Rad protection Unit 3 (both sets)
1/92
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
93 Terms
NCRP occupational exposure limits
annual effective dose
50 mSv
does not include medical or background radiaiton exposure
cumulative effective dose
age in years x 10 mSv
ALARA
concept
as low as reasonably achievable
collimate
technique
shielding
minimize repeats
methods to reduce exposure
avoid repeat exposure
collimation- increase (make light field smaller)
cumulative timer
highest occupational exposures are: fluoro, portables, and OR
stand 90 degrees from the patient
filtration
non useful low energy photons are removed, less scatter
distance from patient…
patient is a source of scatter radiation
3 feet from the patient (1 meter), the scatter radiation is approximately 1/1000 the intensity
example: if patient exposure is 20 mGy, technologist standing 1 meter at 90 degrees would be exposed to 0.02 mGy
methods to reduce your exposure
protective apparel
lead aprons and protective barries
proper exposure factors
controls scatter (lower kVp, less scatter produced)
correct image acquisition
reduces repeats
high speed image receptors
high speed systems use smaller exposures which causes less scatter
beam limiting devices
reduces scatter
protection of pregnant personnel
should be able to continue duties without interruption of employment
voluntary declaring vs. not declaring
couseling
second “baby badge” is issued worn at waist level
to reduce risk of leukemia or other malignancies
0.5 mSv in one month
5 mSv for the entire pregnancy
must read and sign a form acknowledging counseling
if wearing a lead apron, the 2nd badge is worn inside the apron at waist level
baby badge has a separate reading on the dose report
maternal tissue decreases fetus dose by 30%
work schedule rotation
does not necessarily have to be done
types of radiation
primary radiation
scatter radiation
leakage radiation
primary radiation
useful beam
emerges directly from the tube collimator
scatter radiation
highest does to technologist
primary beam passes through matter and goes in various directions
leakage radiation
escapes the tube housing
protective structural shielding
usually lead or concrete
barriers
primary protective barrier
secondary protective barrier
primary protective barrier
located perpedicular to the primary beam travel (undeflected line of travel)
prevents direct or unscattered radiation from reaching personnel and general public
for 130 kVp of peak energy a 1/16 (~1.6mm)inch of lead or lead equivalent and extends 7 feet (2.1m) upward from the floor if the tube is 5-7 from the wall (1.5-2.1m)
secondary protective barrier
any wall or barrier that is never hit by the primary beam
protects agaist scatter and leakage radiation
1/32 inch of lead or lead equivalent (~0.8 mm)
overlaps the primary barries by ½ inch (~1.3 mm) and extends to the ceiling
protective device requirements
lead apron
0.5 mm lead (Pb) for fluroscopy, AIR, or operating systems aboe 100 kVp (NCRP #102)
protects from 95-99% of scattered radiation
gloves
minimum of 0.25 mm lead (Pb)
neck and thyroid
must be at least 0.5 mm lead (Pb)
protective eyeglasses
0.35 mm lead (Pb) to protect the eyes
protective tube housing
lead lined metal that protects personnel and patients from leakage and off focus radiation
cannot exceed 1 mGy per hour at 1 m away from housing
no one should be touching the xray tube housing during an exposure
protection during fluoroscopy
proper position to be standing
avoid high scatter areas
try to stand behind the physician/ radiologist or RA
90 degrees from the patient, away from the source
wrap around lead
need to move around the room to obtain supplies
should be thyroid shield
unprotected areas are getting 10-20x more exposure
collimation
filtration
technical factors
high speed image receptors
correct image acquisition
appropriate skin to source distance
cumulative timer
rotational scheduling of personnel
personnel must wear the badge on the outside of the lead apron at collar level
remote control fluoro units
can perform the study from the control booth and enter room only when necessary
scatter protection barrier in fluoro
protective curtain
0.25 mm lead equivalent
gonadal protection
bucky slot cover
0.25 mm lead equivalent
protection in mobile radiogrpahy
cord length should be long enough to stand 6 feet (2m) from the patient
stand 90 degrees from the patient
use distance as a means of protection
wear protective shield
yell “x-ray” before taking exposure
do not hold the image receptor
use cassette holders, pillows, sponges, or even a box of gloves
protection in C-arm fluoroscopy
proper position to be standing
in a lateral view, on the side of the patient away from the x-ray tube
protective shields and radiation monitros for all personnel
properly orient the c-arm with the image intensifier on top
minimise beam on time
position the image intensifier as close to the patient as possible to lower the beam intensity needed
advanced interventional radiology (AIR) protection
low dose fluoroscopy mode/ pulse fluoro
collimation
last image hold
shortening duration of studies
extremity monitors
rings- NCRP annual limits to 500 mSv
imaging personnel protection guidelines
technologist should never stand in the path of the primary beam
if holding is necessary, try to utilize a non-occupationally exposed person or immobilization
pregnant technologist technologist are never to hold a patient for an exposure
exposures should never be made witht the doors to room open
cardinal principles of radiation protection
Time- amount of exposure is directly proportional to duration of the exposure
Distance- most effective means of protection, it is indirectly proportional
Shielding- absorbs most of the energy of scatter radiation
~ 85% effectiveness
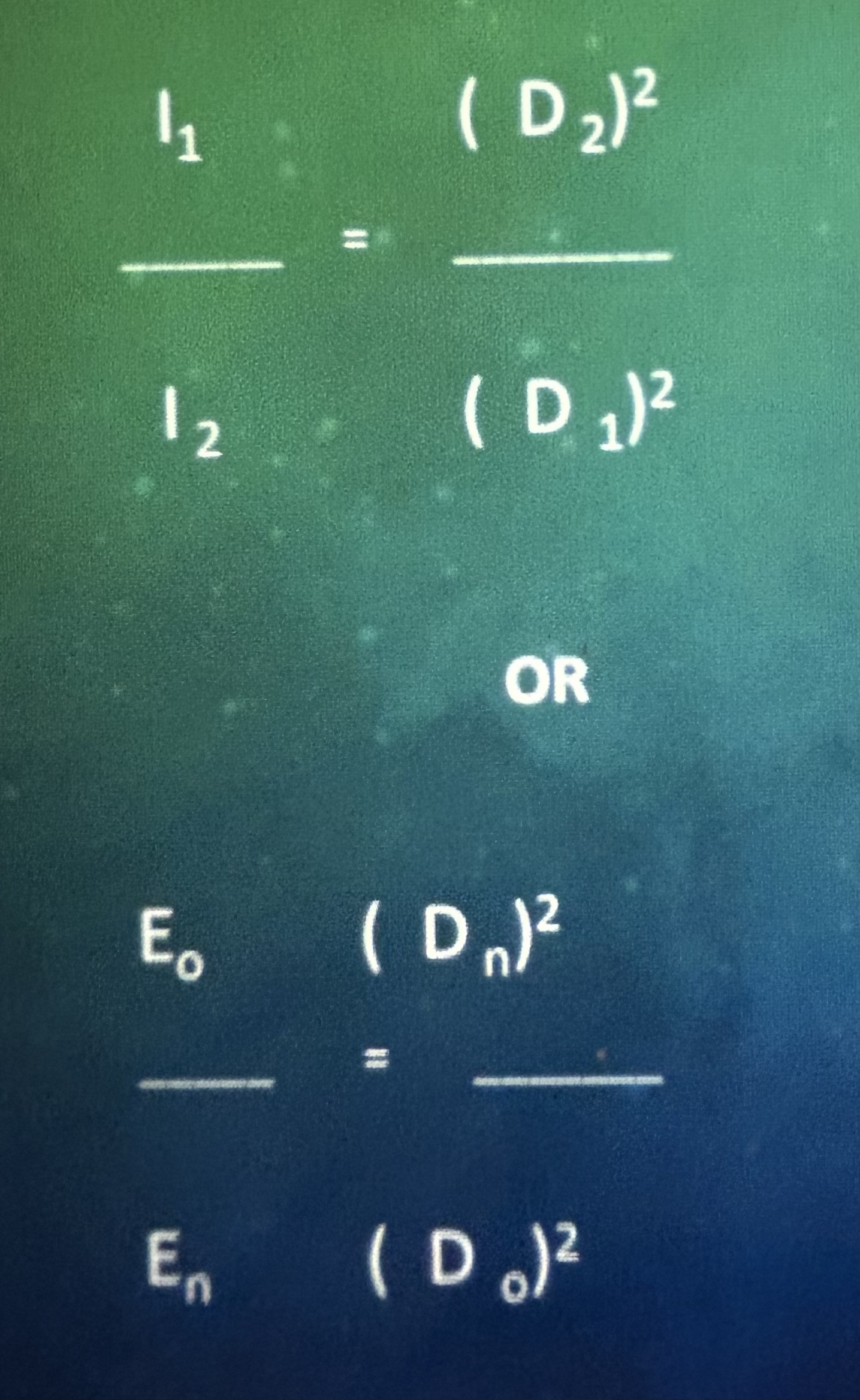
Inverse square law (ISL) equation
diagnostic protection design
workload (W)
radiation on time during a week
mAs/week or mA- minute/week
Use (U)
amount of time the bean is directed at the structure'
takes into account primary or secondary radiation
occupancy (T)
time that the area is occupied behind a barrier
waiting room
empty courtyard
distance (D)
distance from the source to the structure
calculating barrier requirements
W x U x T
needs to be calculated for every barrier in an x-ray room
areas of the department
controlled- occupied by workers who are trained and wearing monitoring devices; maximum permitted equivalent dose is 100 mrem per week
uncontrolled- occupied by the general public; maximum permitted equivalent dose is 2 mrem per week
waiting rooms
hallways
bathrooms
stairways
radiation area sign posting
radiation symbol that is magenta, purple or black on a yellow background
radiaiton hazard (rad Onc and NM)
high radiaiton area
very high radiaiton area
Airborne radioactivity
radioactive materials
warning signs
signs that indicate the room is in use
holistic patient care
treat the patient as a whole person rather than a body part
makes patient feel more respected comfortable and more willing to cooperate
effective communication: verbally and body language
introduce yourself
address the patient properly
ease the patient’s stress and anxiety
show understanding and dignity
provide clear and concise intructions
increase their cooperation
give the patient time to ask questions
gain their trust
tell them if there is discomfort or pain in volved
strange sensations
be professional, be present, watch body language
help to make the procedure successful
reduces repeat exposure
patient motion
involuntary
voluntary
involuntary motion
caused by muscles, not controllable
heart
digestive
chills
tremors
spasms
pain
active withdrawal
corrected by decreasing exposure time and increasig imaging receptor speed
voluntary motion
controlled motion
sometimes there can be lack of that controlled motion due to:
patient’s age
breathing patterns
anxiety
physical or mental discomfort
fear of exam/prognosis
mental instability
corrected by gaining patient cooperation and use of proper immobilization
immobilization
piggostat
papoose/octostop
sponges (radiolucent) and sandbags (radioopaque)
mummy wrap/ bunny wrap
tape
velco straps
radiolucent plexiglass
having a non-radiology employee helping to hold
beam limiting devices
limits the primary beam to a smaller area
decreased exposure by reducing the amount of tissue that is exposed to radiation
reduces scatter
types of beam limiting devices
aperture diaphragm
cones
collimators
aperture diaphragm
flat lead with shape and size cut into it that is placed below the window
rectangular
most commot
square
round
reduces scatter
cones
circular metal cylinders connected to the tube housing that limits the size of the beam
can be flared or straight
can be telescoped (10-12 inches) for smaller exposure area
called extensive cylinders
have mostly been replaced by collimators
mostly used in dental radiography but can be used for the heel, skull and spine imaging
collimators
light-localizing variable aperture rectangular collimator
most versatile beam restriction
can change size
should not be opened larger than the size of the image receptor or body part imaging
post shuttering- part of ASRT Practice Standards
can reduce exposure by 20-30%
careful not to over collimate which causes repeat images
there are 2 sets of shutters in a collimator that are 90 degrees from one another
near (upper)
located close to the window
reduces exposure from off focus radiation
far (lower)
located closer to the light source
confines the beam to the area of interest
skin sparing (collimators)
minimizes skin exposure by requiring a 15 cm distance from the skin to the collimator
can be achieved with spacer bars mounted on the tube
positive beam limitation (PBL)
electronic sensors in the bucky that senses the image receptor size that you are using and opens the light field to that size
can be slits or pegs
reduces user errors by matching the light field to the image receptor size
also known as automatic collimation
regulatory guidelines require this to be within 2% accuracy
filtration
hardens the beam by cleaning up the low energy (longer wavelength) x-rays
reduces the skin and superficial exposure to the patient
decreases patient’s absorbed dose because the remaining photons are higher energy (shorter wavelength)
lower energy photons (which were removed) would be more likely to be totaly absorbed and provide no detail to the image
total filtration built into the housing is 2.5 mm Al equivalent for units operating above 70kVp
2 types of filtration
inherent- 0.5 mm Al equivalent
glass envelope, insulating oil, and glass window
added- 2.0 mm Al equivalent
sheets of Al added outside the glass window above the collimator shutters
accessible by pervice person
can be changed as the tube ages
mobile and fluoroscopy units also require 2.5 mm Al equivalent
NCRP #102- list minimum required filtration for x-ray equipment
Radiation Control for Health and Safety Act of 1981 states:
that a diagnostic x-ray beam must always have adequate filtration
to verify that a machine has adequate filtration, the HVL QC test (half value layer) must be measured
measure beam quality or effective energy of the beam
measured at least once a year by physicist or if the tube is replaced or repairs are made
HVL (half value layer)
insufficient HVL test could mean improper filtration
example
exposure from the tube is 350 C/kg
what will be the exposure for:
1 HVL (50%)
175 C/kg
2 HVL (25%)
87.5 C/kg
3 HVL (12.5%)
43.75 C/kg
4 HVL (6.25%)
21.8 C/kg
TVL (tenth value layer)
thickness that will decrease the intensity of the beam by 1/10th
shielding
April 2019- American Association of Physicists in Medicine (AAPM)- statement that shielding of patient gonadal or fetal shielding during diagnostic imaging should be discontinured
CARES committee (communicating advances in radiation education for shielding)
radiosensitive organs
lens of the eye
breasts
reproductive organs
2 types
gonadal
specific area
gonadal shielding
should be used if the gonadal area is within 5cm of the collimation field
could use unless covering the area of interst
first step in gonadal protection is proper collimation
due to the anatomical location, females recieve 3x more exposure than males
if used, appropriate shield placement can reduce the exposure to
females by 50%
males by 90-95%
flat shields
most effective in the AP or PA recumbent positions
shadow shields
careful to place properly or repeat image could be caused
not suitable during fluoro
shaped shields
contoured to enclose the male reproductive organs
can be placed by the patient
can not be used during PA projections
clear shields
transparent lead-plastic material
lap shields (half)
covers only the front or back half of the patient
attached with a velcro strap or on wheels
specific area shields
eyes
breast
thyroid
gloves
compensating filters
used when x-raying a part that has varying thickness to reduce dose and provide a uniform density across the image
decreases the entrance skin exposure (ESE)
constructed of aluminum or lead-acrylic that is attached to the bottom of the collimator
types of compensating filters
wedge filter
used for a foot and spines
trough filter or bilateral wedge
used on chest x-rays
thicker on both sides and thin in the middle
ferlic
hips
boomerang
shoulders
kVp (kilovoltage peak)
maximum possible energy of a photon that exits the x-ray tube, this is a unit selected on the operating console
indirectly proportional to patient exposure
mA (milliamperage)
measurement of x-ray tube current or the number of electrons crossing the tube from cathode, this is a unit selected on the operating console
directly proportional to patient exposure
mAs (milliampere seconds)
controls the amount of radiation produced by the x-ray tube
mA x seconds= mAs
directly proportional to patient exposure
AEC (automatic exposure control)
the cells that are selected on the operating console that will automatically select the mA according to cell selection and body part
exposure index (EI)
the number that is found on the image after processing that measures receptor exposure
exposure index should be in range for the equipment parameters to be a good diagnostic image
under exposure will cause quantum noise (grainy appearance) and should be repeated
over exposure is most cases will appear as a good image
in extreme cases it will cause saturation and should be repeated
use proper exposure factors
makes an optimal image with minimal dose possible
sufficient penetration
higher kVp, lower mAs for body part
when setting manual technique, measure the patient for accuracy'
reliable technique chanrts
AEC (automatic exposure control)
sets the appropriate mA for the body part being x-rayed by selecting cells
image receptor speed
increase in image receptor speed decreased patient exposure but decreases sharpness
digital radiography acts as a 200 or 400 speed image receptor
correct processing (image acquisition)
inadequate processing of image results in repeats
radiographic grids
rule of thumb is to use a grid when part thickness is over 10cm at 60kVp or higher
removes scatter photons that come from the patient before they reach the image receptor
improves the contrast and detail of the image
grids increase patient dose but improves the quality of the image which provides a better diagnosis
use the lowest grid ratio sufficient for the body part
higher grid ratio= higher patient dose
air gap technique
alternative to using a grid to clean up scatter
patient is placed 4-6 inces (10-15cm) away from the image receptor with a 10-12 feet SID
negative side is the increase in magnification and not useful in kVp higher than 90
eliminating repeats will decrease patient exposure
repeat image- is any image that must be done more than once due tohuman or mechanical errors
patient recieves a “double dose”
repeats are unacceptable if done due to carelessness or poor judgment
positioning
technique
repeat analysis
problems with positioning
incorrect centering
inappropriate technical factors
improper collimation
foreign bodies
processing artifacts
patient motion
avoiding unnecessary procedure to reduce patient exposure
chest x-ray
pre-admission
pre employment
routine health checkups
screening for TB
lumbar x-rays
pre-employment
CT whole body scans
check for disease
mobile radiogrpahy
minimal source to skin distance on a mobile fluoroscopy unit is 12 inches (30cm)
the smaller the source to skin distance the larger the entrance exposure
only perform portable x-ray on patients that cannot be transported to the department
digital imaging and computed radiography
just because the image can be electronically manipulated does not excuse overexposing the patient
utilization of technique charts
grids
fluoroscopy
largest exposure to patients in diagnostic radiology
limiting exposure in fluoroscopy
image intesification
increases brightness on screen
intermittent or pulse fluoro
limit maginification mode
limiting field size
technical factors
filtration
reduces skin dose
if you must shield
underneath the patient if the tube is underthe table
source to skin distance
NCRP states 15 inches (38cm) for fixed units and 12 inches (30cm) for mobile
limiting exposure in fluoroscopy cont.
cumulative timing device
audible alarm or interrup of fluoro every 5 minutes of time
the technologist is responsible to record the fluoro time in the electronic medical record
federal regulations tabletop exposure rates should not exceed 88 mGy per minute
primary protective barrier
2 mm lead equivalent for image intensifier built in the equipment
Automatic Brightness Control/ Stabilization (ABC/ABS)
no matter the kVp or mA varying, the brightness of the image remains the same
Automatic Exposure Rate Control (AERC)
adjusts exposure factors automatically as the bean moves over varying thicknesses
fluoro exposure switch/ dead man switch
foot pedal requires direct pressure to continue fluoro exposure
so, if the user would “fall over dead” the exposure would stop
fluoroscopically guided positioning (FGP)
using fluoroscopy to determine if you are positioned appropriately before taking an image
ASRT stand is that this practice is unethical and should never be used
digital fluoroscopy
beam turns off while image is scanned and then turns back on
pulsed
Dose Area Product (DAP)
newer fluoro systems provide the sum of the air kerma (energy) over the exposed area of the patient
Last image hold
when the foot comes off the pedal, it holes the last image and displays it on the screen until the foot pedal is activated again
C-arm fluoroscopy
used in the OR, Cardiac Cath, and IR
lengthy cases have the potential for high patient doses
properly trained personnel to work the equipment
12 inch (30cm) minimal distance to the patient
spacers are usually placed to maintain a safe distance
C-arm should be positioned with the image intensifier on the top
reduces scatter and patient dose
cinefluoroscopy
used in cardiology and neuroradiology
works like a movie
reduce patient exposure
limit time without losing information
collimate
last frame hold
interventional radiology
invasive sterile procedures performed by a physician under fluoro
FDA requires documentation in the patient chart if skin does is 1-2 Gy
federal regulations for table-top exposure rates for procedures with high level control fluoro (HLCF) exposure limits are 176 mGy per minute
HLCF allows for visualization of smaller and lower contrast objects
should be performed by an educated and trained physician
keeps patient doses and occupational doses down
radiation patient dose measurements
entrance skin exposure (ESE)
includes skin and glandular
skin dose
absorbed dose to the most superficial layers
gonadal dose
genetically significant dose (GSD)- assess the effects of gonadal dose
approximate dose in US is 0.2mSv
bone marrow dose
dose to entire active bone marrow
also known as the mean marrow dose
pregnant patient
asking LMP
RH policy should be followed
10-day rule
ICRP recommendation from 1970
ACR’s position on pregnant patients
elective exams should be scheduled according to the 10-day rule
10-25 rad rule
<10 ok
10-25 consider options
>25 not good
radiology departments are responsible to post pregnancy signs
how to reduce dose to a pregant patient
minimize the dose
smallest exposure that will produce optimal images
collimate
RH patient must sign a consent form if the pelvix/abdomen area
mammography
utilizes low kVp
limit number of projections
adequate compression
avoid axillary exposure unless ordered by radiologist
CT
doses are higher than diagnostic radiology
shielding is usually not utilized because of the nature of the exposure
collimators are very tight in CT, exposure is caused by internal scatter
pediatric patients
more sensitive to exposure due to rapidly dividing cells
due to their longer life span it can increase changes of developing a radiation induced leukemia or radiogenic malignancy such as lung or thyroid
decreasing exposure to pediatric patients
communicate at their level
minimize repeats
minimize number of images taken
use collimation
use short exposure times/ appropriate exposure factors
less exposure is needed to obtain optimal images
shiel
morbid obesity
have patient centered to table because landmarks are hard to palpate
skeletal anatomy does not change in position and organs are not larger except:
thoracic cage expanded 2”
stomach may slightly be larger
colon may spread out
increase kVp to increase penetration of the x-ray beam
use grids to clean up scatter
in most cases it is not appropriate to increase the image receptor size
smaller collimaiton decreases scatter
image gently campaigns
CT- one size does not fit all
digital- back to basics
NM- go with the guidelines
fluoro- pause and pulse
AIR- step lightly
equipment safety
on and off switches
interlocks
detents
fluoro locks
visual/audio monitors
control panel
laser light
tape measures
emergency controls