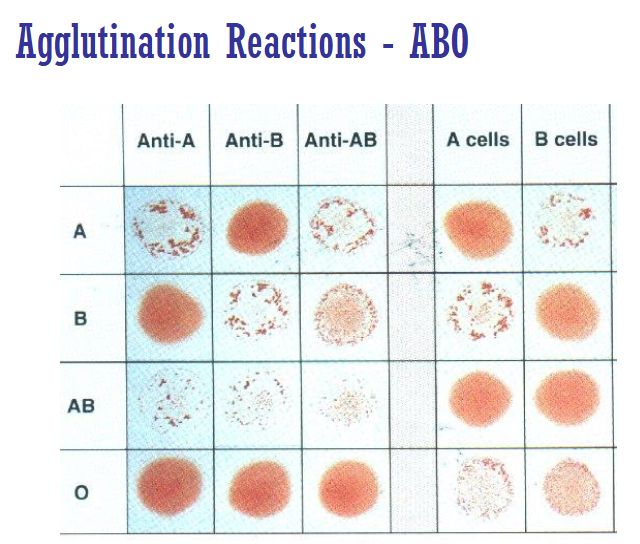
forward/front typing
test individual's RBCs with commercial antisera
looks for RBC antigens
reverse/back typing
tests patient plasma/serum with commercial RBCs
looks for antibodies against RBCs
relationship between forward and reverse typing?
inverse reciprocal relationship
the results of the two tests act as a built-in cross-check for accuracy
ex: someone with A antigen will have anti-B antibody
reagents for ABO testing
Anti-A, Anti-B, Anti-D, & Rh control for forward typing
A1 and B cells for reverse typing
A2 cells are also available (not routinely used)
T/F: reverse typing should be done on infants
false ; only forward typing should be performed
ABO antibody production is too low at birth
Most antibodies in cord blood are maternal
Reciprocal ABO antibodies are naturally occurring antibodies
Fully developed at 3 to 6 months after birth
ABO antibodies
Predominantly IgM (pentamer)
There are small quantities of IgG present
O blood type produce Anti-A, Anti-B and Anti-A,B
Anti-A,B is IgG and is a separate "cross-reacting" antibody
Activate complement, cause intravascular hemolysis
React best at room temperature (22 C) or colder
Produce strong direct agglutination reactions
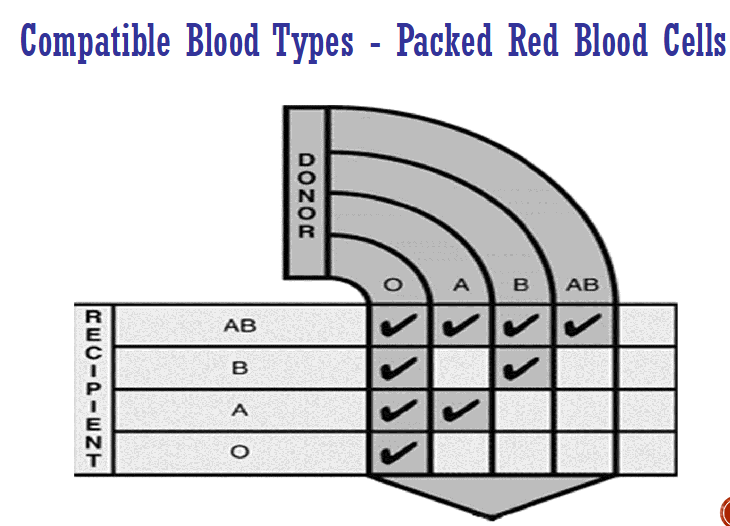
patient with type A blood has what type of antibodies? who can they donate/receive blood from?
antibodies: Anti-B
can donate blood to: type AB & A
can receive blood from: type A & O
patient with type B blood has what type of antibodies? who can they donate/receive blood from?
antibodies: Anti-A
can donate blood to: type AB & B
can receive blood from: type B & O
patient with type AB blood has what type of antibodies? who can they donate/receive blood from?
antibodies: none
can donate blood to: type AB
can receive blood from: type A, B, AB, O
patient with type O blood has what type of antibodies? who can they donate/receive blood from?
antibodies: Anti-A & Anti-B
can donate blood to: type A, B, AB, O
can receive blood from: type O
what blood type is known as the universal donor for RBC donation? universal recipient?
universal donor: type O (specifically O neg)
universal recipient type AB (specifically AB+)
**remember that it is the reverse for plasma !!!
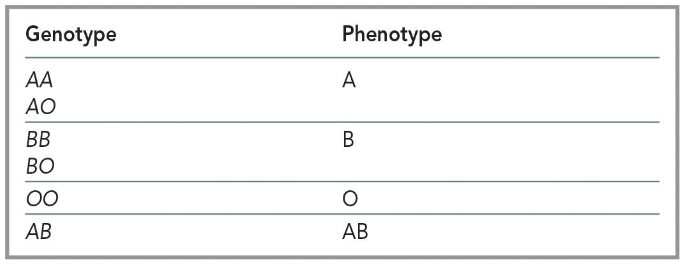
inheritance of ABO blood groups
based on Mendelian genetics
Codominant expression (A, B)
O gene is considered an amorph
No detectable antigen produced by the inheritance of this gene, only H precursor substance (H antigen)
O phenotype can only be produced by two O genes (OO), autosomal recessive
what chromosome is the ABO blood groups on?
chromosome 9
Three alleles: A, B, or O
A and B are co-dominant, A and B are dominant over O
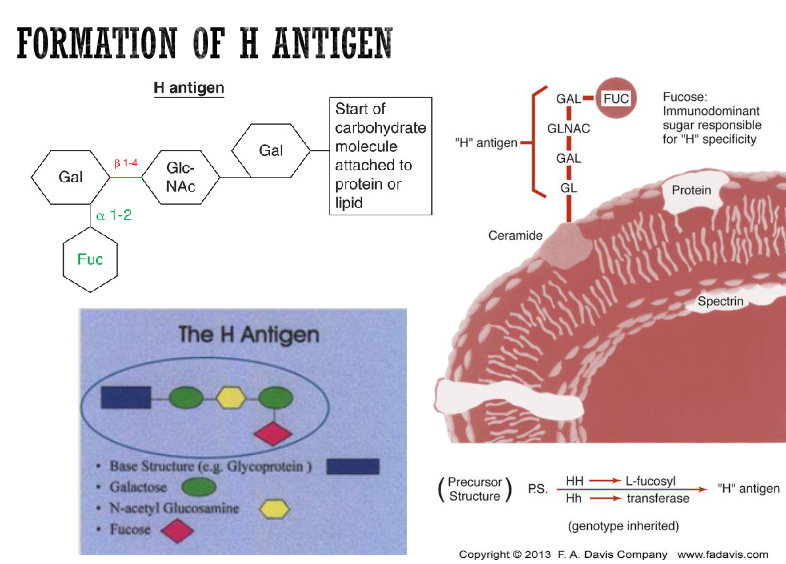
H gene (FUT1)
inherited independent of the ABO genes, must be present to form ABO antigens on the RBCs
Located on chromosome 19
Codes for L-fucosyltransferase
L-fucose = H antigen, which the A and/or B antigens are attached
HH genotype very common (99.99%)
Hh rare
hh extremely rare (Bombay)
H antigen is precursor substance for ABO
ABO immunodominant sugars
sugar that makes one antigen different from another antigen
ABO antigens reside on sugar molecules attached to outside of RBC membrane
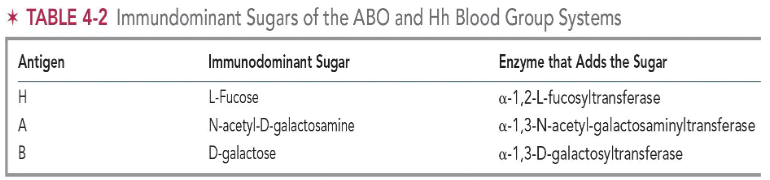
immunodominant sugar for H antigen + enzyme that adds the sugar
sugar: L-fucose / fucose
enzyme: α-1,2-L-fucosyltransferase
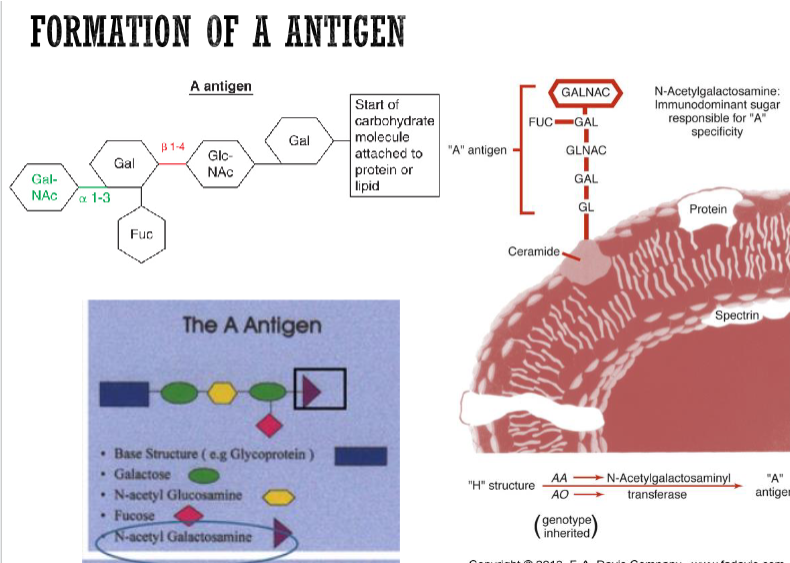
immunodominant sugar for A antigen + enzyme that adds the sugar
sugar: N-acetyl-D-galactosamine
enzyme: α-1,3-N-acetyl-galactosaminyltransferase
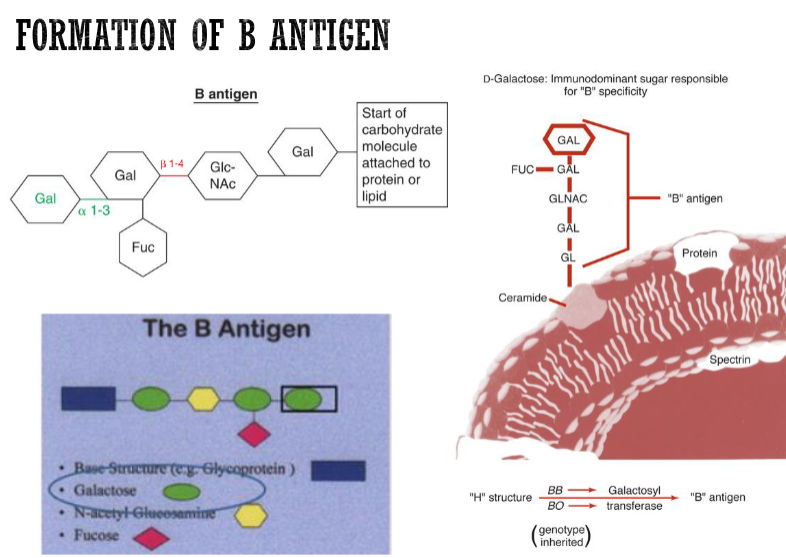
immunodominant sugar for B antigen + enzyme that adds the sugar
sugar: D-galactose
enzyme: α-1,3-D-galactosyltransferase
if H and A genes are present, what are the corresponding enzymes made? what are the antigens on the RBCs?
enzymes: α-1,2-L-fucosyltransferase + α-1,3-N-acetyl-galactosamyltransferase
antigens: H and A ; blood type would be A
if H and B genes are present, what are the corresponding enzymes made? what are the antigens on the RBCs?
enzymes: α-1,2-L-fucosyltransferase + α-1,3-D-galactosyltransferase
antigens: H and B antigens ; blood type would be B
if H and O genes are present, what are the corresponding enzymes made? what are the antigens on the RBCs?
enzymes: α-1,2-L-fucosyltransferase
antigens: H antigen ; blood type would be O
if H, A and B genes are present, what are the corresponding enzymes made? what are the antigens on the RBCs?
enzymes: α-1,2-L-fucosyltransferase + α-1,3-N-acetyl-galactosaminyltransferase + α-1,3-D-galactosyltransferase
antigens: H, A, and B ; blood type would be AB
ABO antigens
ABO antigens are carbohydrate structures
H antigens serves as the precursor substance for both A and B antigens
ABO antigen frequency and subgroups
The most common ABO blood group is O
Subgroups = genetic variation in ABO gene
e.g. A subgroup and B subgroup
formation of A, B, & H antigens
results from the interaction of genes at three separate loci: ABO, Hh (FUT1), and Se (FUT2)
These genes code for specific glycosyltransferases that add sugars to a basic precursor substance
H antigen is the precursor structure on which the A and B antigens are found
ABH antigens are integral parts of the RBC membrane, endothelial cells, platelets, lymphocytes, and epithelial cells
at what age are ABO antigens fully expressed in humans? what age are an individuals own ABO antibodies present?
ABO antigens are fully expressed at 2-4 years of age
ABO antibodies not present until 3 to 6 months
**RBCs of newborns only carry 25-50% of antigens found on adult RBCs—forward typing will be weaker
glycoproteins
RBC carbohydrate/sugar molecules that carry A, B, H antigens attached to protein
ABO and H blood group system carbohydrate chains are composed of hexoses
type I precursor substances
found in gut lining, plasma, and secretions
precursor substances are built off of the type I precursor chain (aka the β-1,3 connection in red—see image)
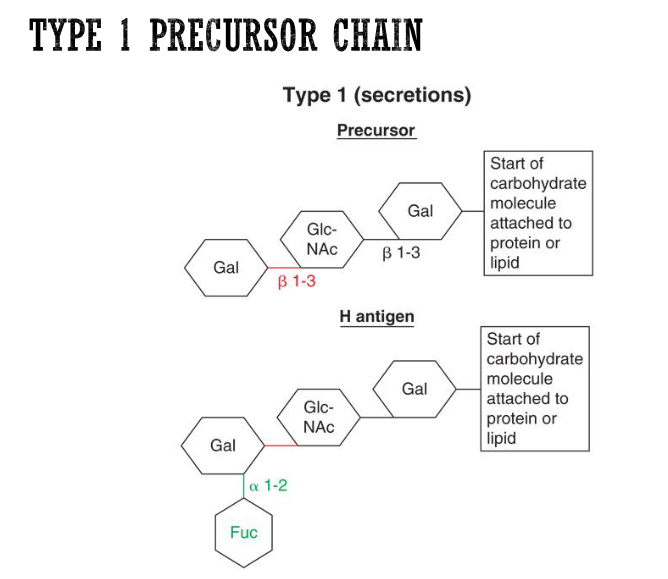
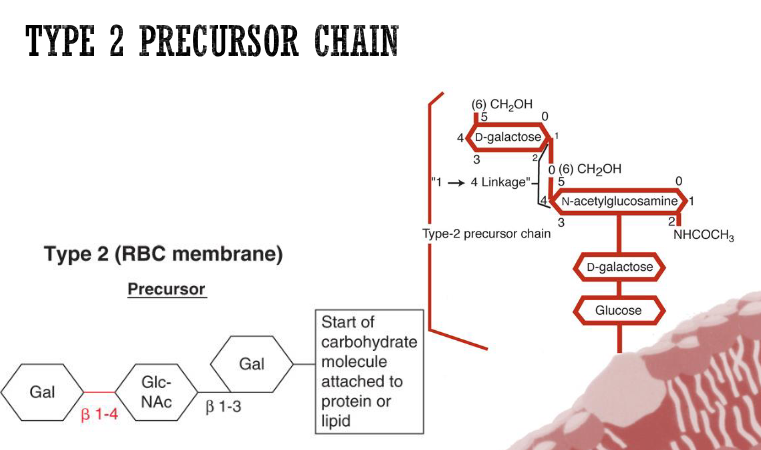
type 2 precursor substances
found in A, B, H antigens ON RBC MEMBRANE
build off type 2 precursor chains (aka the β-1,4 connection in red—see image)
molecular genetics of ABH antigens
Investigation of ABO alleles, epitope structures, and exons
ABO gene located on chromosome 9 and consists of seven exons
Cis-AB
Very rare genotype
Inheritance of both A and B genes from one parent on same (cis) chromosome 9
O gene inherited from the other parent
Offspring inherit 3 ABO genes instead of two
formation of ABH soluble antigens
H (FUT1) and Se (FUT2) genes are closely linked and located on chromosome 19
Se gene must be inherited to form the ABH antigens in all body secretions
ABH-soluble antigens found in all body secretions
80% of the random US population are known secretors
SeSe, Sese
secretors
People who have ABH antigens in their body fluids
Inheritance of Se (FUT2) gene codes for production of transferase that modifies the type 1 precursor substance in secretions = forms H substance
H substance can be modified to express A and B substance in secretions (e.g. saliva)
Group A = secrete glycoproteins carrying both A and H antigens
non-secretors
People who are sese do not produce any A, B, or H antigen in their secretions
Make up ~20% of random US population
presence of Lewis antigens can help determine whether an individual is a secretor or non-secretor
Presence in secretions is dependent on ABO and secretor genes inherited
ABH substances in secretions vs ABH antigens on RBCs
A, B, and/or H soluble substances in secretions are glycoproteins
A, B, and/or H antigens on RBCs are glycolipids, glycoproteins, or glycosphingolipids
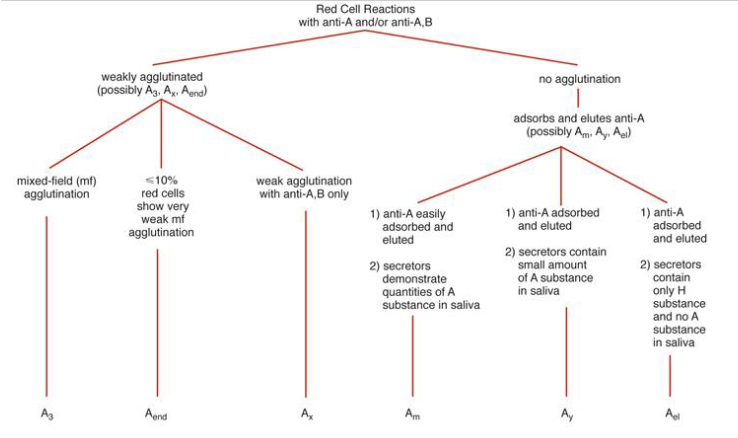
ABO subgroups
phenotypes that show weaker and variable serological reactivity with the commonly used human polyclonal Anti-A, Anti-B, and Anti-A,B reagents
Common subgroups of A
A1 and A2 antigens
Other subgroups: A3, Ax, Ael, and Am → ID by molecular analysis
Subgroups of B extremely rare
B3, Bx, Bel and Bm
Monoclonal typing reagents used routinely in ABO grouping tests currently
Donors with very weak A antigen expression may be mistyped as group O
type A subgroups
First described in 1911 by von Dungen
A1: react with Anti-A, and anti-A1
A2: react with Anti-A only
Differences between A1 and A2 are both quantitative and qualitative
80% of all A (or AB) are A1 (or A1B)
20% of all A (or AB) are A2 (or A2B)
1-8% of A2 individuals
A subgroups are generally more common than B subgroups
how can you differentiate between A1 and A2 subgroups?
use anti-A1 lectin reagent
Anti-A1 lectin agglutinates A1 or A1B cells but does not agglutinate A2 or A2B cells
characteristics of A1 allele
A1 transferase has proline at amino acid 156
Elicits higher concentration of transferase
Transferase is more efficient
Converts almost all of H to A1
810,000 to 1,170,000 antigen sites/RBC
characteristics of A2 allele
A2 transferase has leucine at amino acid 156 and single base deletion
Lower concentration of transferase
Less efficient transferase
240,000-290,000 antigen sites/RBC
(lectin reagents) Dolichos biflorus
aka anti-A1 lectin
agglutinates A1 or A1B
(lectin reagents) Bandeiraea simplicifolia
aka anti-B lectin
agglutinates B cells
(lectin reagents) Ulex europaeus
aka anti-H lectin
agglutinates O cells (H specificity) and other ABO blood groups depending on the amount of H antigen available on RBC surface
The amount of H antigen on RBCs of different blood types:
O > A2 > B > A2B > A1 > A1B
weak A subgroups
include: A3, Ax, Aend, Am, Ay, and Ael
Most often discovered via ABO discrepancy
Unexpected reactions in the forward and/or reverse typing
Varying expression of four characteristics
Decreased number of A antigen sites per RBC
Degree of agglutination by anti-A,B
Increased detectability of H antigen
Presence of absence of anti-A1 in serum
weak B subgroups
Very rare and less frequent than A subgroups
Usually recognized by variations in the strength of the reaction using anti-B and anti-A,B antisera
Result of alternative alleles at the B locus
Serological techniques characterize B subgroups in the following categories
B3, Bx, Bm, Bel
criteria for differentiation of weak B phenotypes
Reactivity with anti-B, anti-A,B and anti-H
Presence or absence of ABO antibodies
Absorption-elution with anti-B
B substance in saliva
Molecular testing
bombay phenotype
First reported by Bhende in 1951 in Bombay, India
Inheritance of a double dose of the h gene, producing the genotype hh
No H antigen made
ABO genes cannot be expressed
ABH antigens cannot be formed
Anti-A, Anti-B, Anti-A,B, and anti-H present
if an individual had the genotype hh and sese, would they have RBC antigens and ABH substances in their secretions?
nope
lacks H antigen to attach immunodominant sugars for a blood type
lacks Se gene for ABH to be present in secretions
para-bombay phenotype
hh and SeSe/Sese genotypes
H, A, and/or B antigens in secretions and plasma
bombay phenotype & testing
Fail to react with anti-A, anti-B, anti-A,B and anti-H antisera
In blood group testing, the Bombay would phenotype as an O blood group
Unlike the anti-H found occasionally in the serum of A1 and A1B individuals, the Bombay anti-H can often be potent and reacts strongly at 37 C
IgM antibody → can bind complement → cause intravascular hemolysis
Can only be transfused with another Bombay (Oh)
list the blood types in order of most to least H antigen present on the RBCs
O > A2 > B > A2B > A1 > A1B
Greatest amount of H antigen found on O cells
Least amount of H found on A1B cells
two transferase are present to attach sugar onto the H antigen, meaning that almost all H antigen is converted into A1/B antigen
anti-H antibody
Anti-H is occasionally found in the A1 and A1B serum
H antigen well hidden by N-acetyl-D-galactosamine
Reminder = conversion of H antigen into A antigen
Anti-H naturally occurring IgM cold agglutinin that reacts best below RT
Can cause intravascular hemolysis
Possible problems in antibody screening procedures
Use of anti-H antisera (anti-H lectin)
bombay phenotype transfusion considerations
Only blood from another Bombay individual will be compatible
Underlying molecular defect of the Bombay phenotype
ABH antigens & antibodies in disease
Hypogammaglobulinemia
Leukemias, e.g. CLL (absence of isoagglutinins)
Depress antigen strength
Other leukemias with chromosome 9 translocations
Any hemolytic disease inducing stress hematopoiesis (e.g. thalassemia)
"Acquired B" phenomenon in group A1 individuals
Group A1 RBCs absorb bacterial-like polysaccharide = reacts with anti-B reagent
ABO hemolytic disease of the fetus and newborn (HDFN)
Maternal IgG antibodies cross placenta causing hemolysis of fetal RBCs with corresponding antigen
Mainly occurs when mother is blood group O (anti-A,B = IgG) and fetus is blood type A or B
May occur with the first pregnancy
More common than Rh HDFN but not as severe
Common cause of jaundice in newborn
Spherocytes observed on smear