Bone Tissue
1/87
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
88 Terms
the skeletal system
206 bones form the structural framework for the body
the bones, along with their cartilages, make up this system
bone
living tissue, with each individual bone is an organ
skeletal system function
bones support the soft tissues
provide attachment the sites for muscles, to assist them in movement
protect internal organs
stores and release of minerals (calcium, phosphorus)
triglyceride storage (yellow marrow)
hemopoiesis
skeletal tissue
compact bone
spongy bone
ligaments
tendons
compact bone
dense connective tissue
white
smooth solid
spongy bone
internal to compact bone
houses bone marrow
ligaments
dense regular connective tissue
bone to bone
tendons
dense regular connective tissue
bone to muscle
classification of bones
long bones
short bones
flat bones
irregular bones
long bones
length > width
most common
vary in size
short bones
length is approx equal to width
carpals and tarsals
includes sesamoid bones (embedded within a tendon)
flat bones
flat and slightly curved
scapular and skull bones
surface for muscle attachment
irregular bones
elaborate complex shapes
vertebrae
gross anatomy of long bones
diaphysis
epiphysis
metaphysis
epiphyseal plate
epiphyseal line
periosteum
outer fibrous layer
inner cellular layer
articular cartilage (hyaline cartilage)
medullary cavity
endosteum
diaphysis
provide leverage and weight support
epiphysis
end of long bone
resists stress from many direction
forms joints
houses spongy bone
has a proximal and distal end
metaphysis
between diaphysis and epiphysis and contains
epiphyseal plate
epiphyseal line
epiphyseal plate
less than 21yo
thin layer of hyaline cartilage for continued length growth
epiphyseal line
greater than 21yo remnant of plate
periosteum
covers outer surface except areas covered by articular cartilage
two layers
outer fibrous layer
inner cellular layer
outer fibrous layer
dense irregular connective tissue
protects bone
anchors blood vessels and nerves
attaches tendons and ligaments
inner cellular laye
composed of osteoblasts and osteoclasts
articular cartilage (hyaline cartilage)
covers joint surface of epiphysis
reduces friction
absorbs shock
medullary cavity
hollow cylindrical space
houses red and yellow bone marrow
endosteum
lining the medullary cavity, an incomplete layer of cells
vascular membrane of connective tissue
red bone marrow
hemopoietic
where red blood cells (RBCs), white blood cells, and platelets are produced
also has reticular connective tissue and fat
yellow bone marrow
replaces red bone marrow in long bones
contains fat (adipose tissue)
can serve as source of energy
blood supply and innervation
bones are highly vascularized, with vessels enter from periosteum
nutrient foramen allows entry of a nutrient artery and vein
nerves accompany the blood vessels to innervate the bone, periosteum, endosteum, marrow
short, flat, and irregular bones
external surface is still compact bone
interior is entirely spongy bone (diploe)
no medullary cavity
ossificaiton
formation and development of bone tissue
8th though 12th week of embryonic development
2 types:
intramembranous ossification
endochondral ossification
intramembranous ossification
primarily in flat bones of skulls
begins when mesenchyme becomes thicker and condensed
intramembranous ossification steps
ossification centers form
osteoid undergoes calcification
formation of trabeculae
development of the periosteum
endochondral ossification
development of most bones including long and short bones, the bones of the axial (ribs and vertebrae), and the appendicular skeleton (e.g. upper and lower limbs)
requires the use of a cartilage model
endochondral ossification steps
fetal hyaline cartilage model develops
growth of the cartilage model
development of the primary ossification center
development of medullary cavity
development of secondary ossification centers
formation of articular cartilage and epiphyseal plate
factors affecting bone length change
genetic factors determine bone shape and size
factors that alter the mineralization process or the production of organic matrix
hormones
hormones that promote bone growth
growth hormone: epiphyseal plate
insulin like growth factors: epiphyseal plate
thyroid hormone
sex hormones
thyroid hormone
increase metabolic rate of bone cells
sex hormones (estrogen, testosterone)
increase cartilage growth and bone formation—epiphyseal plate
hormones that inhibit bone growth
glucocorticoids
serotonin
glucocorticoids
impairs growth at epiphyseal plate
serotonin
osteoprogenitor cells stop differentiating
parathyroid hormone (PTH)
secreted by the parathyroid galnds
PTH increases blood Ca2+ level by activating osteoclast activity
PTH stimulates formation of calcitriol (active form of vitamin D), a hormone that promotes absorption of Ca2+ from GIT into the blood
calcitonin (CT)
secreted by the parafollicular cells of the thyroid glands
CT inhibit the activity of osteoclasts
promote Ca2+ deposition into bones thus decrease blood Ca2+ level
bone cell types
osteogenic cell
osteocyte
osteoblast
osteoclast
bone connective tissue
composed of both cells and extracellular matrix
osteogenic cell (osteoprogenitor cell)
stem cells derived from mesenchyme
produce osteoblasts
found in periosteum and endosteum
mesenchyme
embryonic connective tissue
osteoblasts
side-by-side on periosteum
abundant rough ER and golgi apparatus
secretes osteiod (semisolid bone matrix)
become entrapped from crystal deposition
differentiates into osteocytes
no mitosis
osteocytes
mature bone cells that maintain bone matrix
detects mechanical stress on bones
signals to osteoblasts to make new bone matrix at surface
no mitosis
osteoclasts
found on bone surface
phagocytic cells—multinuclear
from cells similar to monocytes and macrophages
break down bones for resorption
resorption lacuna
resorption lacuna
depression or pit on bone surfaces where osteoclasts are located
bone matrix
the nonliving, mineralized extracellular substance that forms the structural framework of bone tissue
made of organic and inorganic portions
organic
osteoids from osteoblasts
inorganic
salt crystals
osteoid
proteins secreted by osteoblasts
osteoid composition
collagen
semi-solid ground substance
proteoglycans (chondroitin surface)
glycoproteins
osteoid function
components five tensile strength
resist stretching and twisting
flexibility
inorganic portion
salt crystals
deposit along long axis of collagen fibers
rigidity and inflexibility—compressional strength
salt crystals
primarily calcium phosphate
calcium hydroxide
hydroxyapatite (contains calcium and phosphate)
sodium, magnesium, sulfate, fluoride
bone formation
requires vitamin D and C
osteoblast secretes osteoid
calcification
ions precipitate out of solution
osteoblasts then become trapped, turning into ostecytes
calcification
osteoid hardens as hydroxyapatite crystals deposit in bone matrix (in and around collagen)
bone reabsorption
the balance between osteoblast and osteoclast activity is what causes subtle bone remodelling
bone matrix destroyed
osteoclasts secrete proteolytic enzymes digests collagen proteoglycans
hydrochloric acid dissolved mineral parts
calcium and phosphate enter blood
bone remodeling
breakage
resorption
reversal
formation
osteoporosis
low bone density, “porous bones”
over bony reabsorption, with inadequate formation of new bone
found in elderly, or postmenopause due to low estrogen levels
paget’s disease of the bone
disordered bony remodeling
first overactive osteoclasts
then osteoblasts lay down large, weak, brittle bones prone to fracture
osteons (haversian system)
basic functional and structural unit
parallel to diaphysis of long bone
allows for great resistance to stresses applied in many directions
central canal
center of osteon
parallel to osteon
contains blood vessels and nerves
concentric lamellae
rings of bone connective tissue
collagen fibers at 90 degree angles
strength and resilience
osteocytes
cell that maintains bone matrix
found in small spaces between adjacent lamellae
space is called lacunae
canaliculi are interconnecting channels—extend from each lacunae
connect lacunae and central canal
house osteocyte cytoplasmic projections
permit intercellular contact and communication
perforating canals
contain blood vessels and nerve similar to central canal
perpendicular to central canal
connects central canals
interstitial lamellae
between osteons
no central canal
spongy (cancellous) bone
no osteons
trabeculae
parallel lamellae
trabeculae
open lattice of narrow rods and plates
bone marrow fills in between
cartilage
strong, flexible, and semi-rigid supporting tissue
avascular, nourished by long ranged diffusion
2 types of growth
interstitial
appositional
certain bone growth depends on cartilage growth
interstitial cartilage growth
chondrocytes lay down matrix in existing tissue to increase length
mainly in childhood and adolescence
appositional cartilage growth
chondroblasts lay down new matrix on surface to increase width
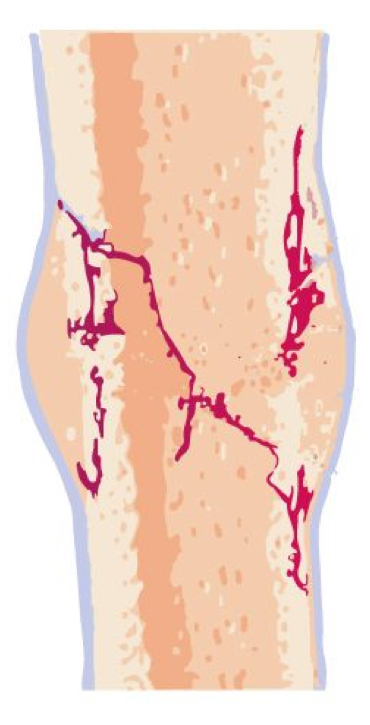
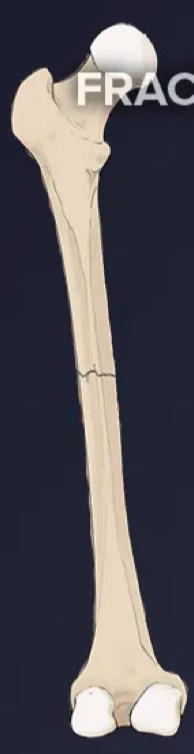
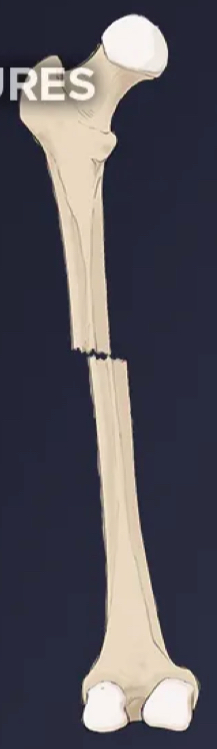
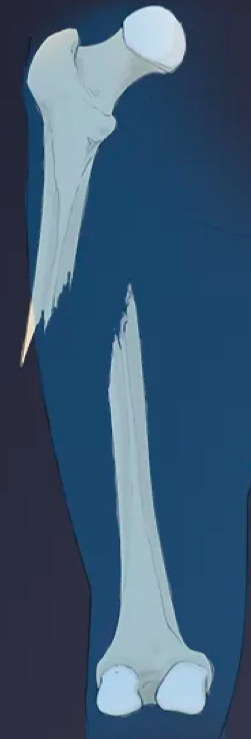
bone fractures
transverse (nondisplaced)
transverse (displaced)
compound
oblique
comminuted
greenstick
transverse (nondisplaced
transverse (displaced)
compound
oblique

comminuted

greenstick

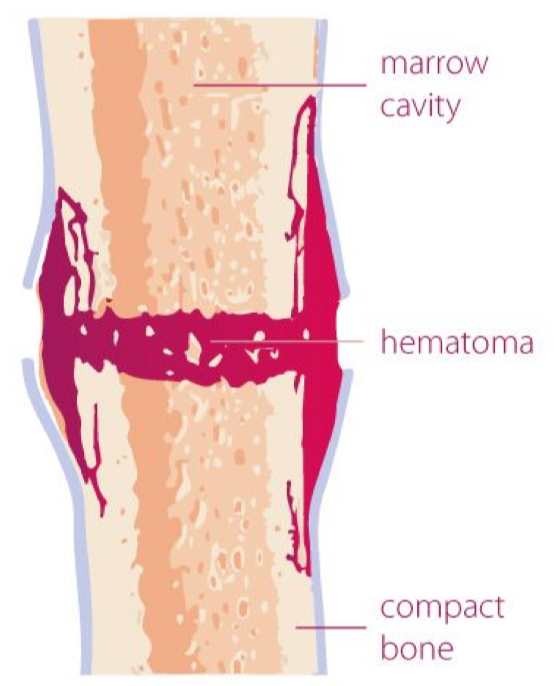
hematoma formation
blood vessels in the broken bone tear and hemorrhage, resulting in the formation of clotted blood, or a hematoma, at the site of the break
the severed blood vessels at the broken ends of the bone are sealed by the clotting process
bone cells deprived of nutrients begin to die
0-2 weeks
fibrocartilaginous callus formation
within days of the fracture, capillaries grow into the hematoma, while phagocytic cells begin to clear away the dead cells
fibroblasts and osteoblasts enter the area and begin to reform bone
the repair tissue between the broken bone ends, the fibrocartilaginous callus, is composed of both hyaline and fibrocartilage
some bone spicules may also appear at this point
2-3 weeks
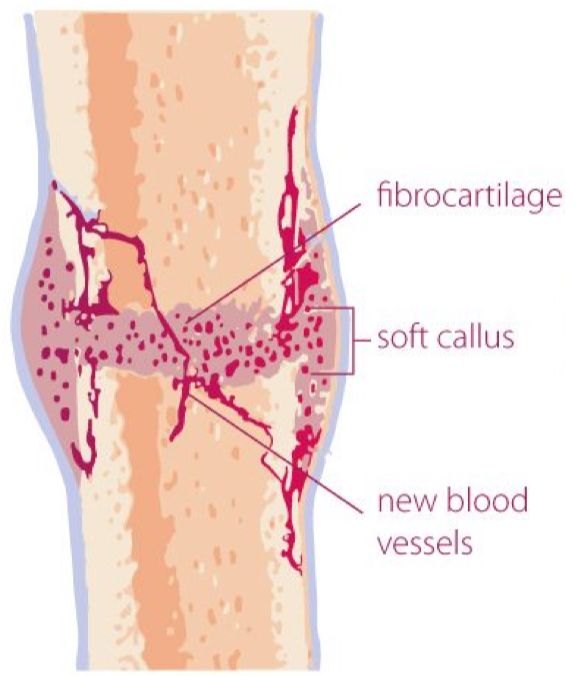
fibroblasts
produce collagen fibers that connect the broken bone ends, while osteoblasts start to form spongy bone
bony callus formation
the fibrocartilaginous callus is converted into a bony callus of spongy bone
it takes about two months for the broken bone ends to be firmly joined together after the fracture
similar to the endochondral formation of bone when cartilage becomes ossified;
osteoblasts, osteoclasts, and bone matrix are present
3-6 weeks
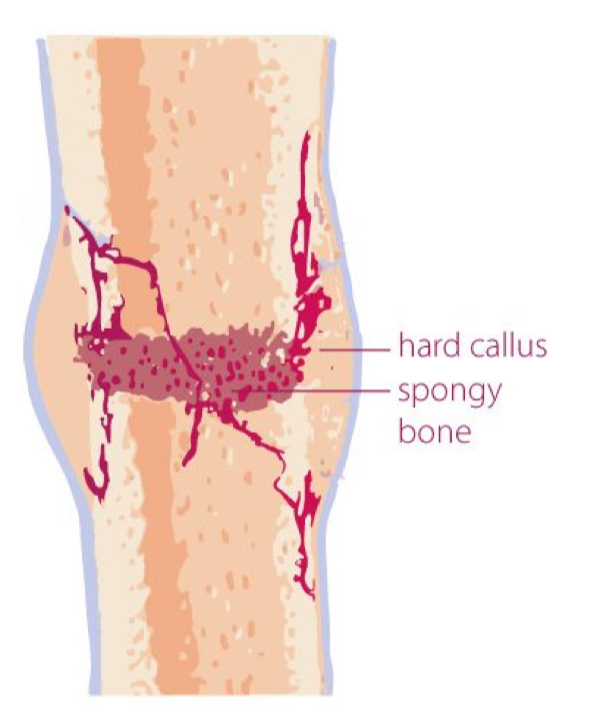
bony remodelling
the bony callus is then remodeled by osteoclasts and osteoblasts, with excess material on the exterior of the bone and within the medullary cavity being removed
compact bone is added to create bone tissue that is similar to the original, unbroken bone
this remodeling can take many months
the bone may remain uneven for years
8 weeks-2 years