Deep neck and Orbit
1/154
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
155 Terms
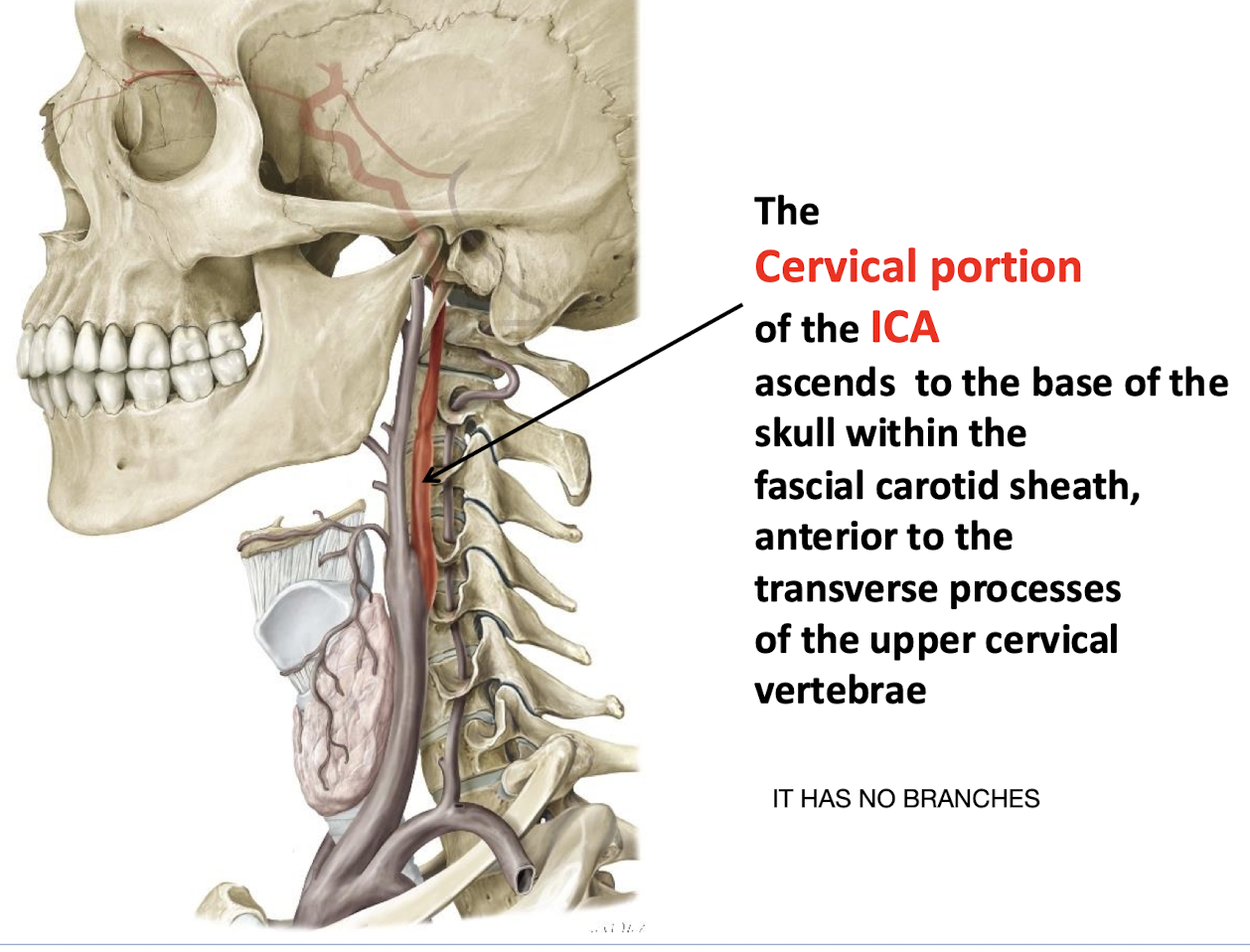
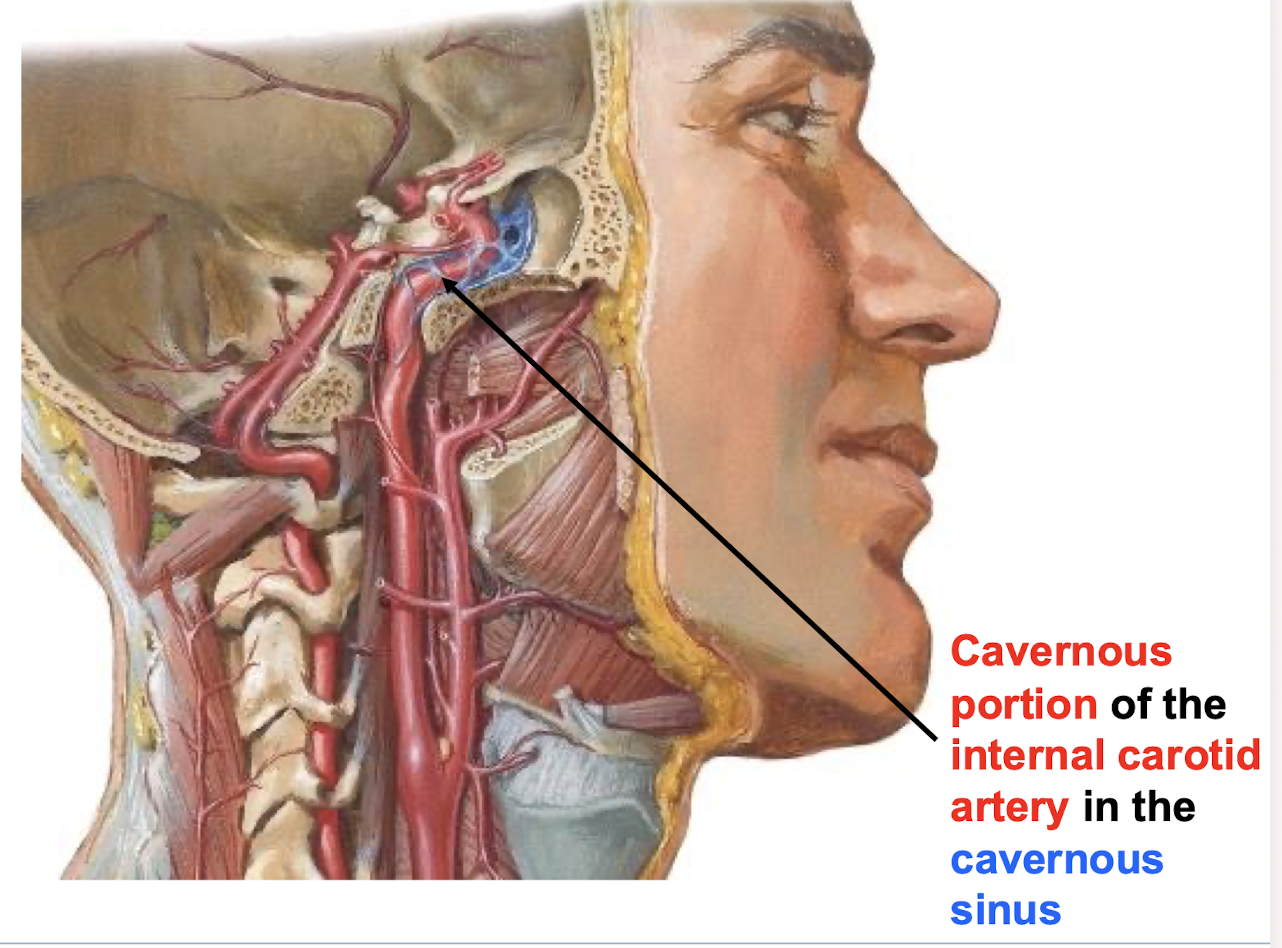
What structure is the cervical portion of the ICA located within as it ascends to the base of the skull; and what is notable about its branches?
It ascends to the base of the skull within the fascial carotid sheath; anterior to the transverse processes of the upper cervical vertebrae; IT HAS NO BRANCHES
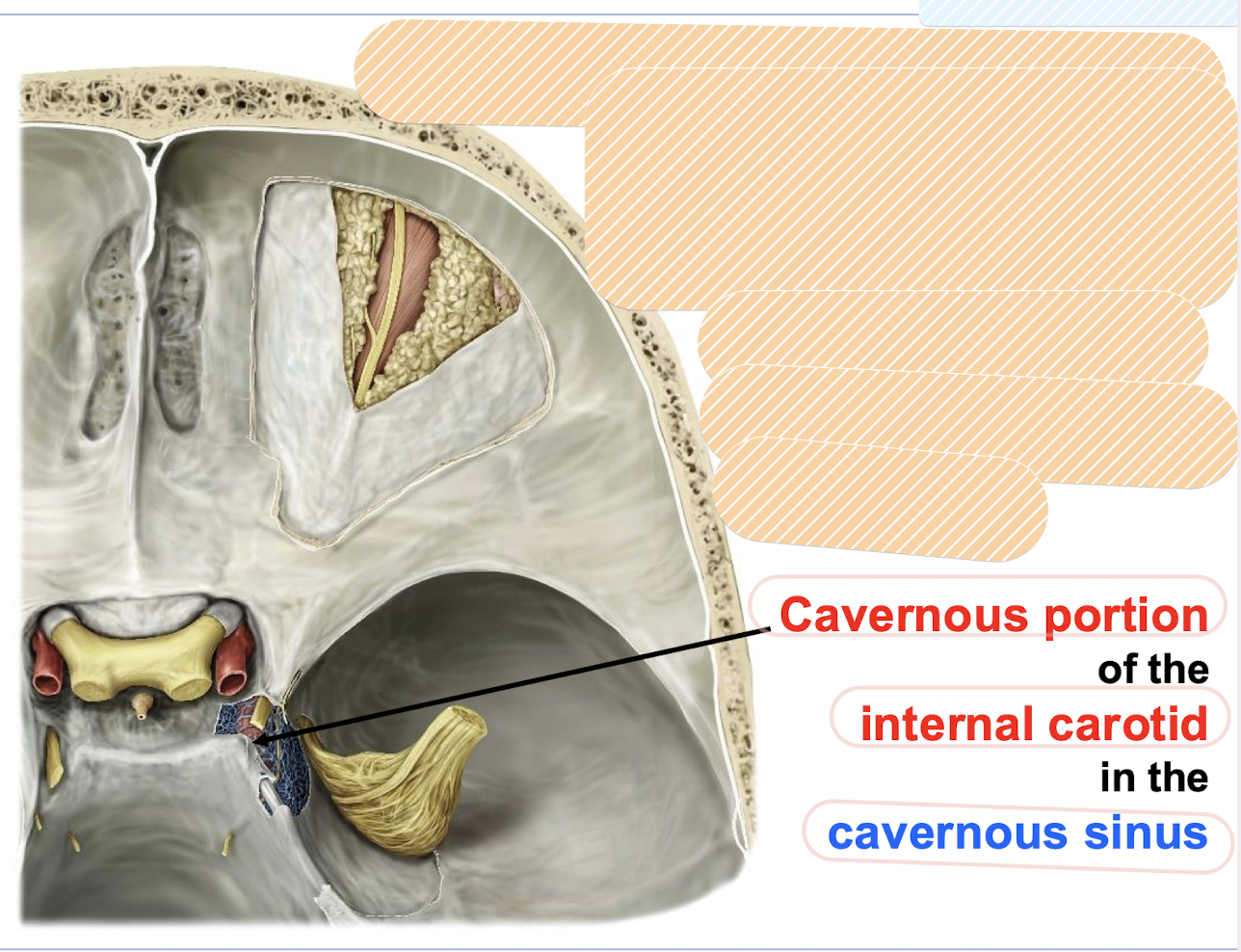
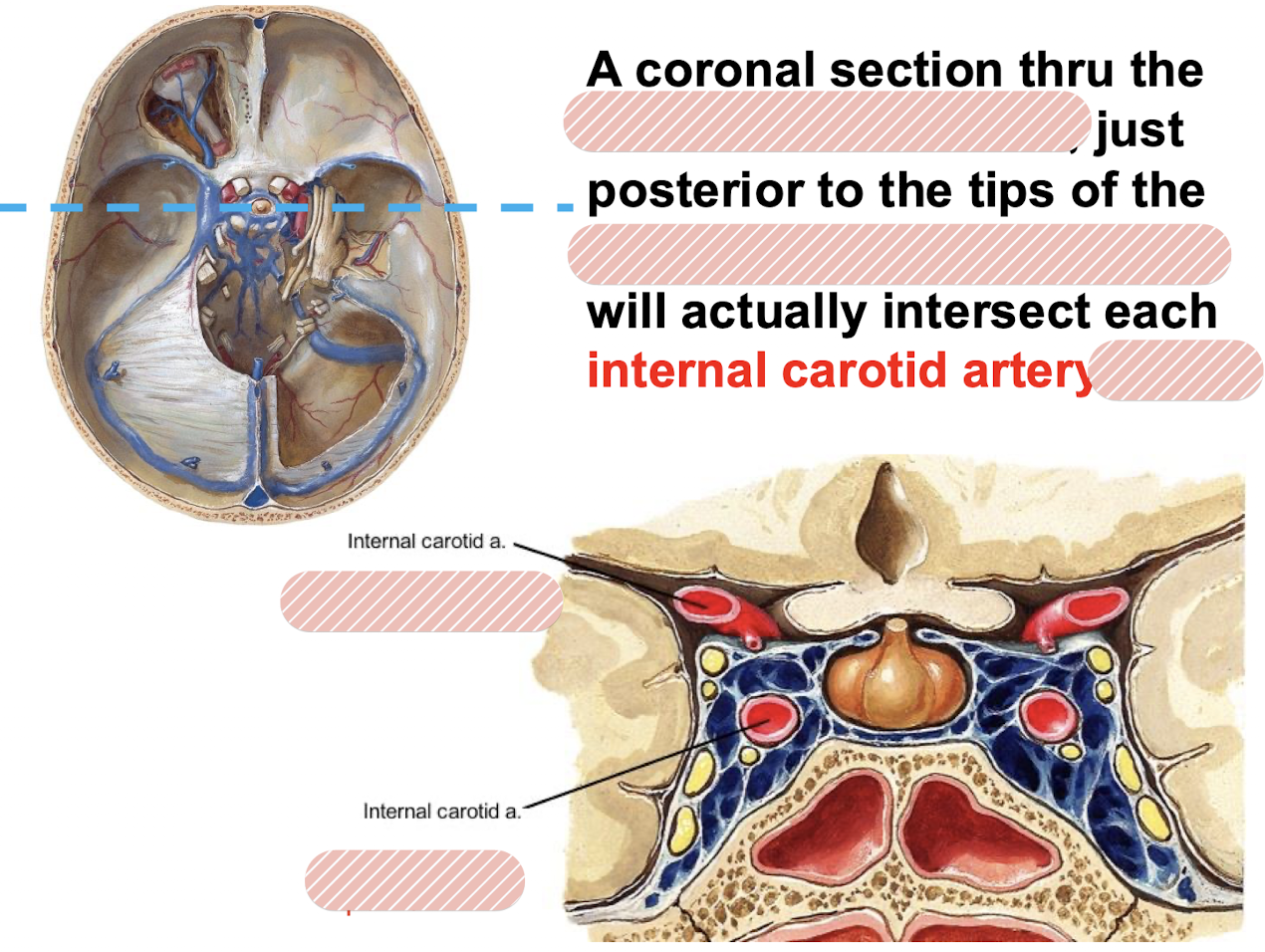
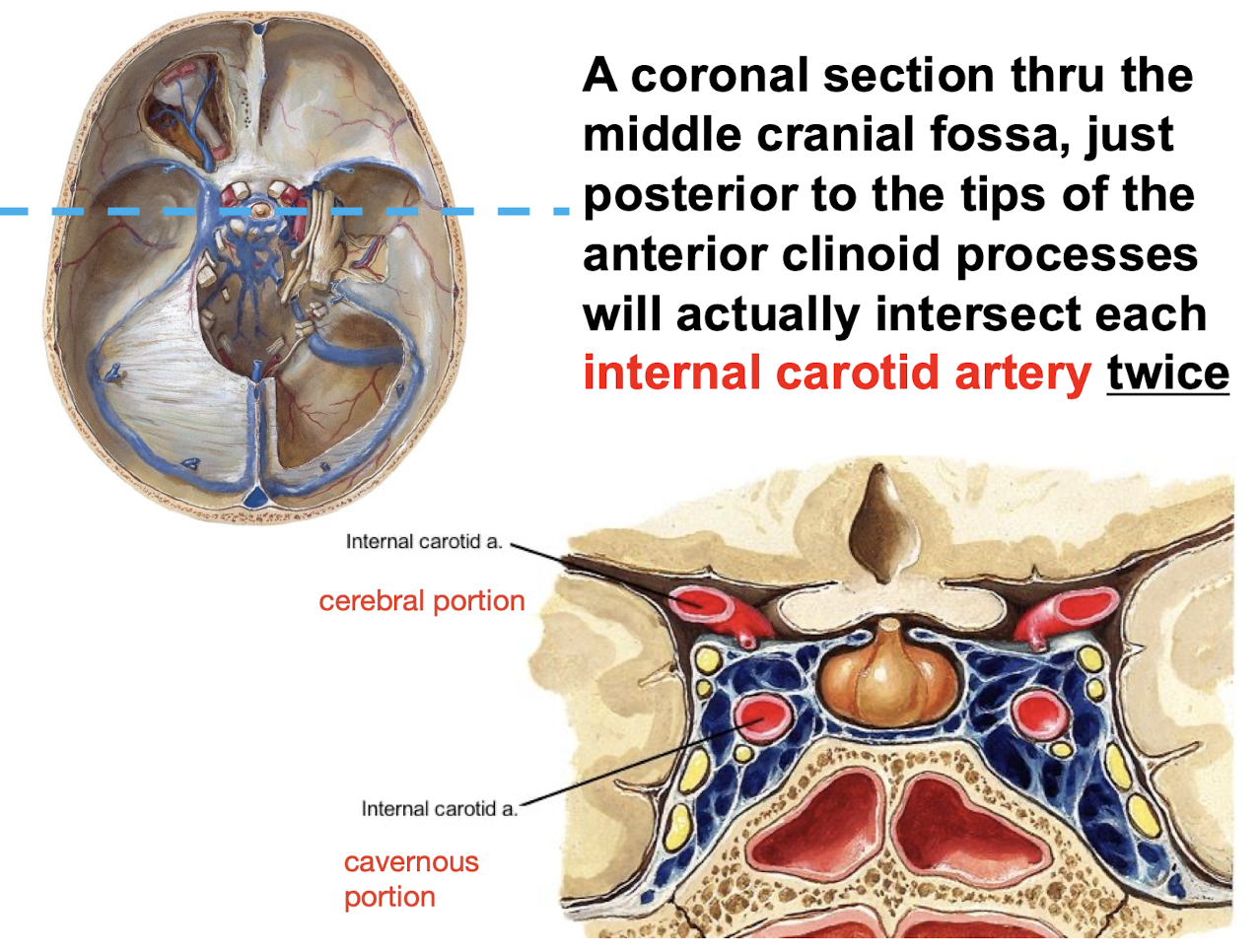
Where does and what portion of the ICA enters the cranial cavity; and where does the cavernous portion course?
The petrous portion enters the cranial cavity through the CAROTID CANAL; and then the cavernous portion courses through the cavernous sinus just lateral to the sella turcica
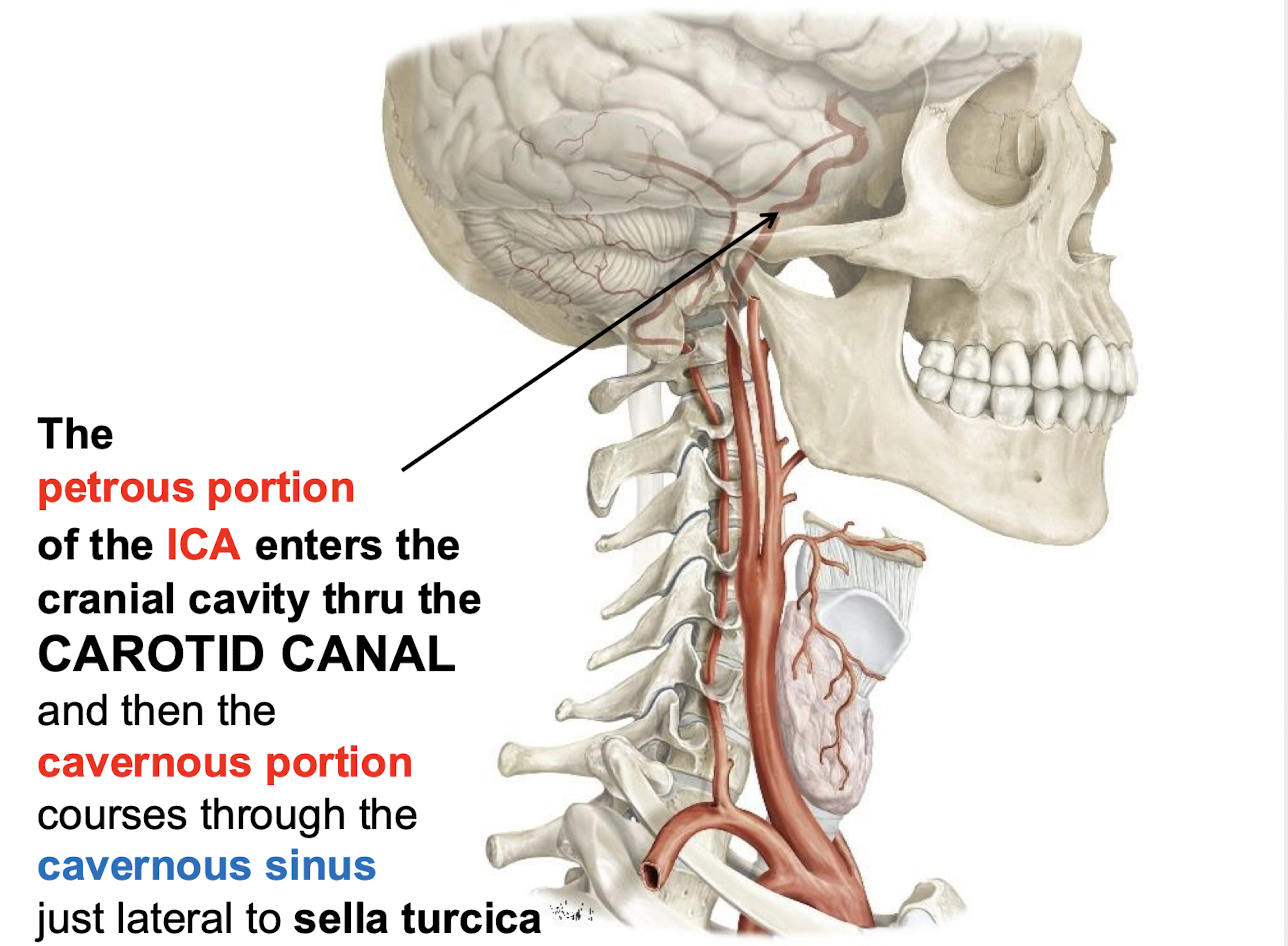
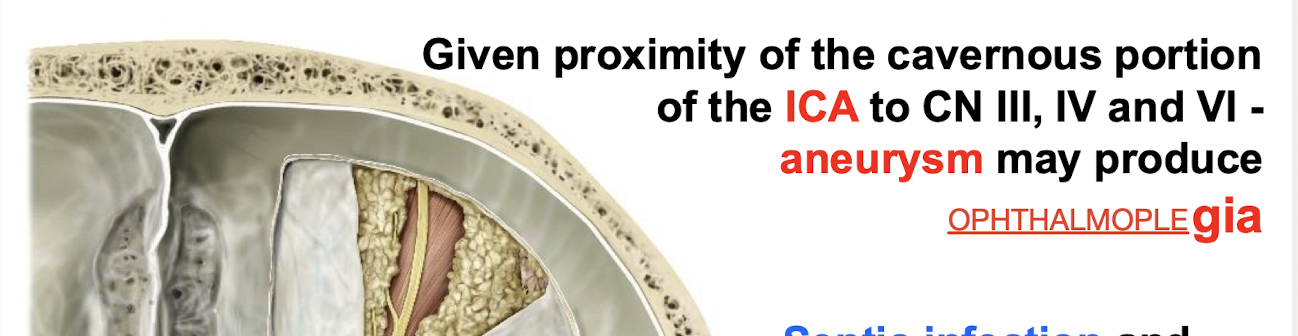
What symptoms might an aneurysm of the cavernous portion of the ICA produce? What nerves is this related to?
Due to the proximity of the cavernous portion of the ICA to CN III; IV; and VI. An aneurysm may produce OPHTHALMOPLEGIA (paralysis or weakness of eye muscles)
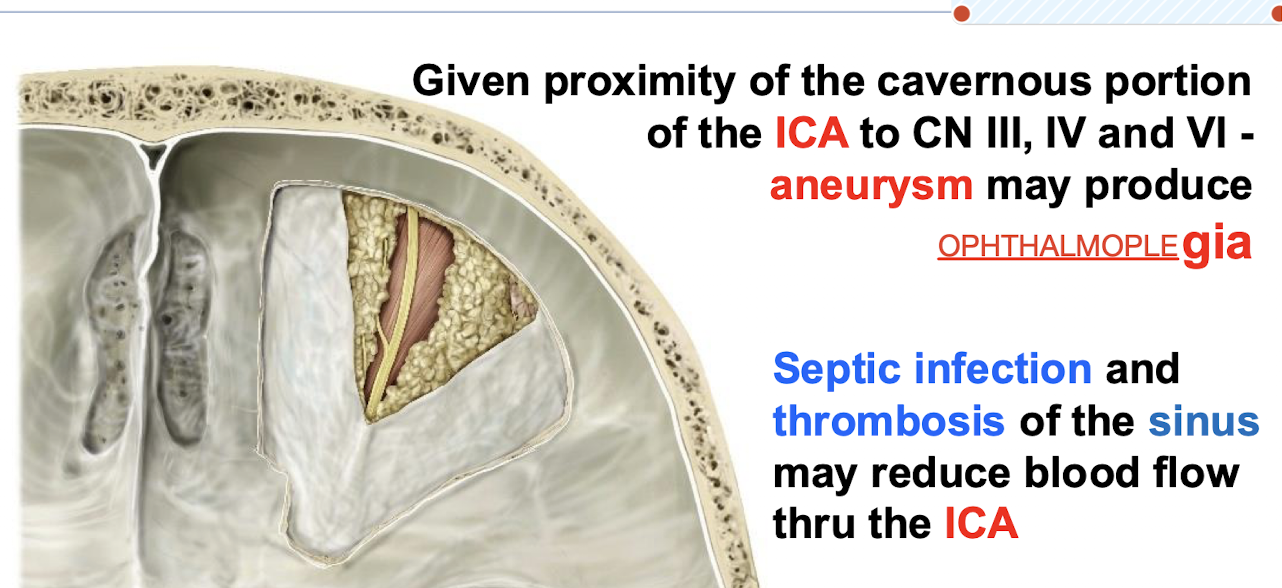
What problems related to the cavernous sinus may affect the ICA?
Septic infection and thrombosis of the cavernous sinus may reduce blood flow through the ICA.
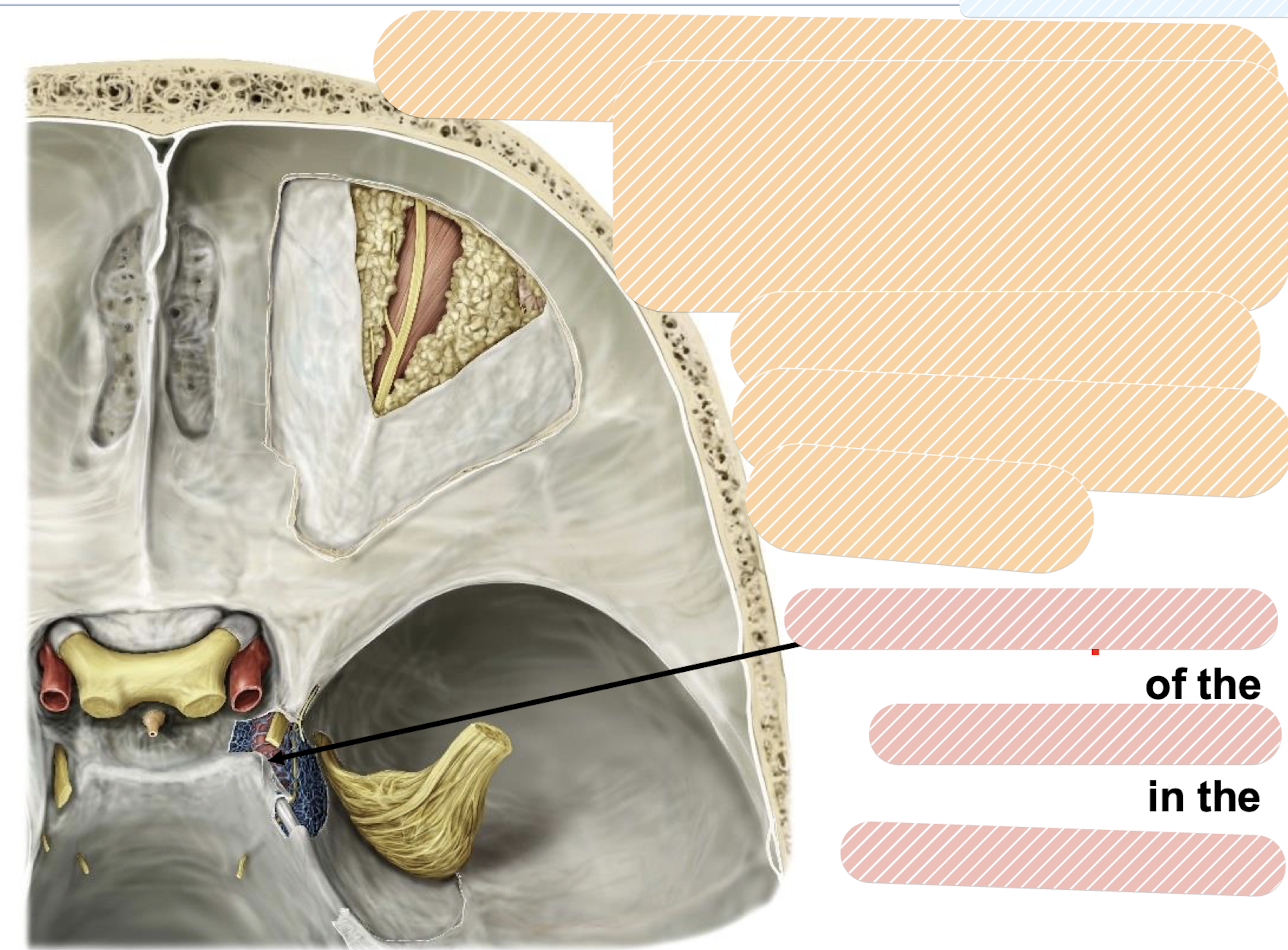
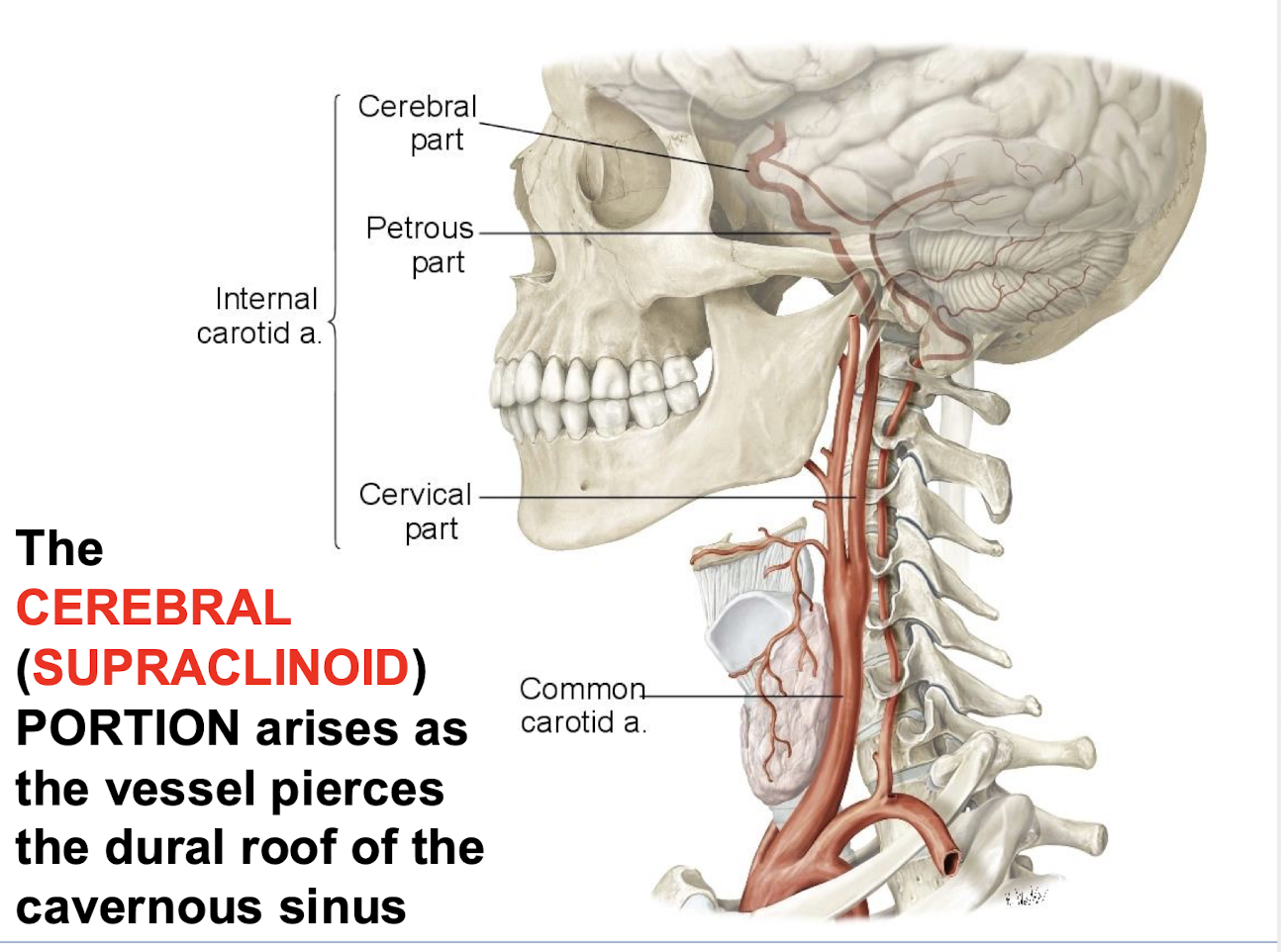
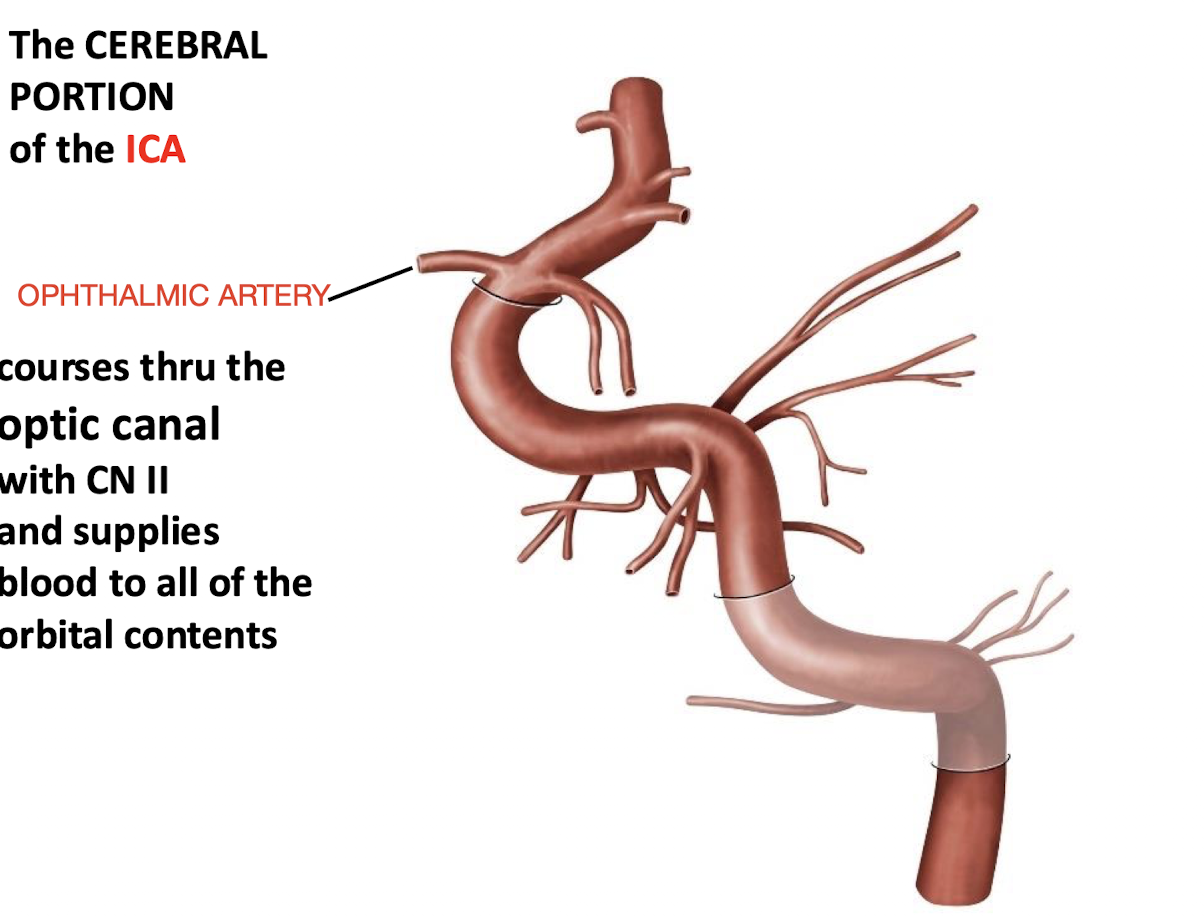
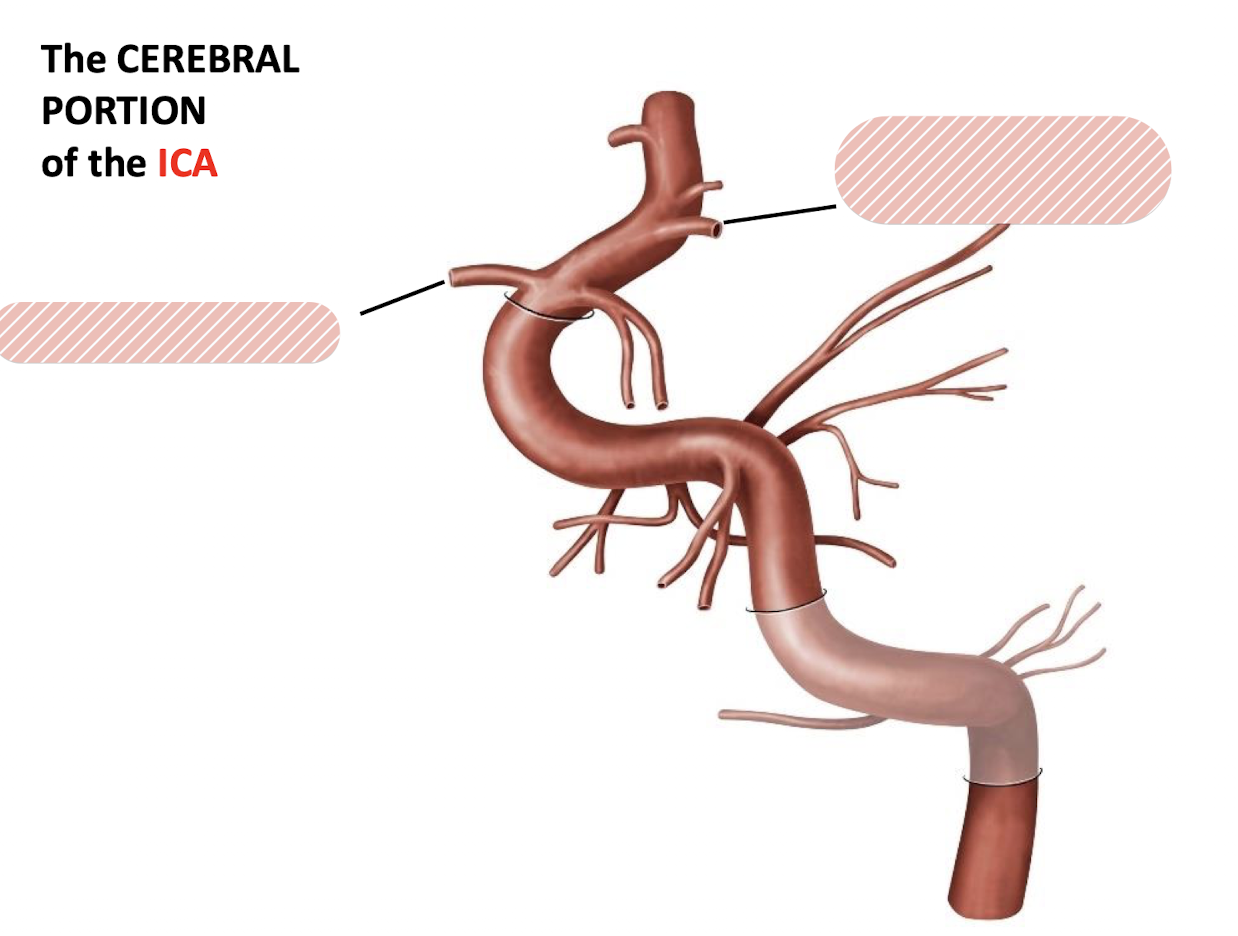
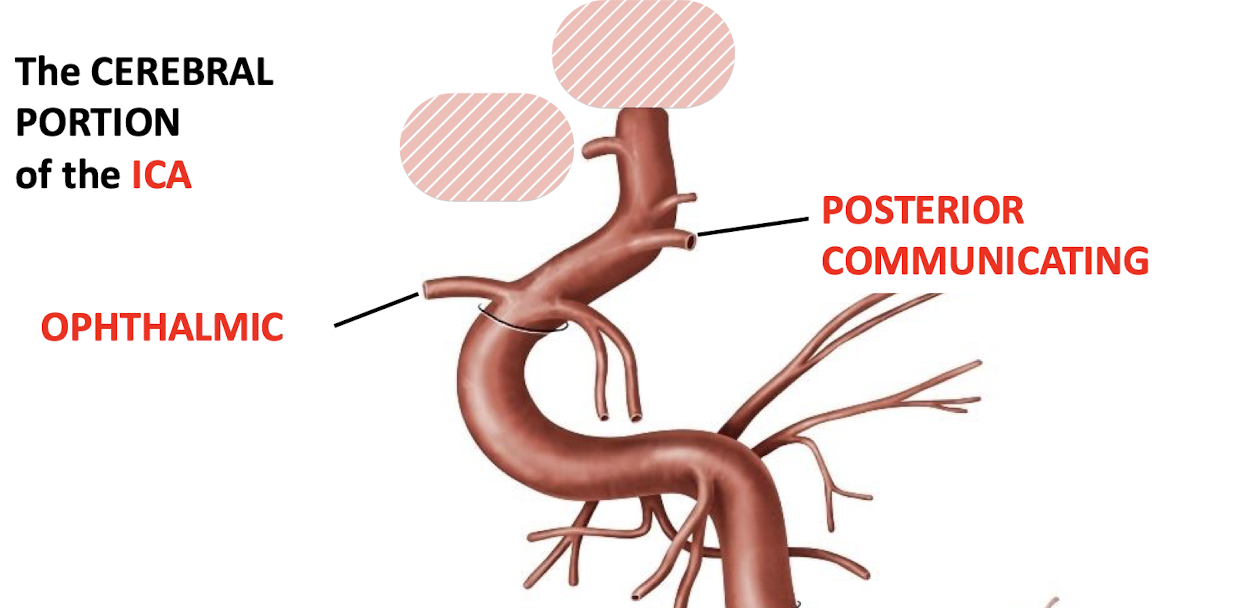
What is the CEREBRAL (SUPRACLINOID) PORTION of the ICA?
The part that arises as the vessel pierces the dural roof of the cavernous sinus.
What artery originates from the cerebral portion of the Internal Carotid Artery and supplies the orbital contents?
The ophtalmic artery courses through the optic canal with CN II; and supplies blood to all of the orbital contents
What are the key branches of the OPHTHALMIC artery
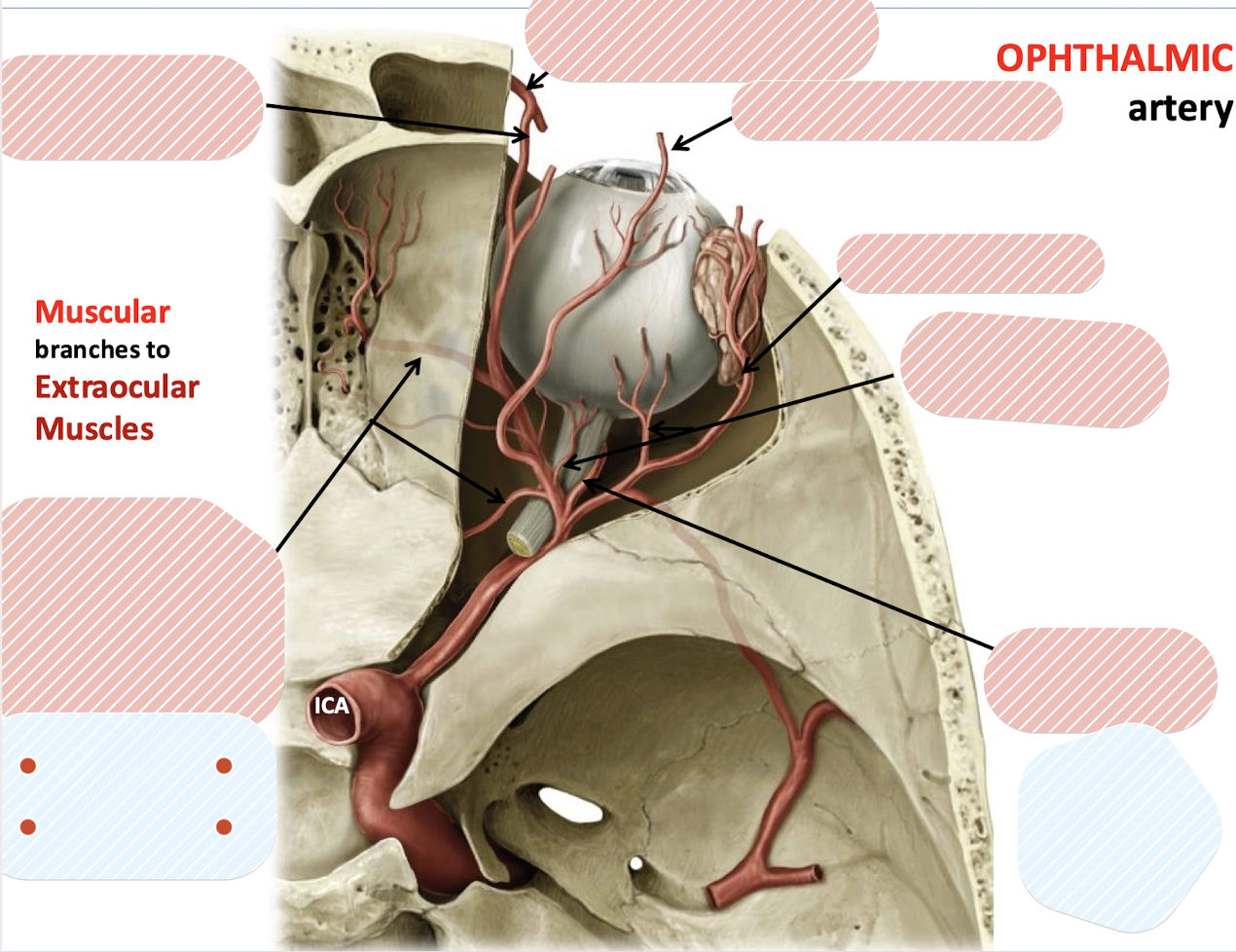
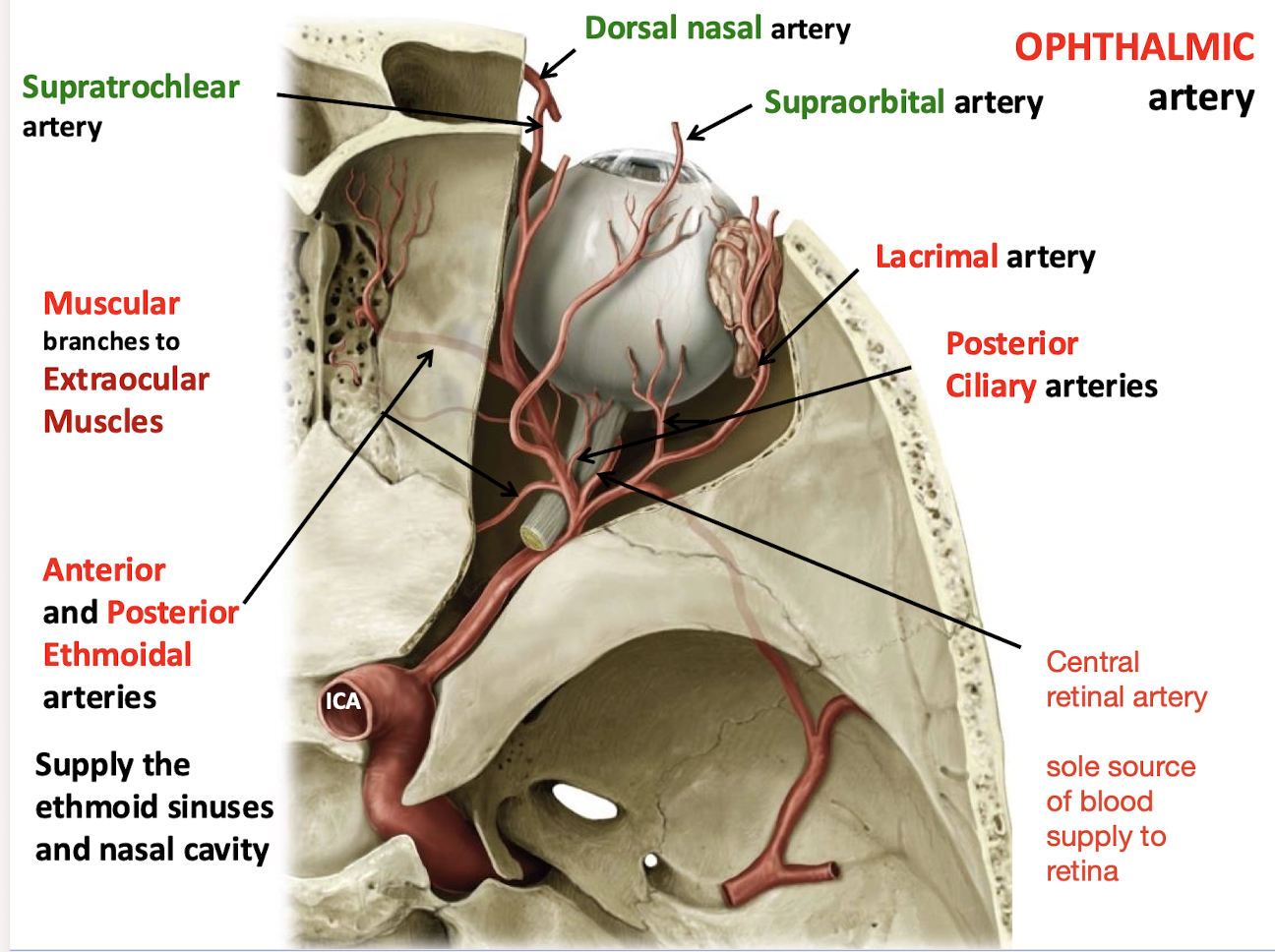
Anterior and Posterior Ethmoidal arteries; Supratrochlear artery; Supraorbital artery; Lacrimal artery; Posterior Ciliary arteries; Muscular branches to Extraocular Muscles; Central retinal artery
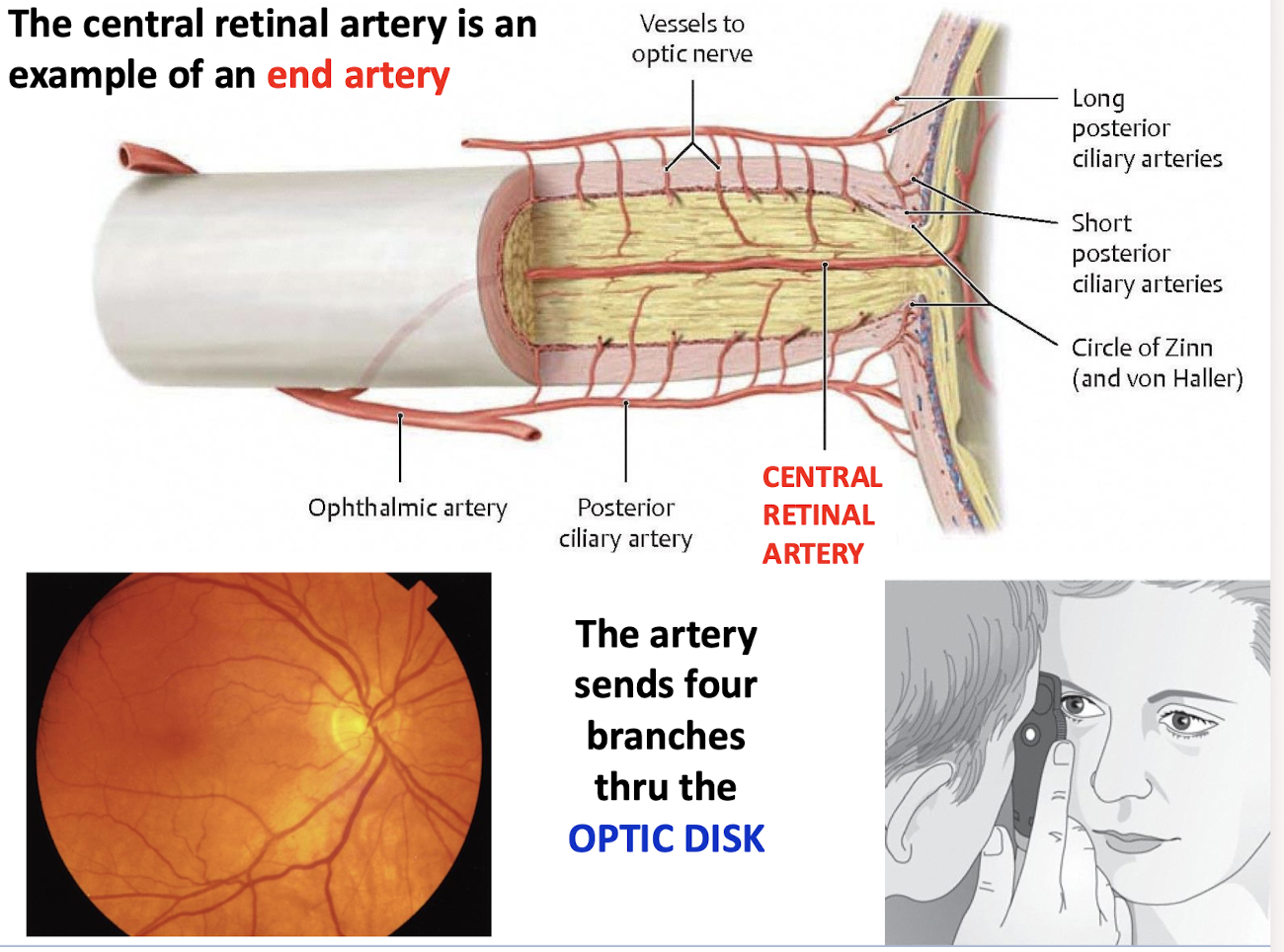
What is the sole source of blood supply to the retina; and what type of artery is it an example of?
Central retinal artery; an example of an end artery
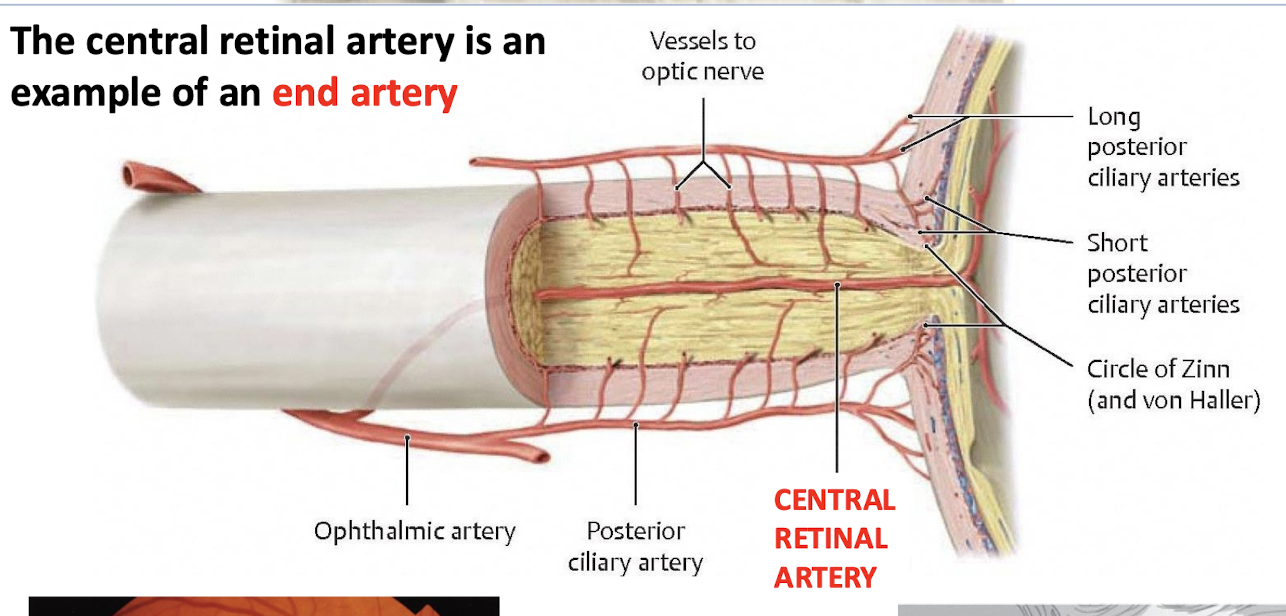
How many branches does the central retinal artery have and what do they course through?
Four branches through the OPTIC DISK
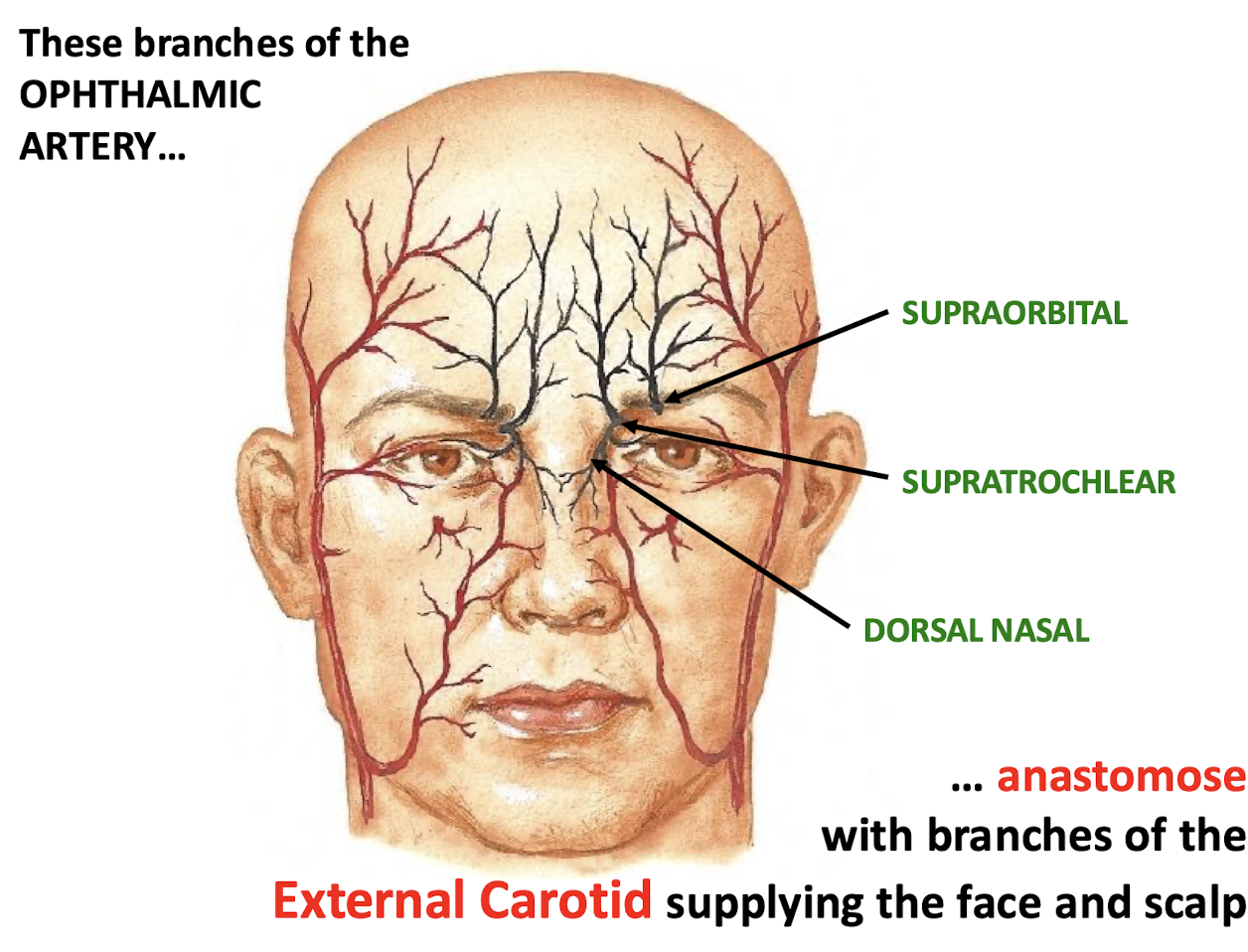
Which three branches of the OPHTHALMIC ARTERY supply the skin of the forehead; root; and bridge of the nose
Supratrochlear artery; Supraorbital artery; Dorsal nasal artery
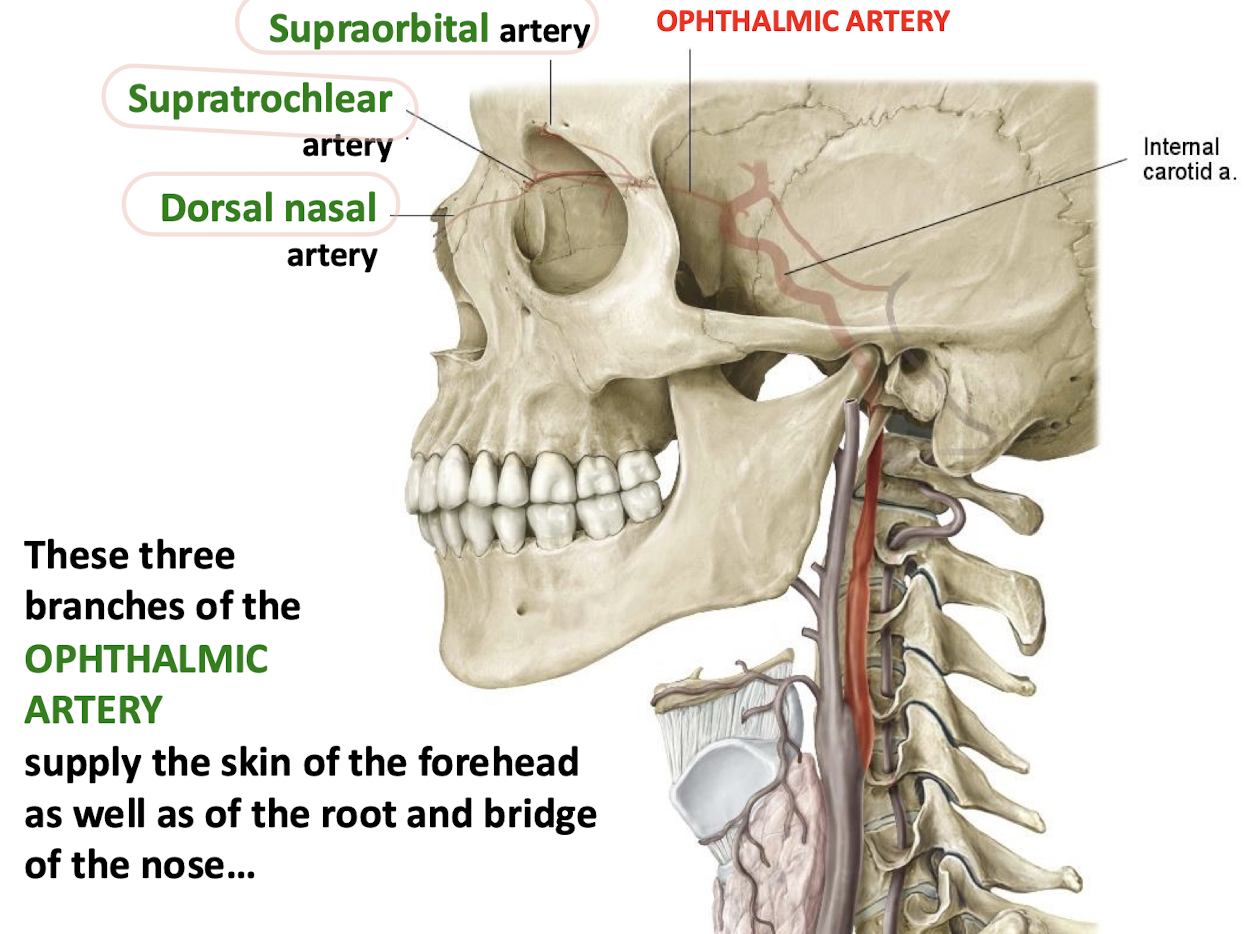
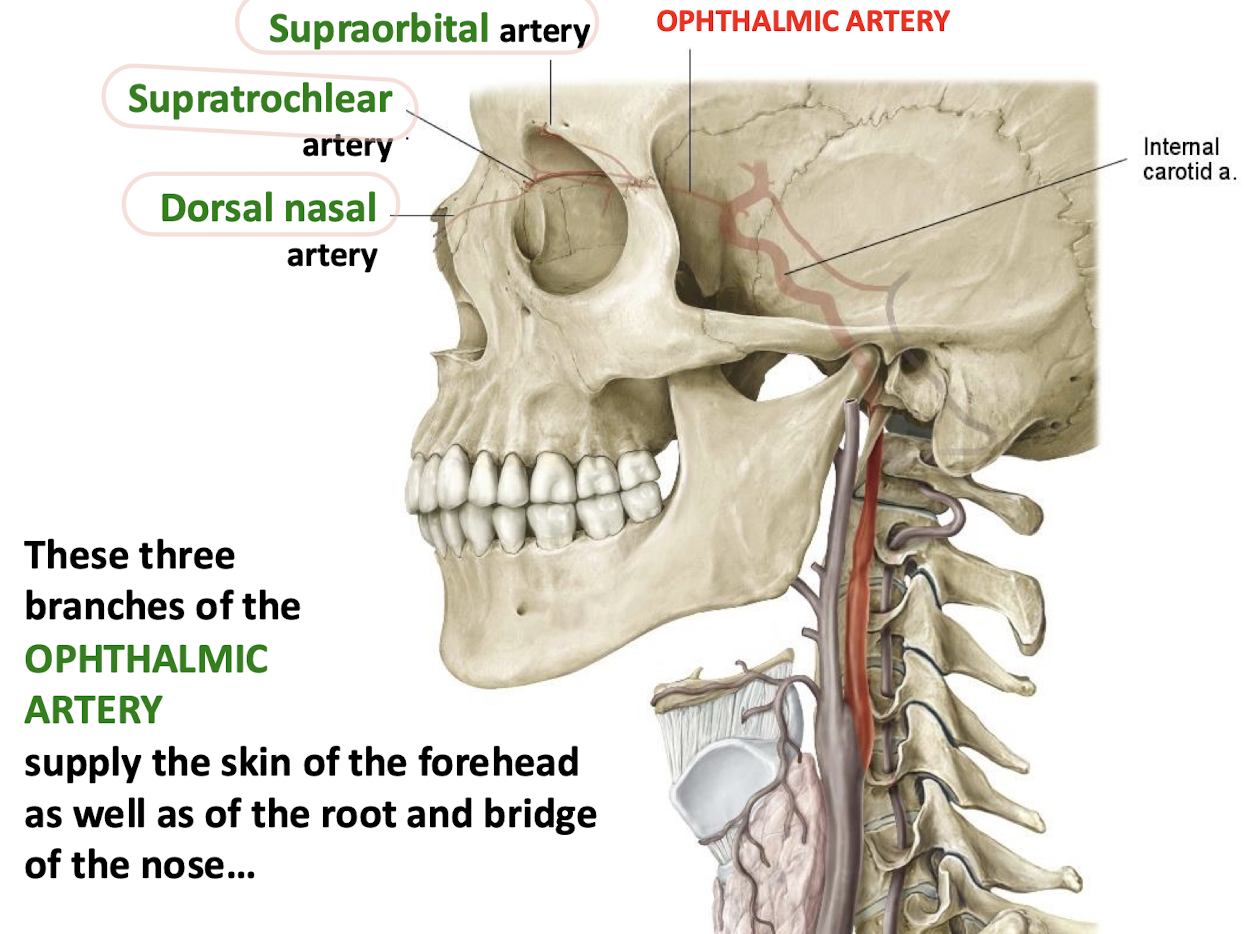
What do the supraorbital, supratrochlear and dorsal nasal branches of the opthalmic artery anastamose with?
Branches of the external carotid supplying the face and scalp
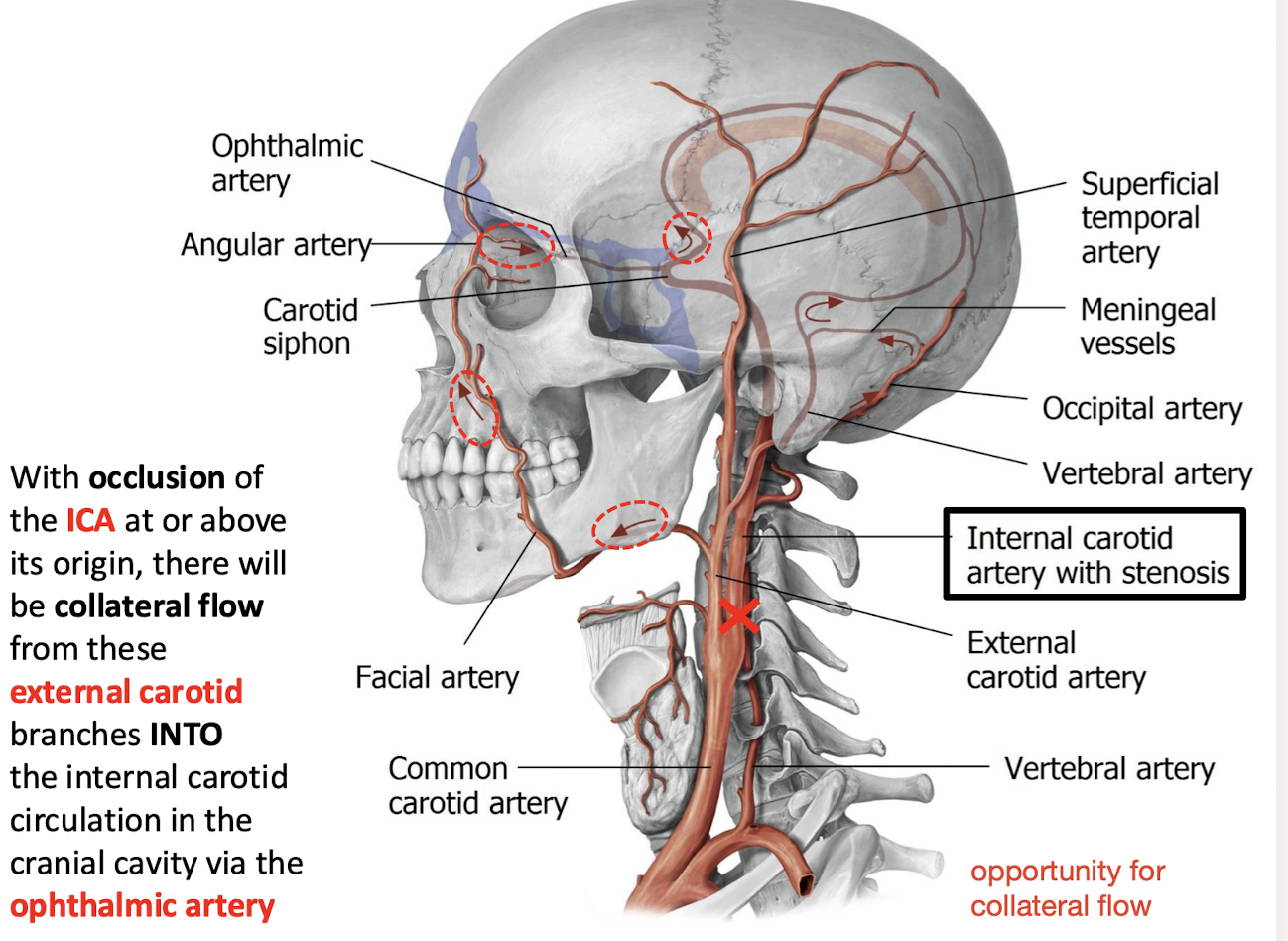
With occlusion of the ICA at or above its origin; how does collateral flow occur into the internal carotid circulation in the cranial cavity?
Collateral flow occurs from external carotid branches INTO the internal carotid circulation via the OPHTHALMIC artery
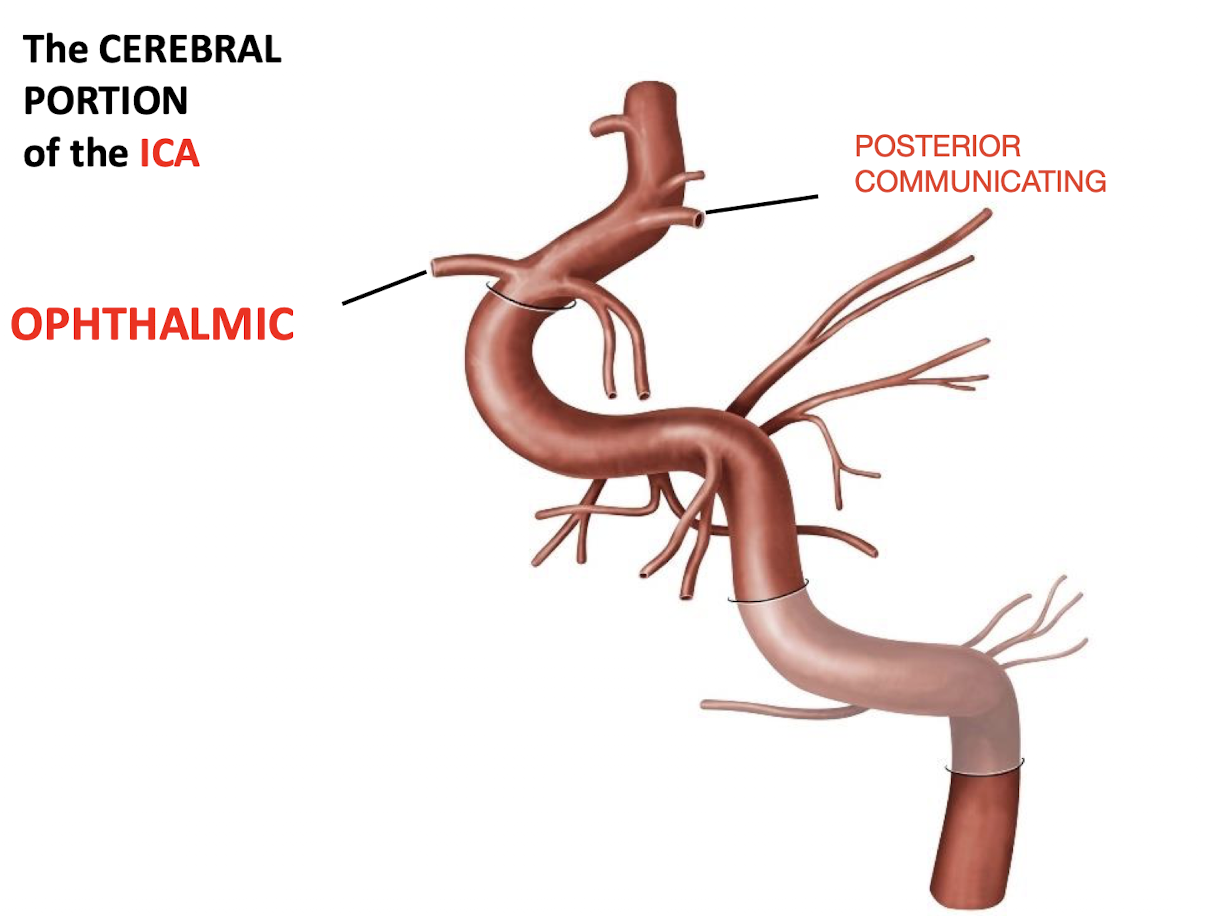
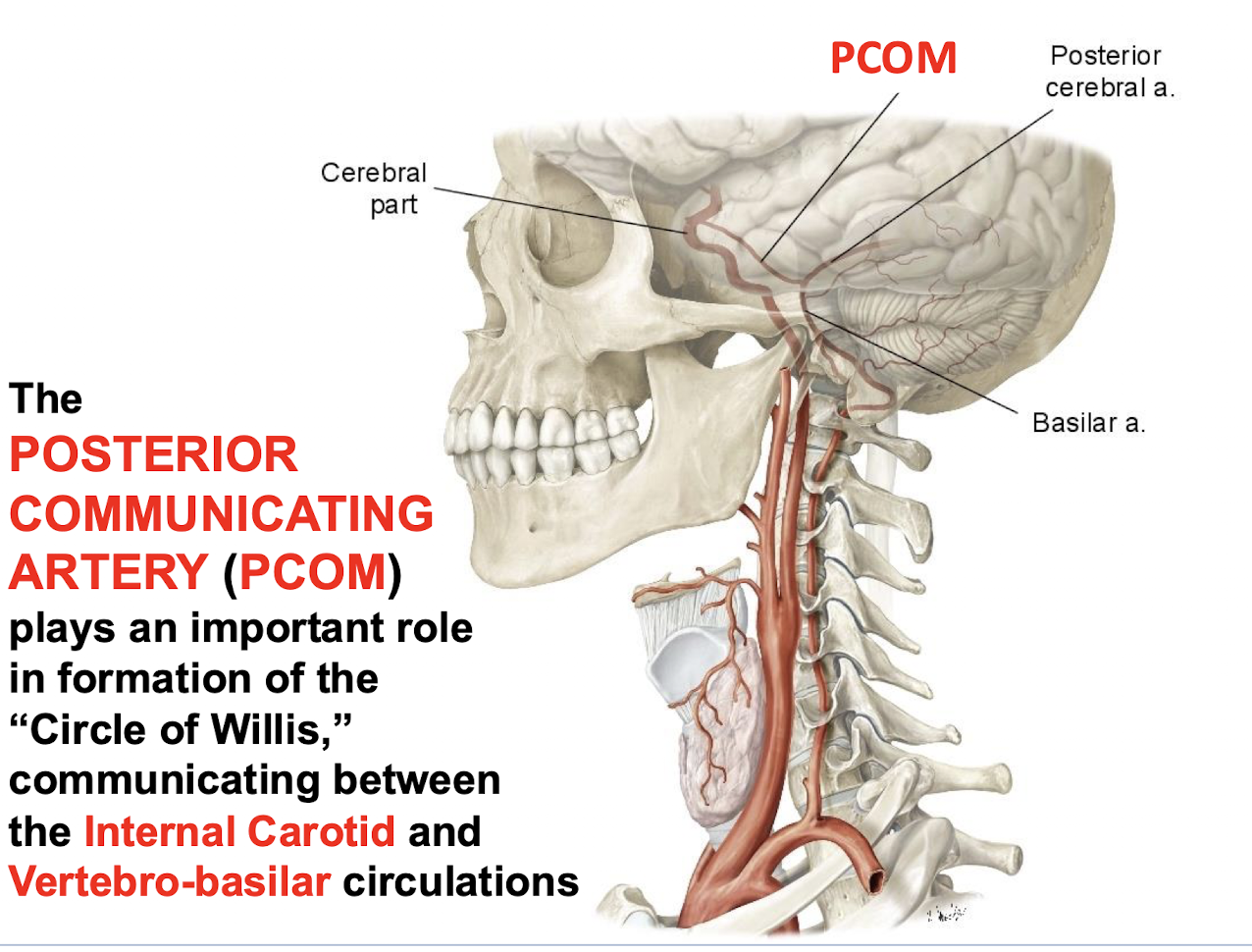
What important role does the POSTERIOR COMMUNICATING ARTERY (PCOM) play in circulation?
It plays an important role in formation of the “Circle of Willis;” communicating between the Internal Carotid and Vertebro-basilar circulations.
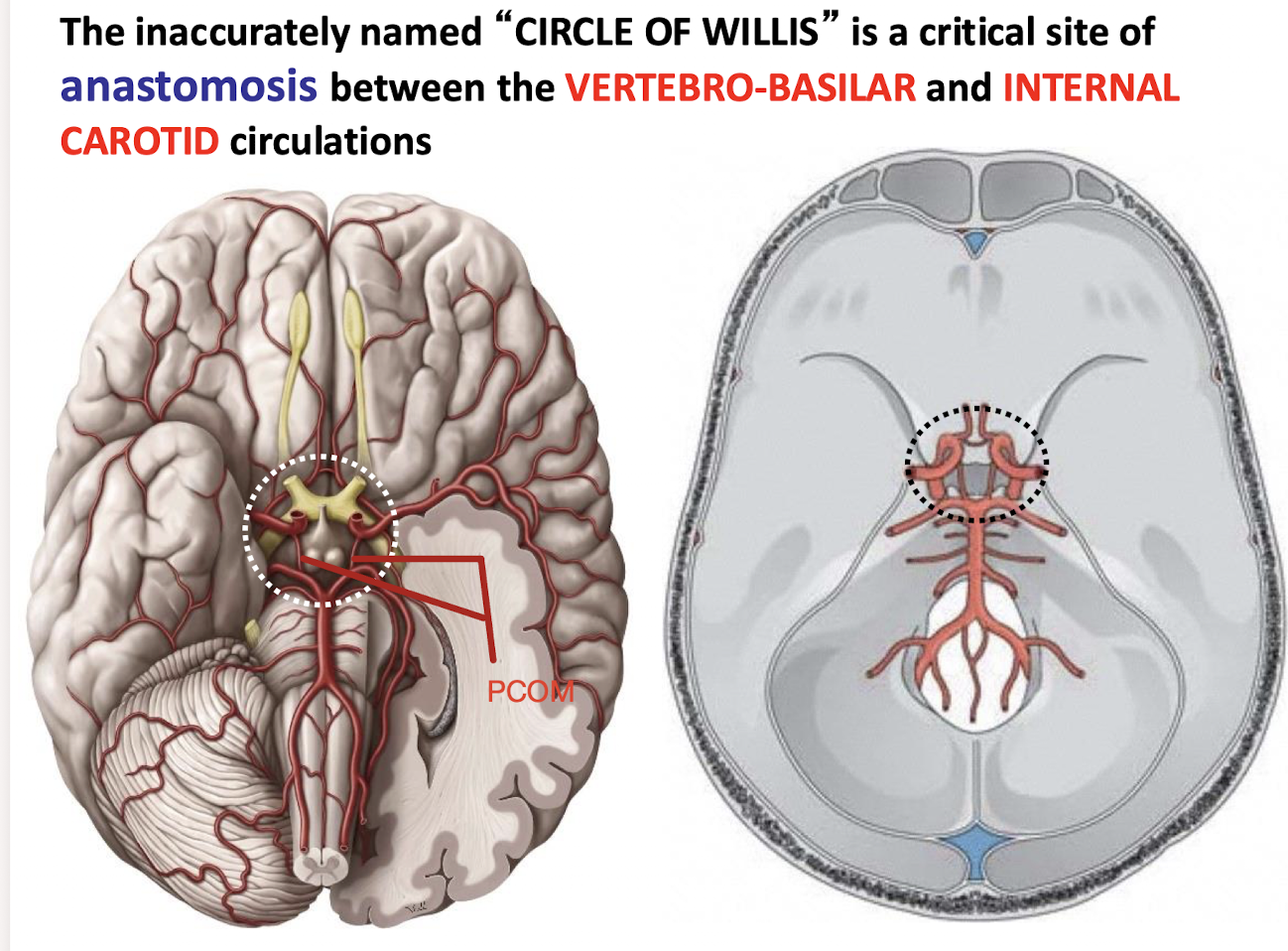
What structure is the critical site of anastomosis between the VERTEBRO-BASILAR and INTERNAL CAROTID circulations?
The inaccurately named “CIRCLE OF WILLIS”
What two main arteries arise from the terminal bifurcation of the CEREBRAL PORTION of the ICA
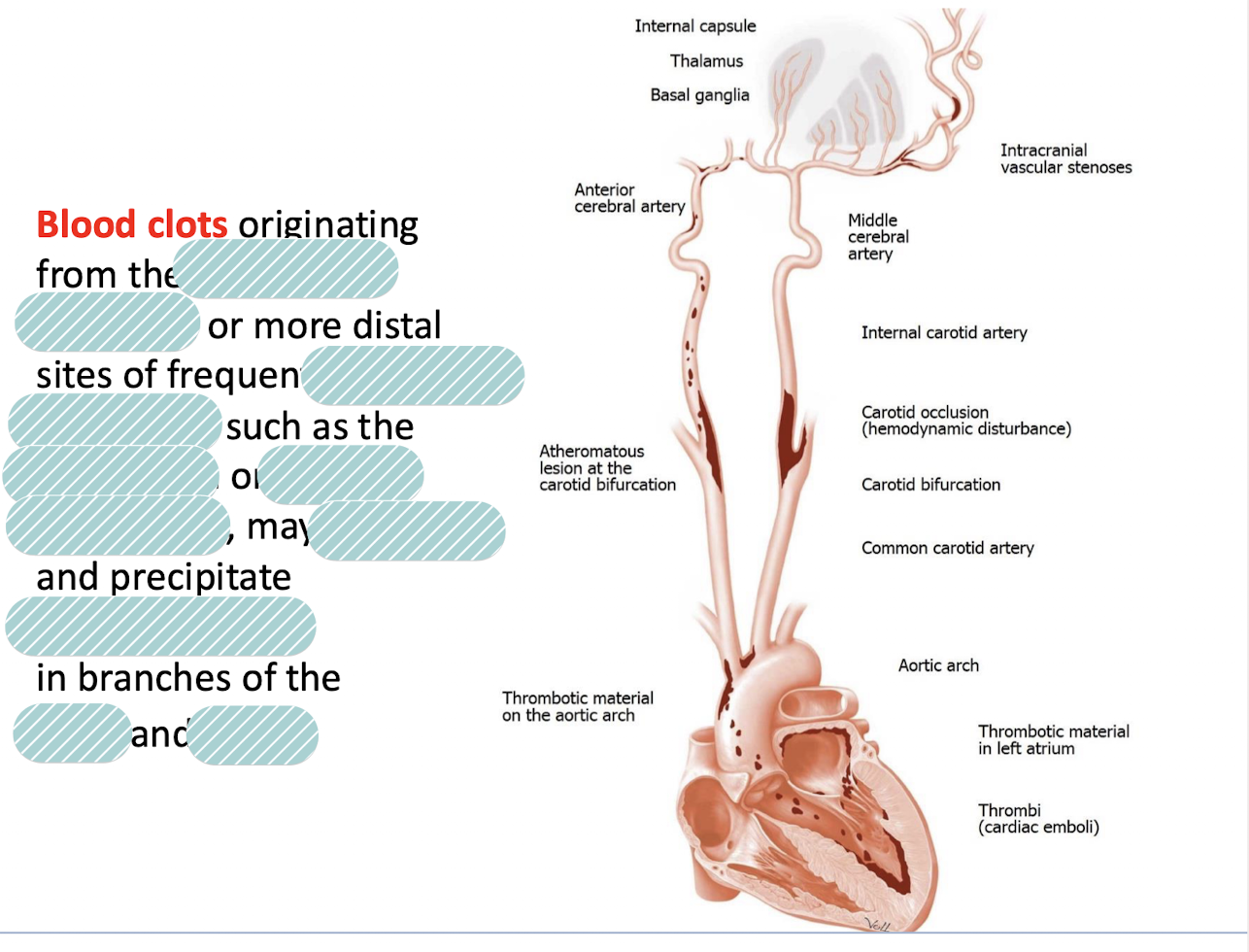
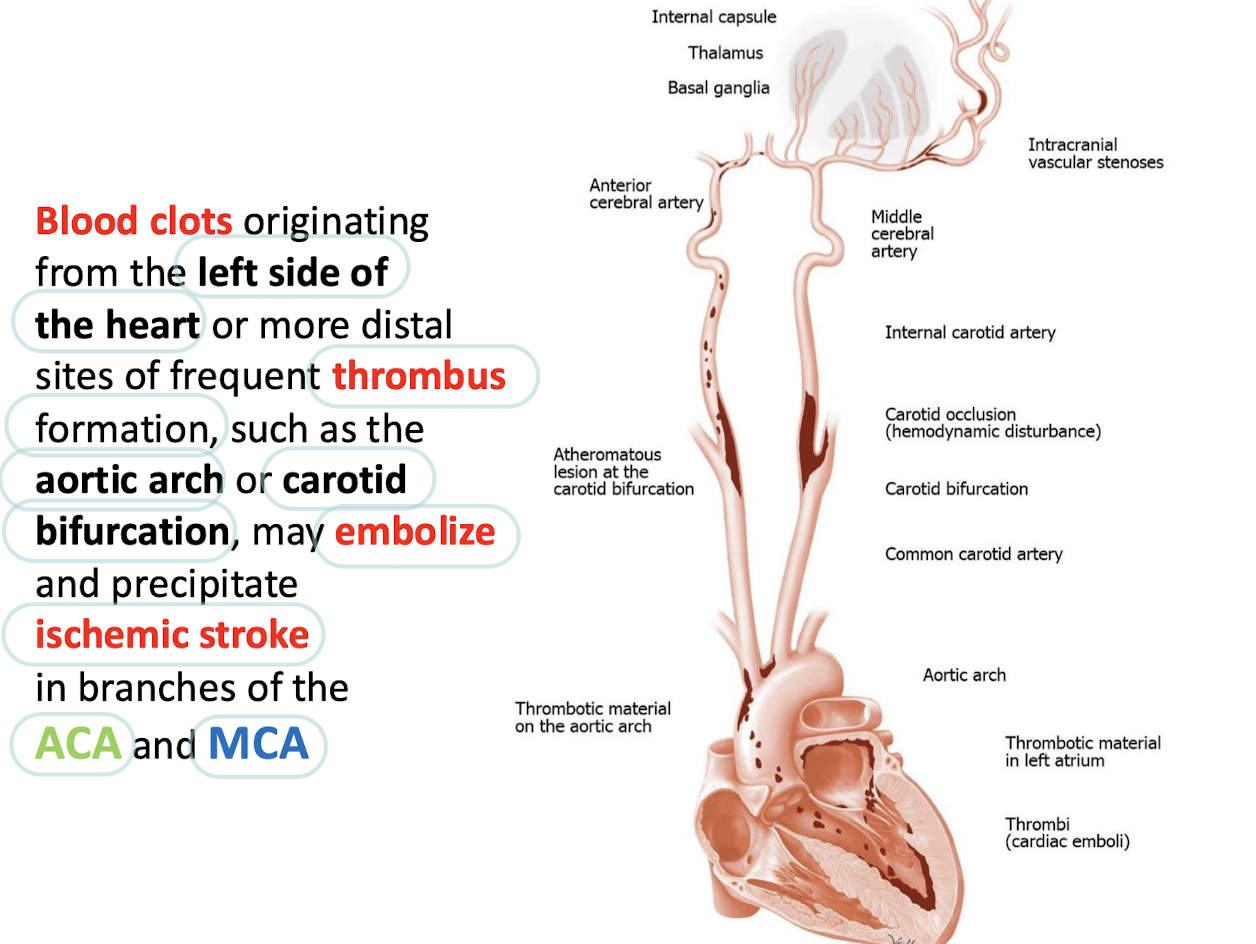
The ANTERIOR CEREBRAL ARTERY (ACA) and MIDDLE CEREBRAL ARTERY (MCA)
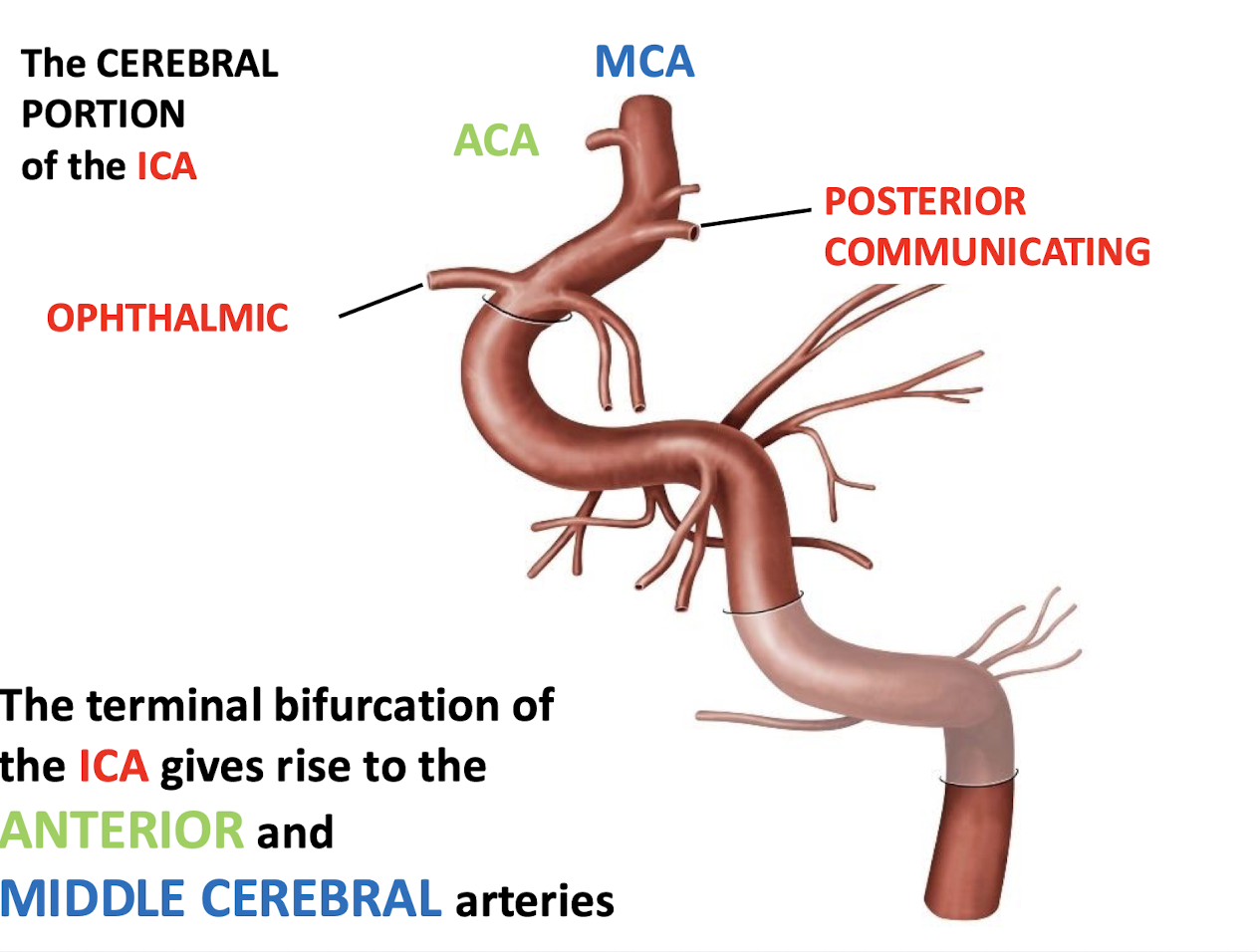
The ACA and MCA
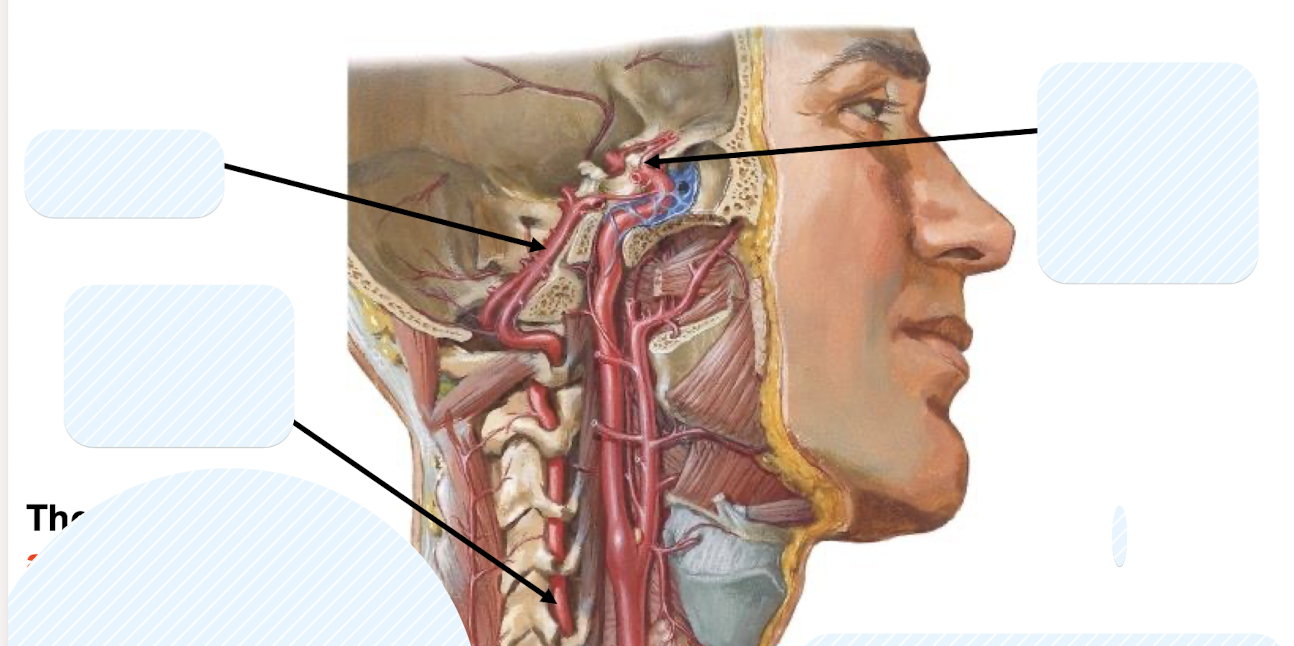
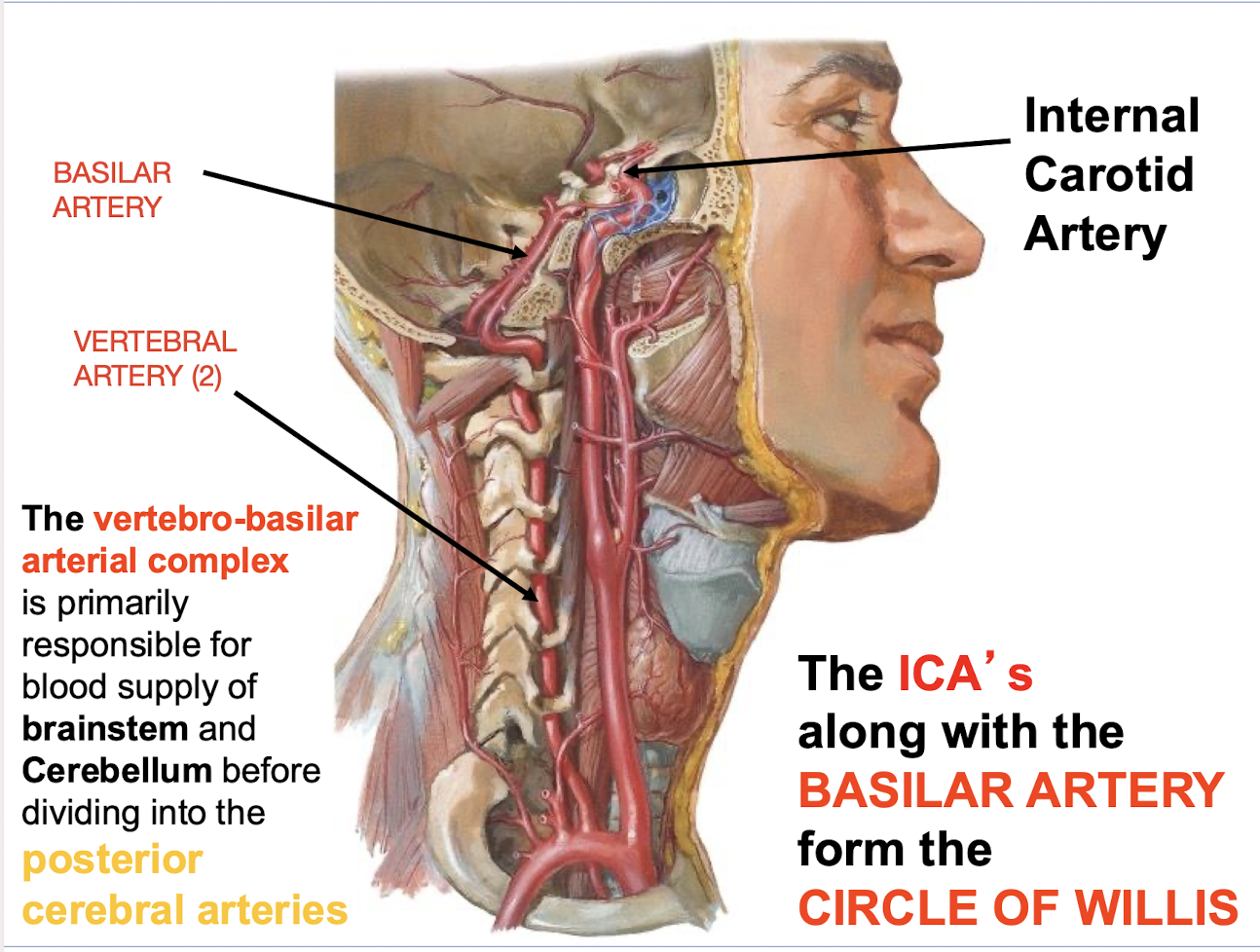
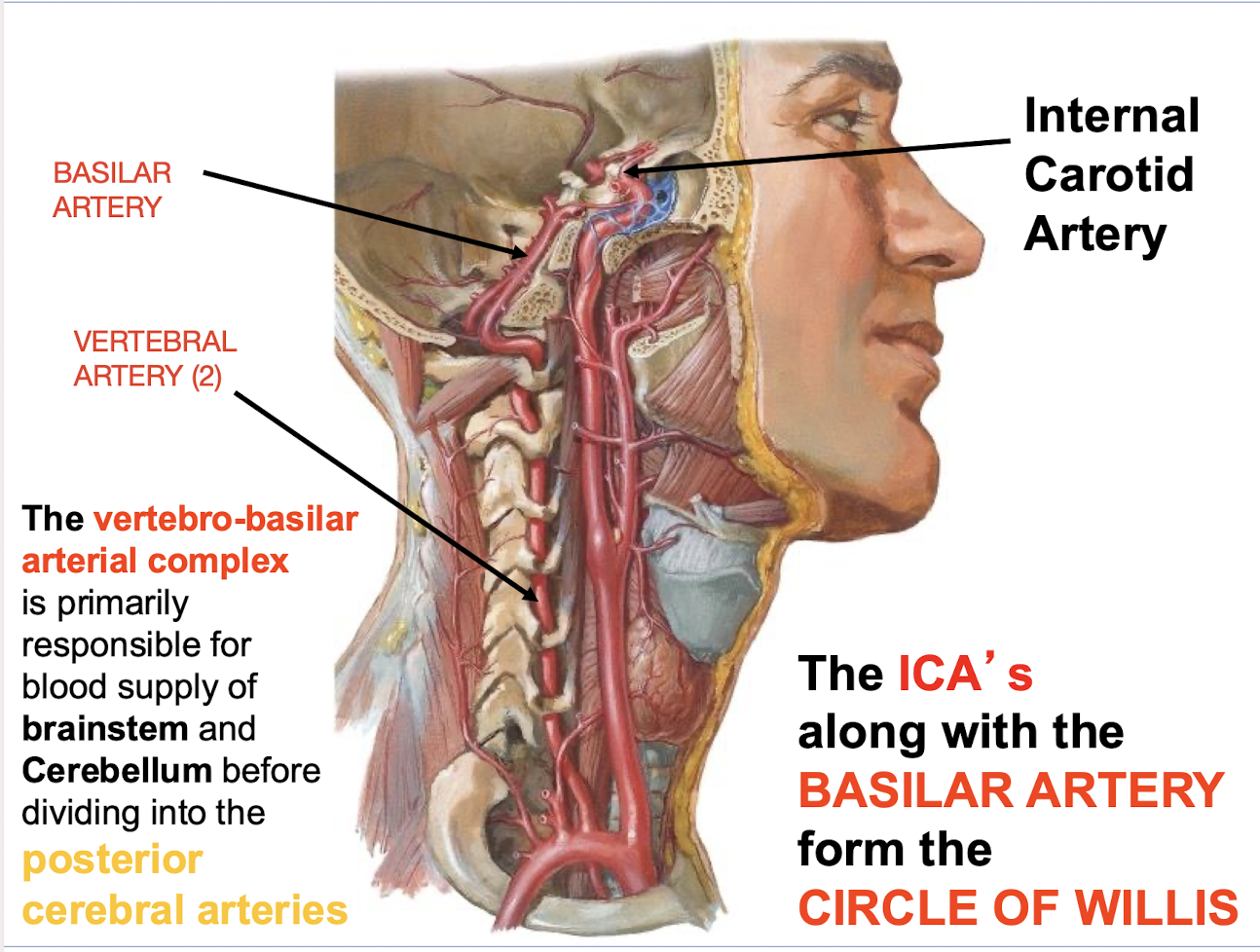
The ICA’s along with which major artery form the Circle of Willlis (central arterial network)?
The BASILAR ARTERY
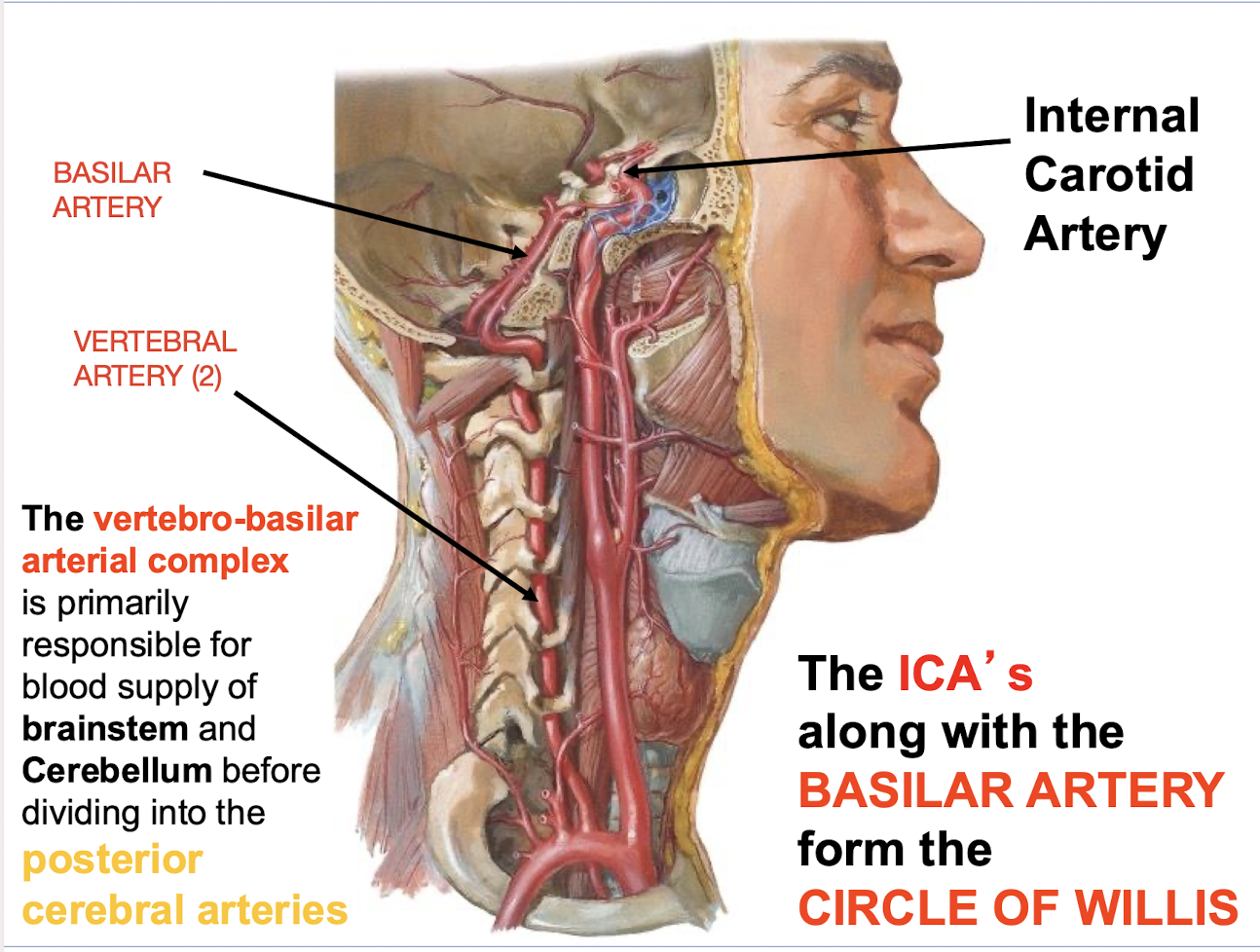
What is the primary responsibility of the vertebro-basilar arterial complex before it divides into the __________
Blood supply of the brainstem and Cerebellum.
divides into the Posterior Cerebral Arteries (PCA)
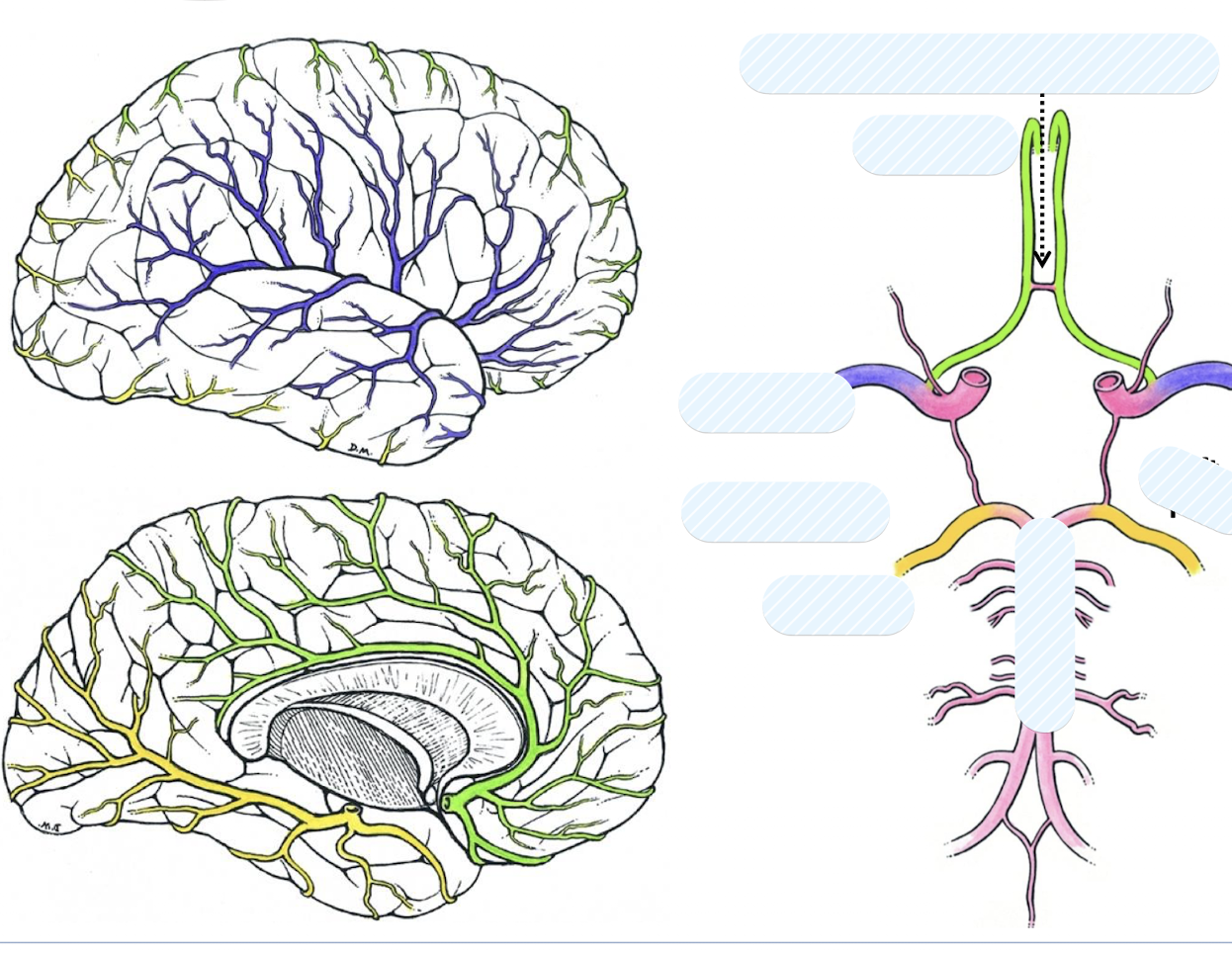
ACA (Anterior Cerebral Artery) 🟩 → medial frontal & parietal lobes
MCA (Middle Cerebral Artery) 🔵 → lateral brain
PCA (Posterior Cerebral Artery) 🟡 → occipital & inferior temporal lobes
ACOM (Anterior Communicating Artery) 🔴 → connects right & left ACA
PCOM (Posterior Communicating Artery) ⚫ → connects ICA (Internal Carotid Artery) ↔ PCA (Posterior Cerebral Artery)
ICA ❤ → gives off ACA & MCA
Basilar Artery 💗 → gives off PCA; formed by vertebral arteries
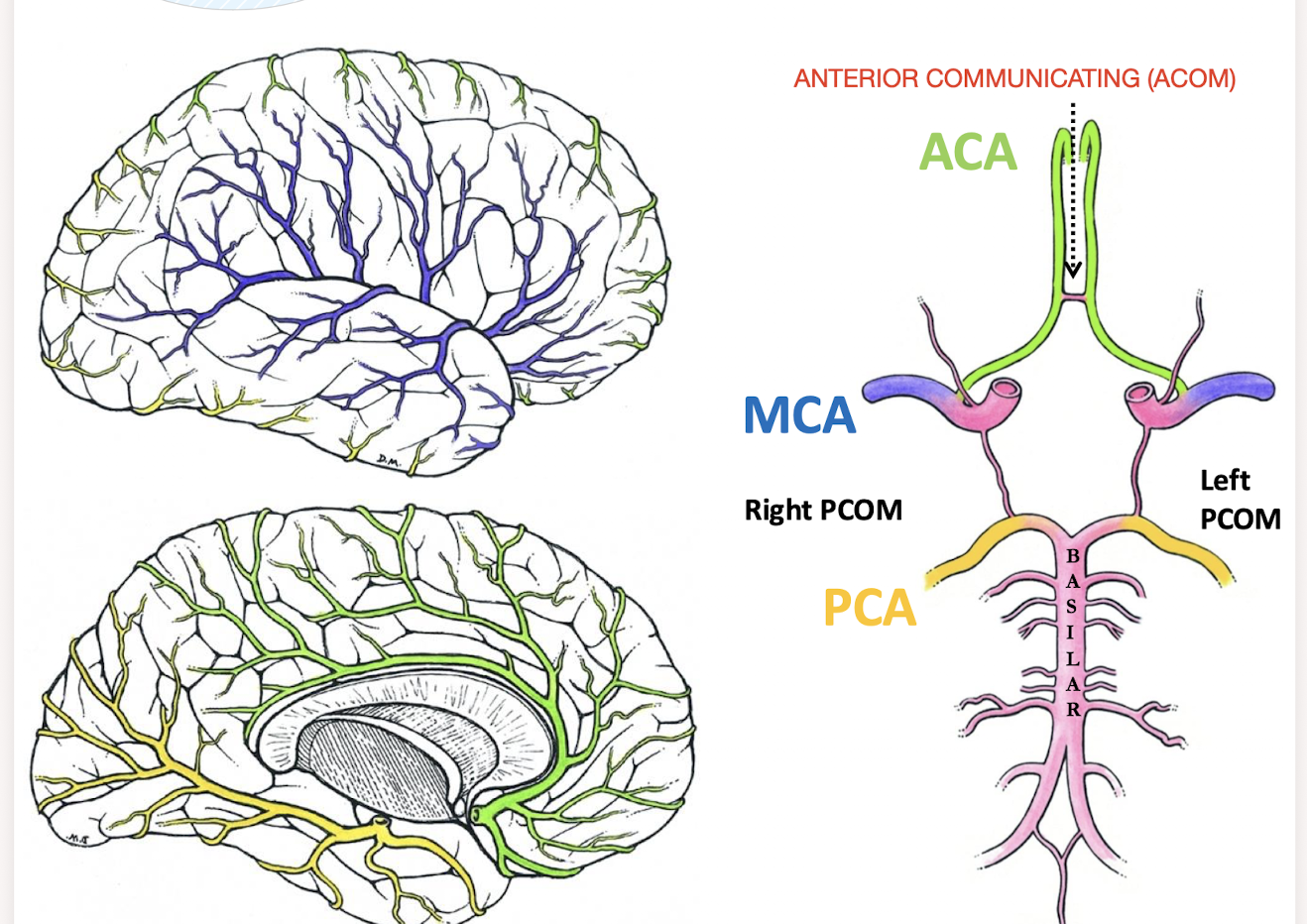
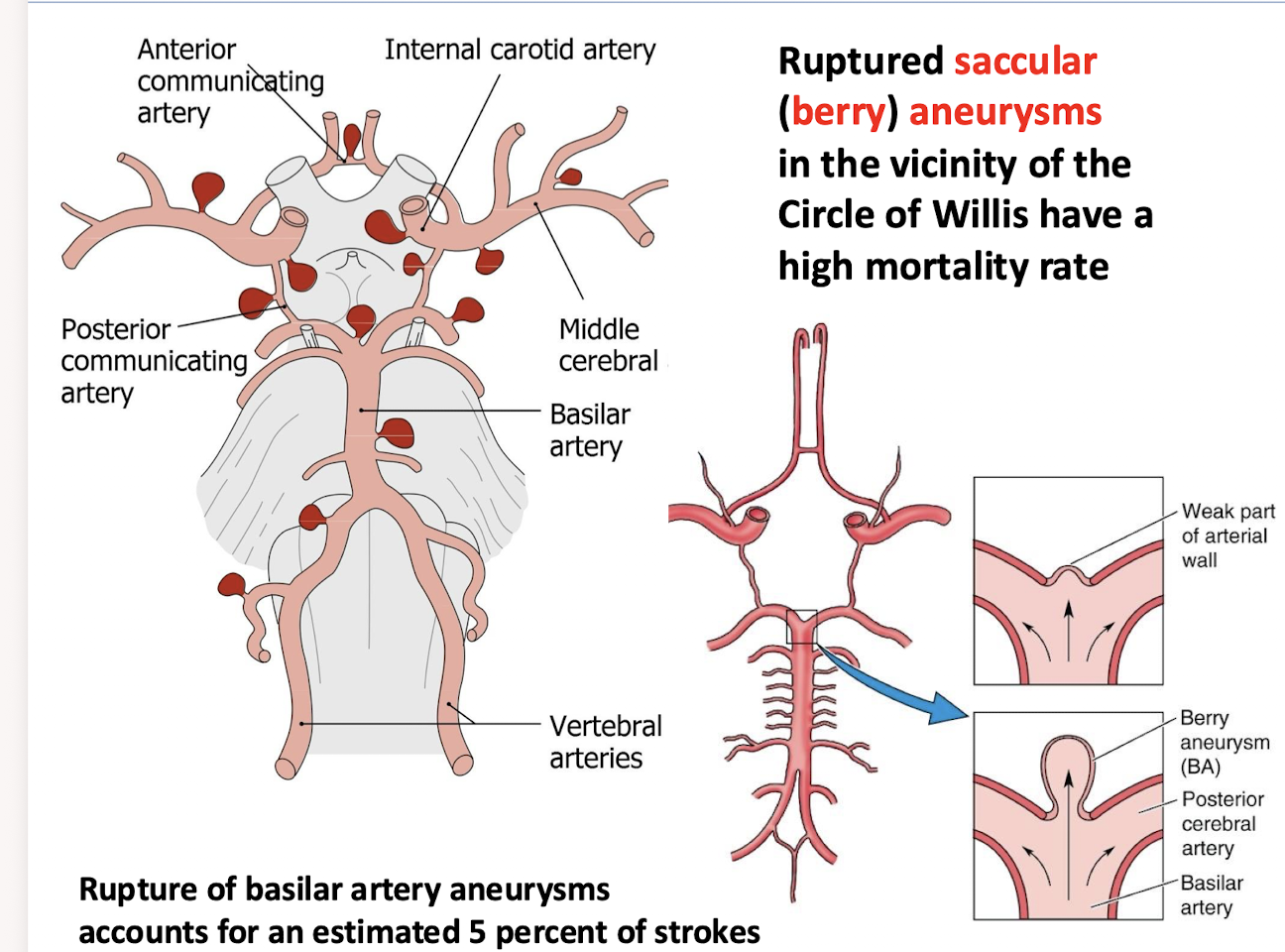
What kind of aneurysms in the vicinity of the Circle of Wilis have a high mortalitity rate. What is the statistic for rupture of basilar artery aneurysms
Ruptured saccular (berry) aneurysms
Rupture of basilar artery anuerysms accounts for an estimated 5 percent of strokes
Where do arteries supplying the brain run?
In the SUBARACHNOID SPACE
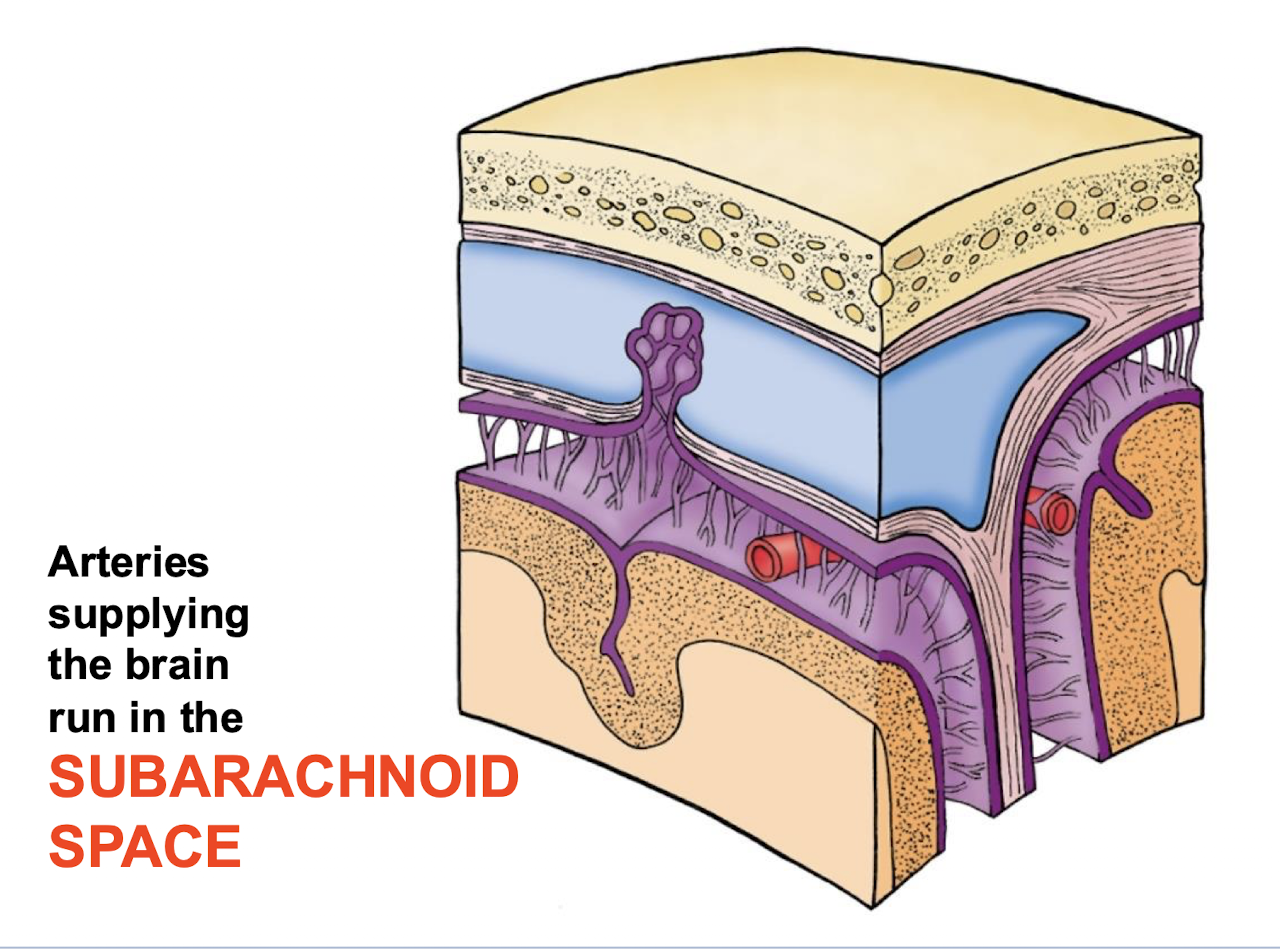
What type of hemorrhage may result from head trauma or rupture of an aneurysm or an AVM (Arteriovenous Malformartion) near the CIRCLE OF WILLIS?
SUBARACHNOID HEMORRHAGE. Starts as the “worst headache ever”
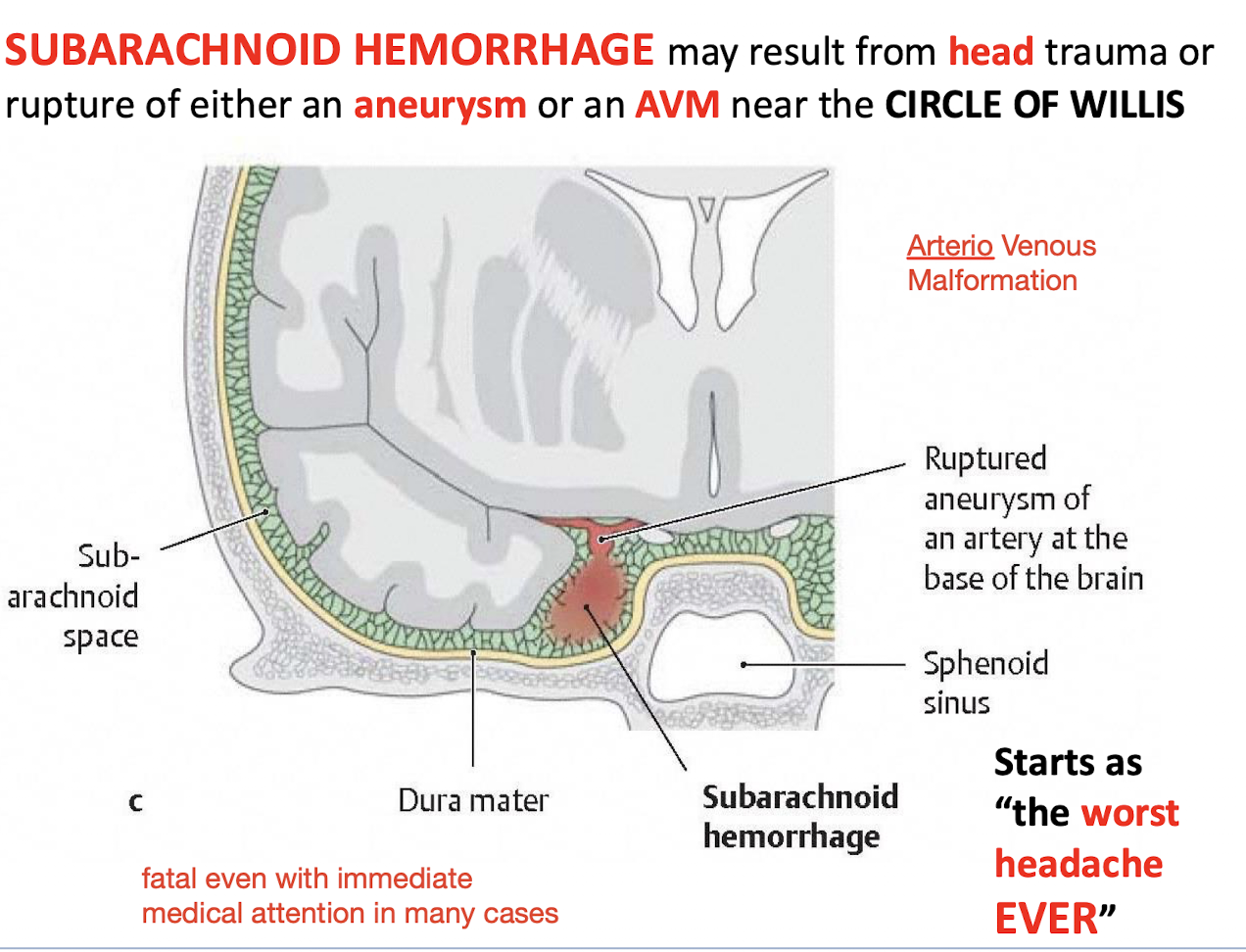
A patient reports a sudden onset of “the worst headache of my life”; what serious vascular event is suggested?
Rupture of a saccular (berry) aneurysm near the CIRCLE OF WILLIS (Subarachnoid Hemorrhage).
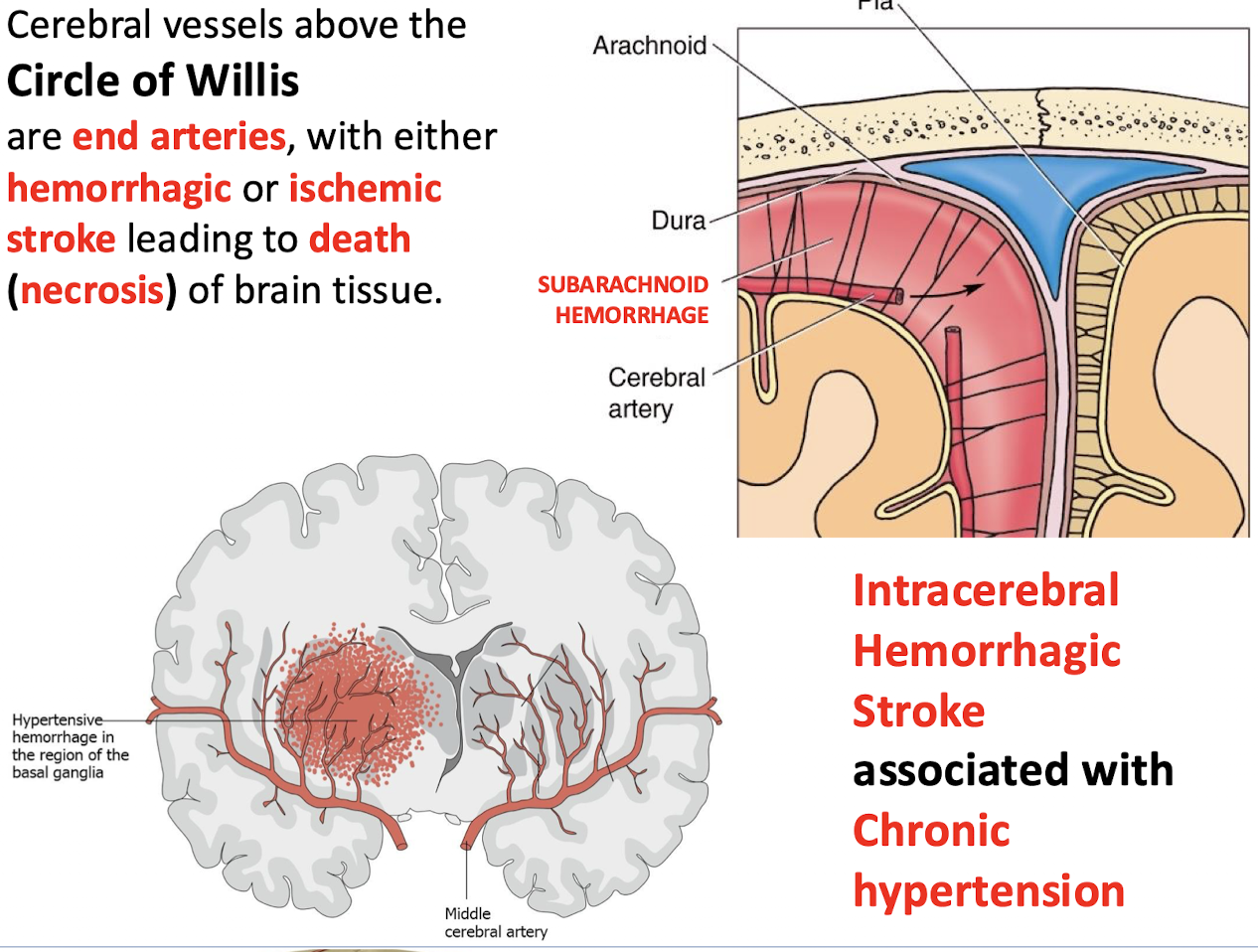
What type of arteries are the vessels above the circle of willis and what is the clinical consequence when the artieries suffer ischemic stroke?
Cerebral vessels above the Circle of Willis are end arteries. The Circle of Willis is the ring at the base, and the ACA, MCA, and PCA are the main arteries that branch upward above it to feed the brain.
The result is Death (necrosis) of brain tissue
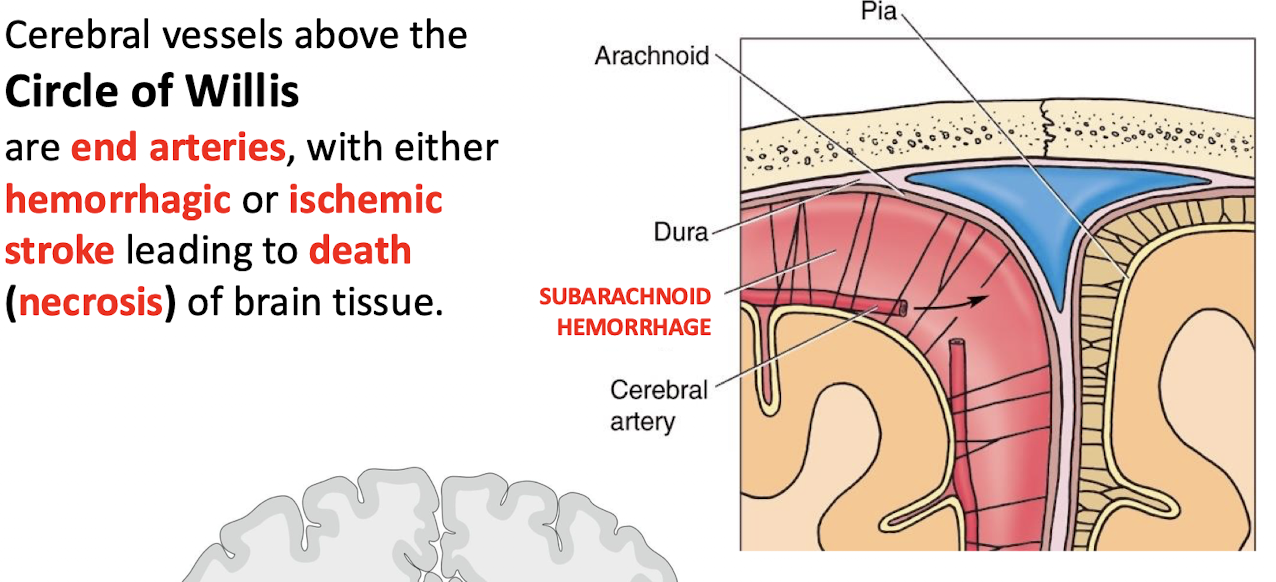
What condition is intracerebral hemorrhagic stroke associated with?
Chronic hypertension
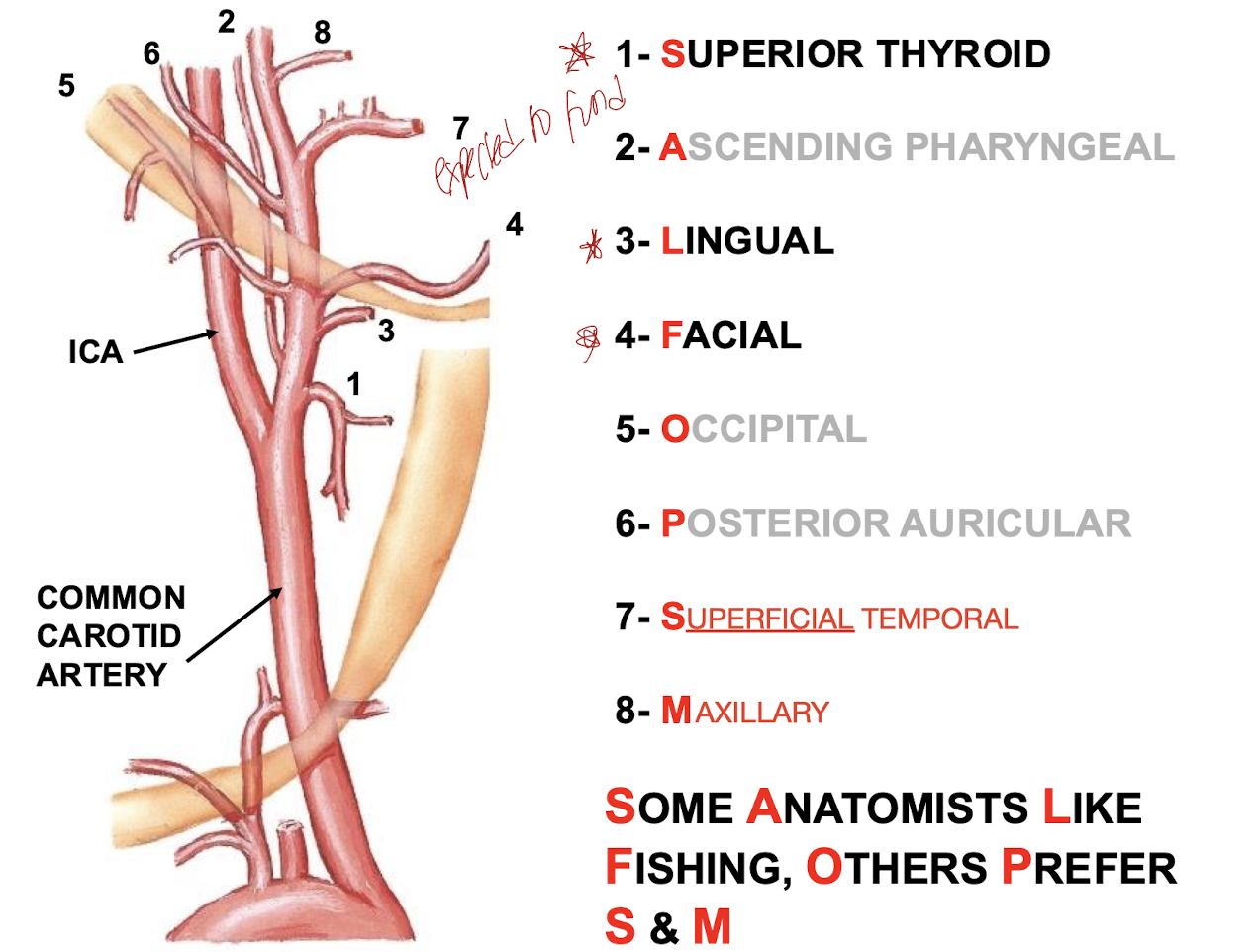
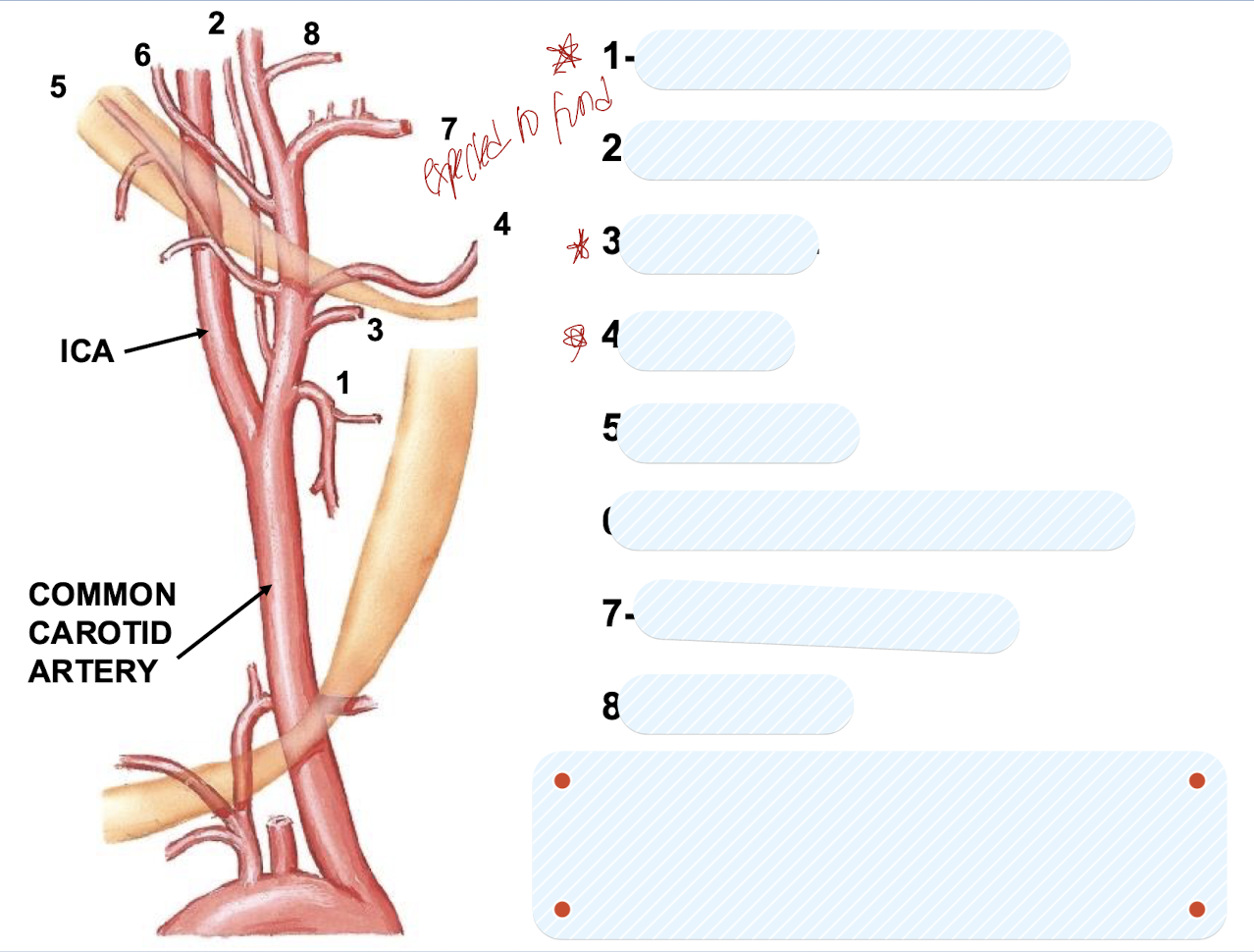
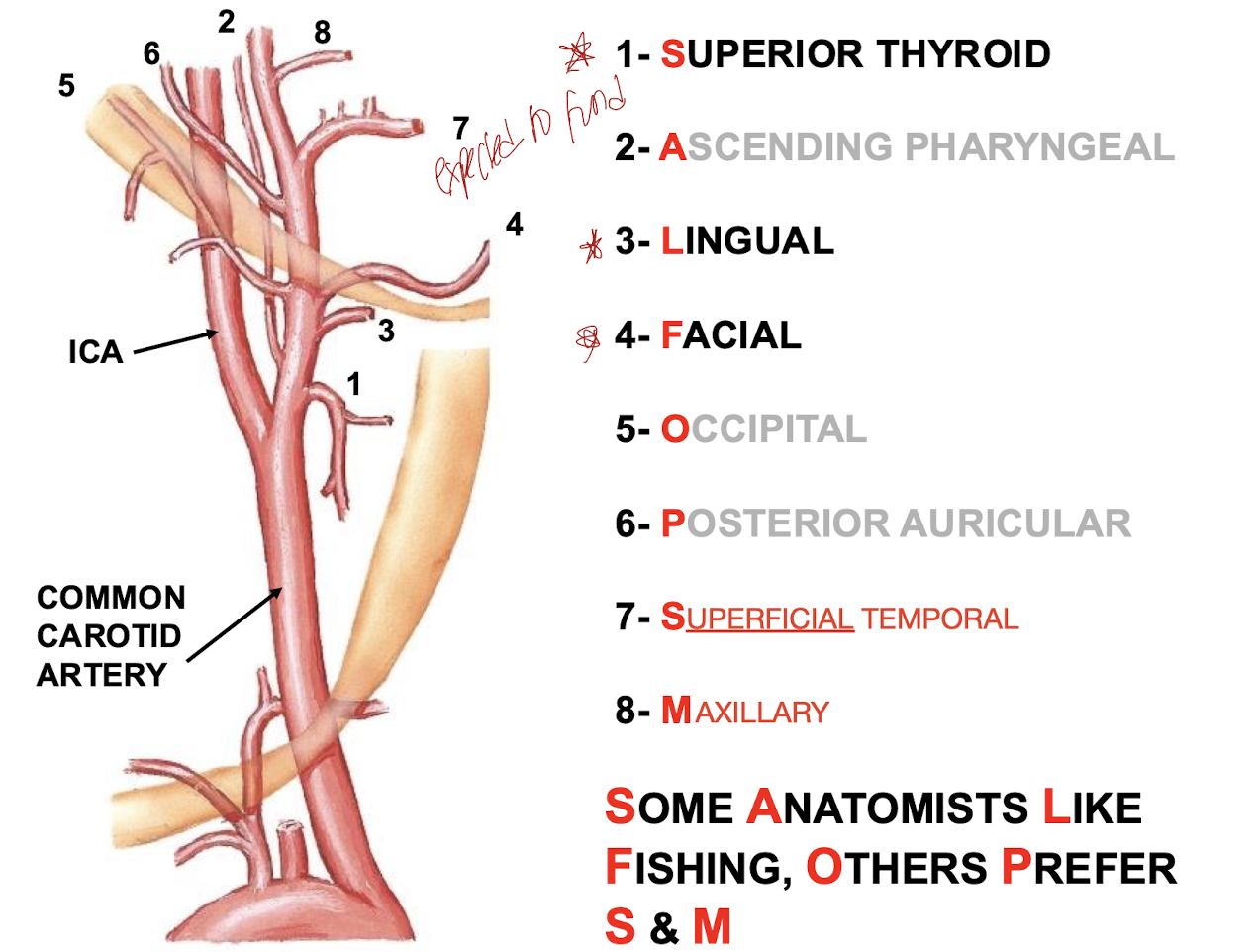
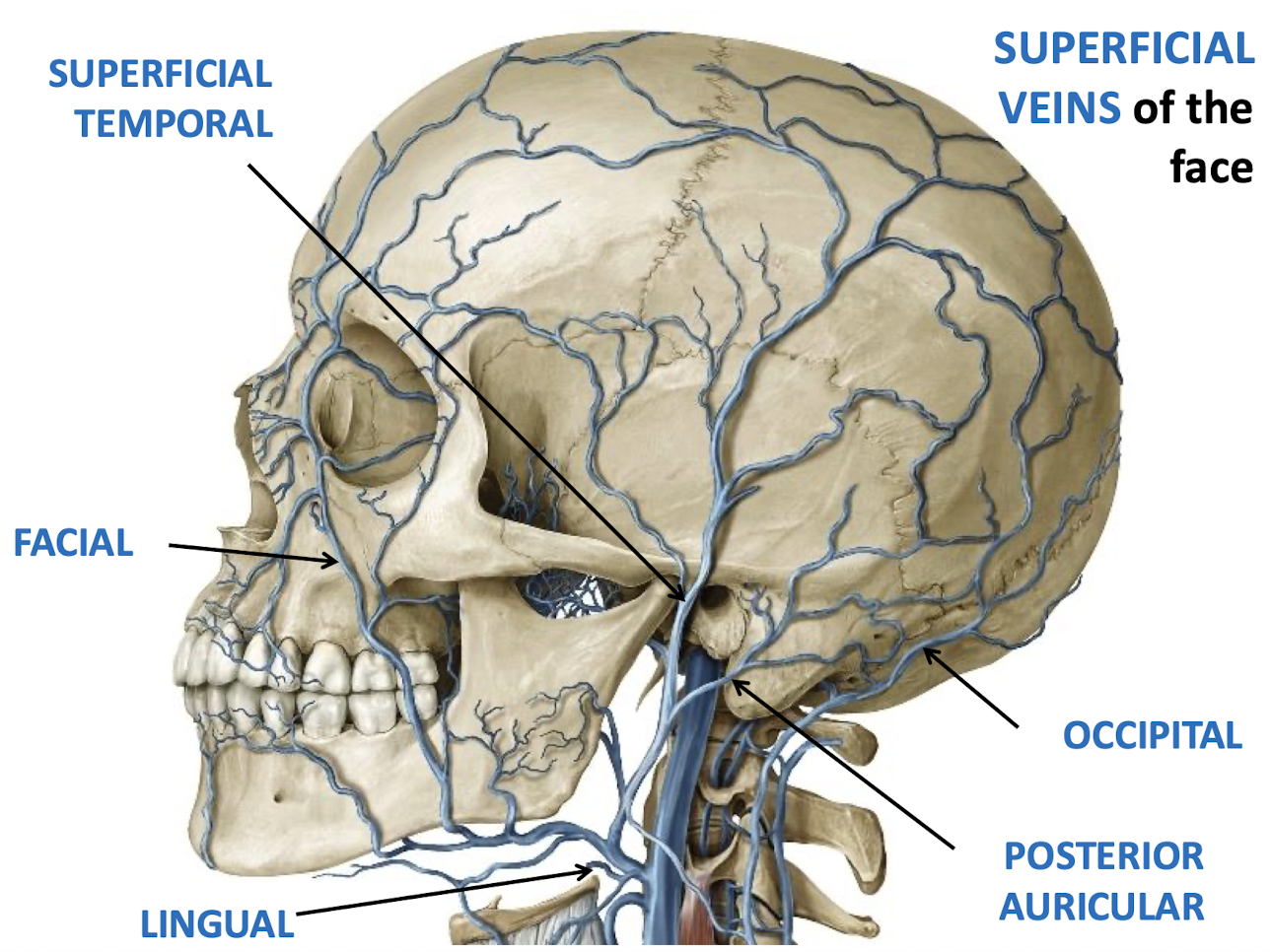
How many branches does the EXTERNAL CAROTID ARTERY have; and what areas do they supply?
Eight branches; that supply blood to the superficial neck and face as well as the contents of the viscerocranial cavities.
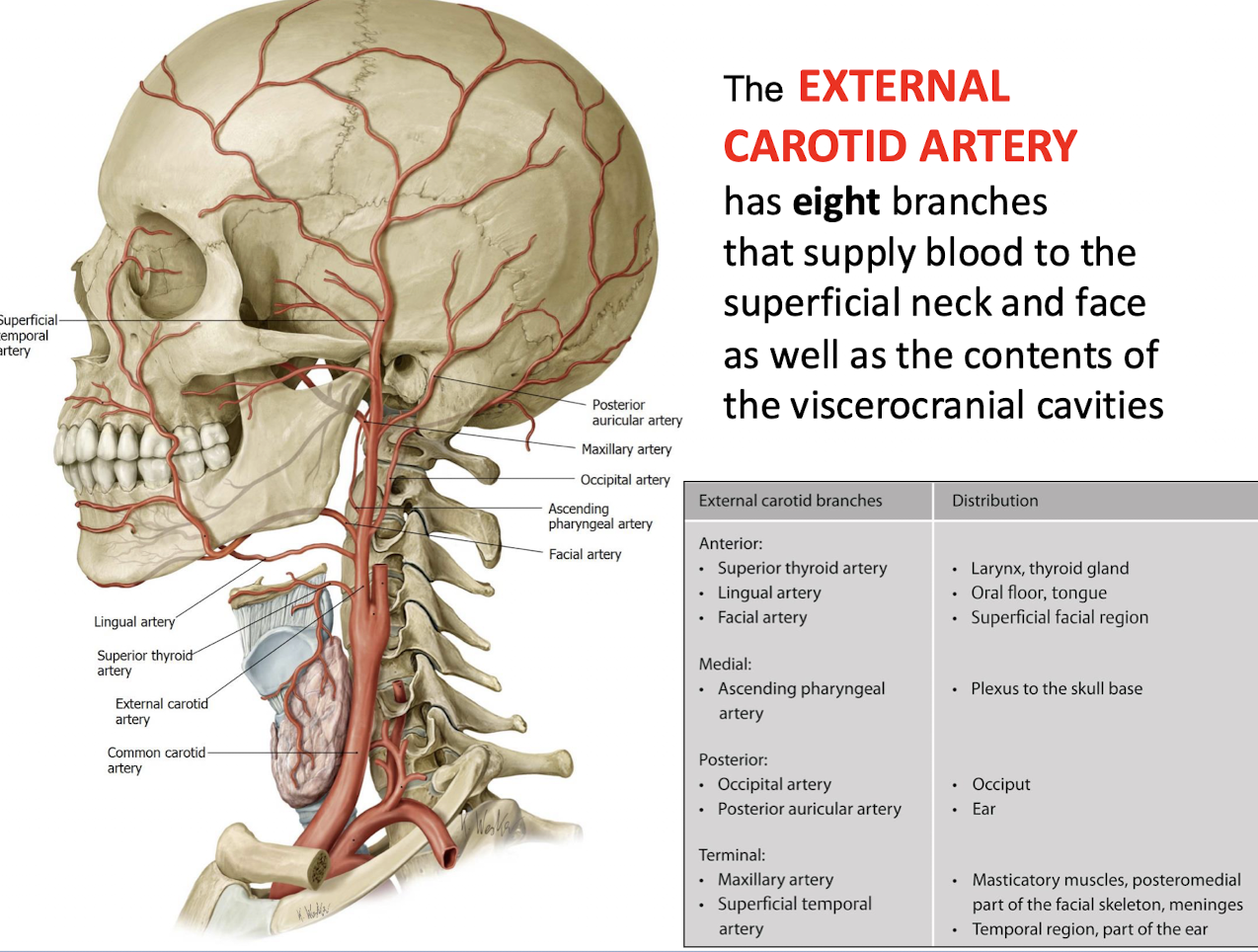
List the eight branches of the External Carotid Artery (ECA).
1- SUPERIOR THYROID;
2- ASCENDING PHARYNGEAL;
3- LINGUAL;
4- FACIAL;
5- OCCIPITAL;
6- POSTERIOR AURICULAR;
7- SUPERFICIAL TEMPORAL;
8- MAXILLARY
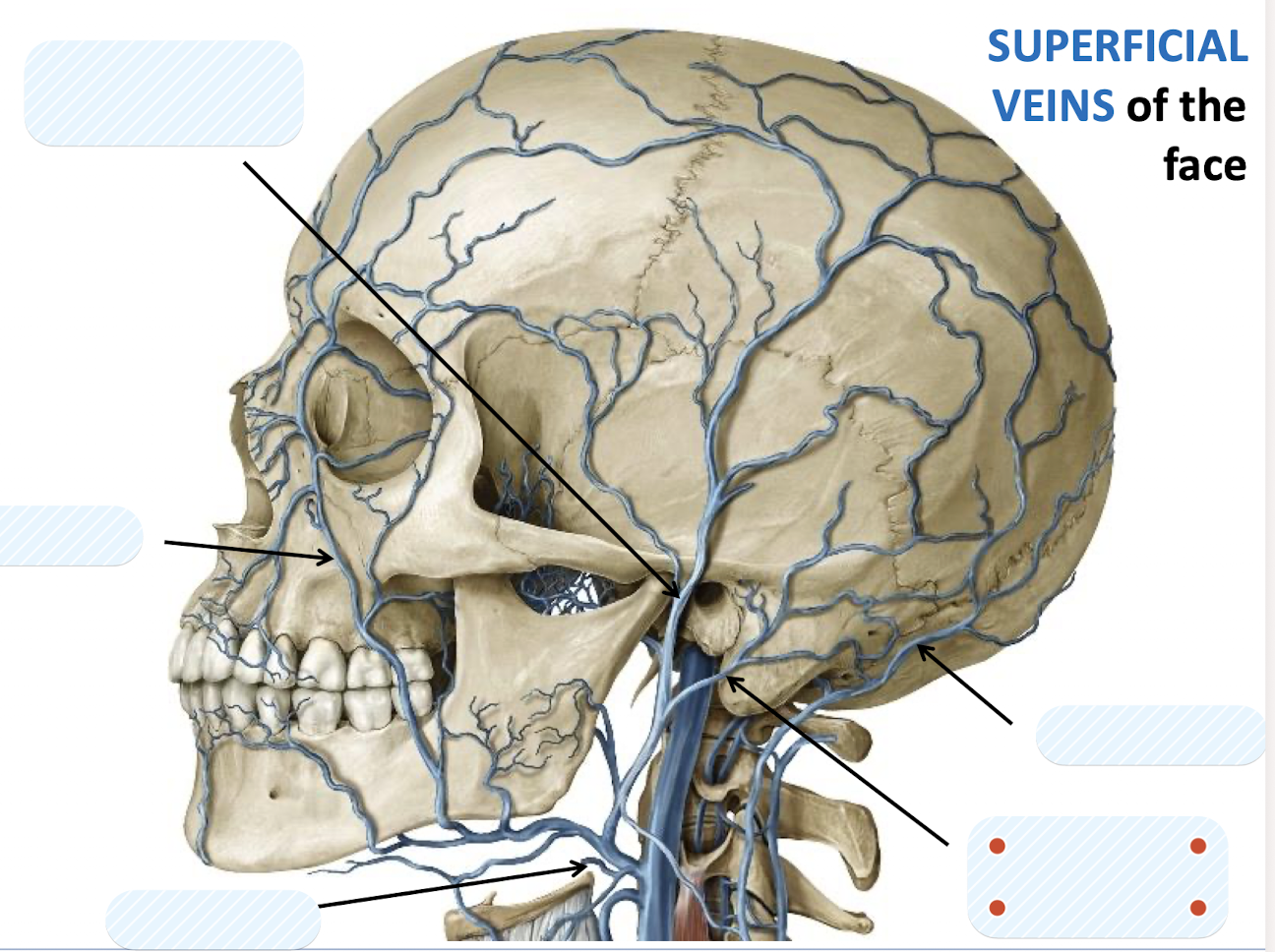
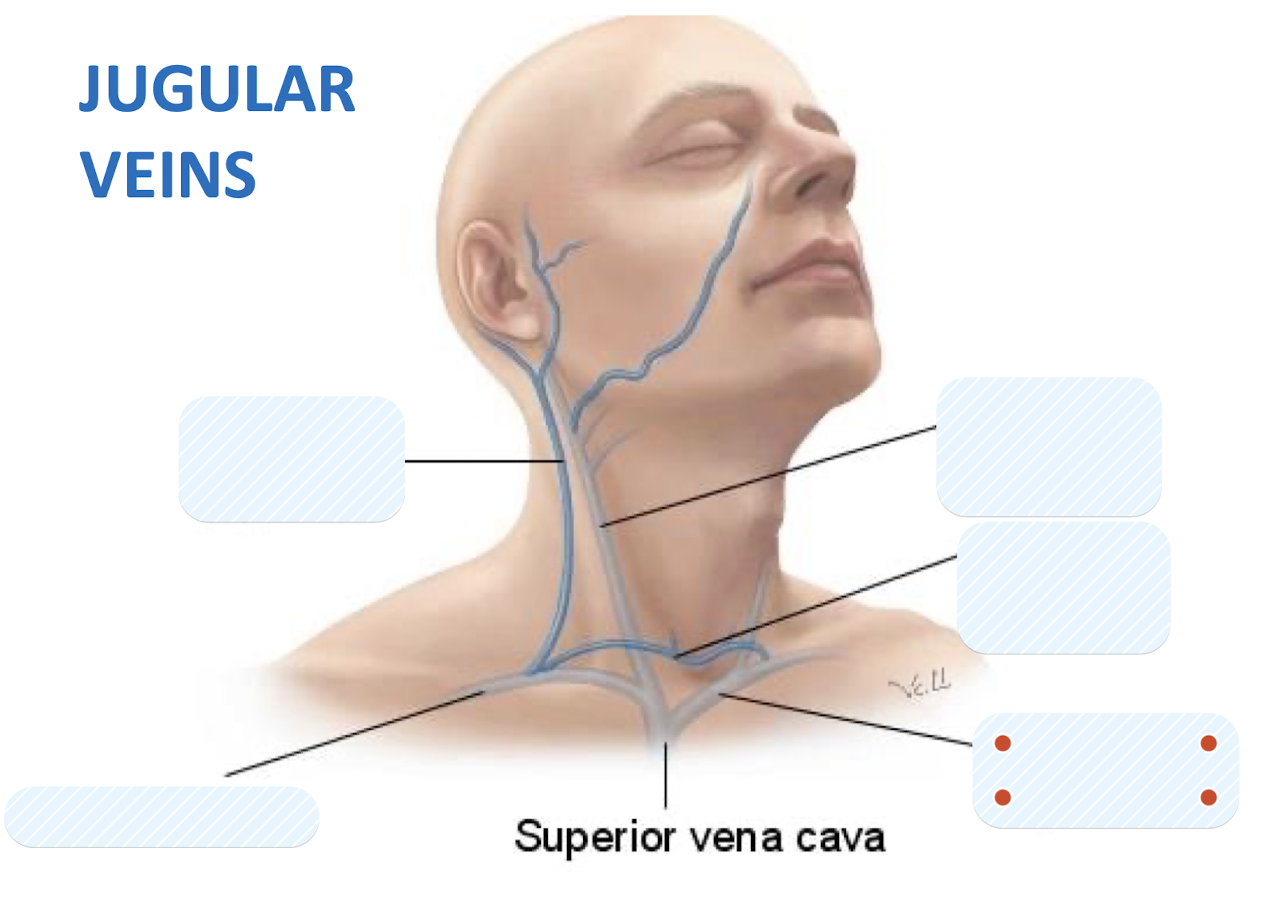
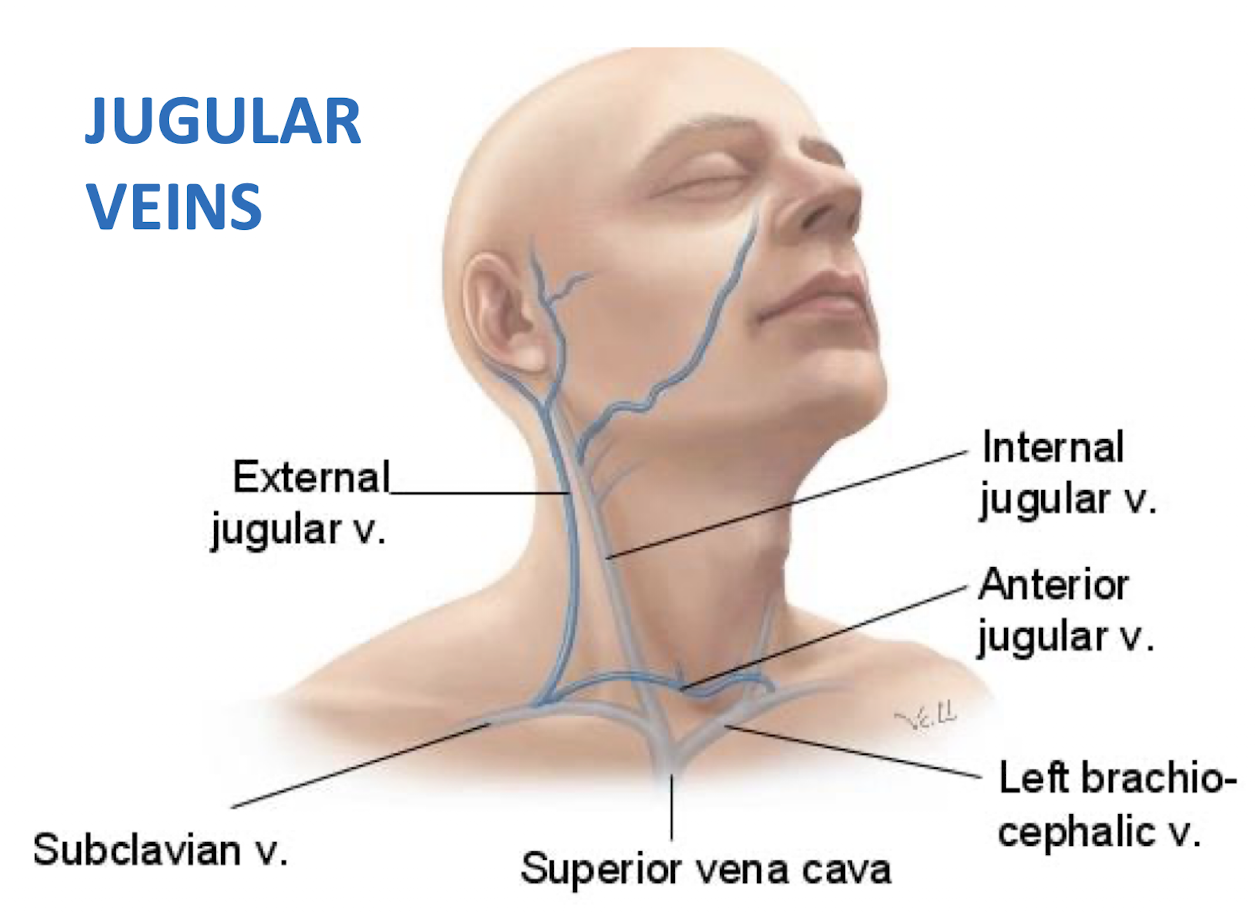
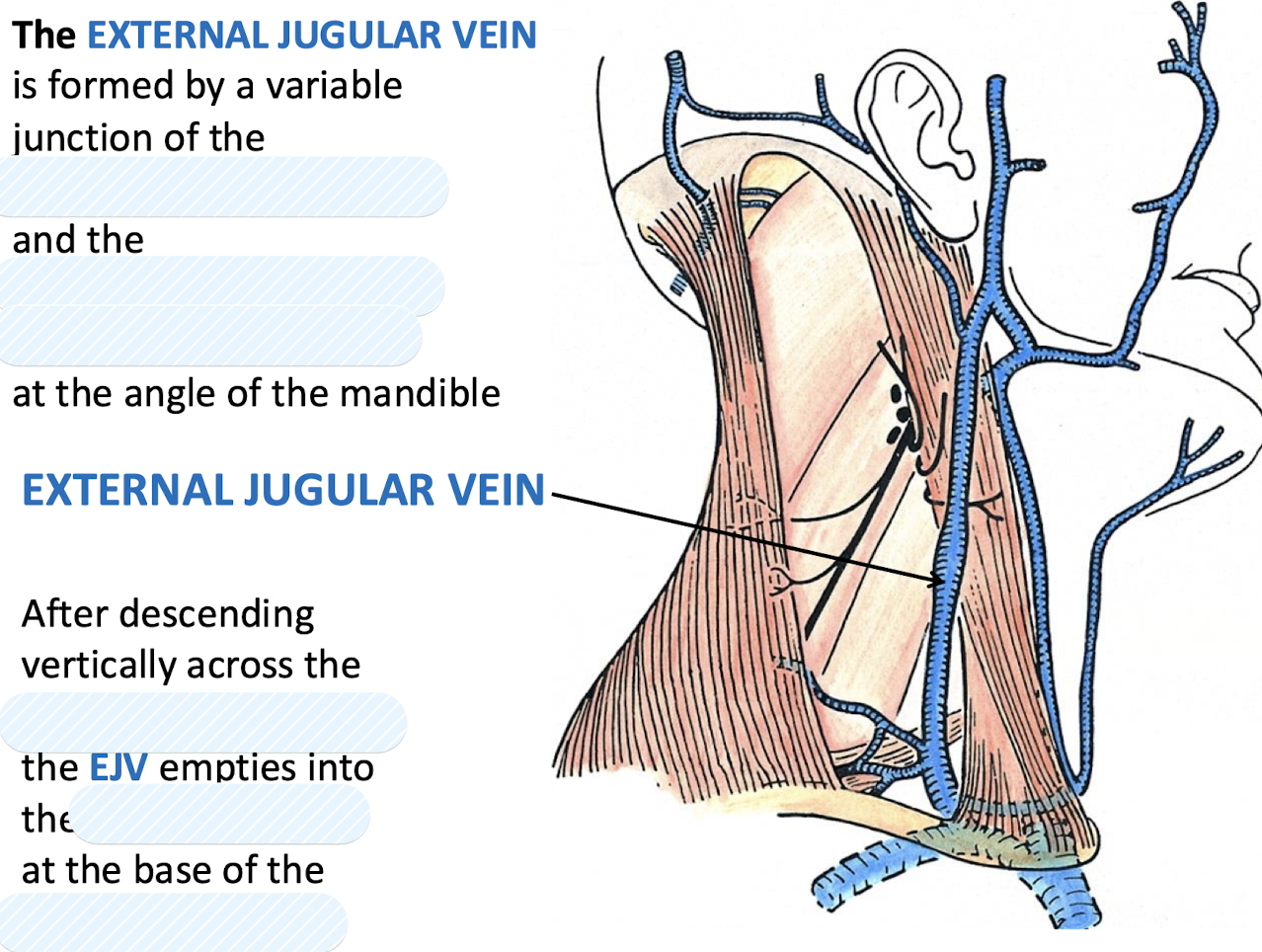
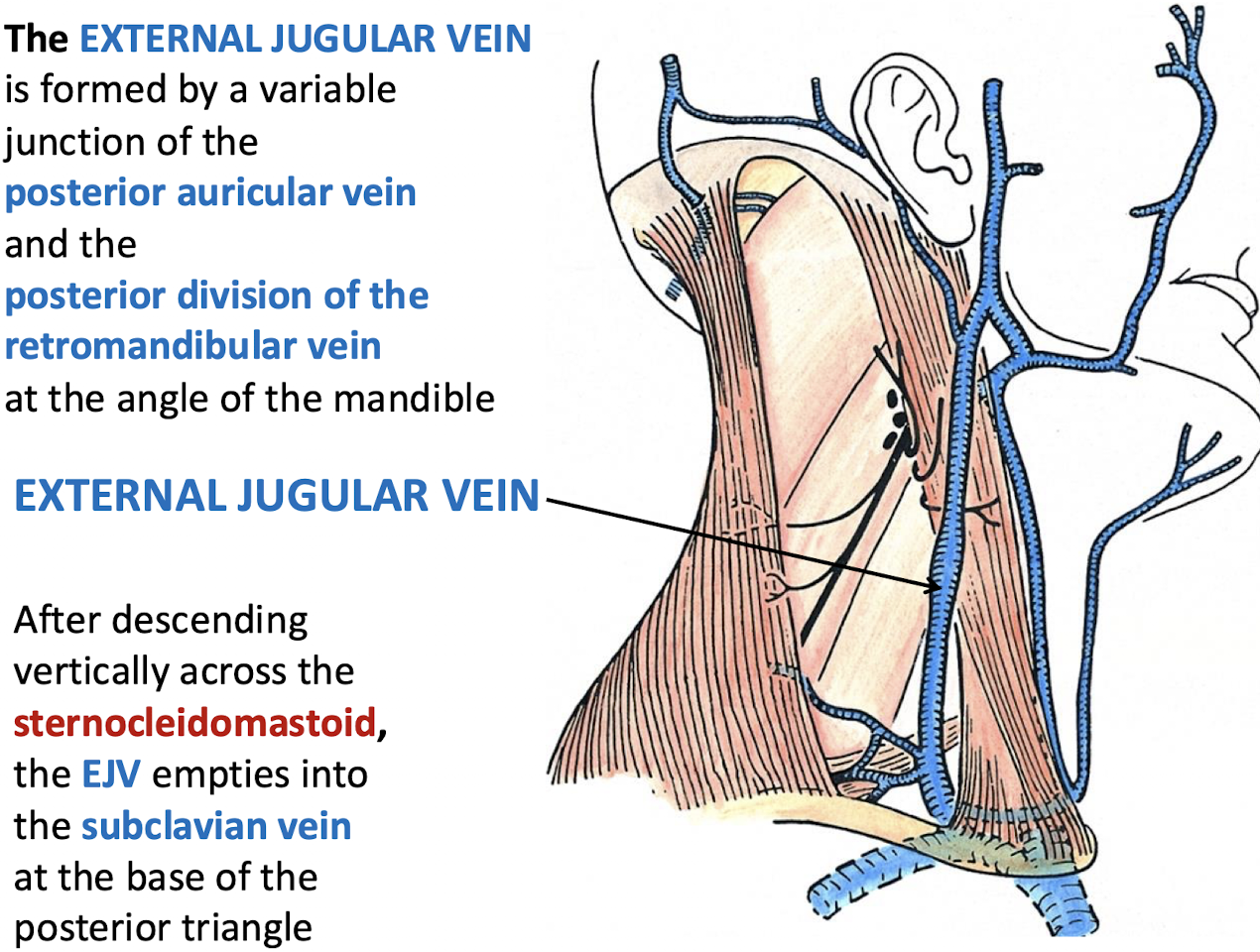
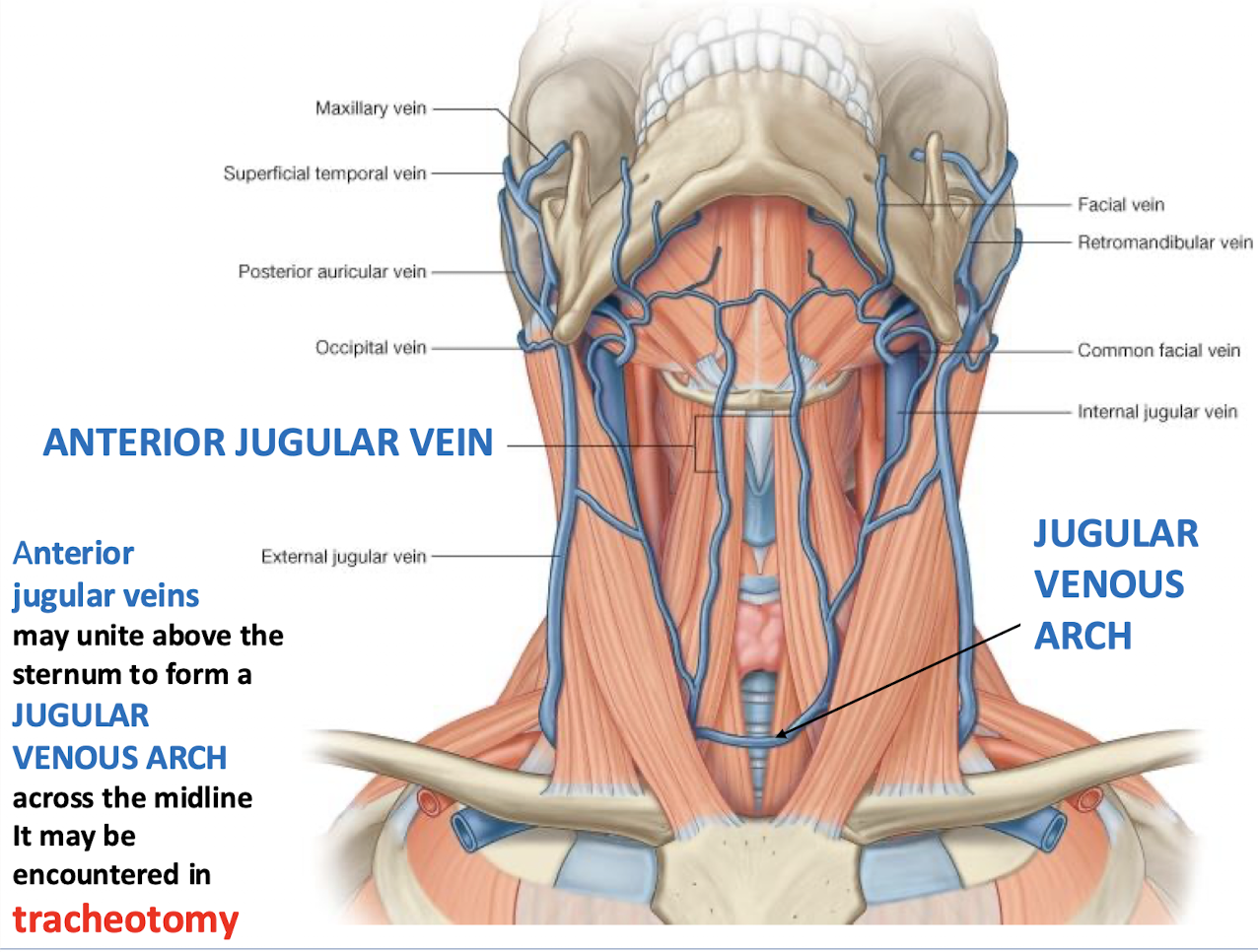
What structure may anterior jugular veins form and what is its clinical significance?
The AJV may unite above the sternum to form a JUGULAR VENOUS ARCH across the midline which may be encountered in tracheotomy
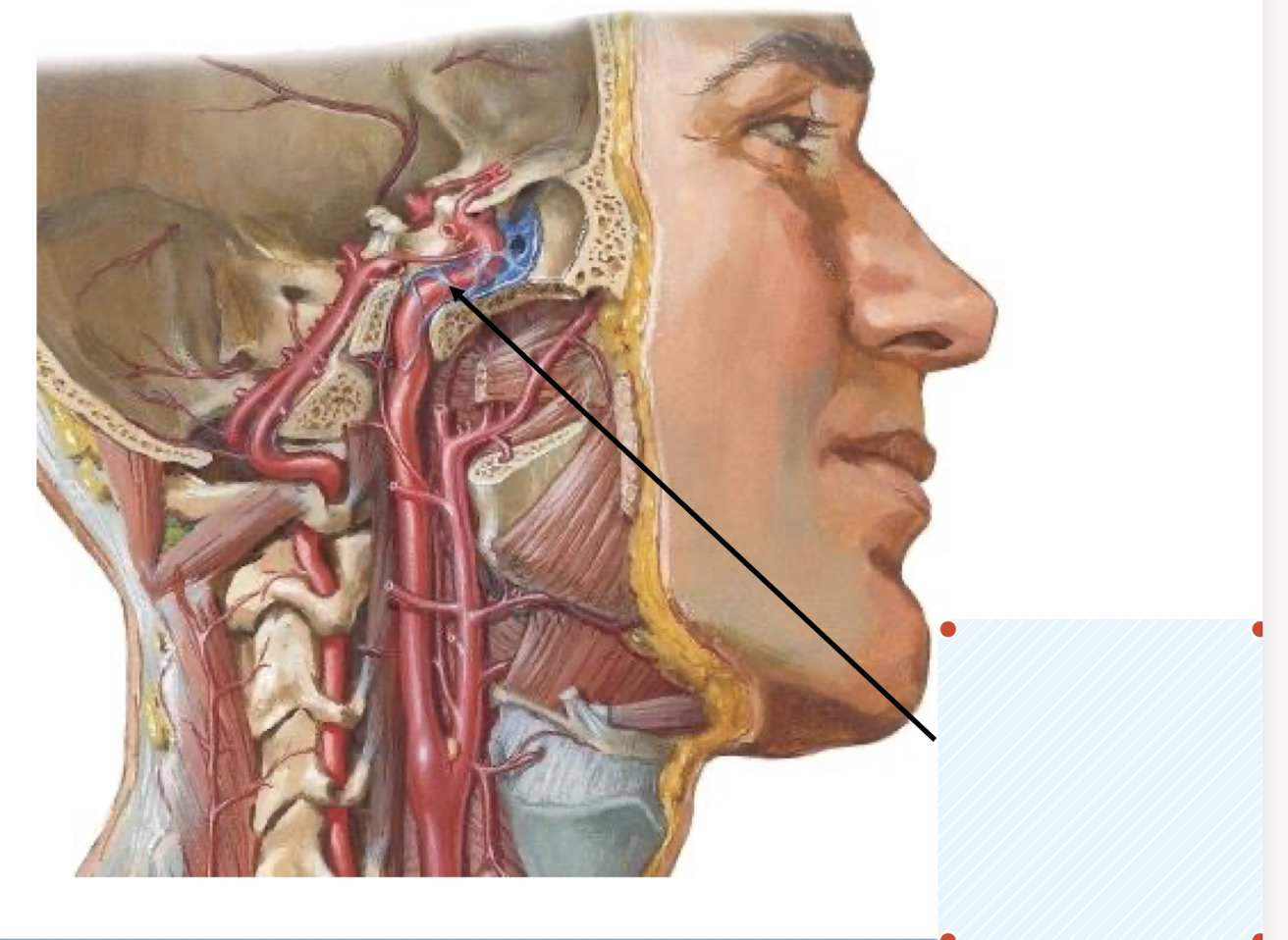
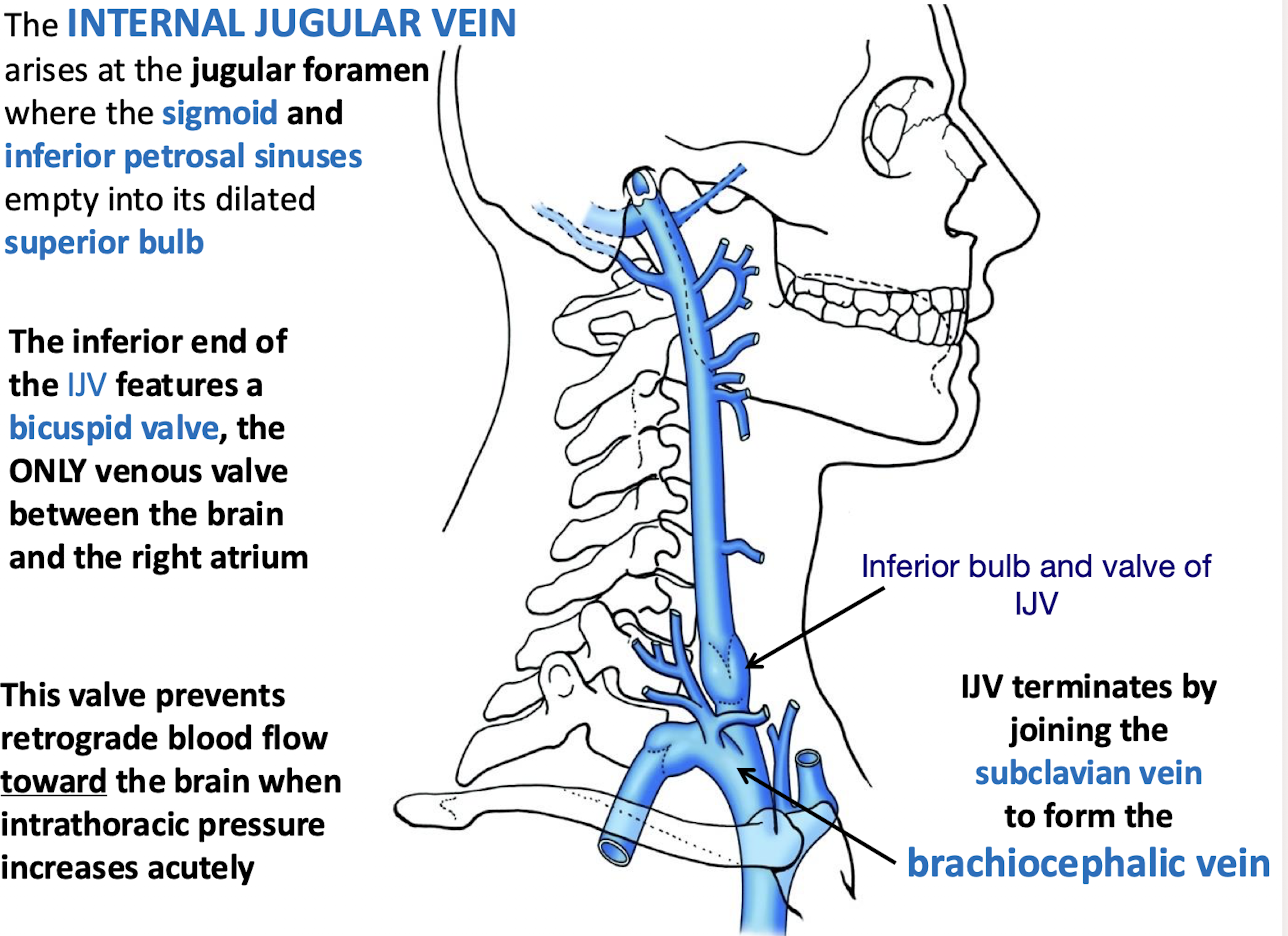
Where does the INTERNAL JUGULAR VEIN (IJV) arise? What empties into it?
At the jugular foramen where the sigmoid and inferior petrosal sinuses empty into its dilated superior bulb.

The inferior end of the IJV features the ONLY venous valve between the brain and the right atrium; what type of valve is it; and what is its function?
It is a bicuspid valve; which prevents retrograde blood flow toward the brain when intrathoracic pressure increases acutely.
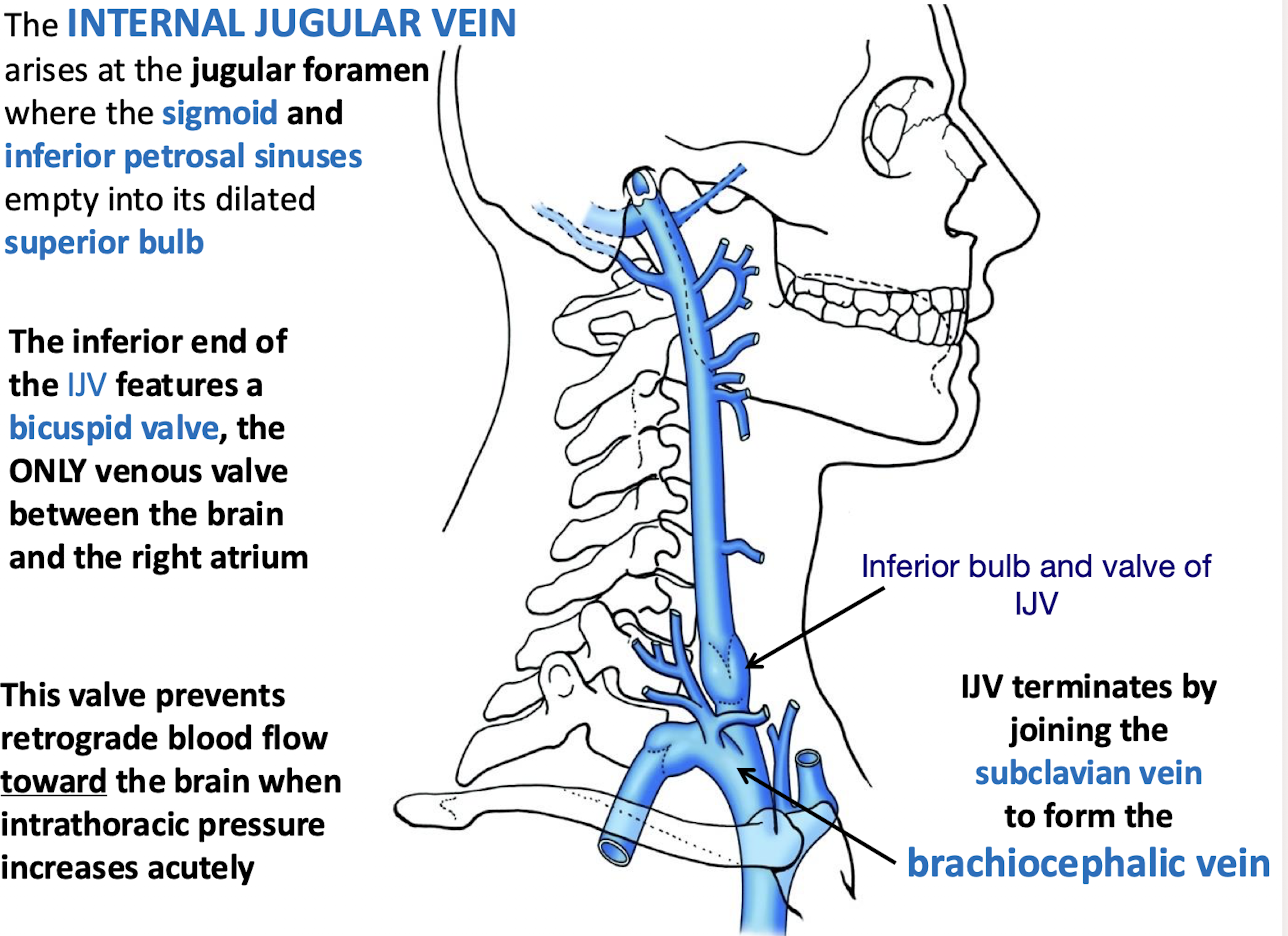
How does the IJV terminate?
By joining the subclavian vein to form the brachiocephalic vein
What causes external jugular vein (EJV) distension?
Right-sided heart failure (cor pulmonale) → ↑ right atrial pressure → blood backs up into SVC (superior vena cava constriction) and EJV becomes engorged.
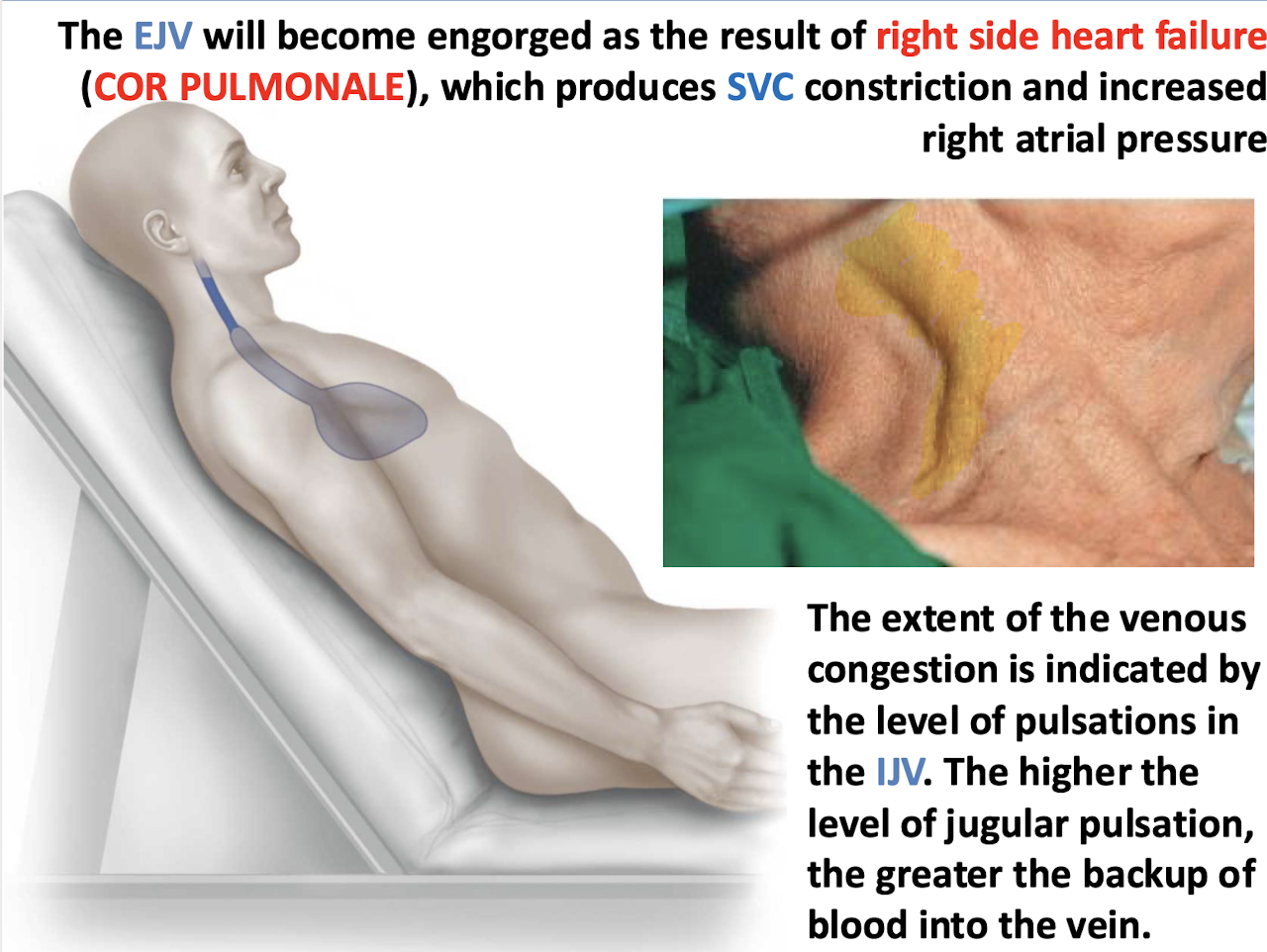
What does elevated internal jugular vein (IJV) pulsation indicate?
Venous congestion and increased right atrial pressure — the higher the jugular pulsation, the worse the backup of blood.
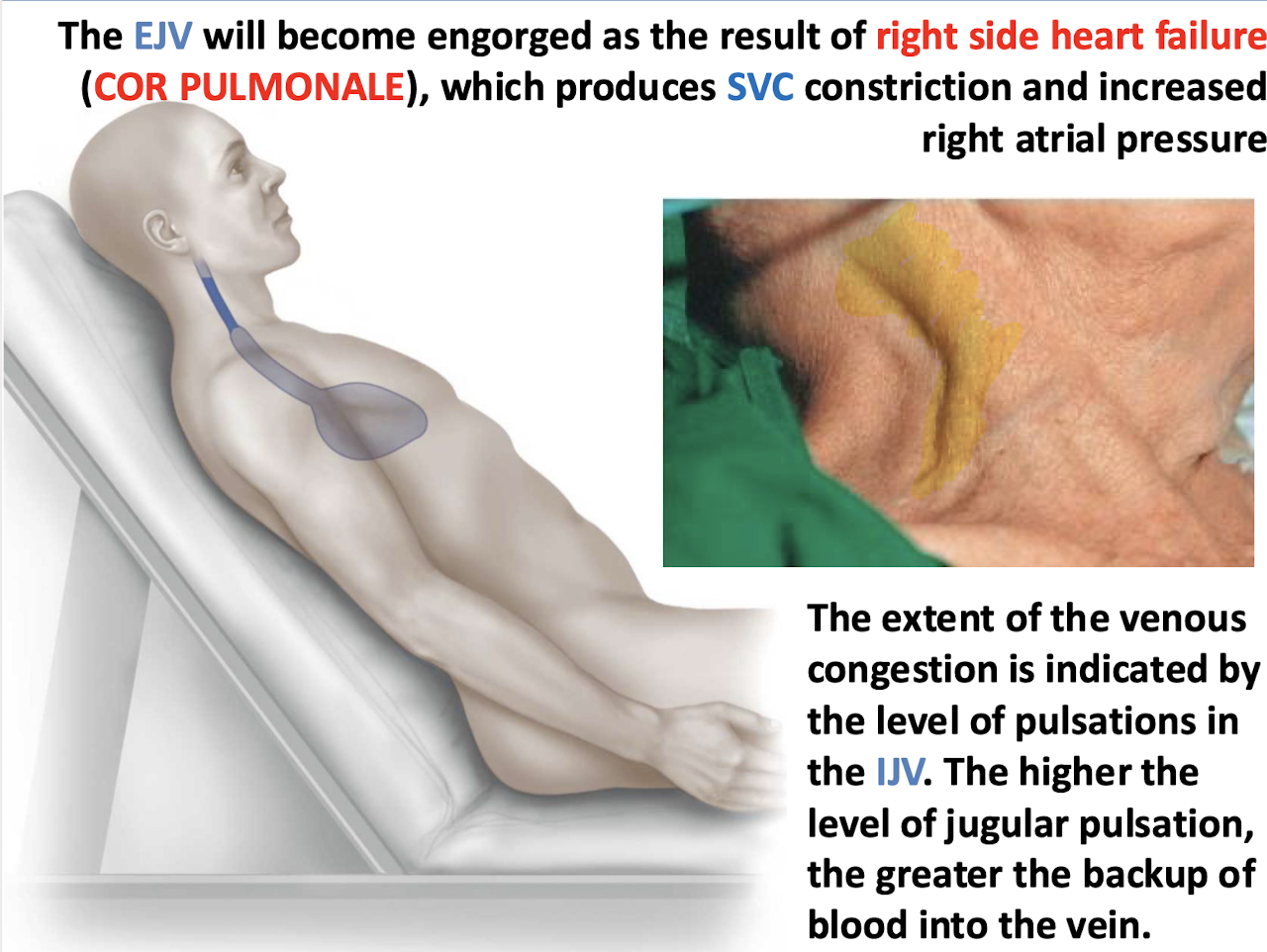
What is the clinical significance of jugular venous distension (JVD)?
It’s a visible sign of elevated right atrial pressure, often due to right-sided heart failure or SVC obstruction.
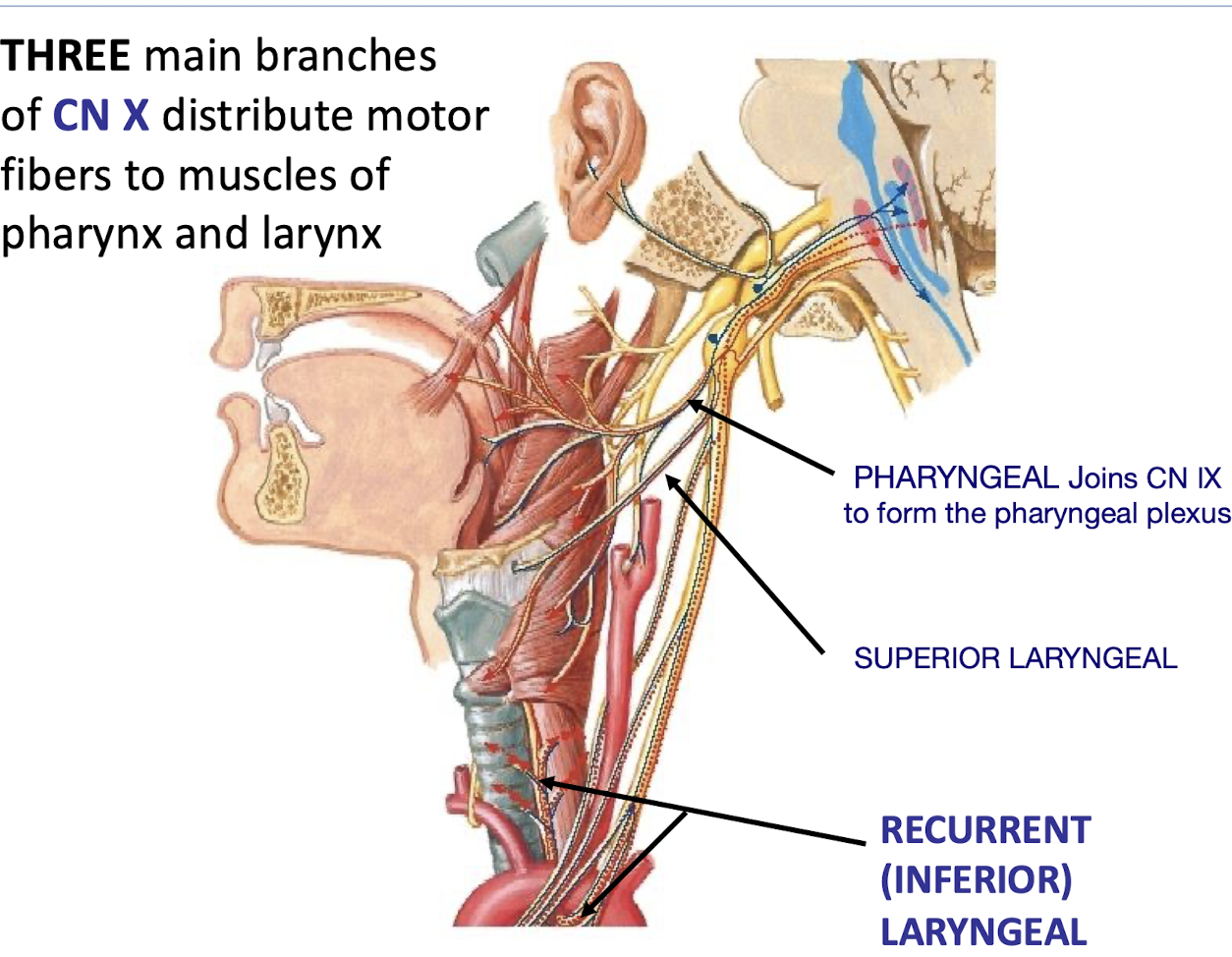
What cranial nerve courses through the carotid sheath along with the major vessels?
The VAGUS NERVE (CN X)
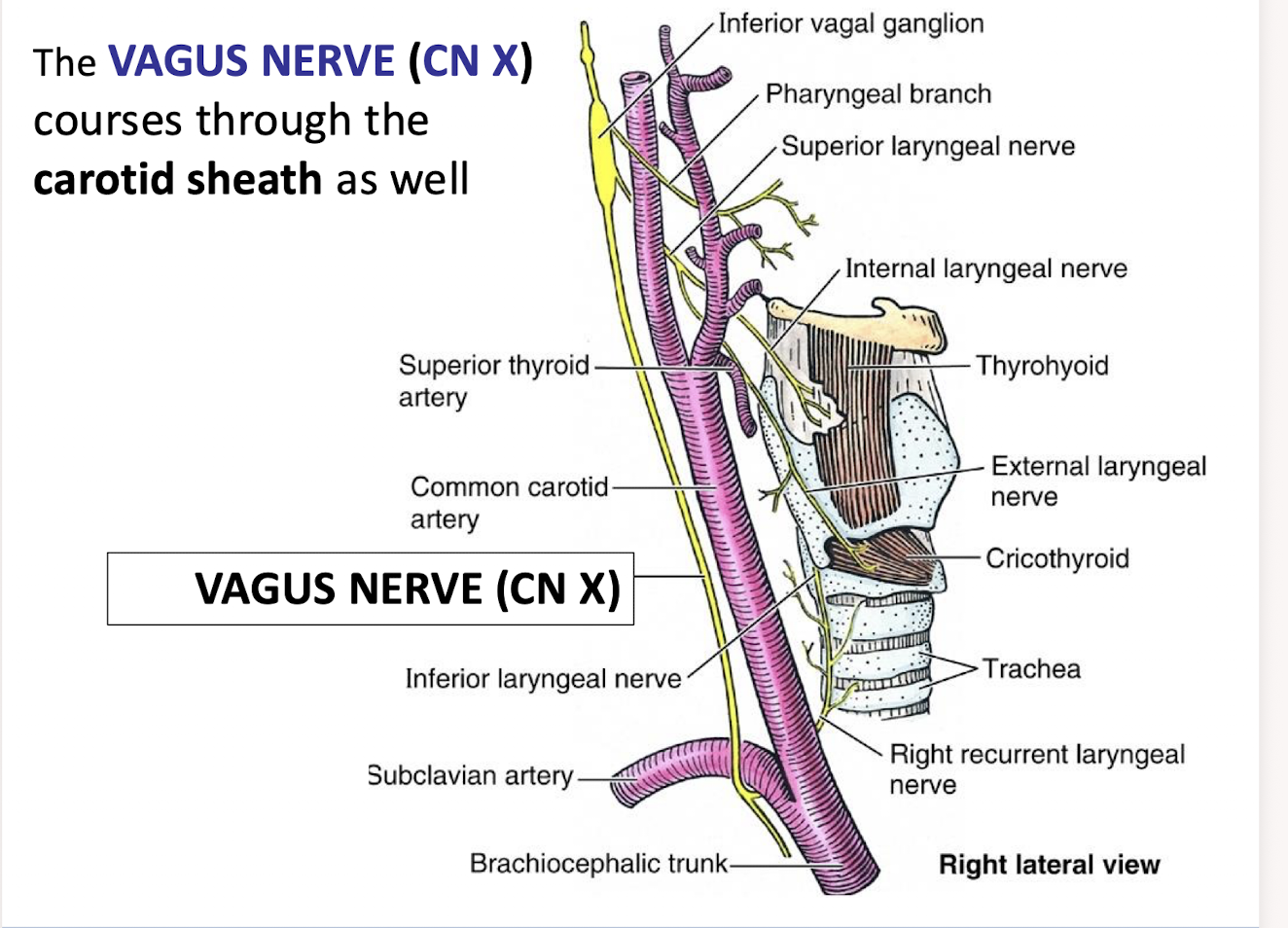
What are the THREE main branches of CN X that distribute motor fibers to muscles of the pharynx and larynx?
RECURRENT (INFERIOR) LARYNGEAL; PHARYNGEAL (joins CN IX) to form pharyngeal plexus; SUPERIOR LARYNGEAL.
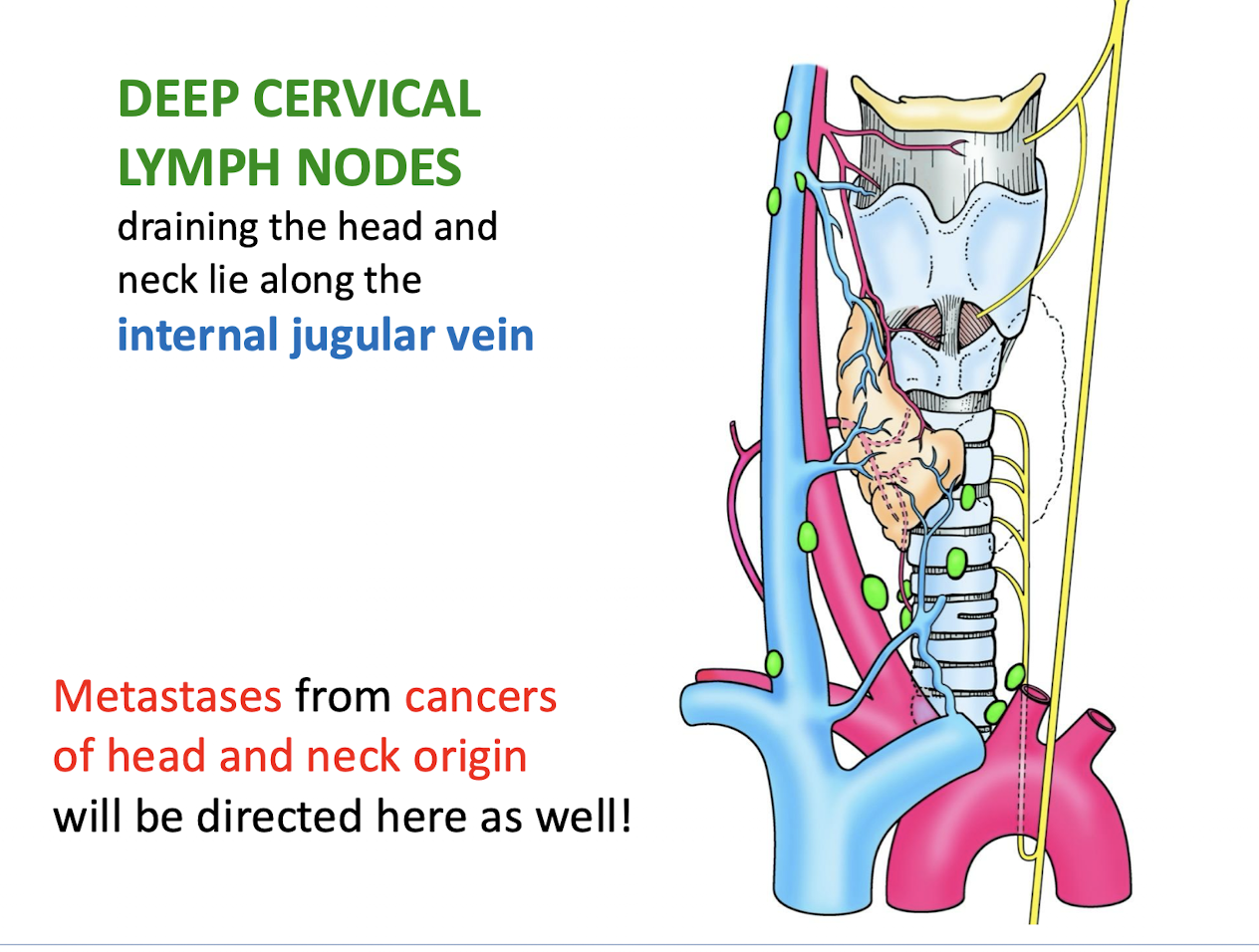
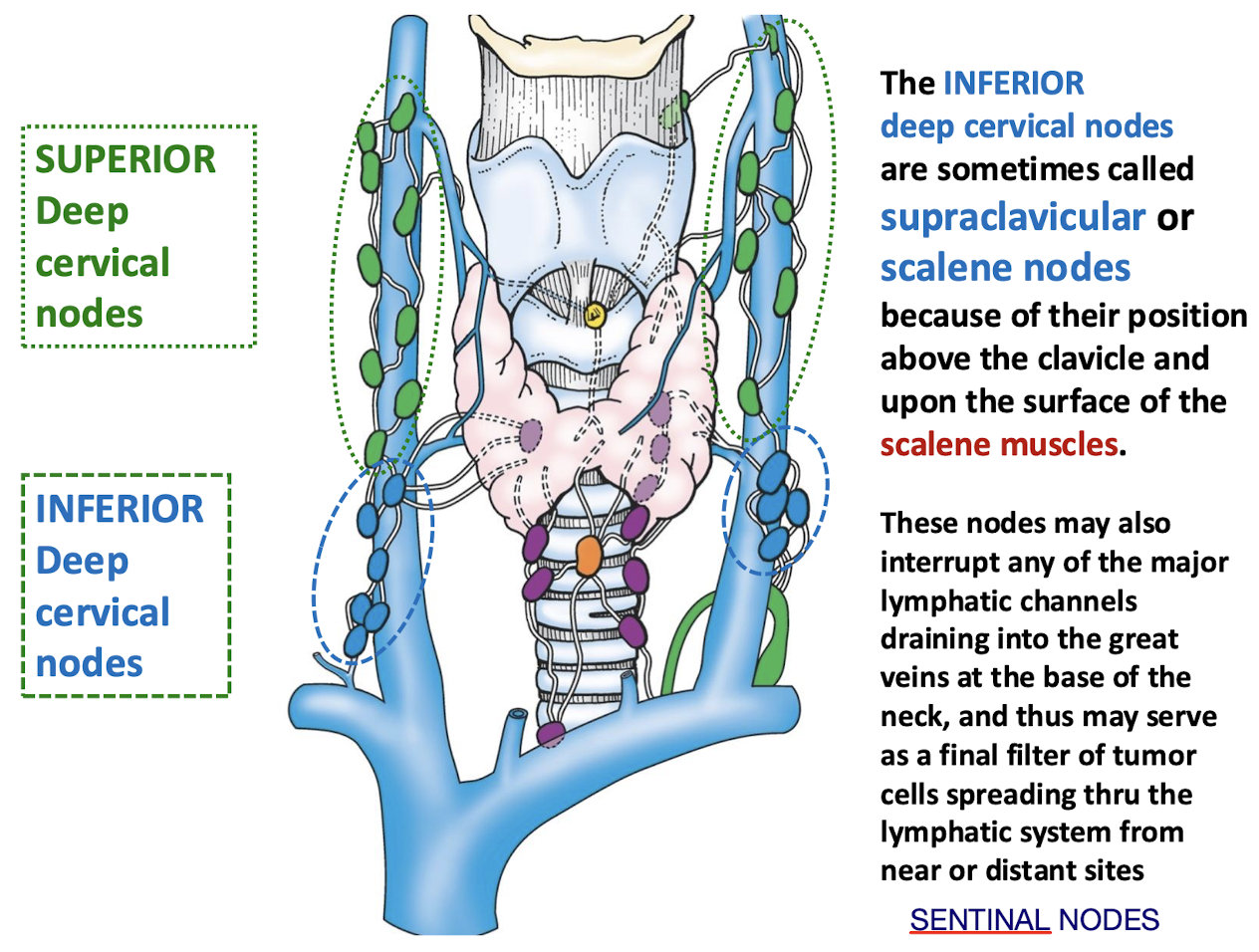
Where do the DEEP CERVICAL LYMPH NODES draining the head and neck lie? What is the clinical consequence?
Along the internal jugular vein. Metastases from cancers of head and neck origin will be directed here as well.
Meaning If there’s a cancer in the head or neck, it often spreads (metastasizes) to these nodes first.
What regions of the lymphatics drain to the deep cervical lymph nodes? How?
Ultimately ALL lymphatics of the HEAD AND NECK drain to the deep cervical lymph nodes along the carotid sheath.
Either directly from tissues or indirectly through groups of outlying regional lymph nodes.
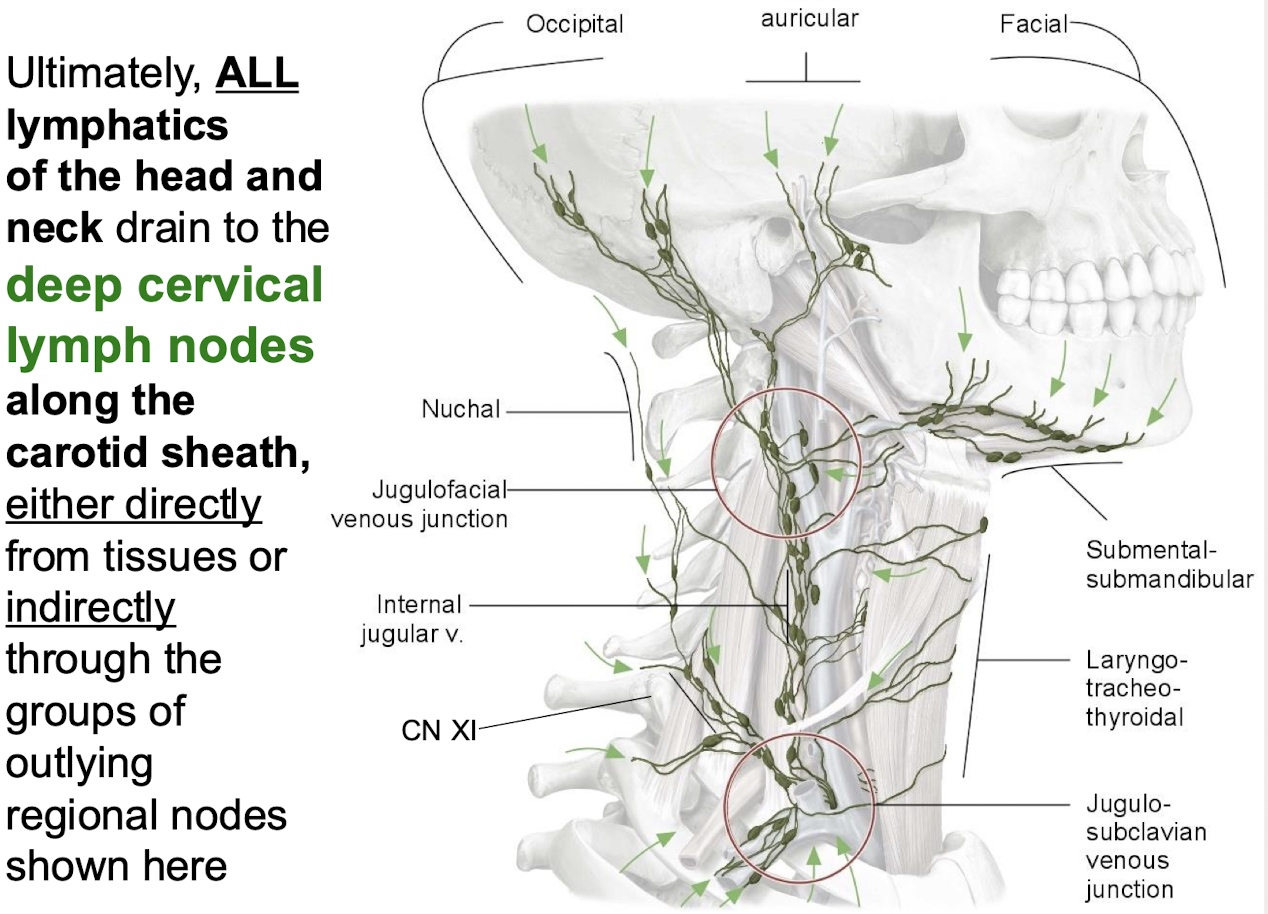
Why are the INFERIOR deep cervical nodes sometimes called supraclavicular or scalene nodes?
Because of their position above the clavicle and upon the surface of the scalene muscles
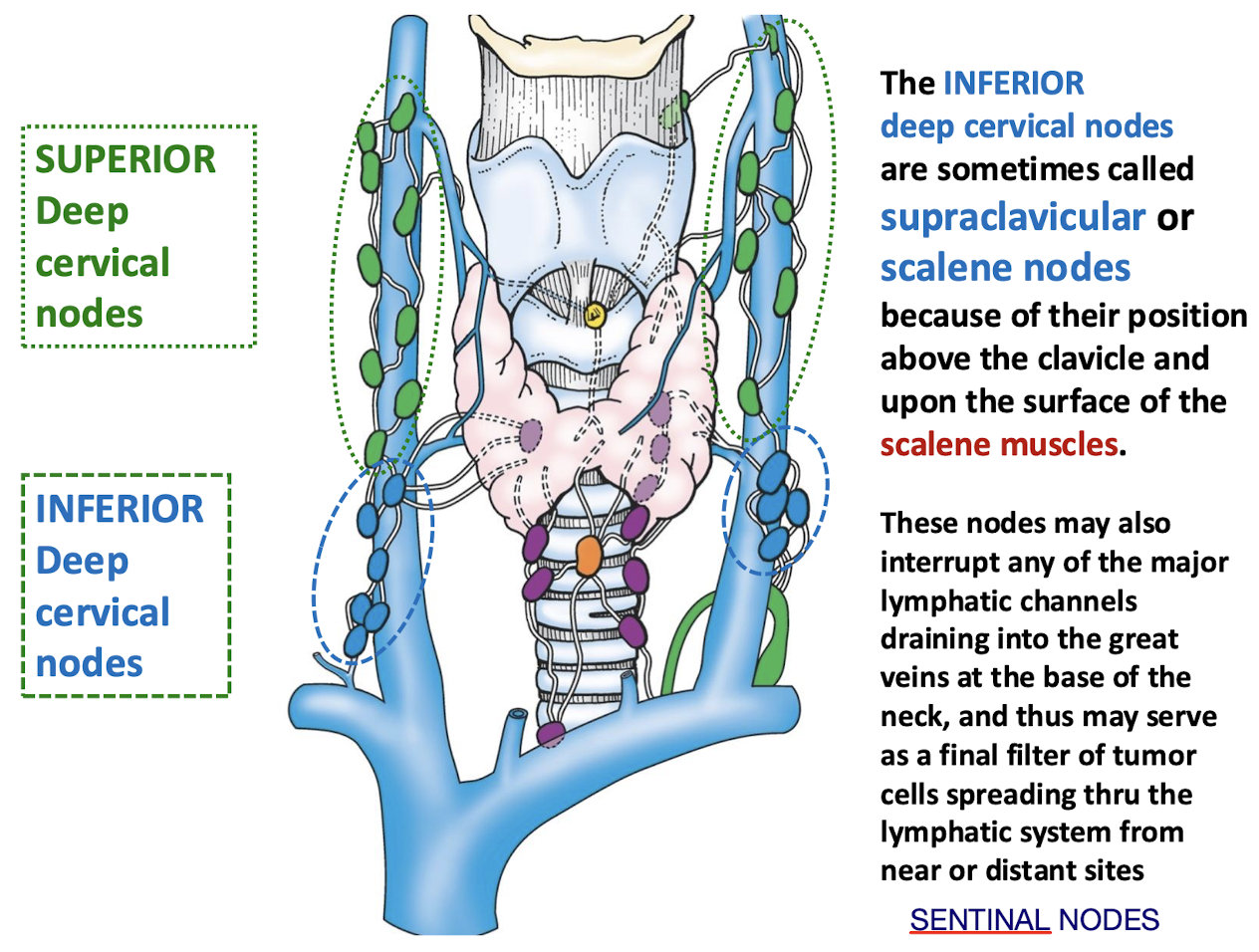
What important clinical function do the inferior deep cervical (scalene) nodes serve regarding cancer spread?
They may serve as a final filter of tumor cells spreading through the lymphatic system from near or distant sites.
If these nodes are involved, it may indicate more advanced spread.
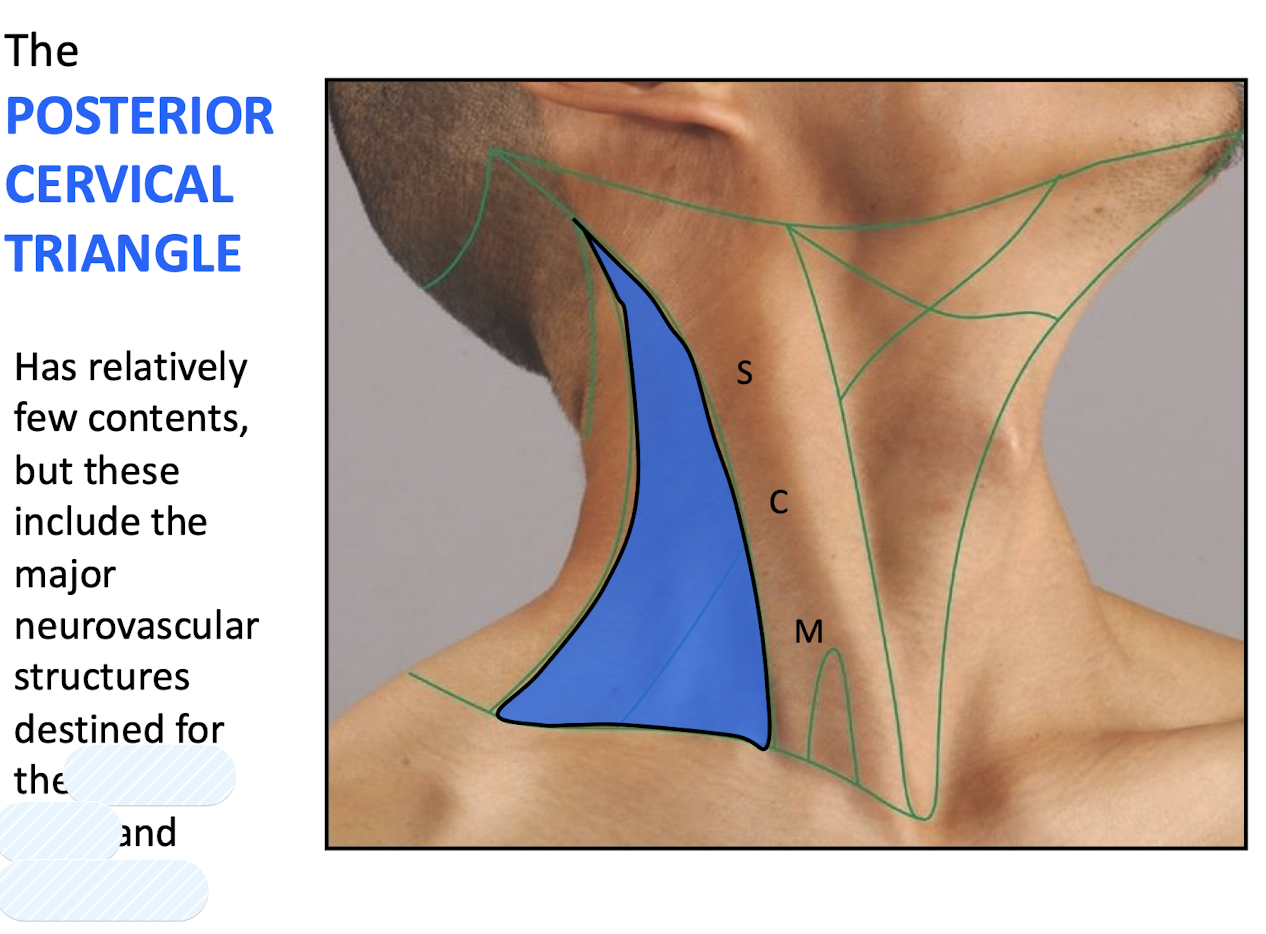
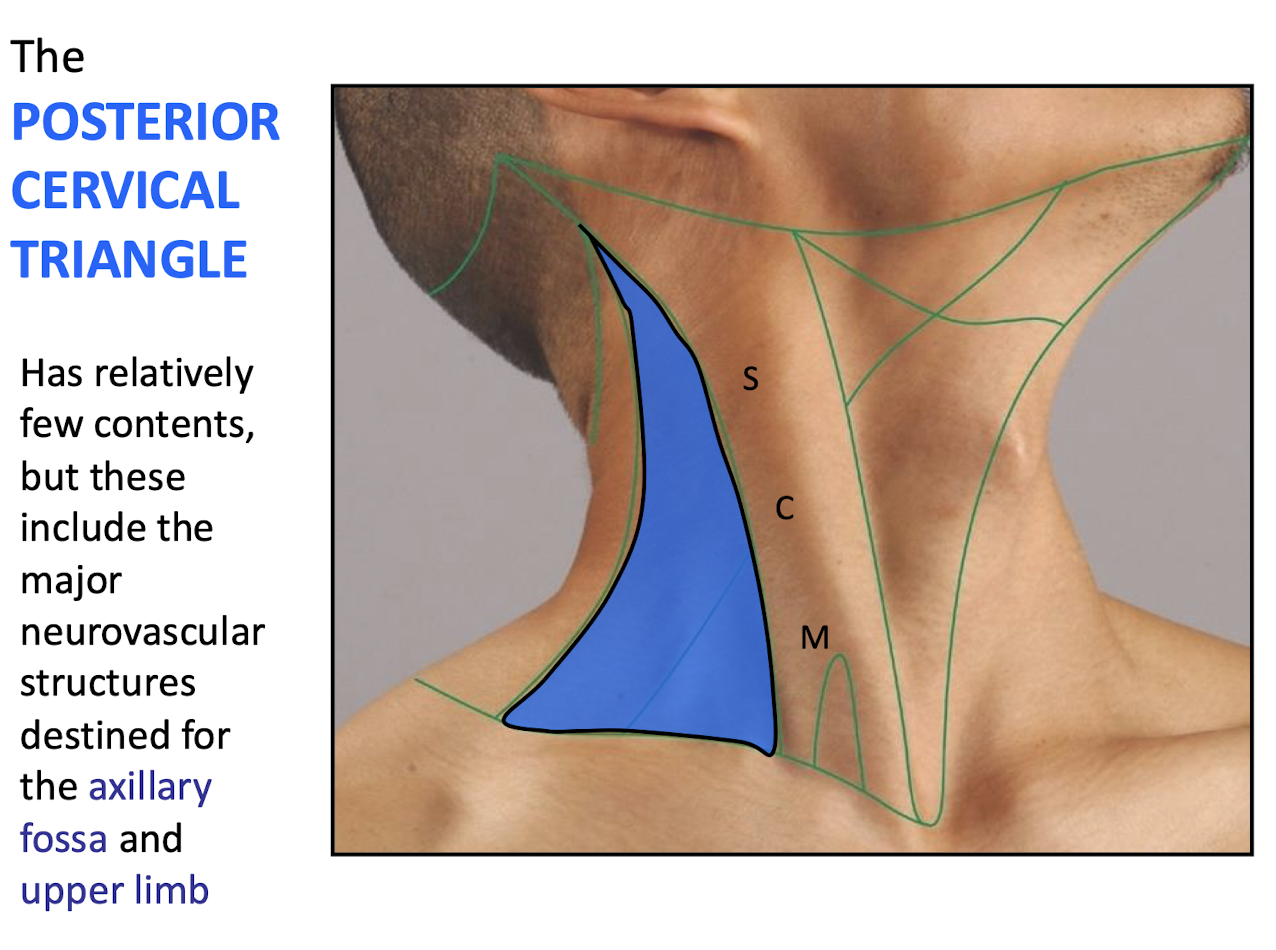
What are the boundaries of the POSTERIOR CERVICAL TRIANGLE?
Posterior border of SCM; Anterior border of TRAPEZIUS; and CLAVICLE
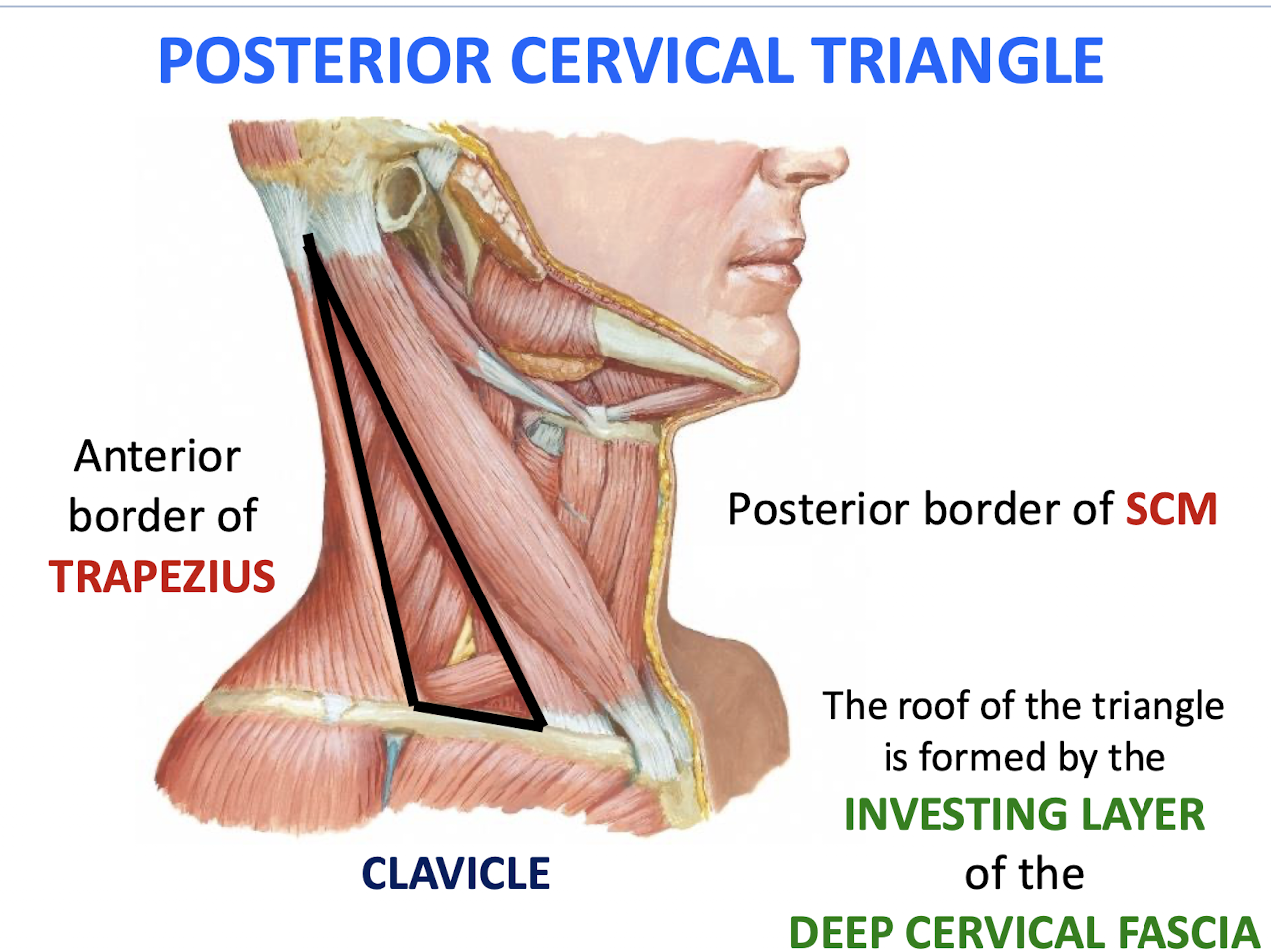
What forms the roof of the Posterior Cervical Triangle?
The INVESTING LAYER of the cervical fascia.
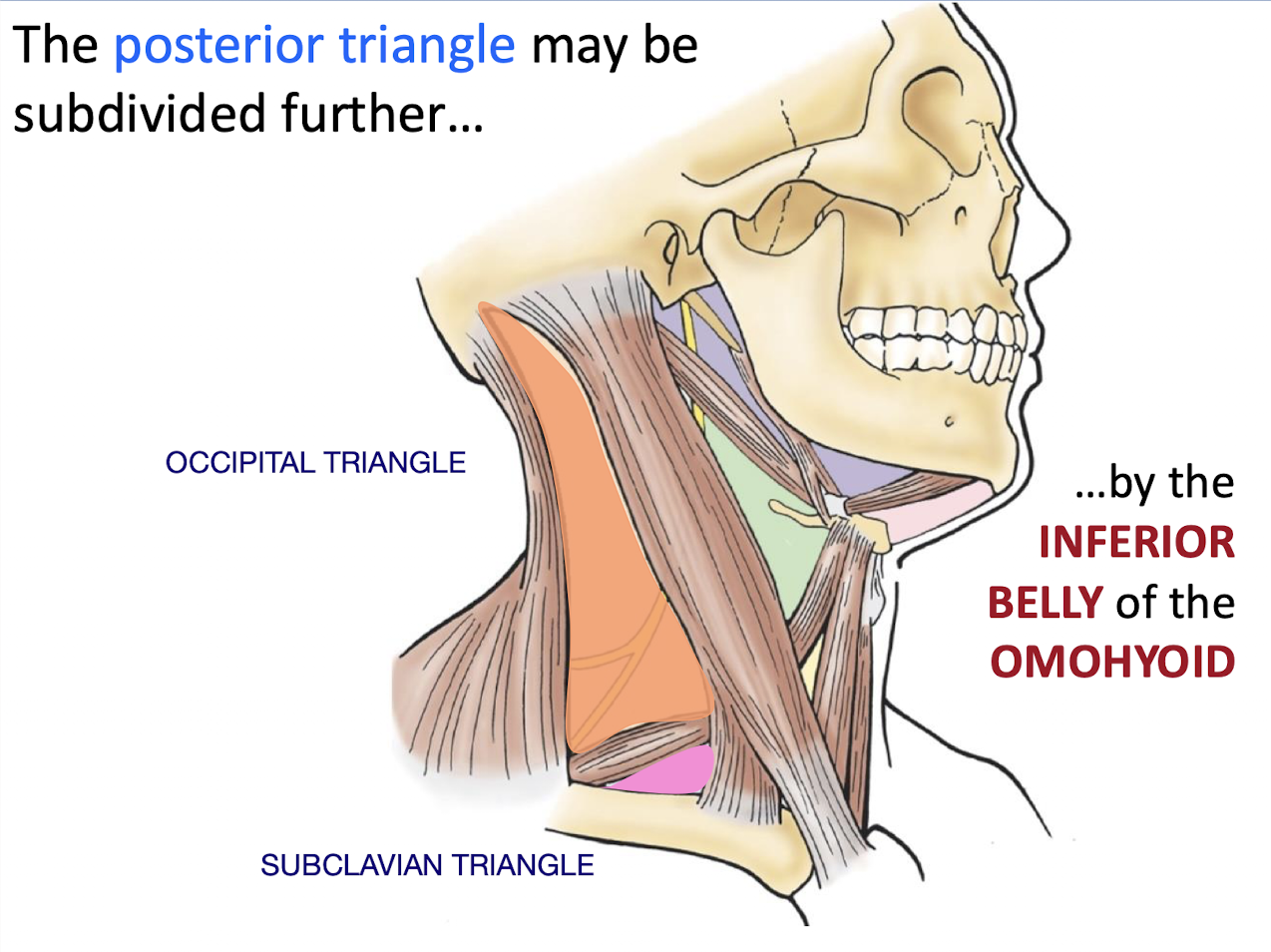
What are the subdivisions of the posterior triangle and what structure subdivides it?
The INFERIOR BELLY of the OMOHYOID subdivides into the Occipital and Subclavian Triangles
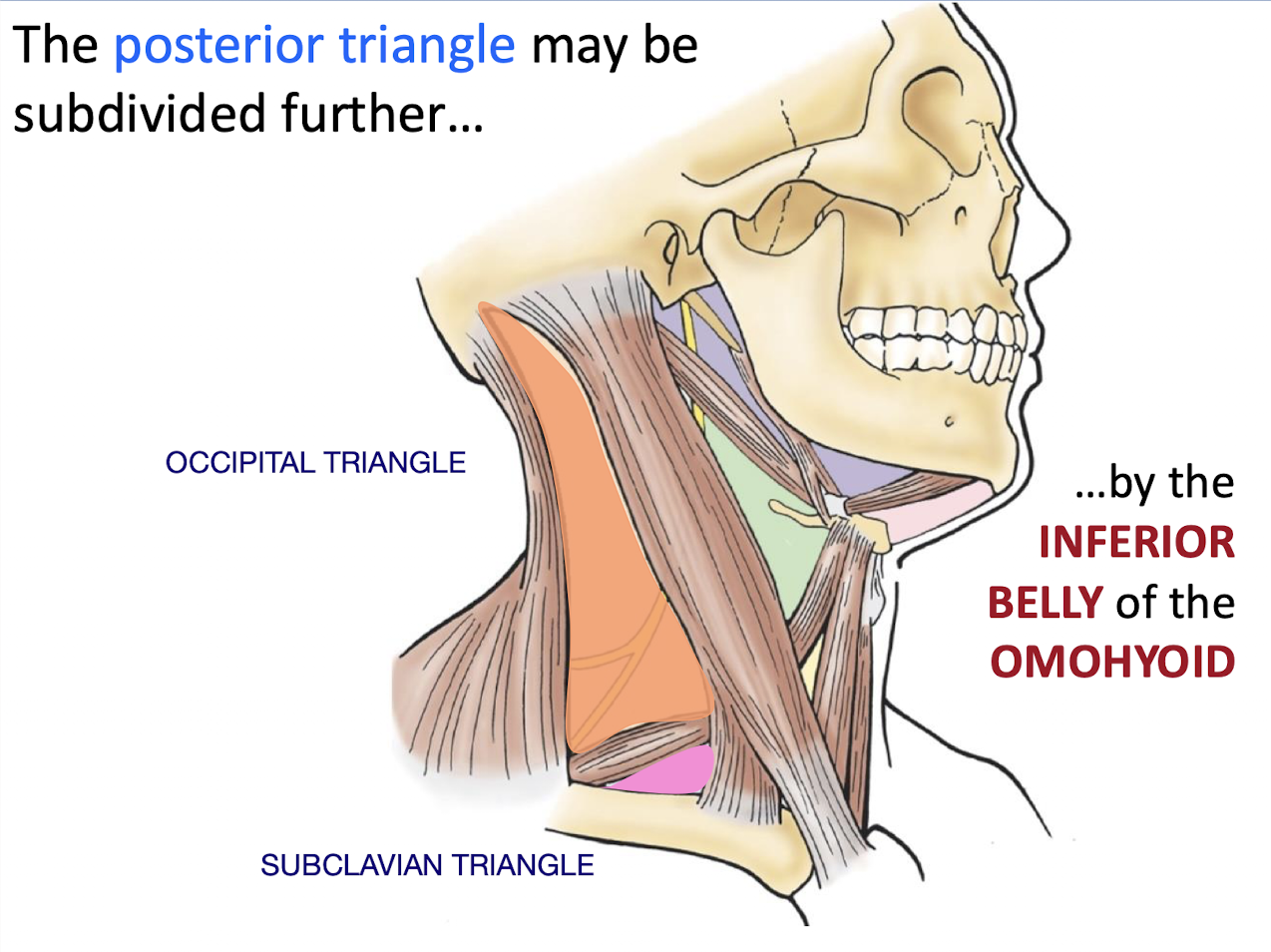
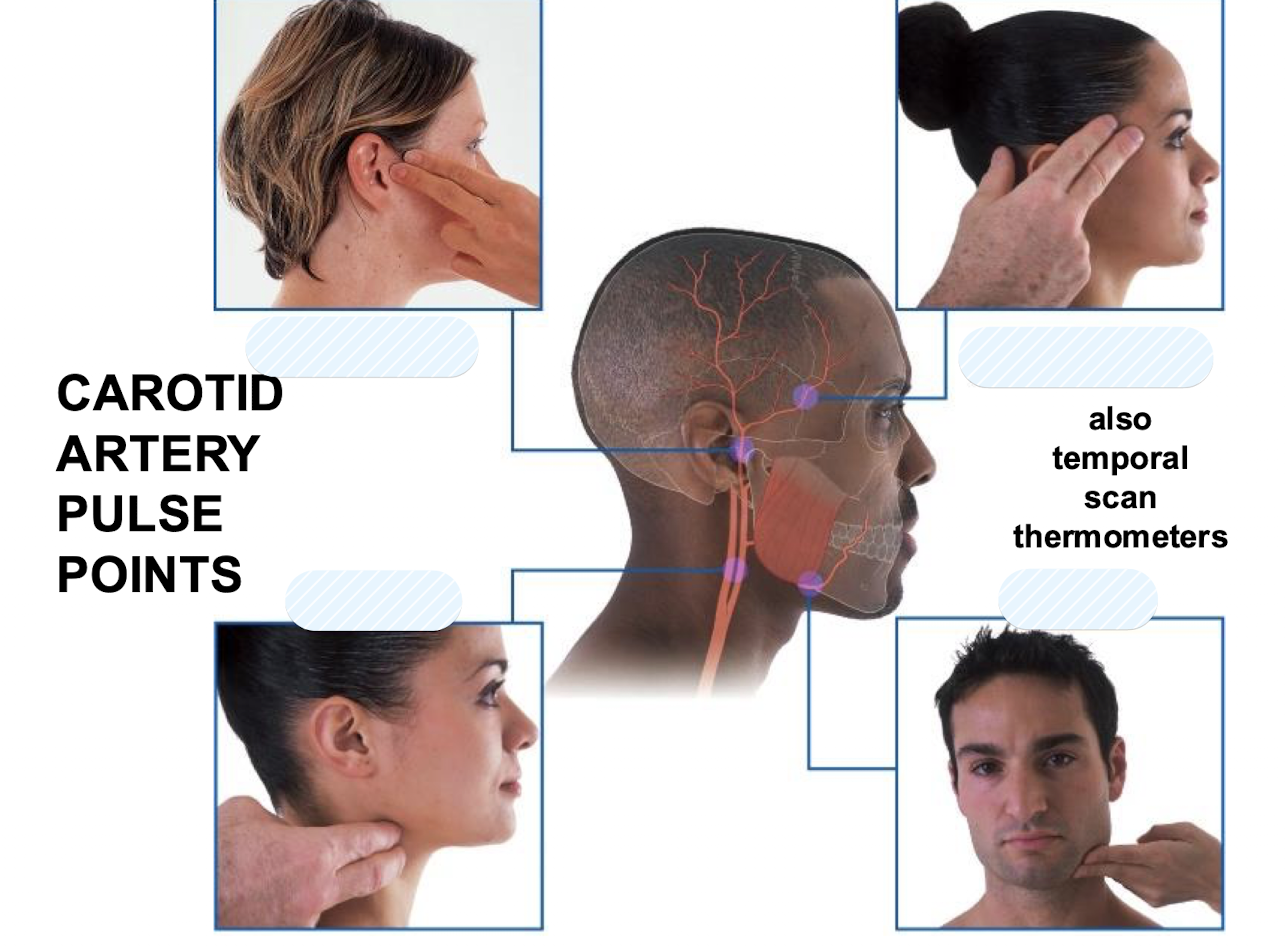
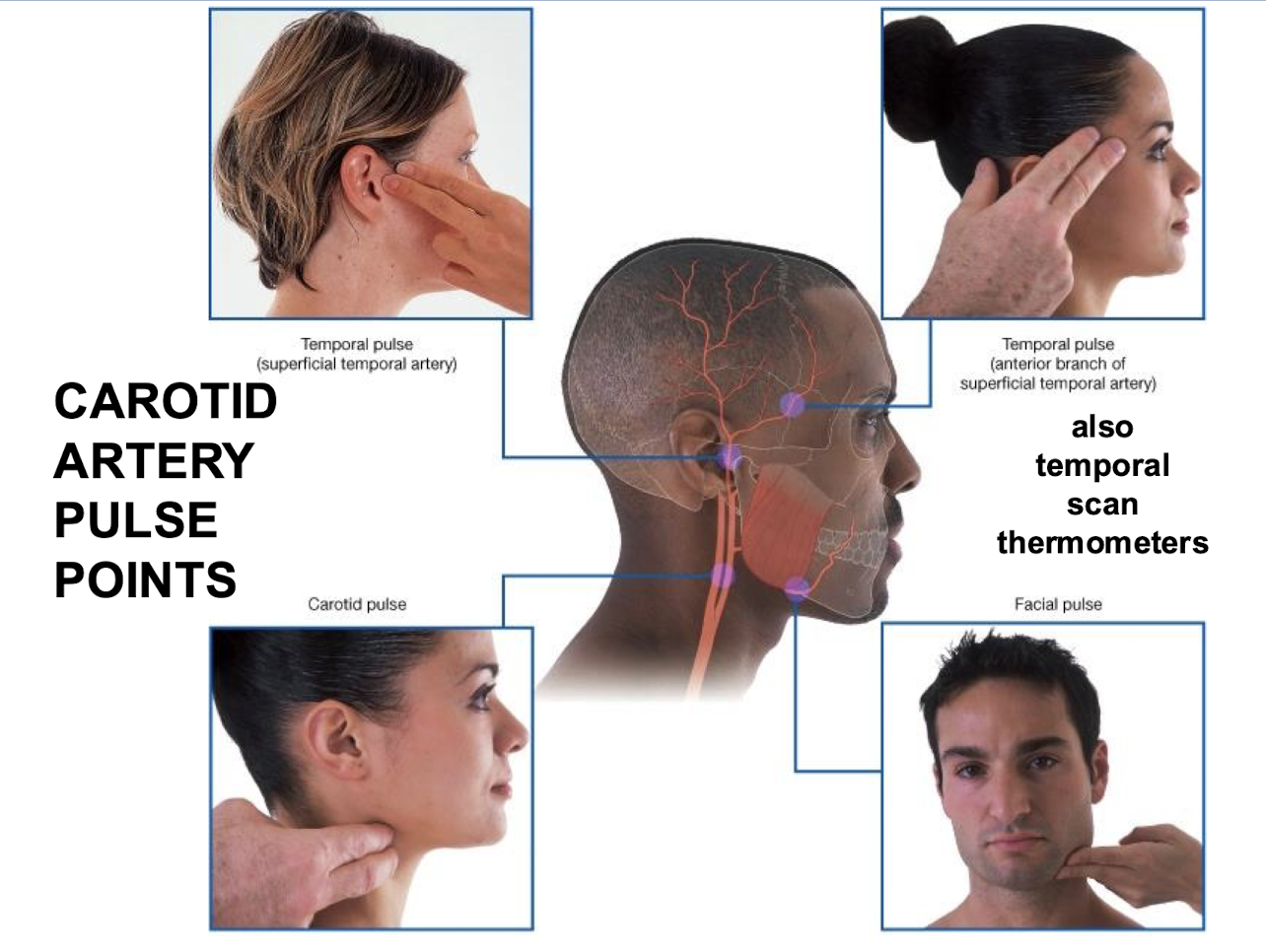
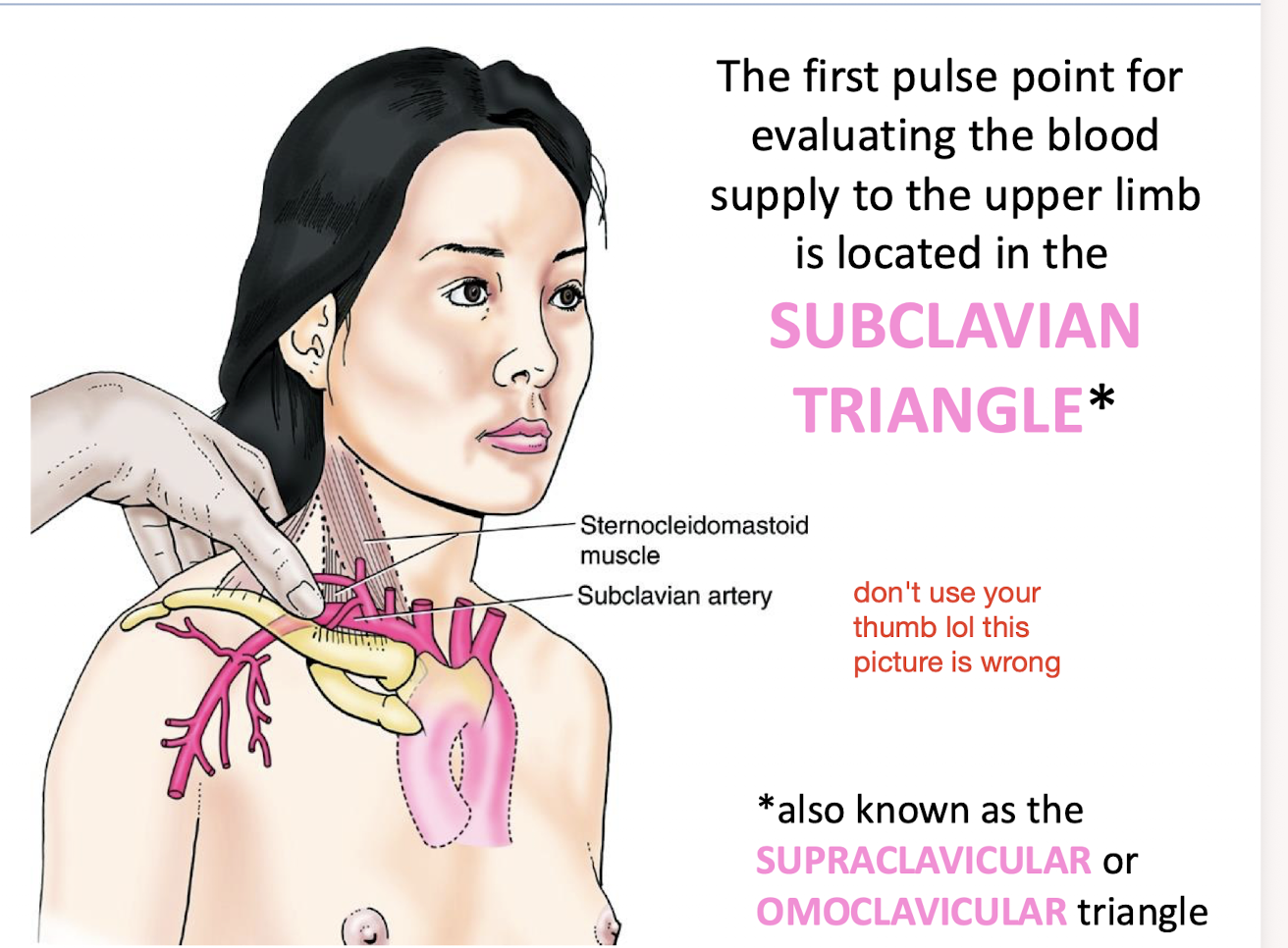
Where is the first pulse point for evaluating the blood supply to the upper limb located?
In the SUBCLAVIAN TRIANGLE (also known as the SUPRACLAVICULAR or OMOCLAVICULAR triangle).
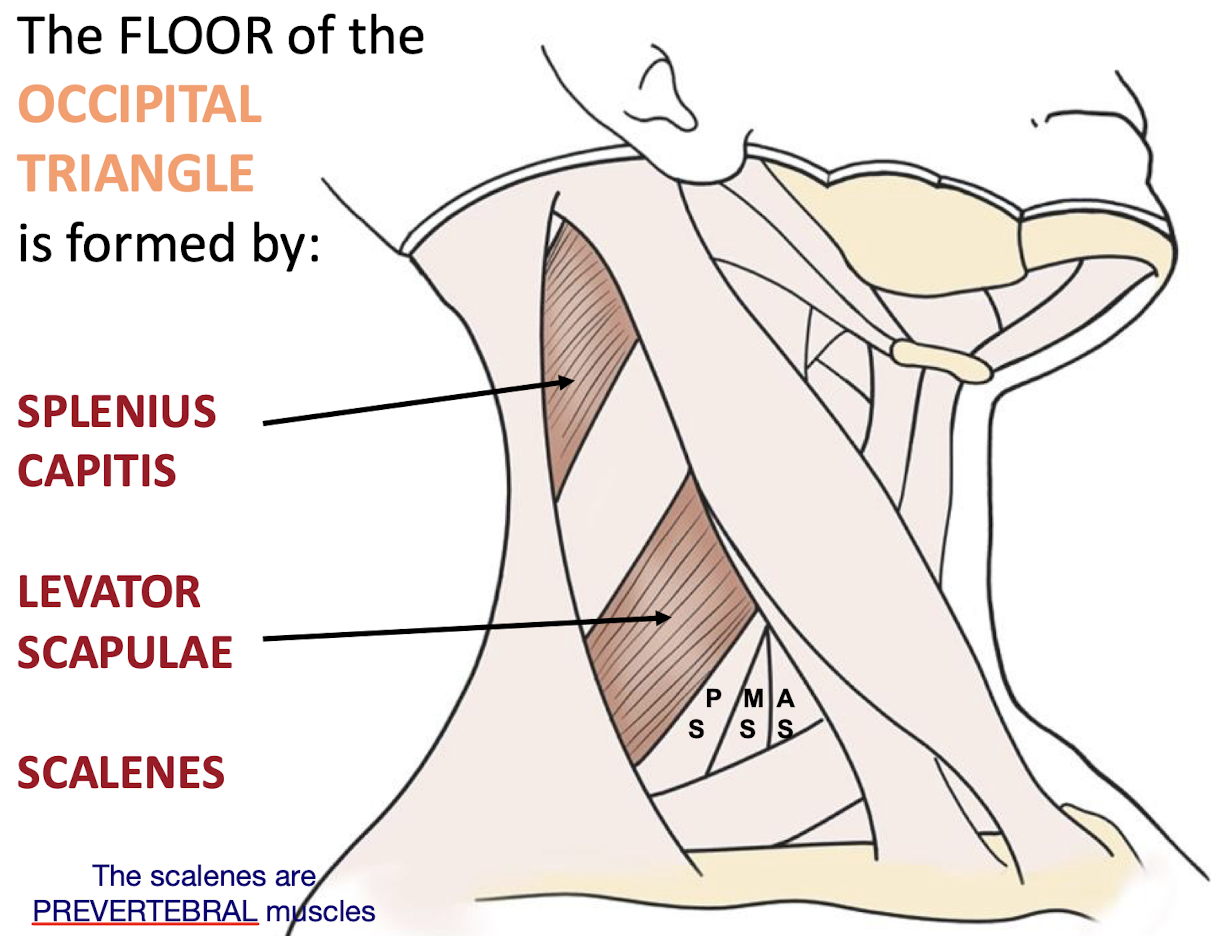
What muscles form the FLOOR of the OCCIPITAL TRIANGLE?
SPLENIUS CAPITIS; LEVATOR SCAPULAE; and SCALENES (Posterior; Middle; Anterior)
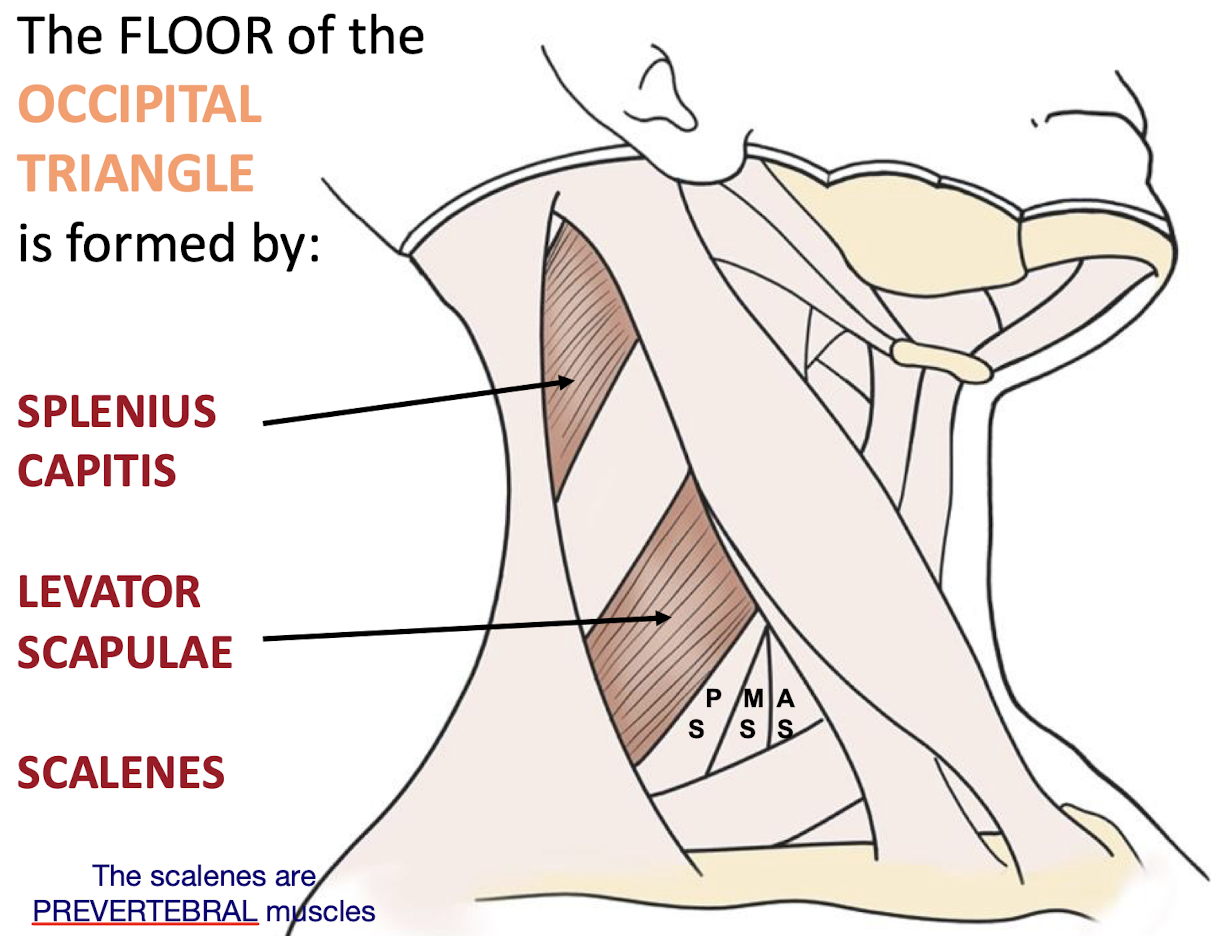
What group of muscles do the scalenes belong to; and where do they attach?
PREVERTEBRAL MUSCLES; they attach primarily to anterior aspects of cervical vertebrae; including vertebral bodies and transverse processes
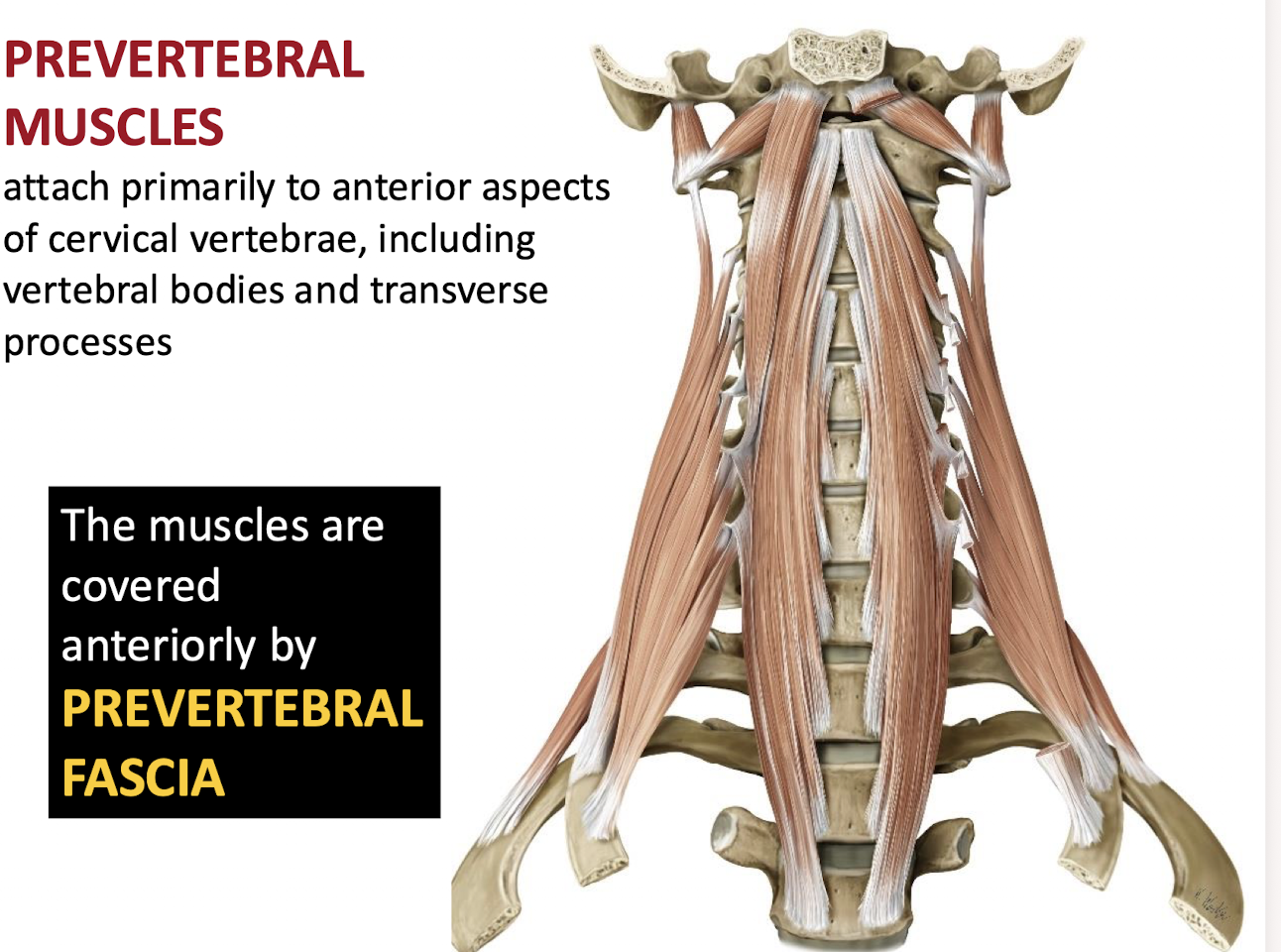
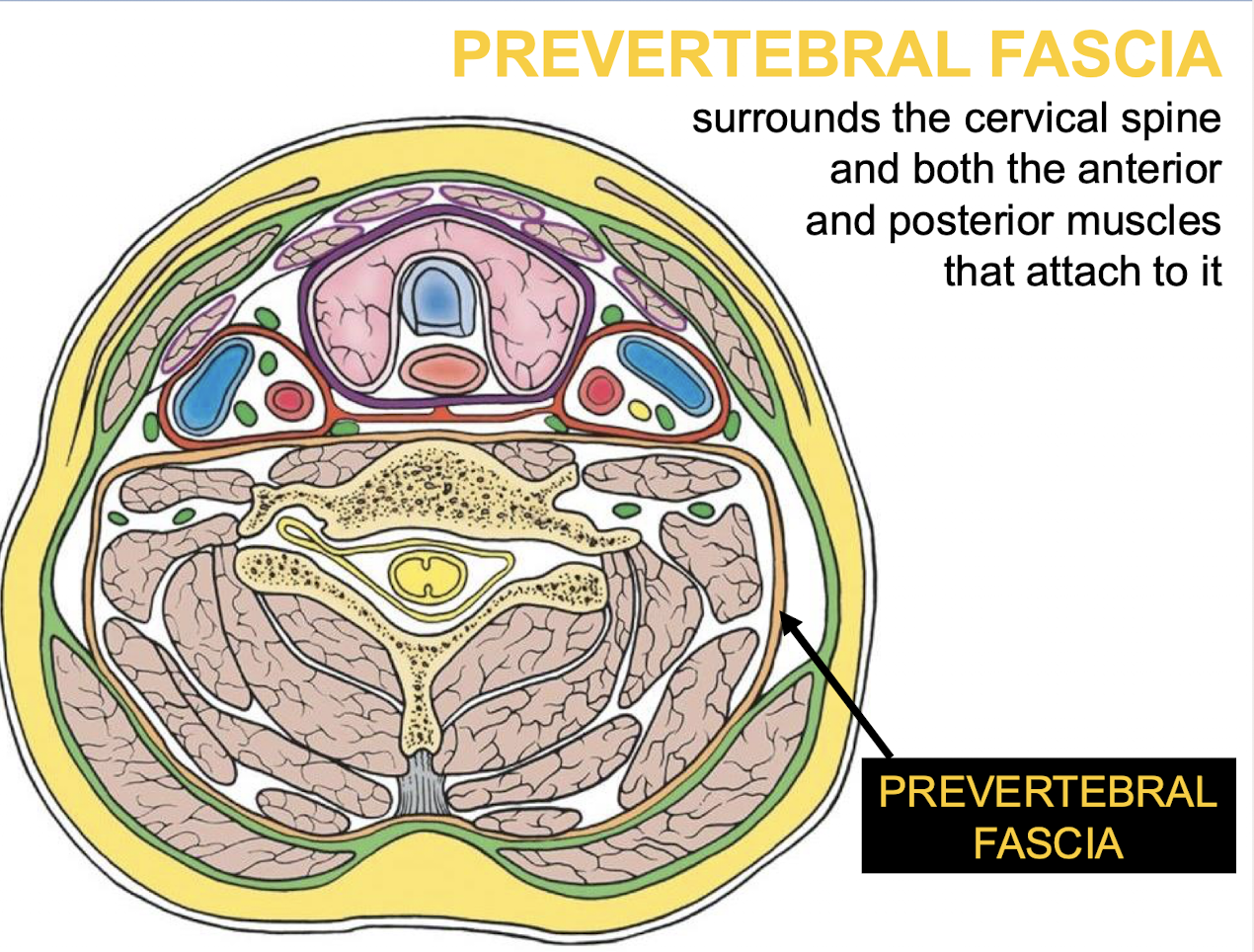
What covers the prevertebral muscles anteriorly?
The PREVERTEBRAL FASCIA.
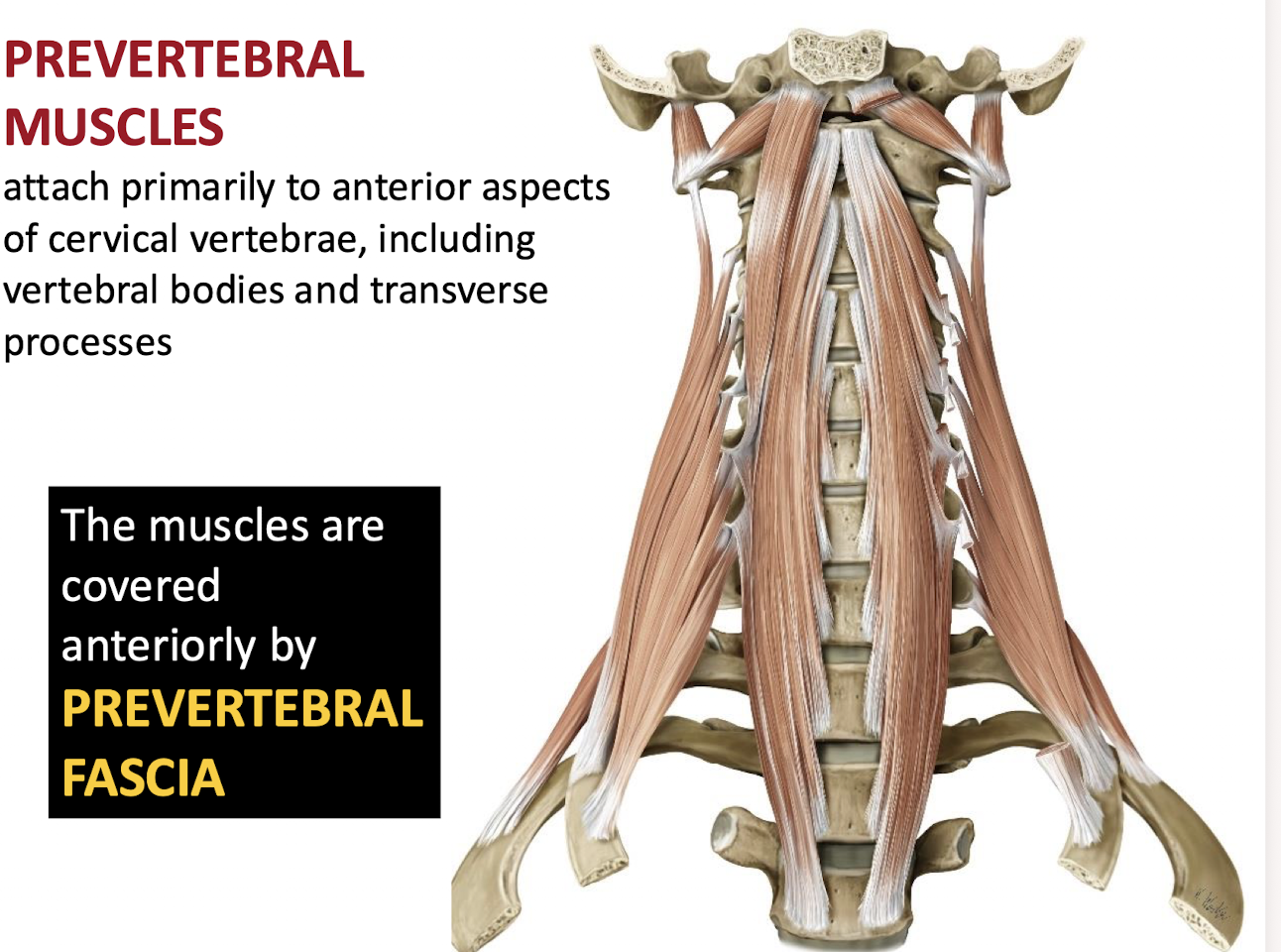
What does prevertebral fascia surround?
The cervical spine + the anterior and posterior muscles that attach to it
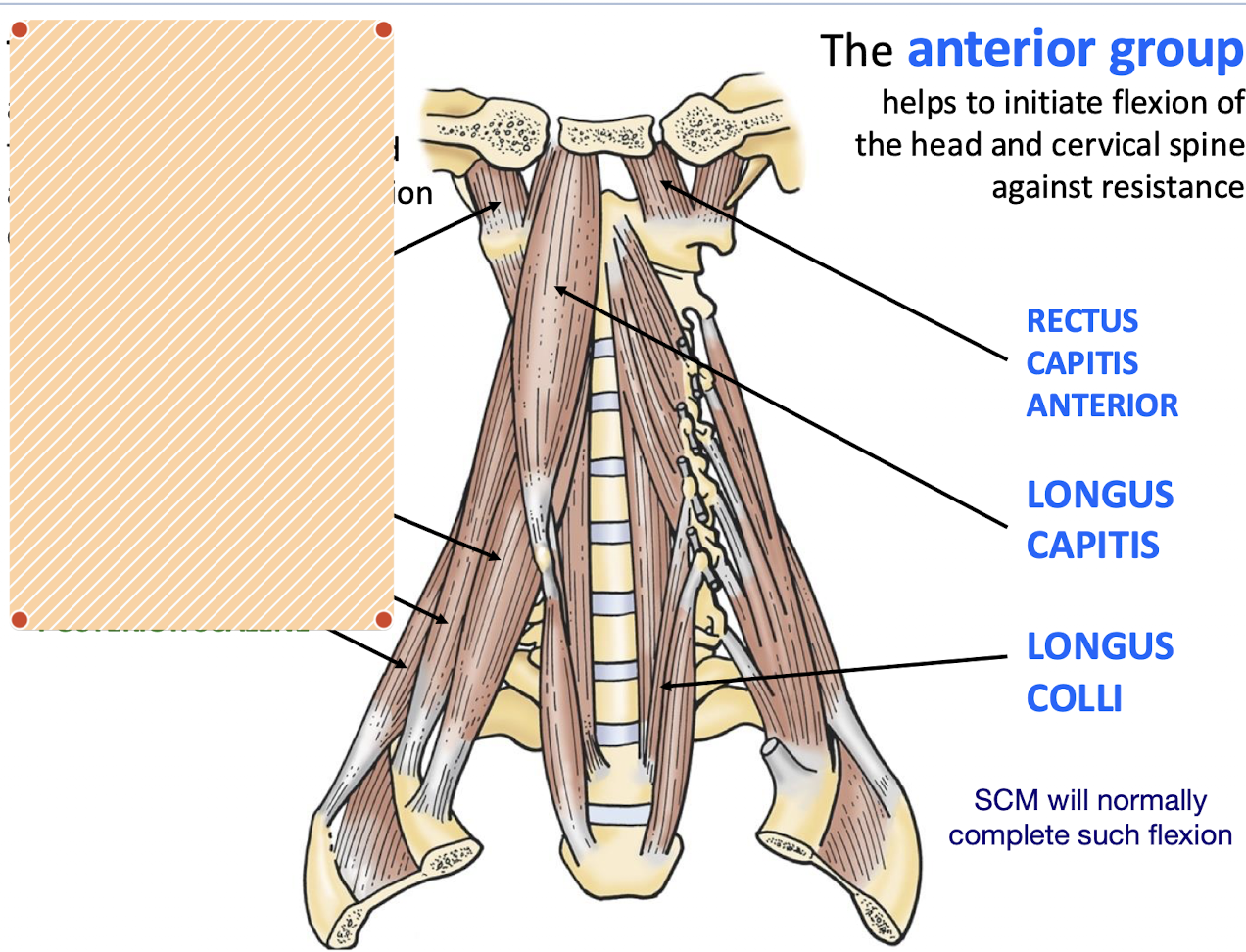
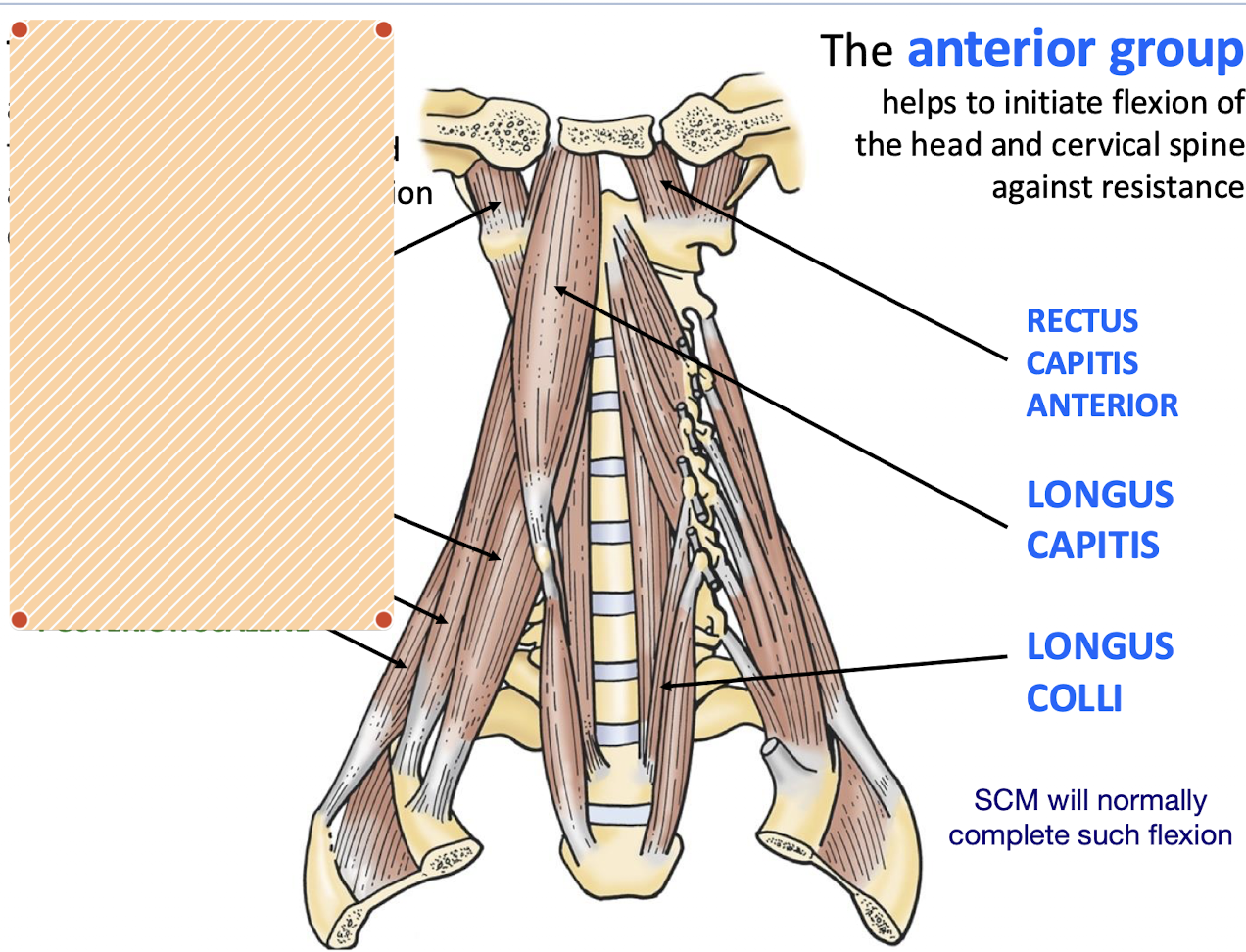
What is the action of the anterior group of prevertebral muscles . What are the examples?
The anterior group helps to initiate flexion of the head and cervical spine against resistance. (The SCM helps to complete the flexion)
Rectus Capitis Anterior, Longus capitis and Longus Colli
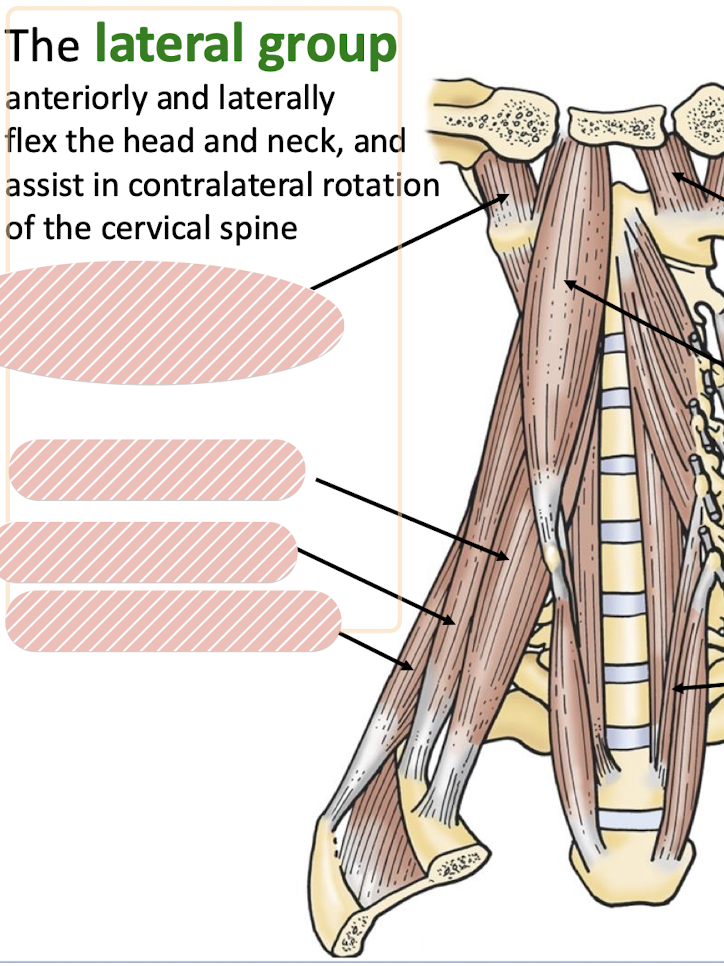
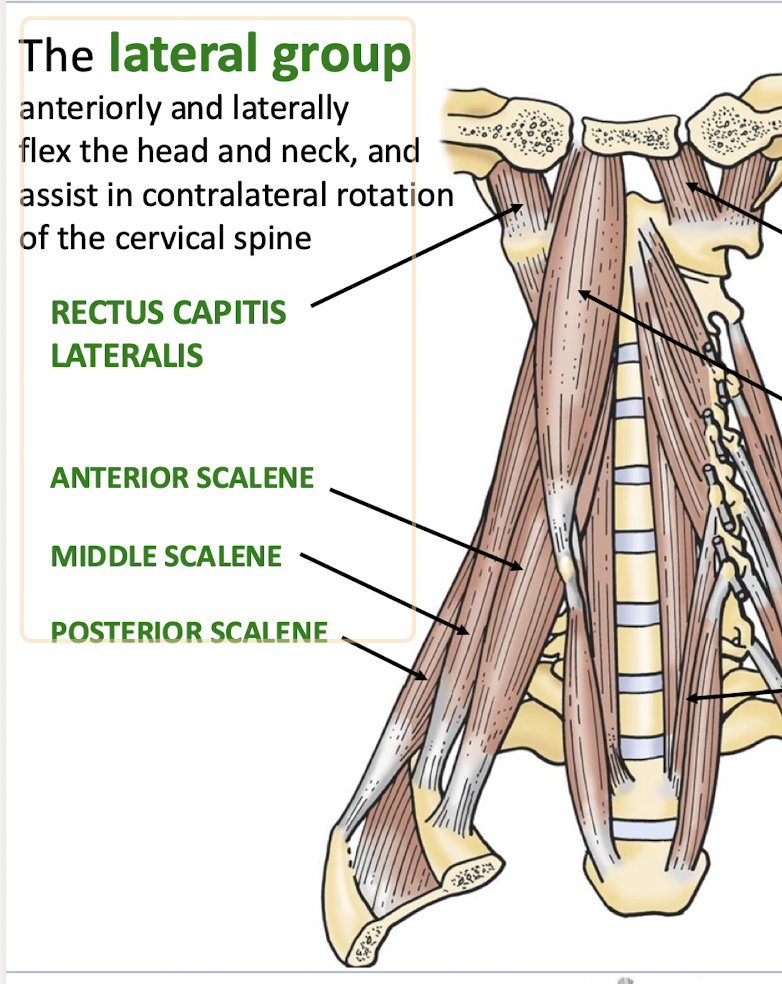
What are the two actions of the lateral group of prevertebral muscles . What are the examples?
They anteriorly and laterally flex the head and neck and assist in contralateral rotation of the cervical spine
RECTUS CAPITIS LATERALIS, ANTERIOR SCALENE, MIDDLE SCALENE, POSTERIOR SCALENE
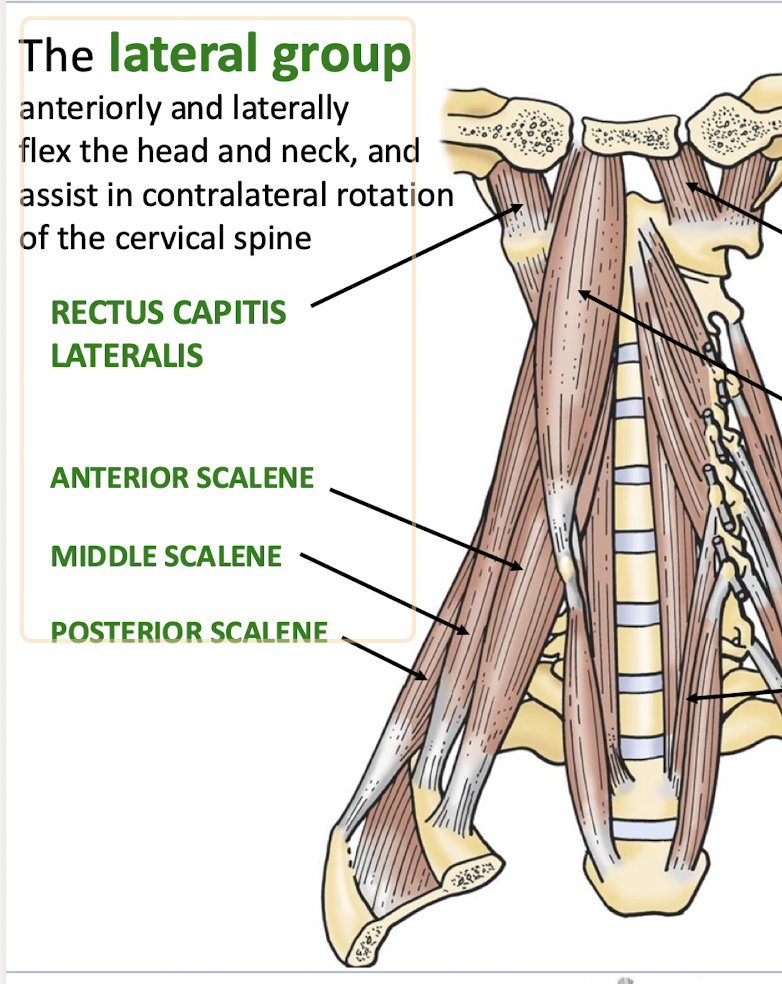
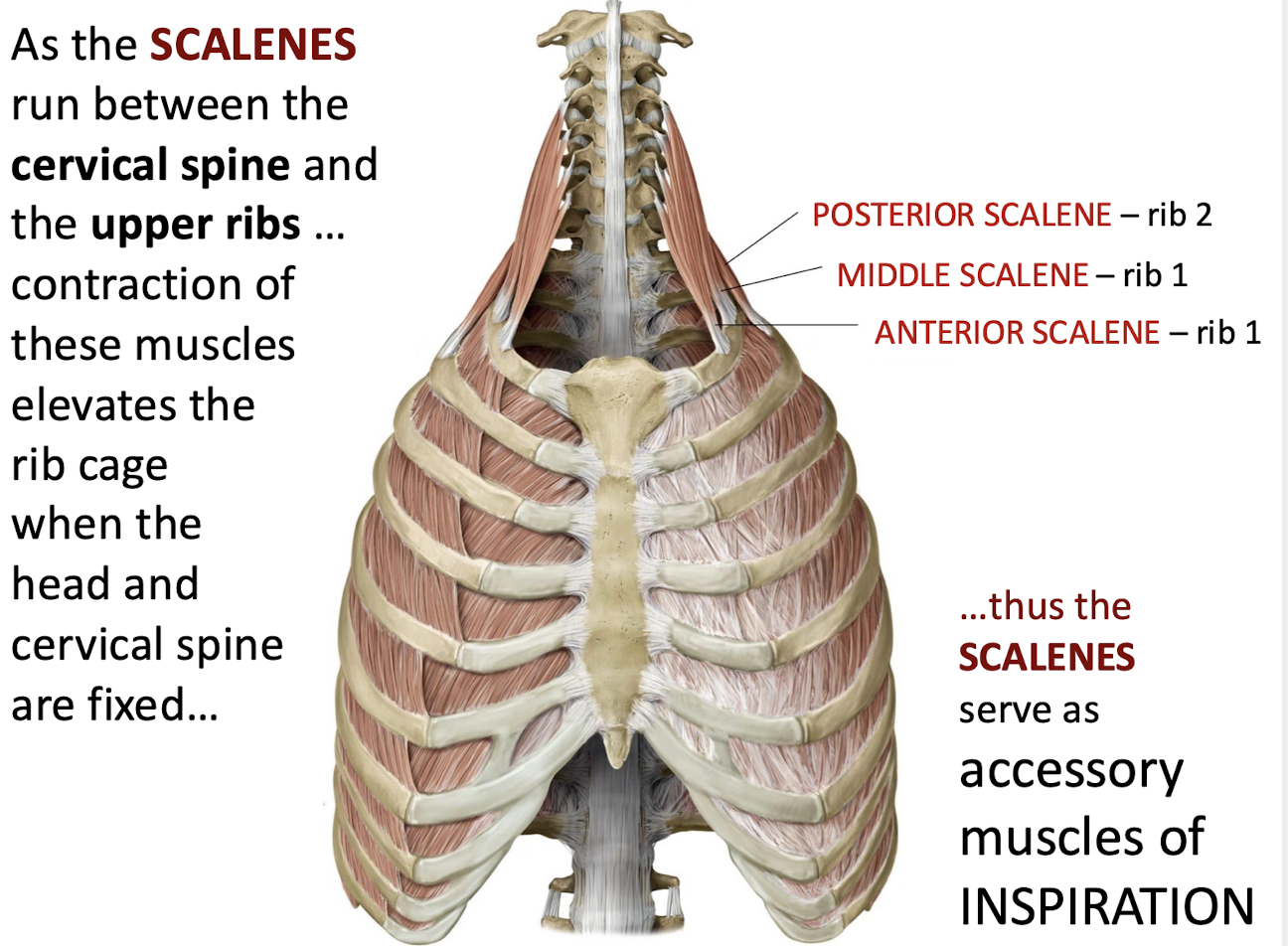
When the head and cervical spine are fixed; what accessory function do the SCALENES serve?
They serve as accessory muscles of respiration by elevating the rib cage
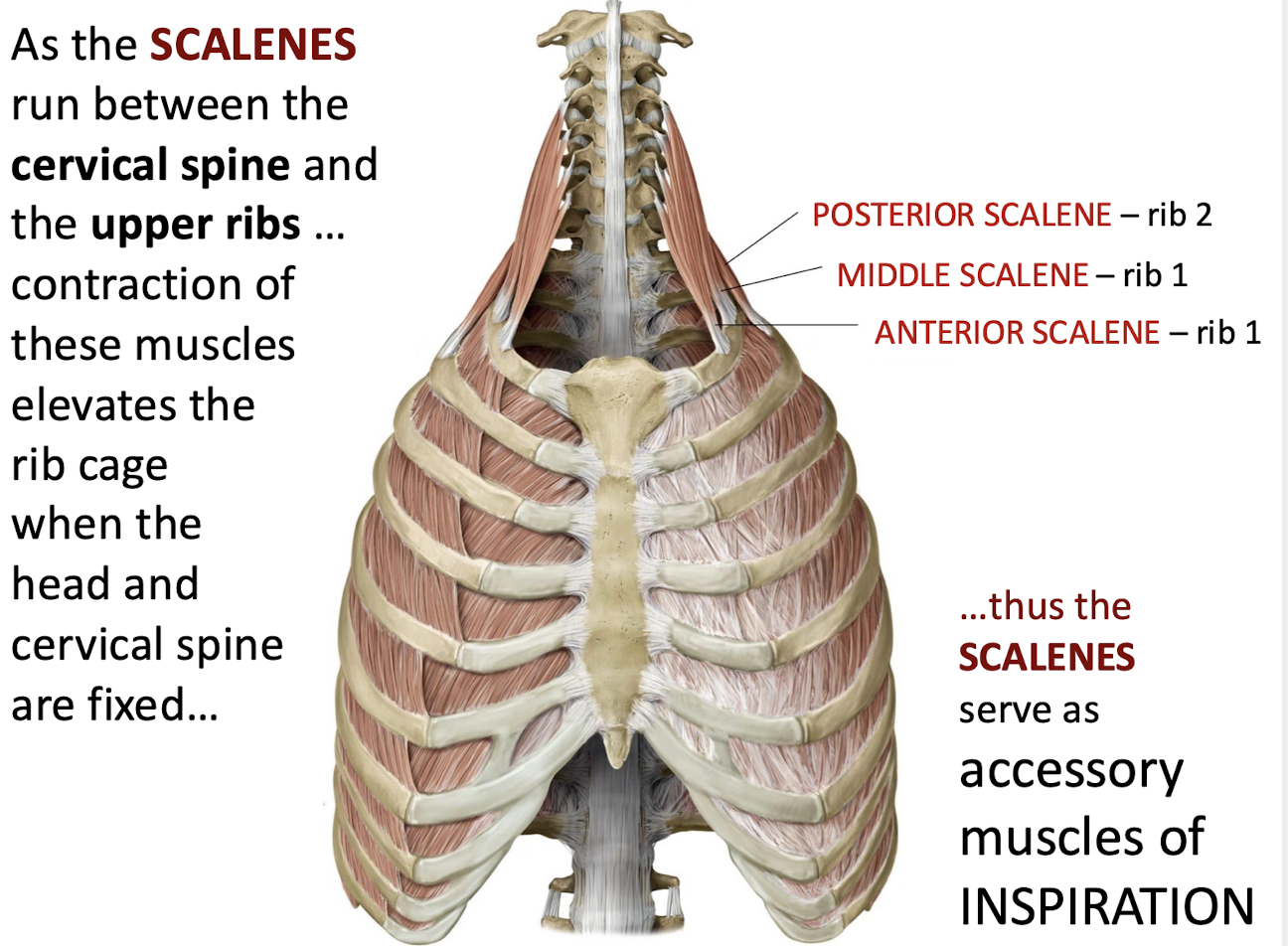
Which rib does the ANTERIOR SCALENE attach to? MIDDLE, POSTERIOR?
Rib 1, Rib 1, Rib 2
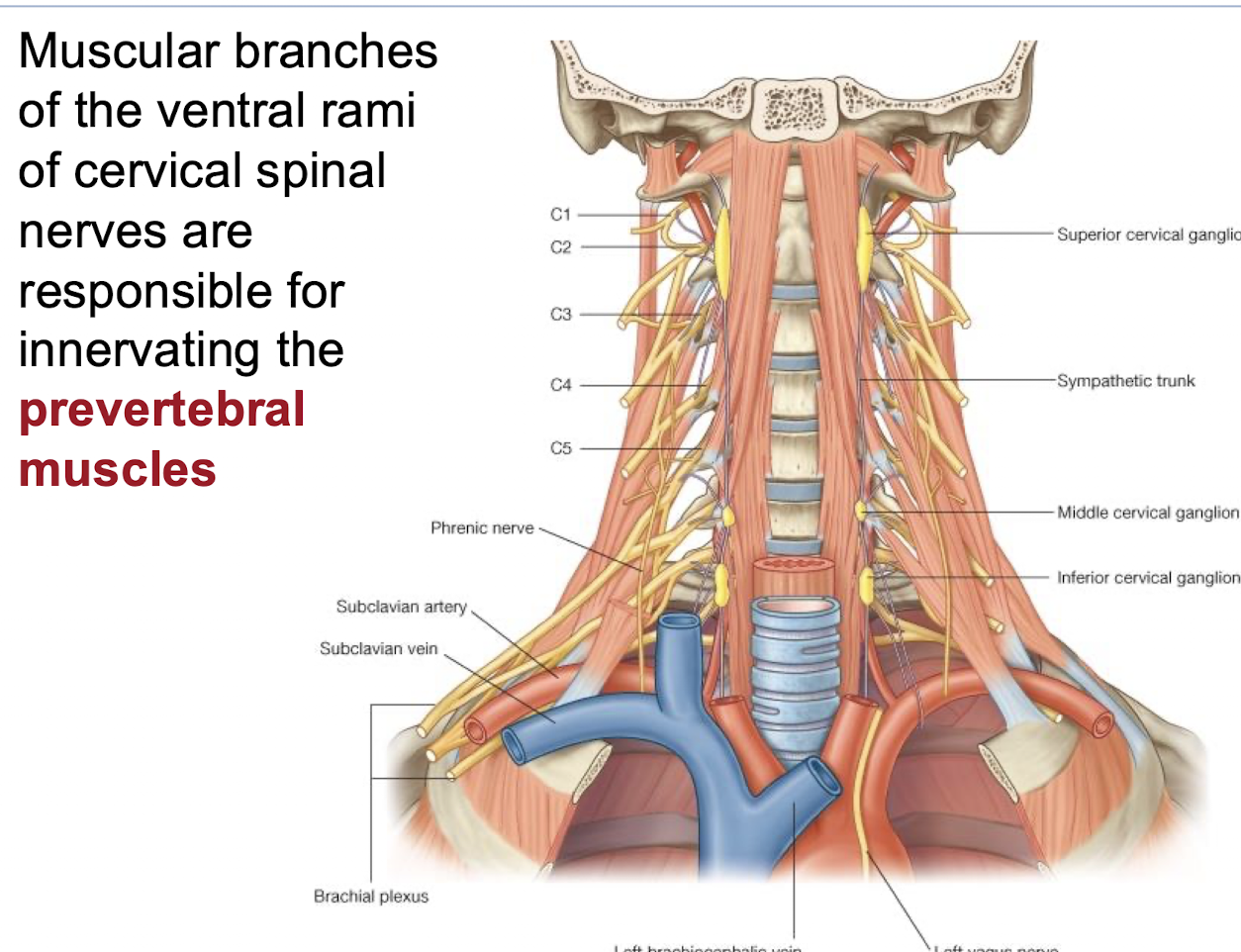
What is responsible for innervating the prevertebral muscles?
Muscular branches of the ventral rami of cervical spinal nerves
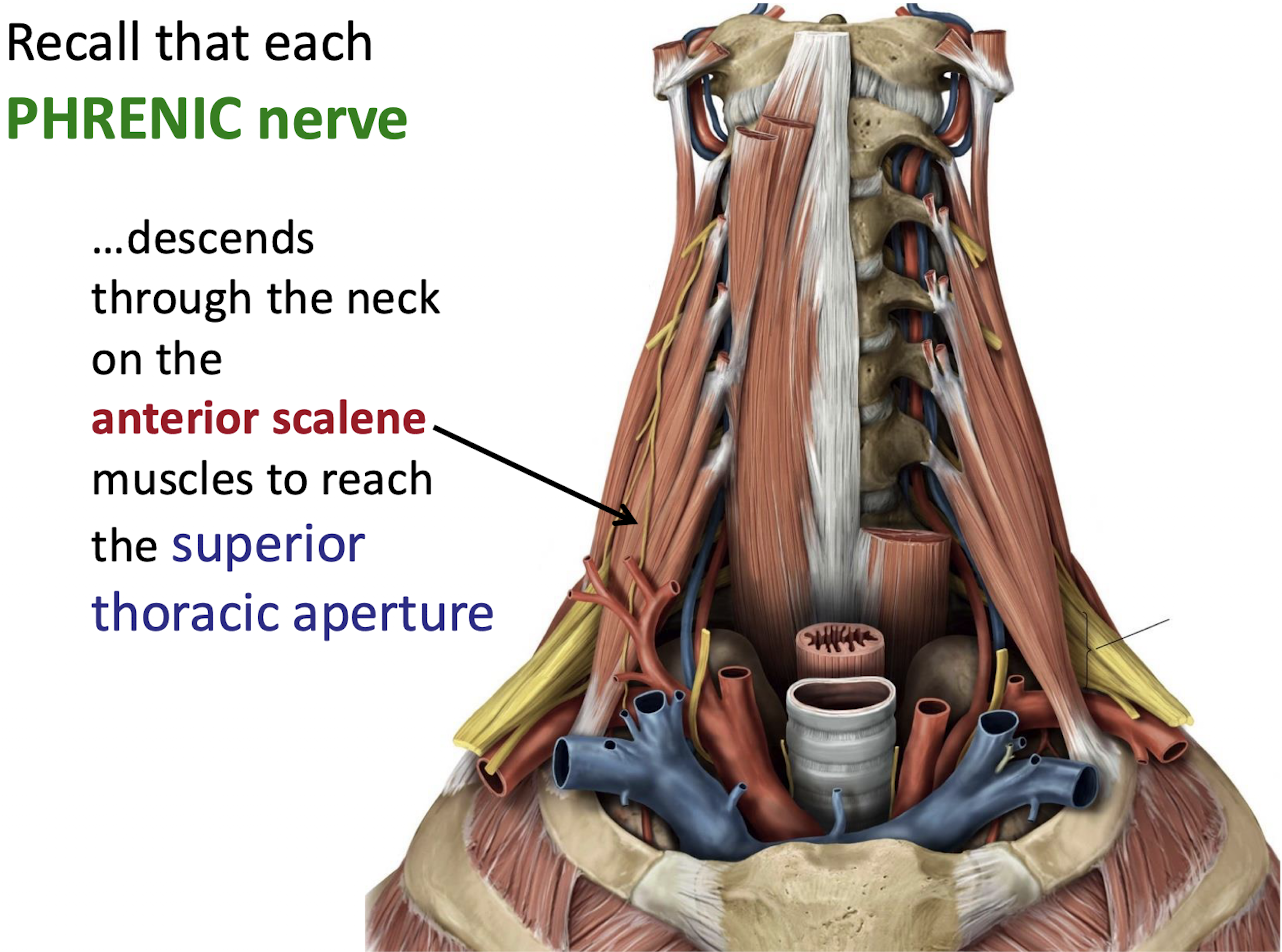
Which major nerve descends through the neck on the anterior scalene muscles to reach the superior thoracic aperture?
The PHRENIC nerve.
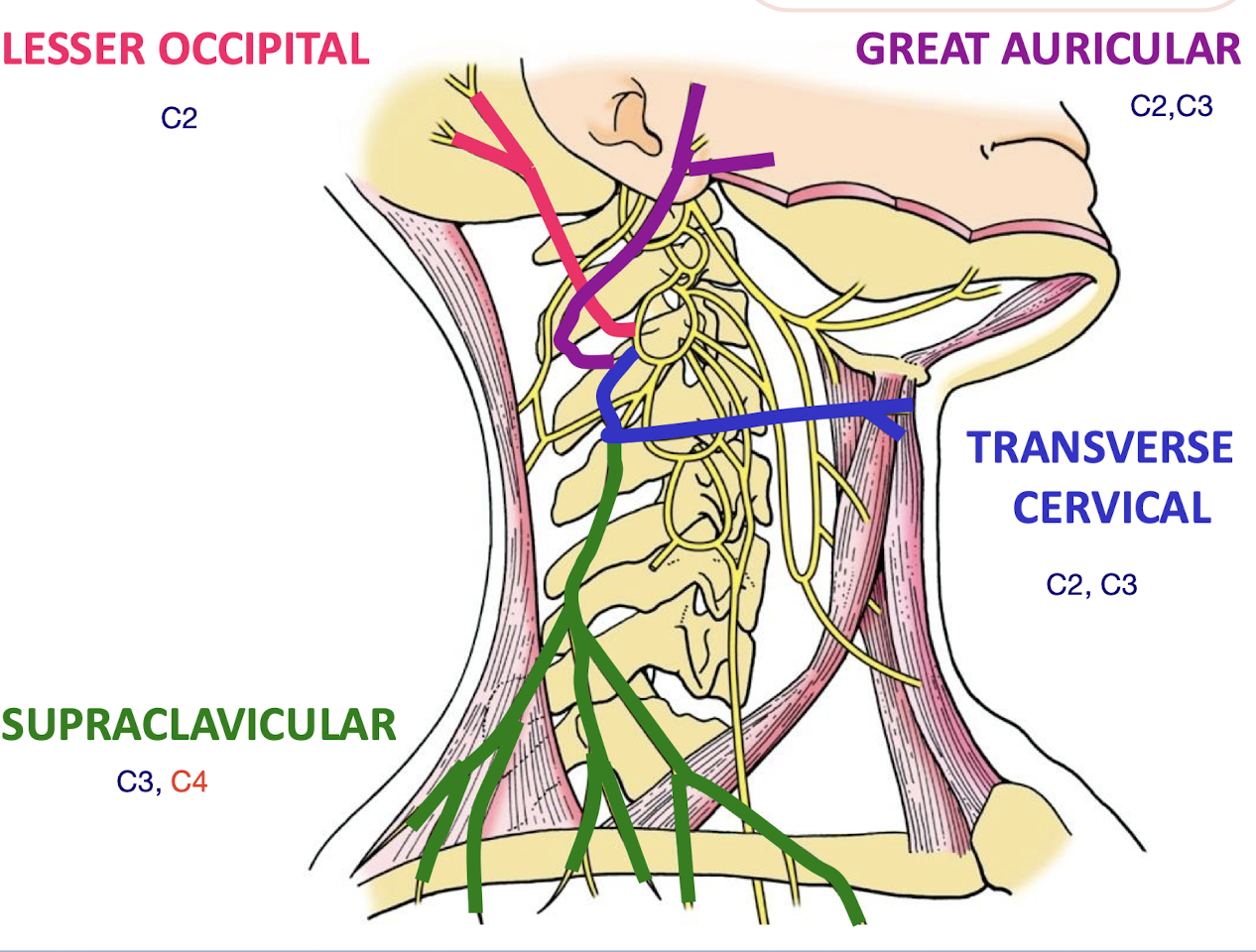
Name the four sets of CUTANEOUS NERVES that arise from the cervical plexus.
TRANSVERSE CERVICAL; GREAT AURICULAR; LESSER OCCIPITAL; SUPRACLAVICULAR
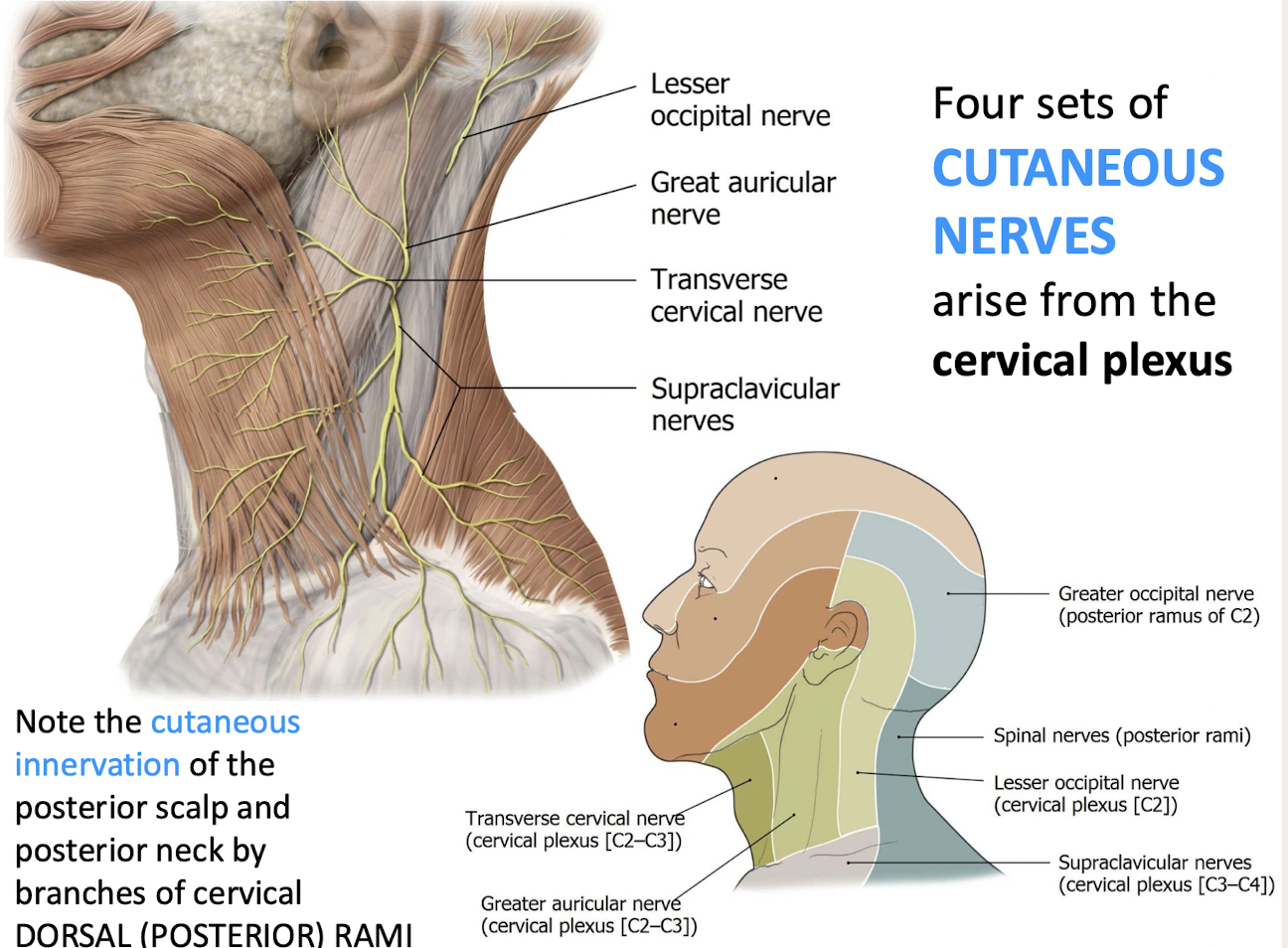
Which nerve innervates the skin of the posterior scalp and neck?
Branches of cervical DORSAL RAMI
distinction: Cervical plexus – This is formed by the ventral rami (anterior branches) of the C1–C4 spinal nerves.
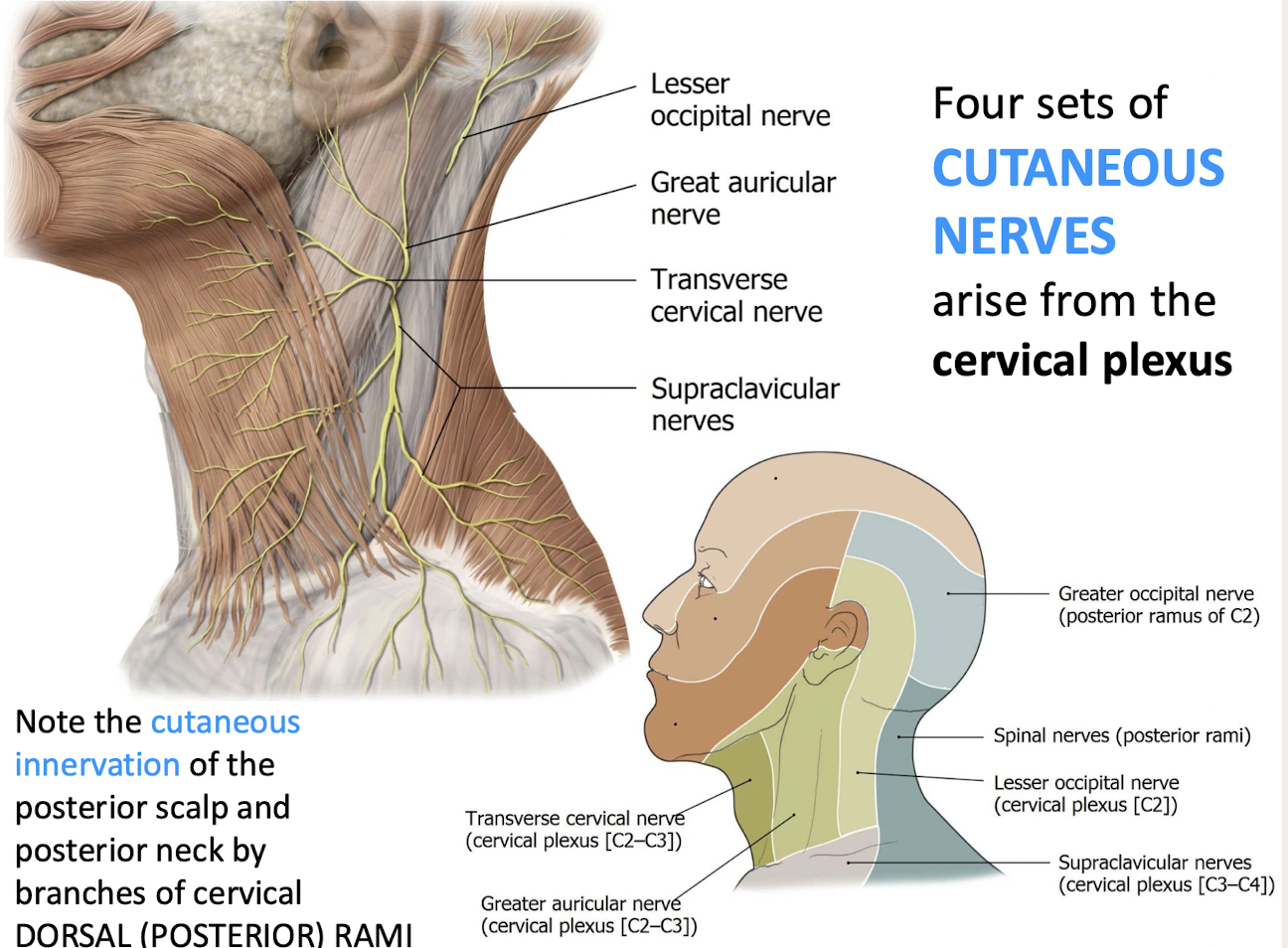
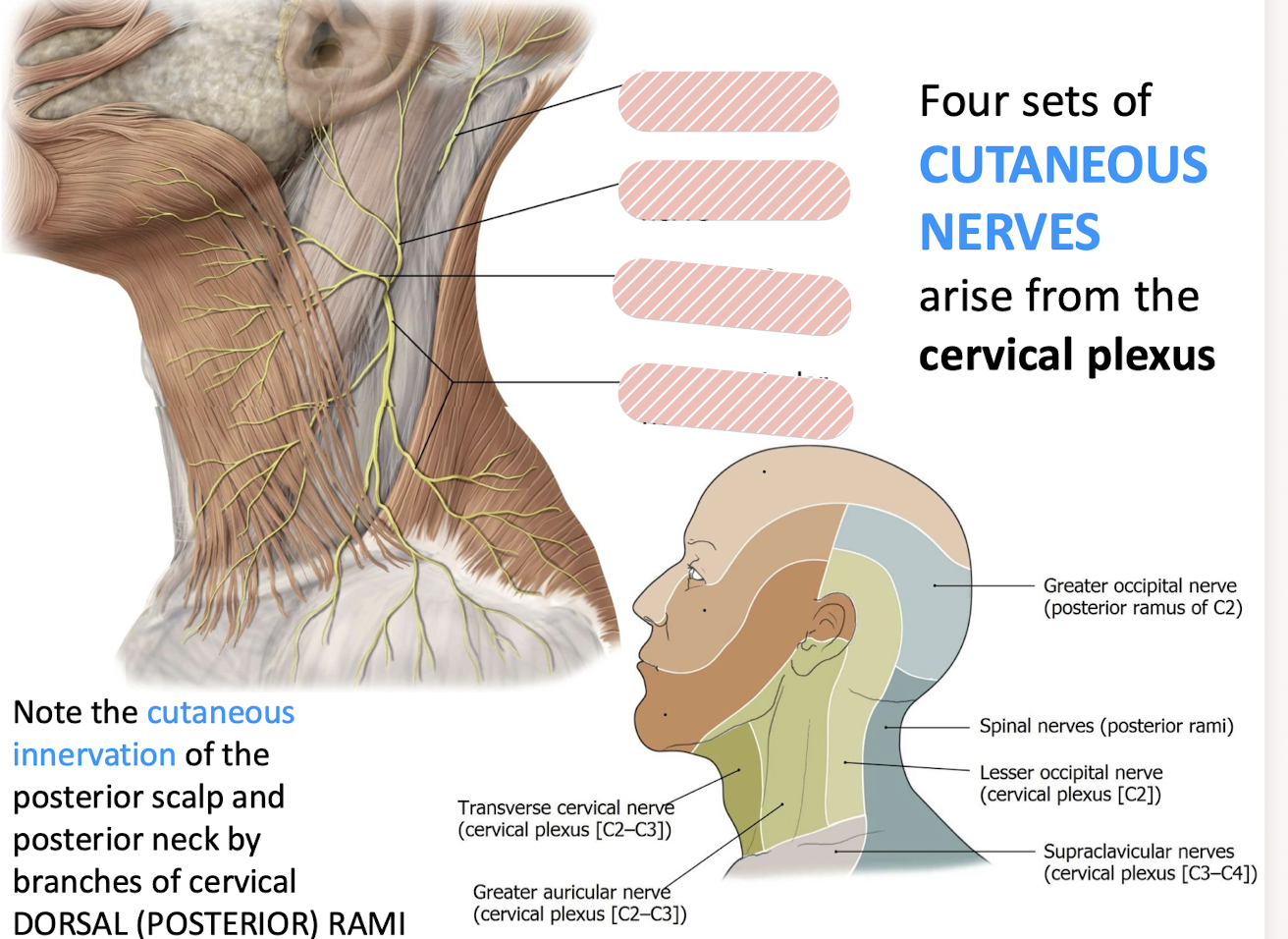
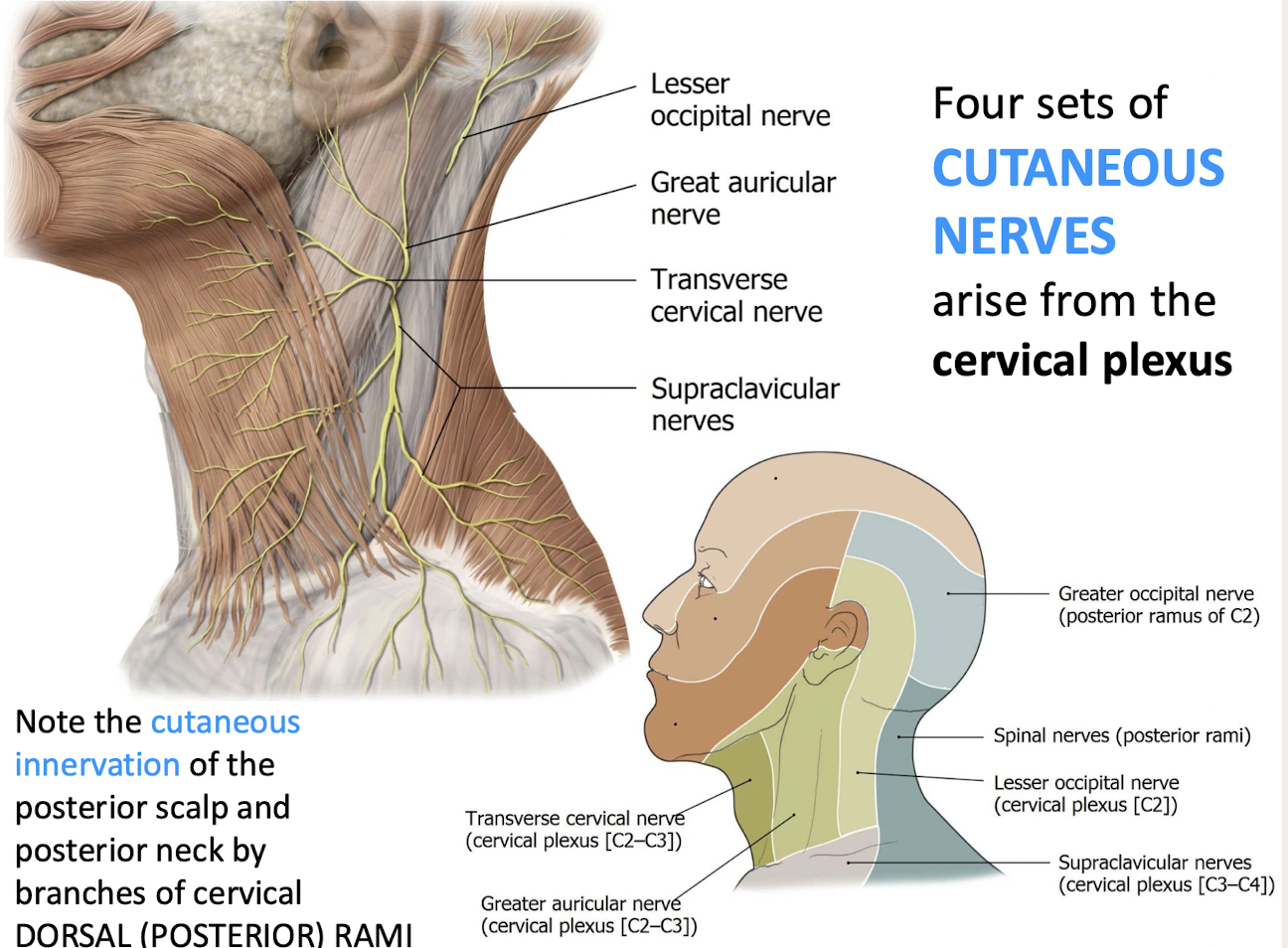
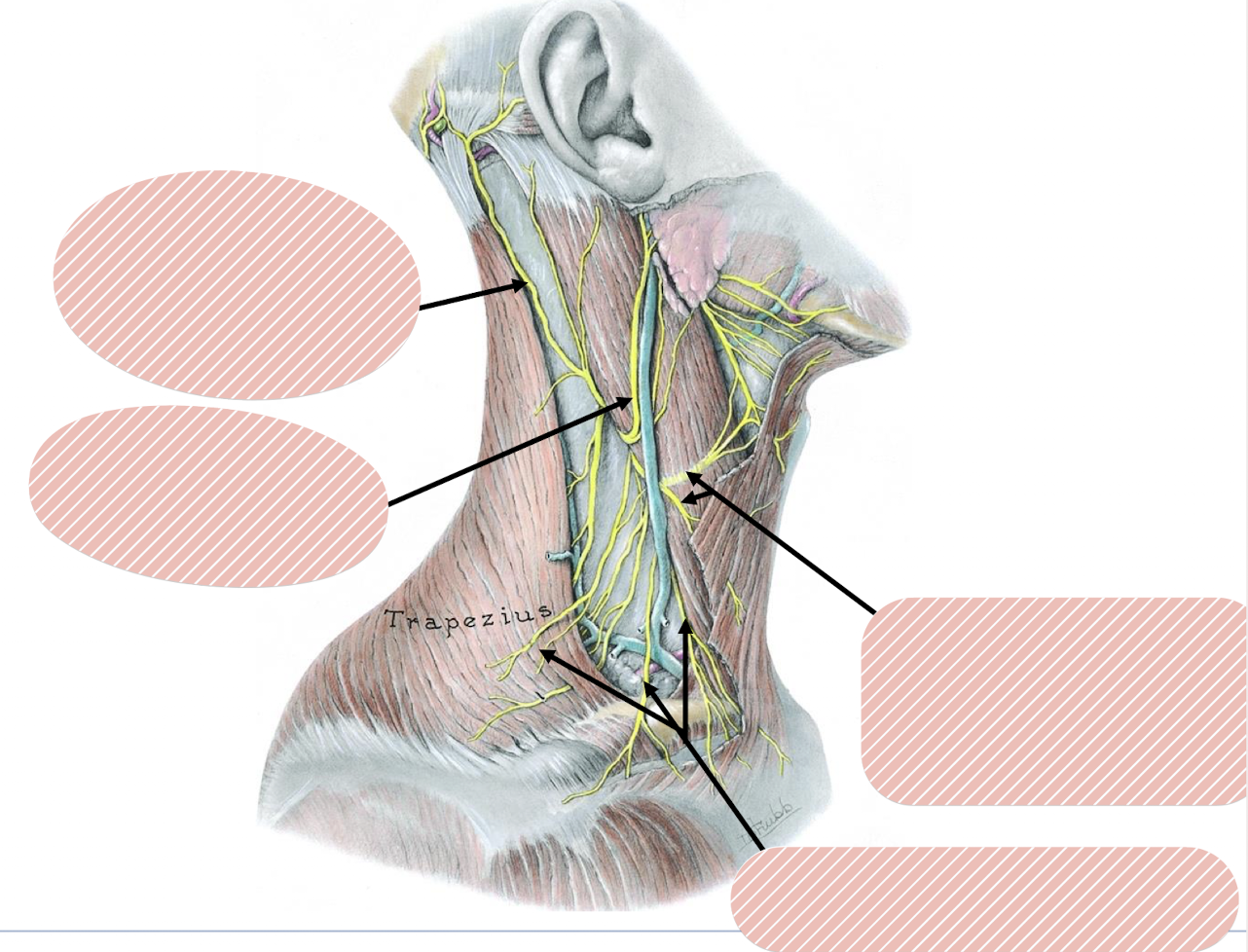
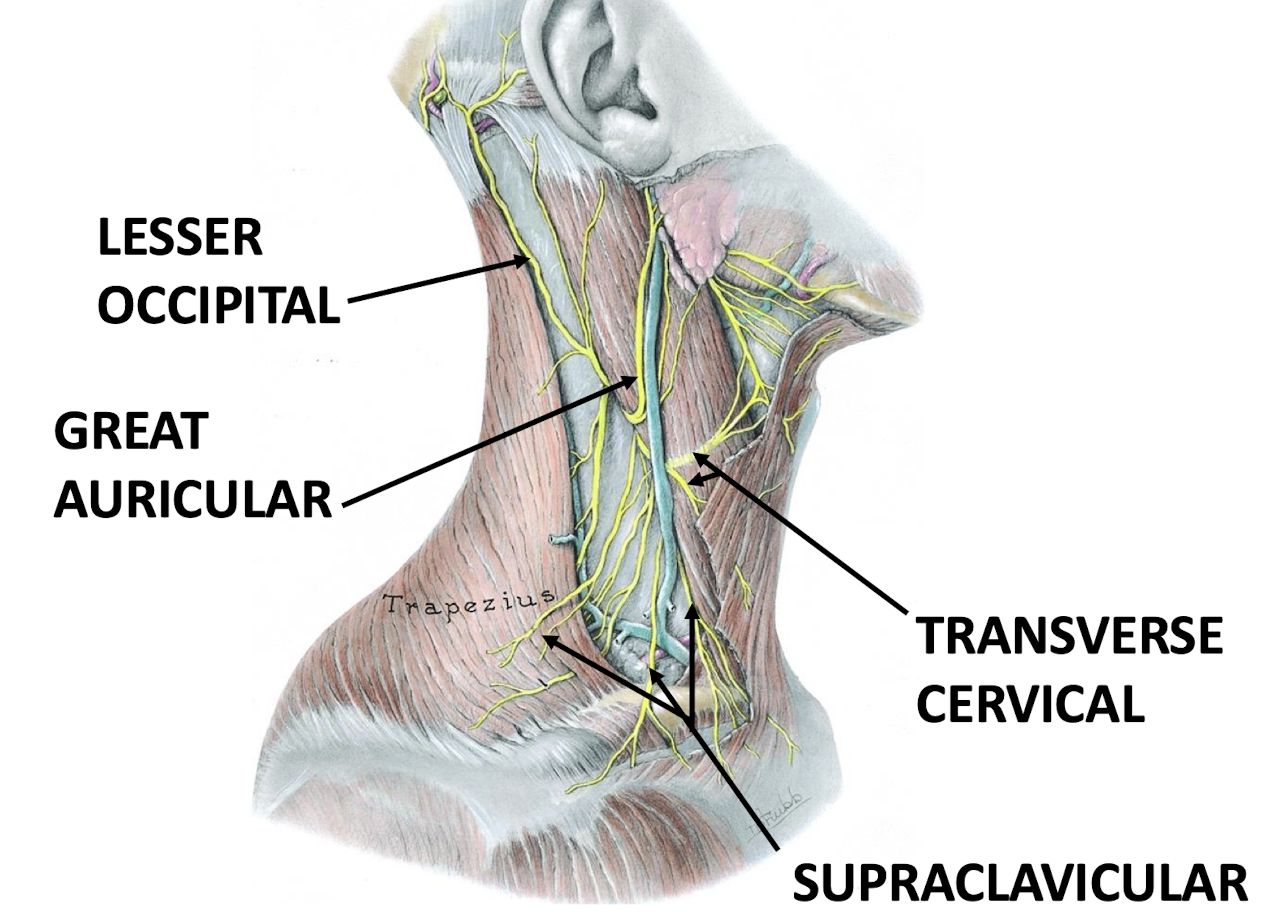
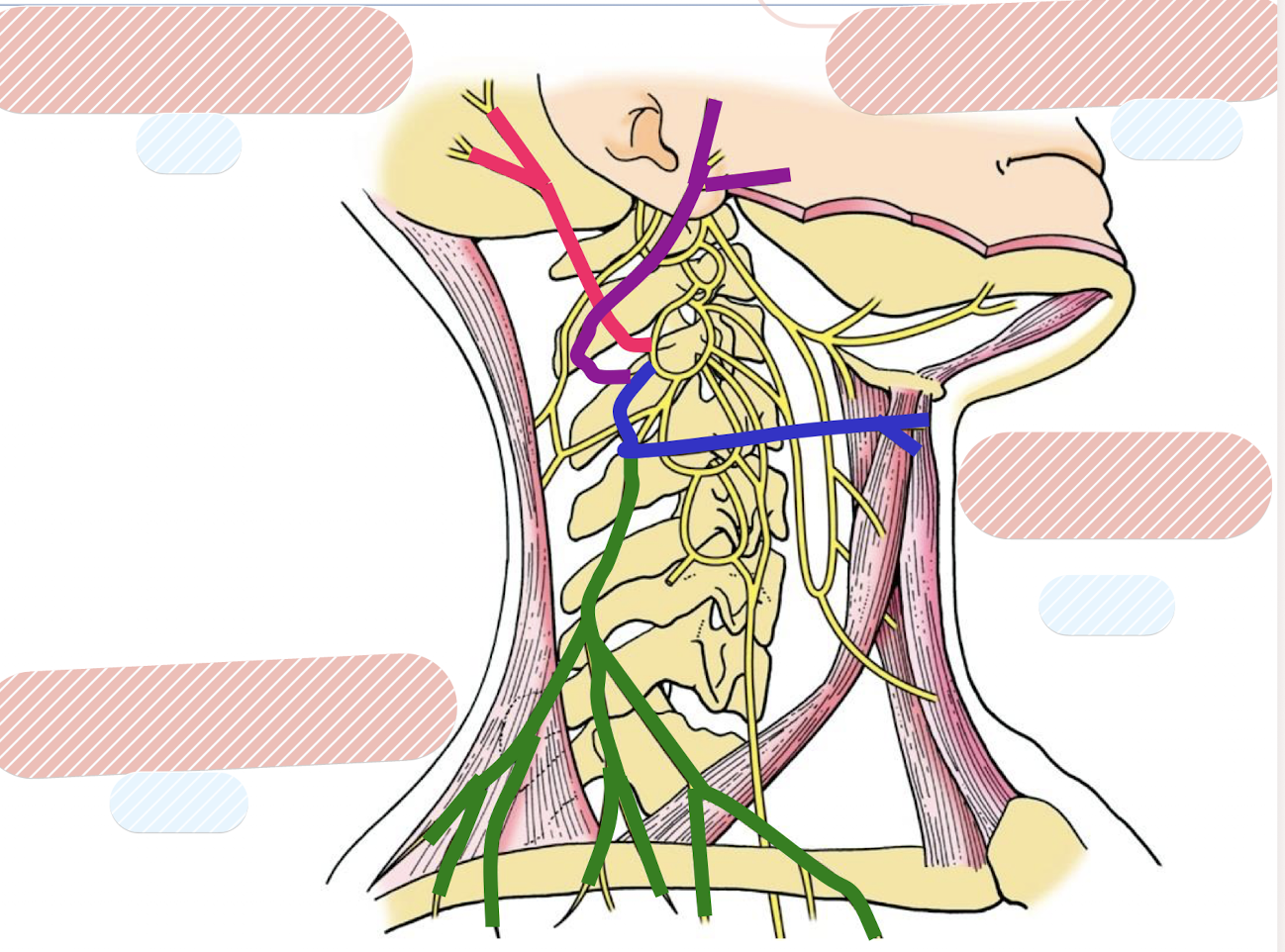
Label the nerves and what cervical branches they come from
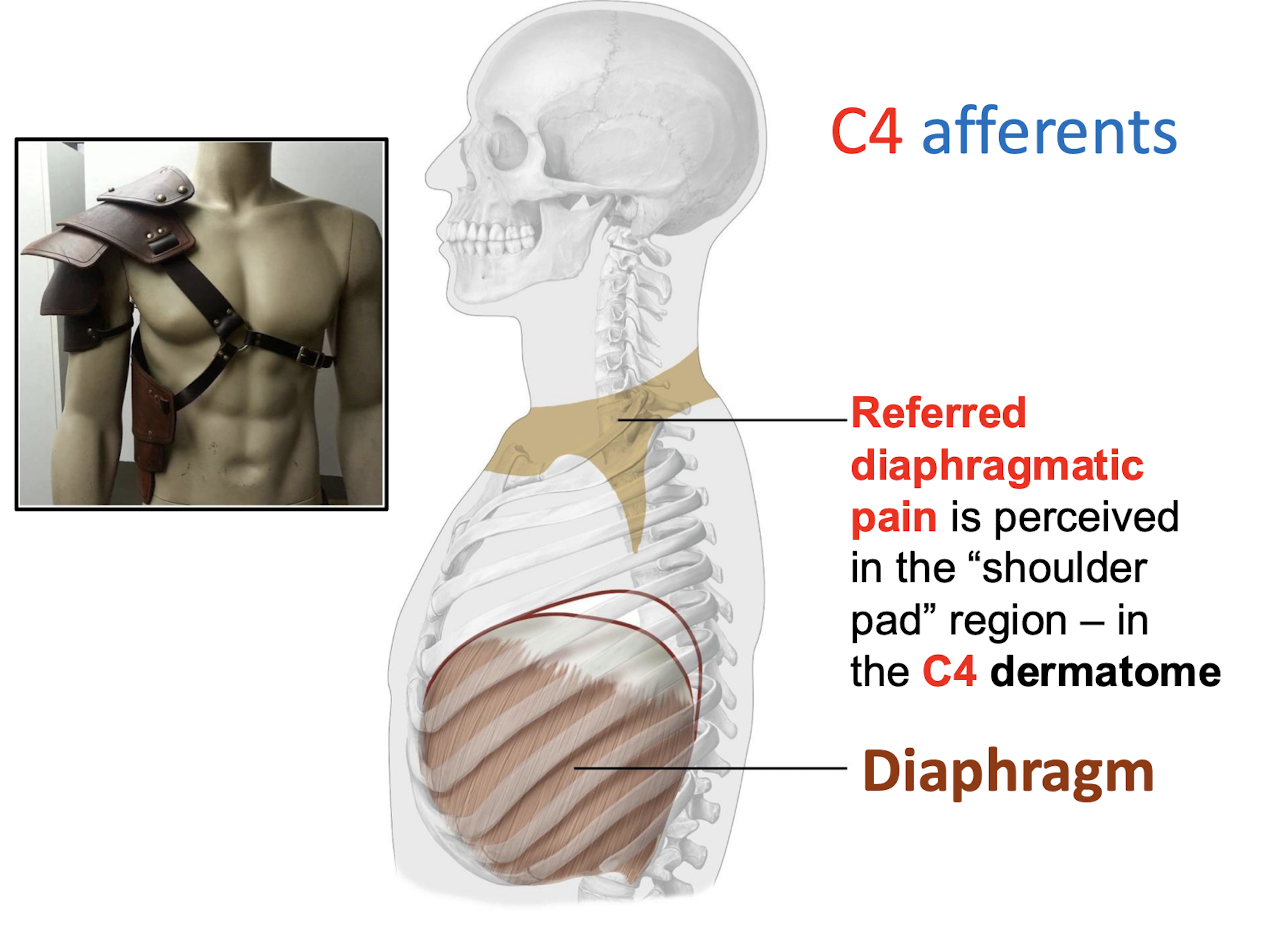
Referred diaphragmatic pain is perceived in what region; corresponding to which dermatome?
In the “shoulder pad” region; in the C4 dermatome by C4 afferents
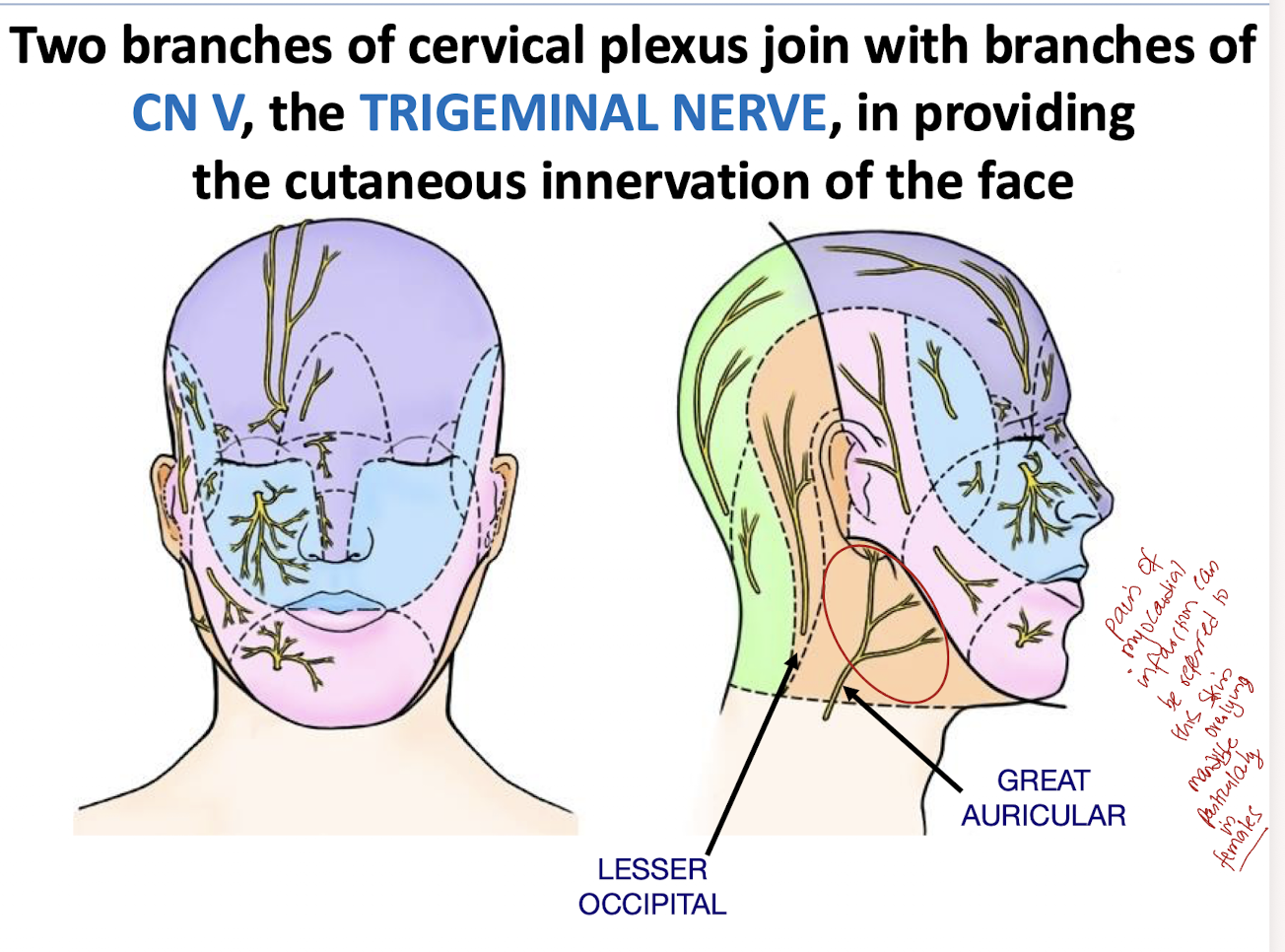
What two branches of the cervical plexus join with branches of the trigeminal nerve to provide cutaneous innervation of the face?
LESSER OCCIPITAL AND GREATER AURICULAR
What is ERB’S POINT (aka PUNCTA NERVOSUM) known for clinically?
These cutaneous nerves (from the cervical plexus) may all be anesthetized by an injection at this location
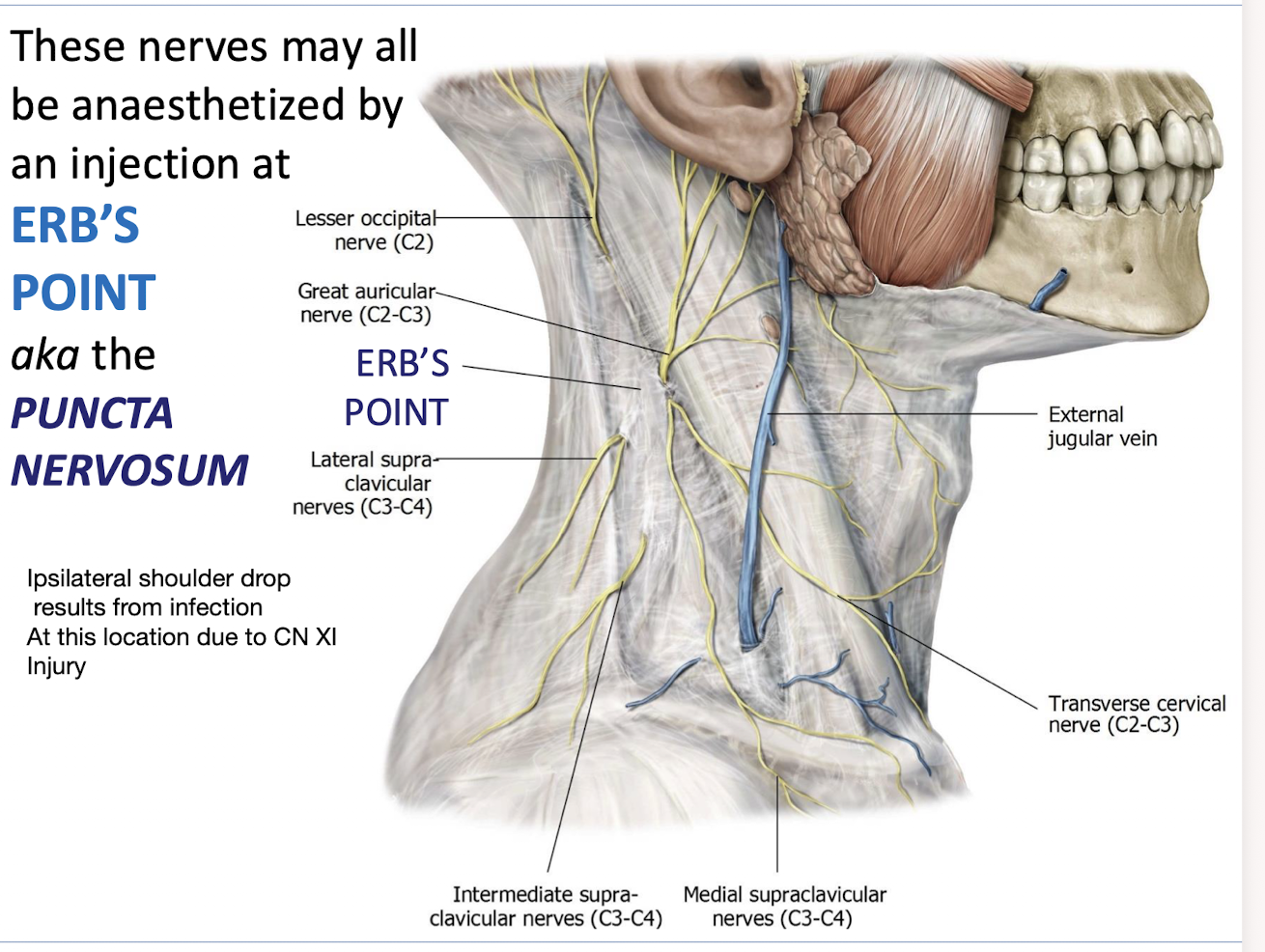
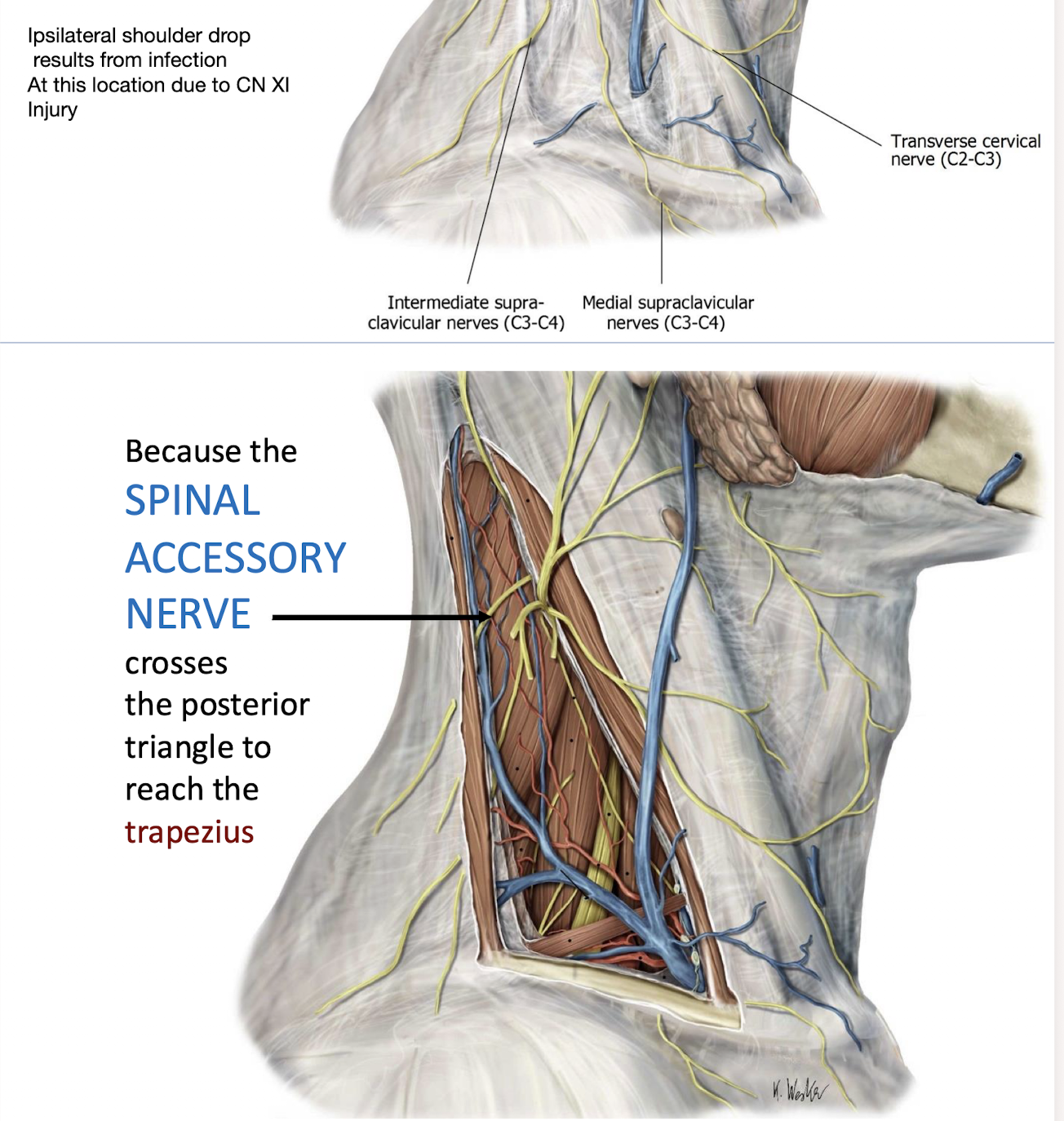
A patient develops Ipsilateral shoulder drop following a minor surgical procedure near the neck; what nerve was likely injured at Erb’s point?
The SPINAL ACCESSORY NERVE (CN XI); because it crosses the posterior triangle to reach the trapezius
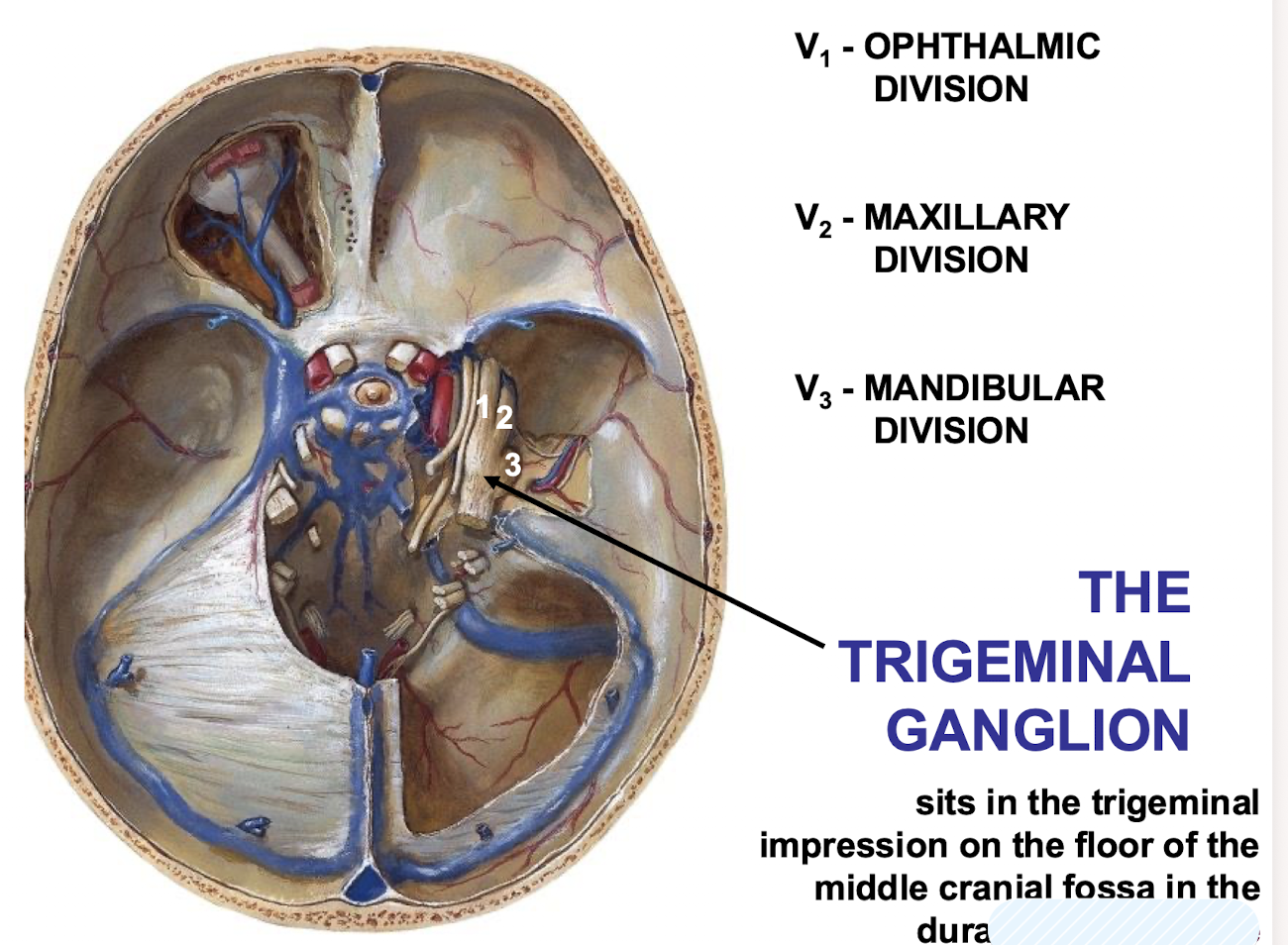
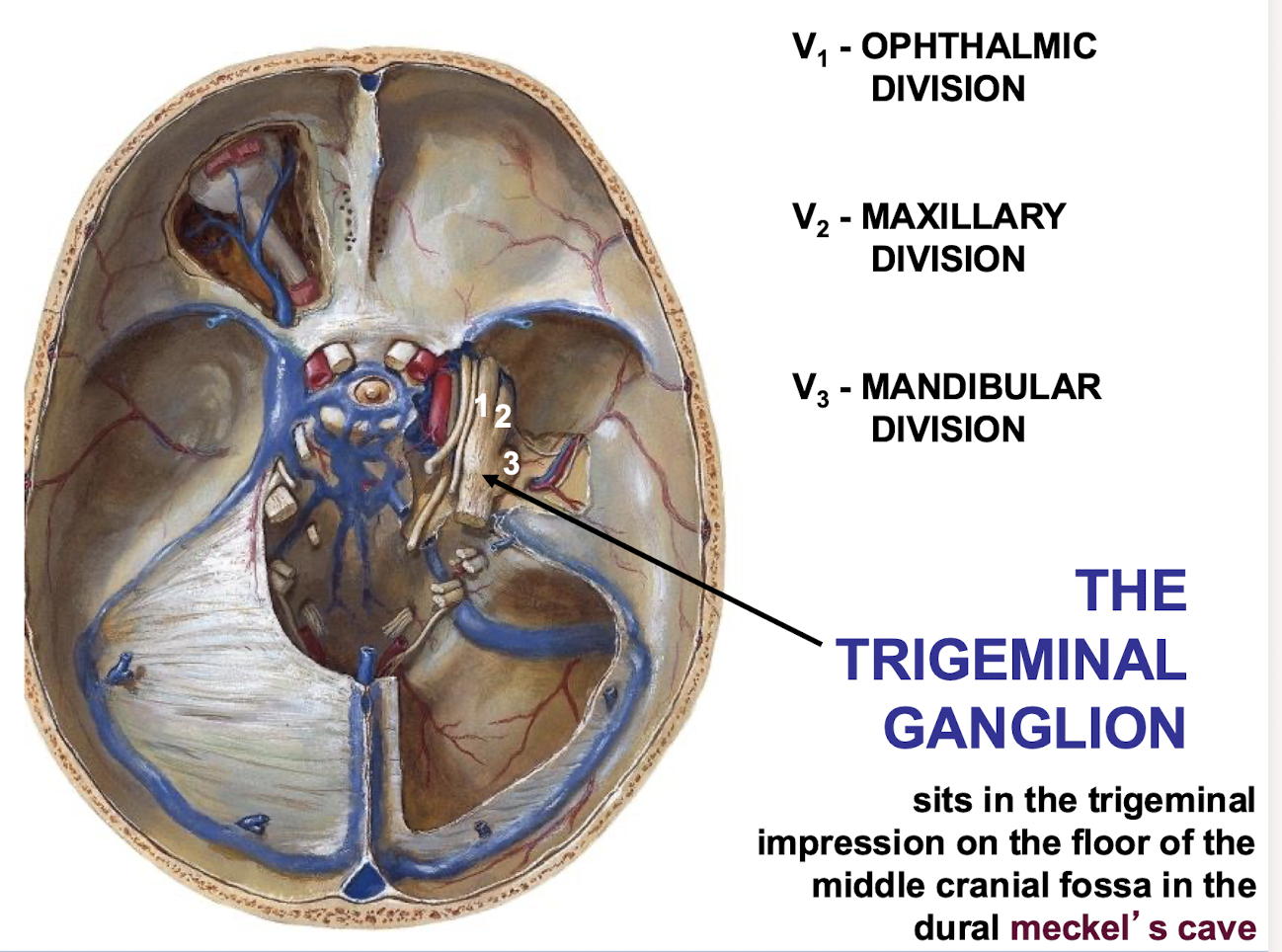
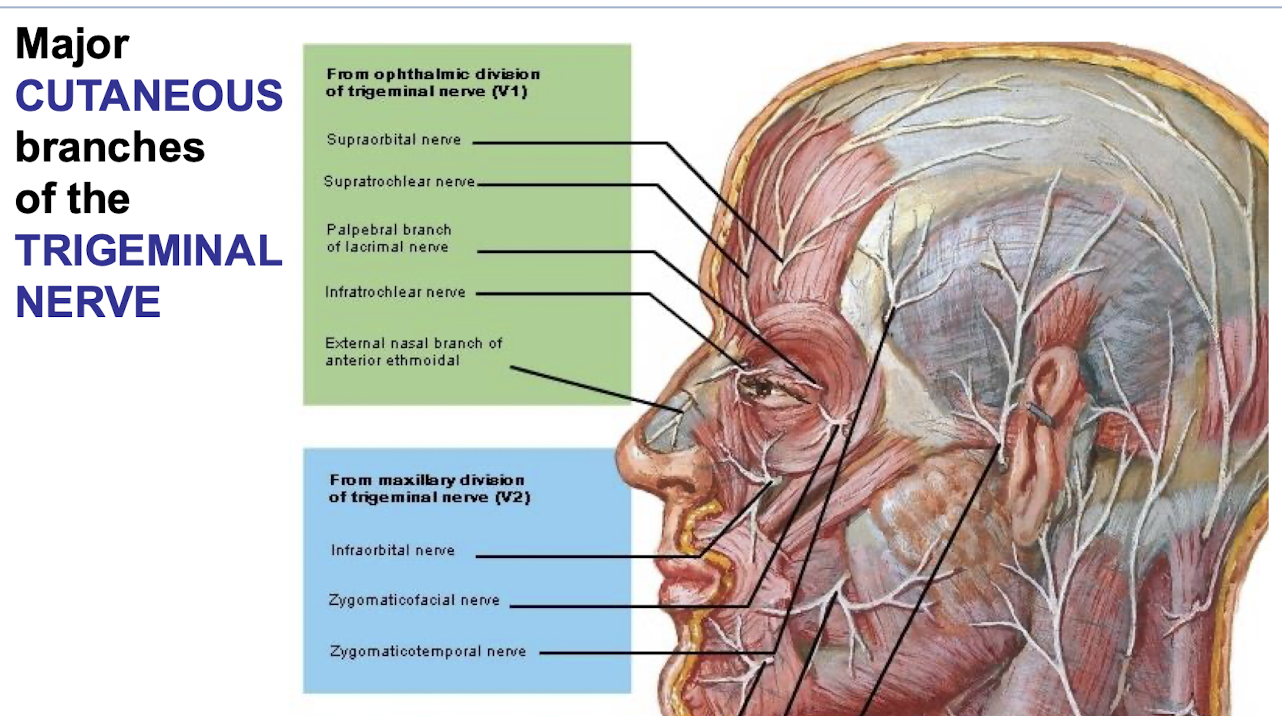
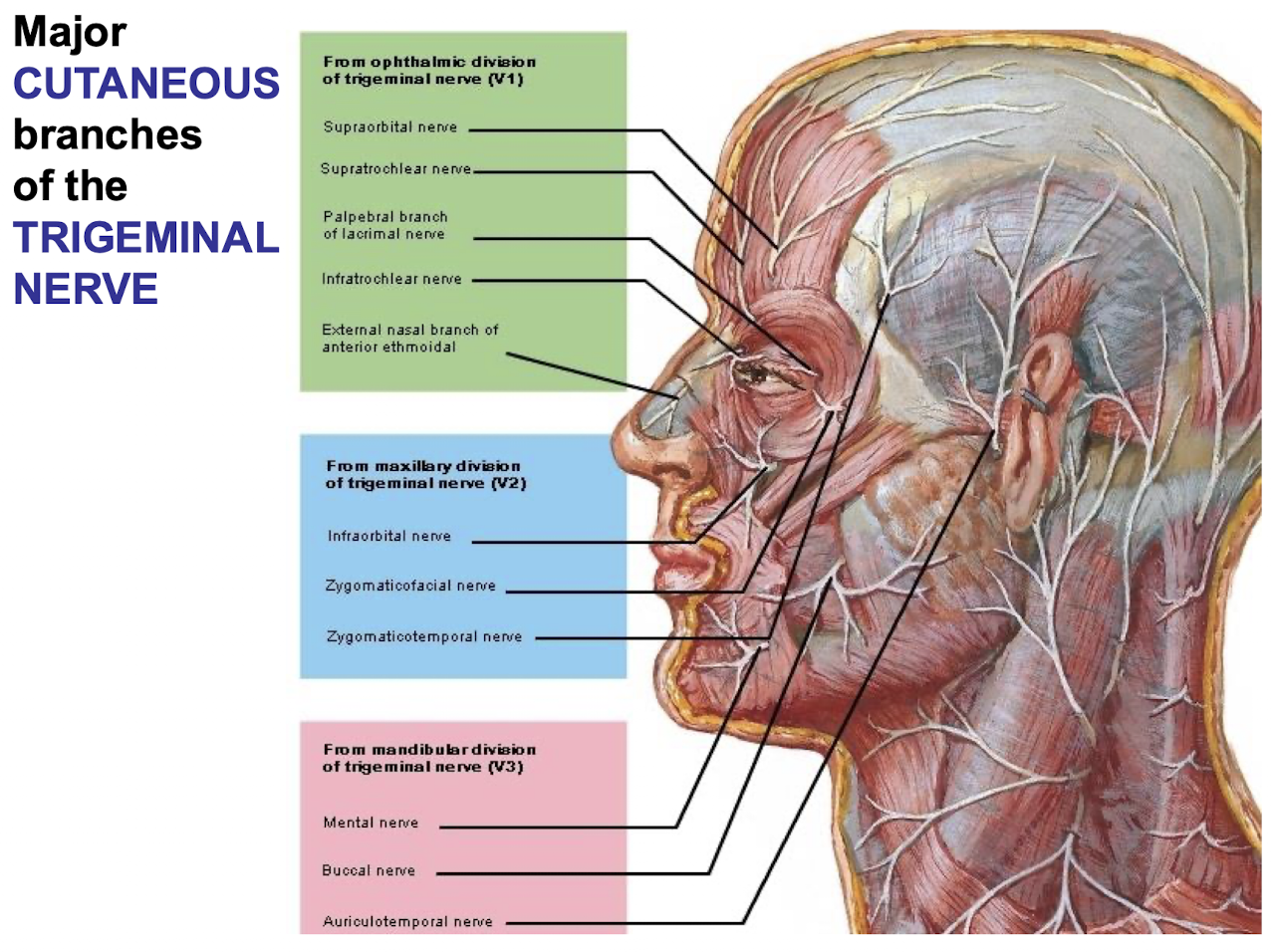
What are the three divisions of the TRIGEMINAL NERVE (CN V)?
V1 - OPHTHALMIC DIVISION; V2 - MAXILLARY DIVISION; V3 - MANDIBULAR DIVISION
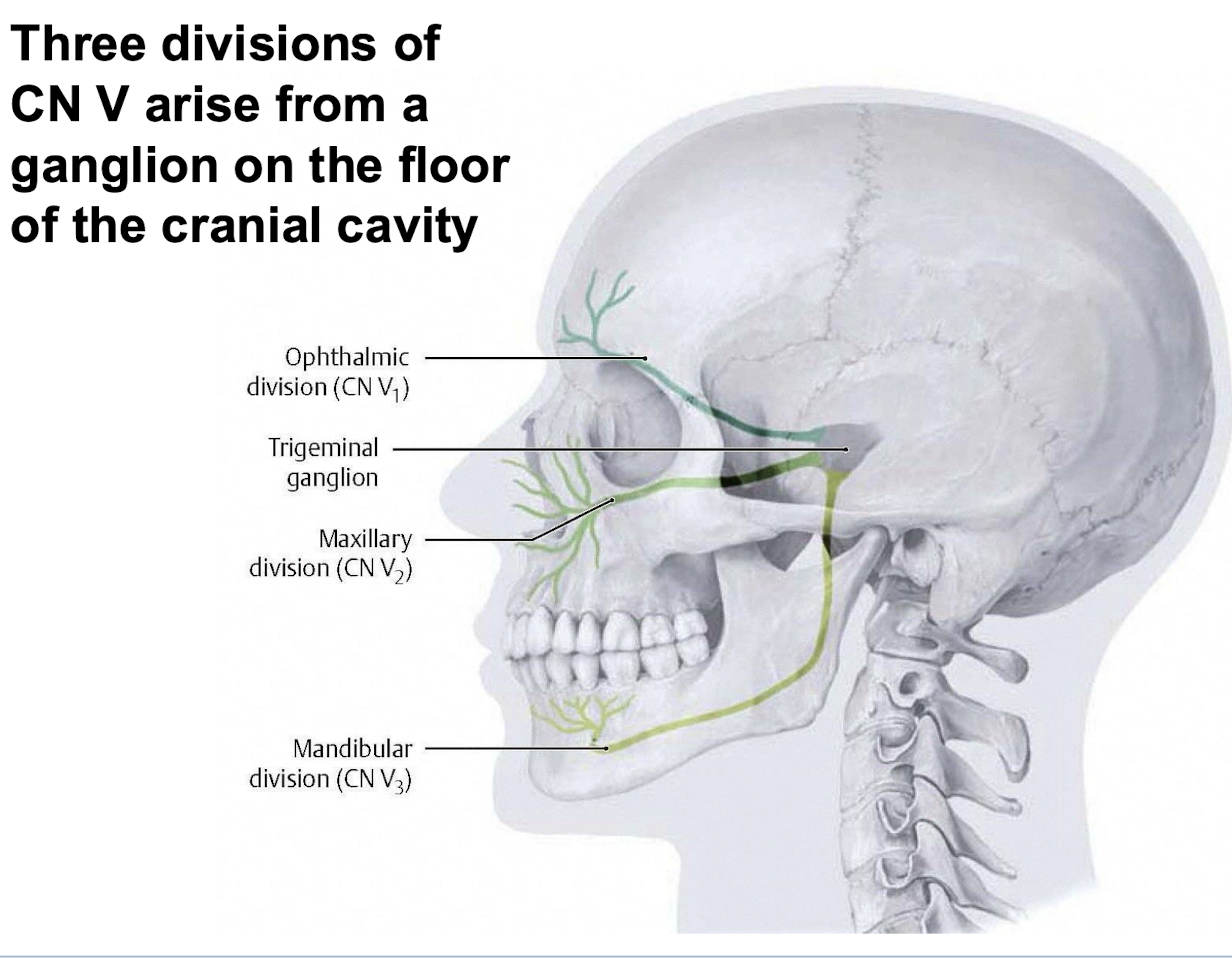
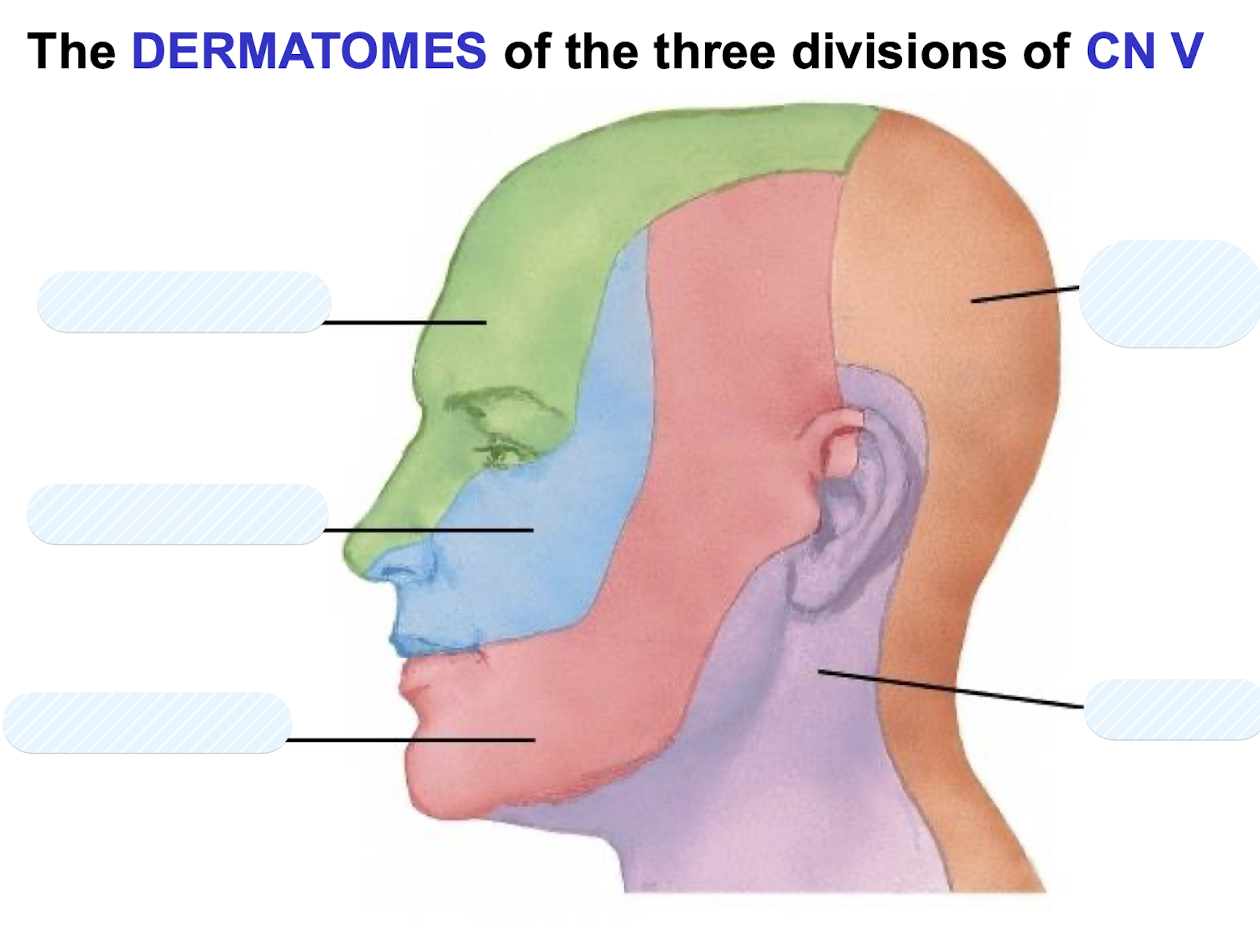
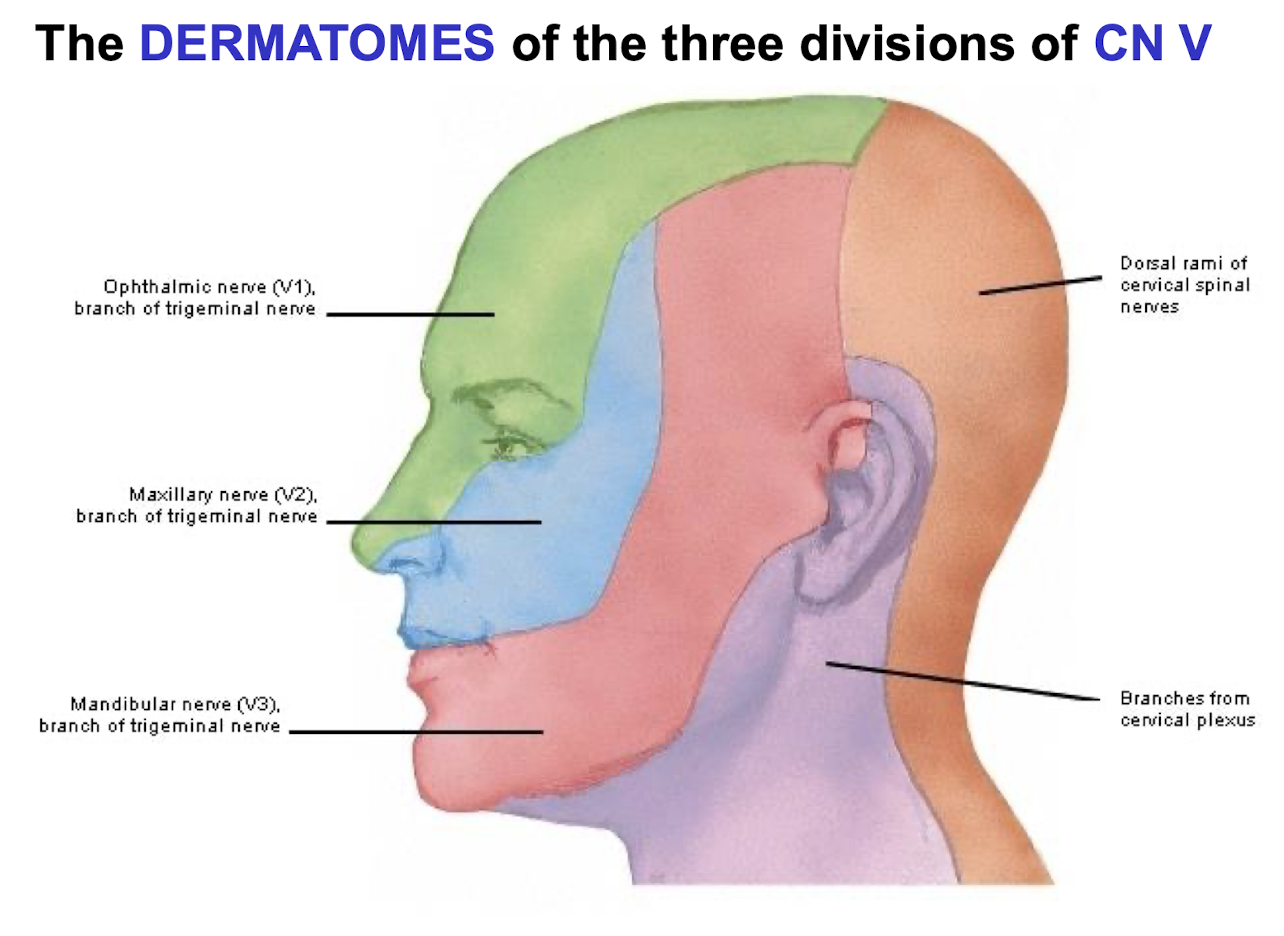
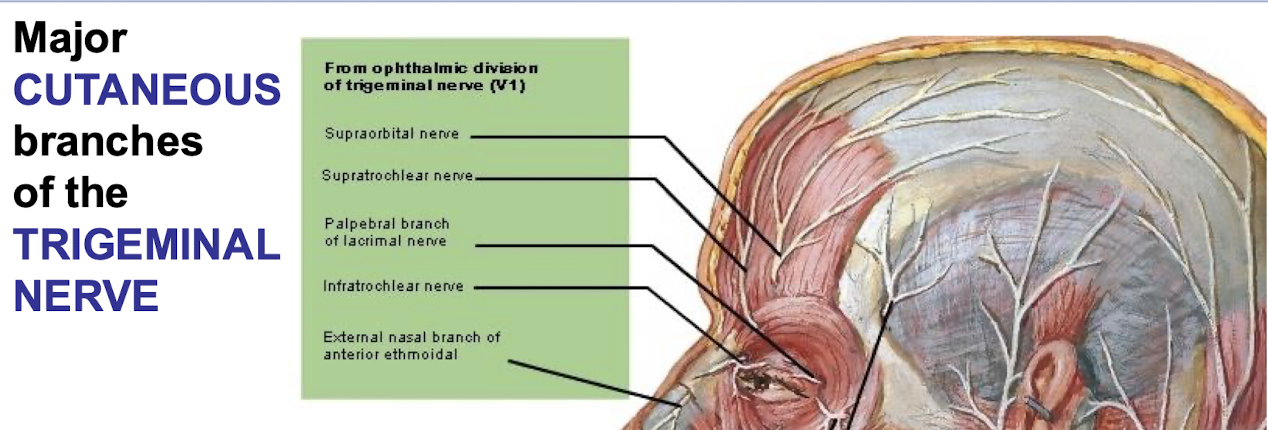
What are the major cutaneous branches of the ophthalmic division of the trigeminal nerve?
Supraorbital, supratrochlear, palpebral branch of lacrimal, infratrochlear, external nasal branch of anterior ethmoidal
What are the major cutaneous branches of the maxillary division of the trigeminal nerve?
Infraorbital, zygomaticofacial, zygomaticotemporal
What are the major cutaneous branches of the mandibular division of the trigeminal nerve?
Mental, buccal, auricotemporal
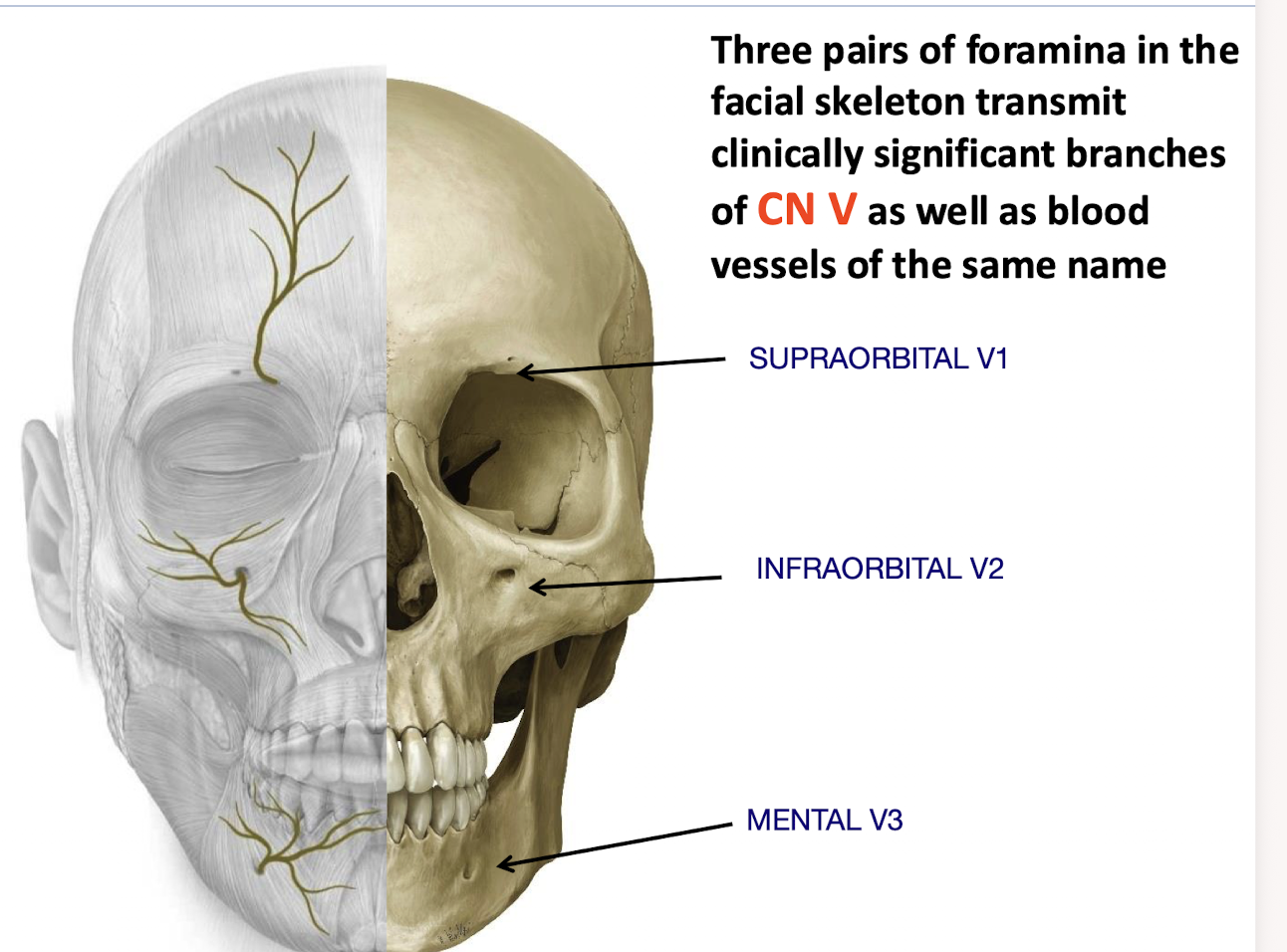
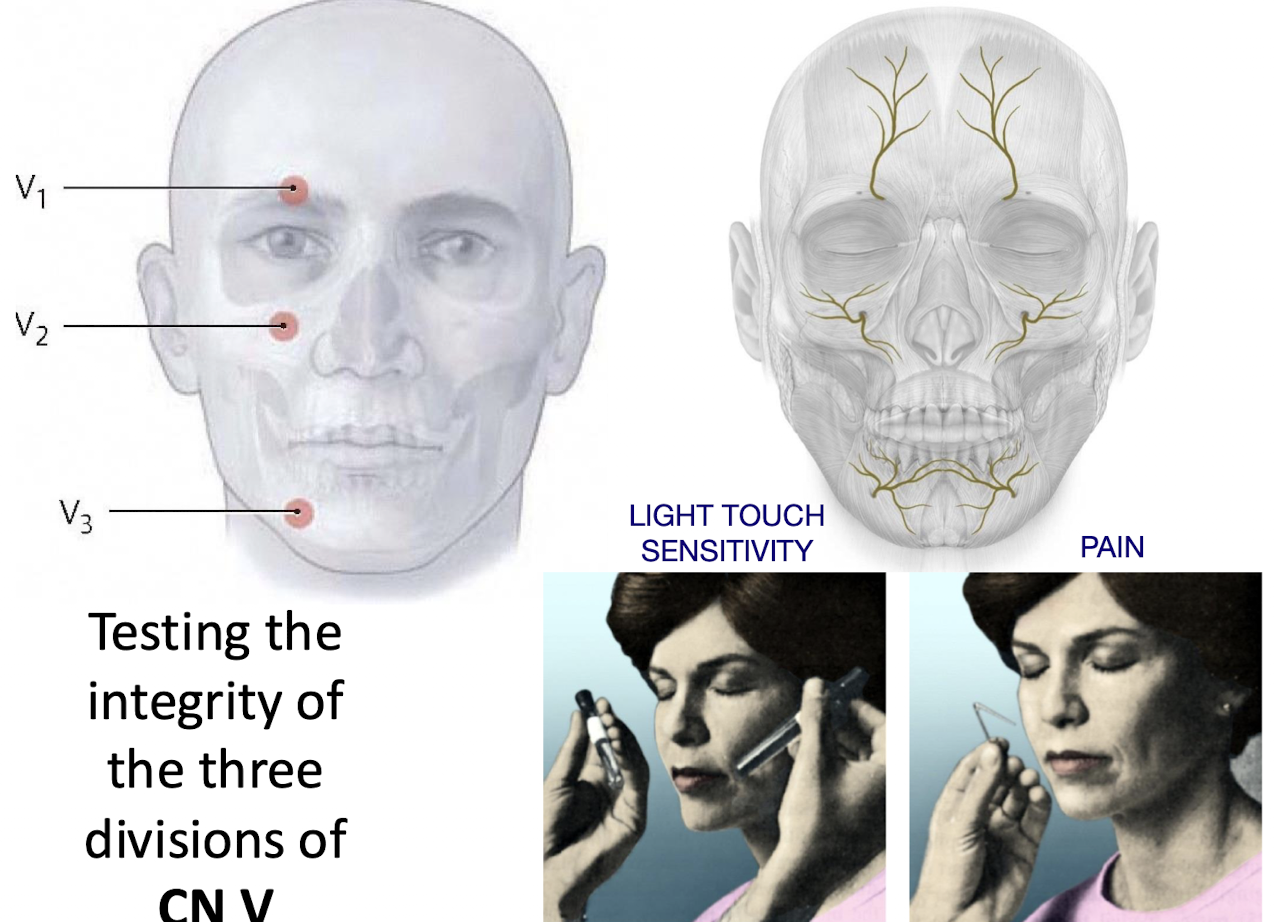
Which foramina in the facial skeleton transmit the cutaneous branches of V1; V2; and V3 respectively?
SUPRAORBITAL (V1); INFRAORBITAL (V2); MENTAL (V3)
How is the integrity of the trigeminal nerve (CN V) tested clinically?
Light Touch Sensitivity:
Use a cotton swab on various areas of the face.
Pain Sensitivity:
Use a pinprick to assess response to sharp stimuli
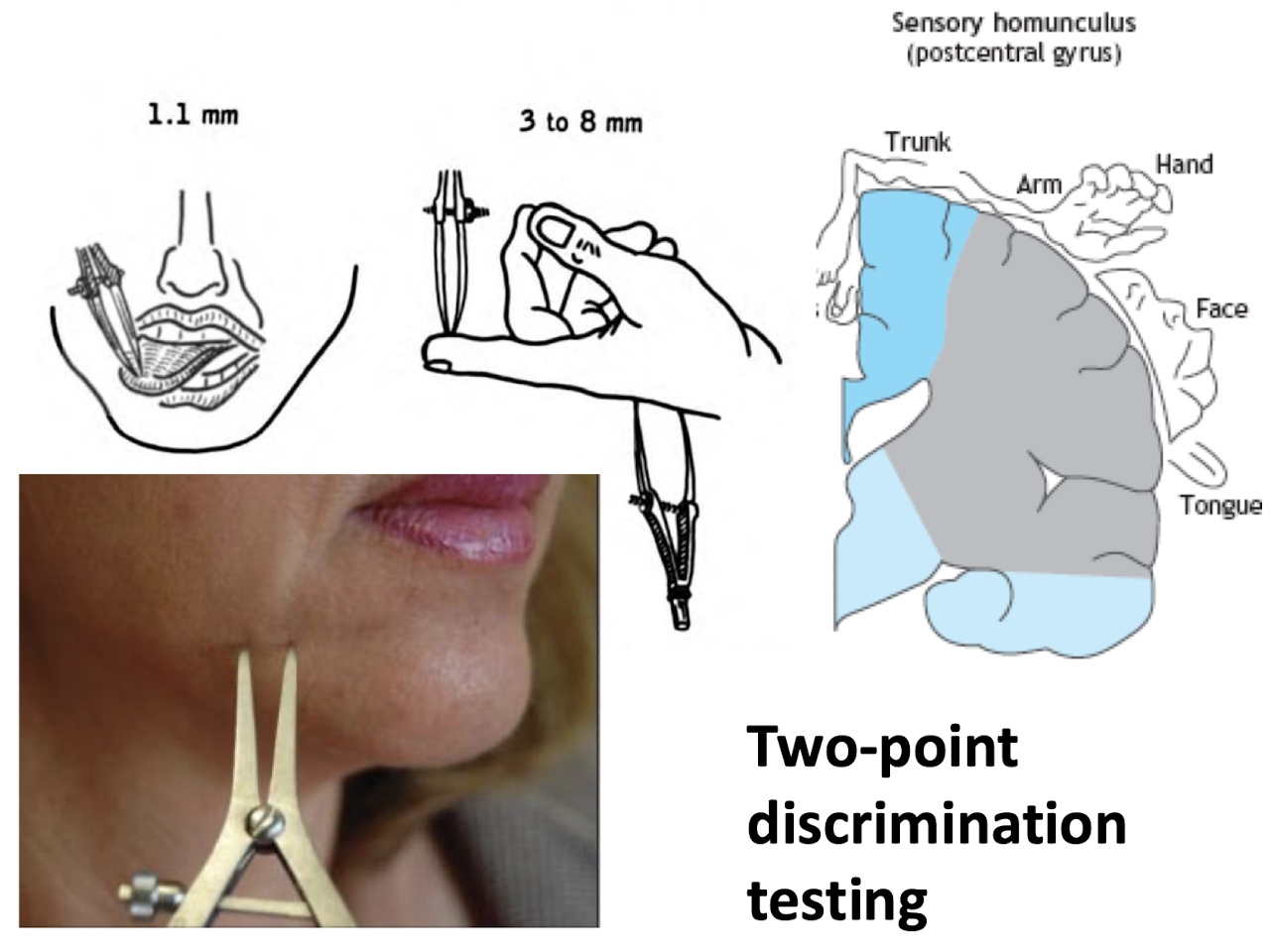
What is two-point discrimination testing and what does it assess? What is the most sensitive area?
Two-point discrimination testing assesses the ability to distinguish two separate points of contact on the skin.
Tool used: Caliper-like instrument
Sensitive areas (e.g., lips and tongue): Can detect points as close as 1.1 mm
Less sensitive areas (e.g., fingers): Detection ranges from 3–8 mm
Sensory homunculus: Represents varying tactile sensitivity across body regions (e.g., face and hands are more sensitive than trunk)
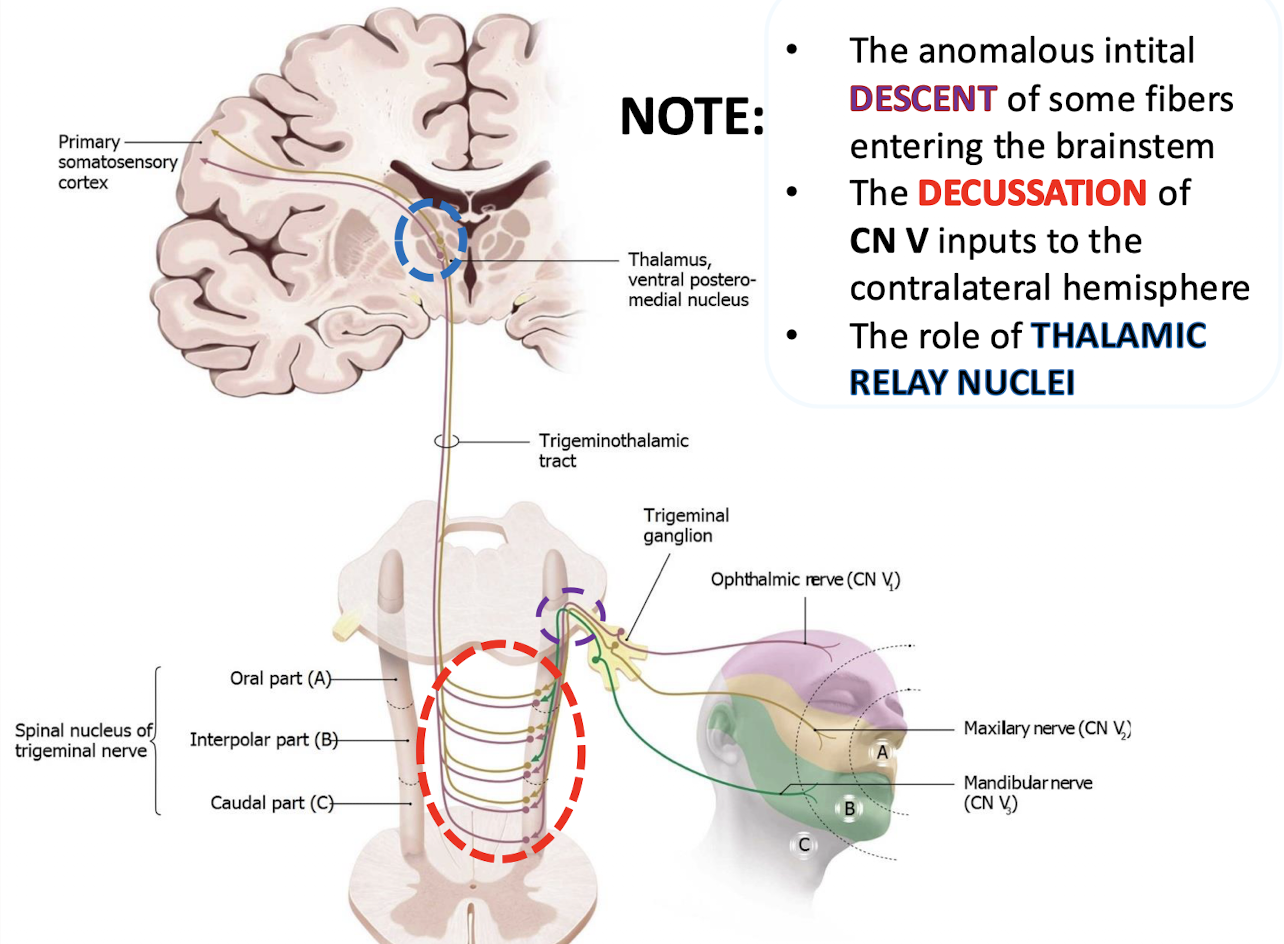
What does the trigeminal sensory pathway diagram show?
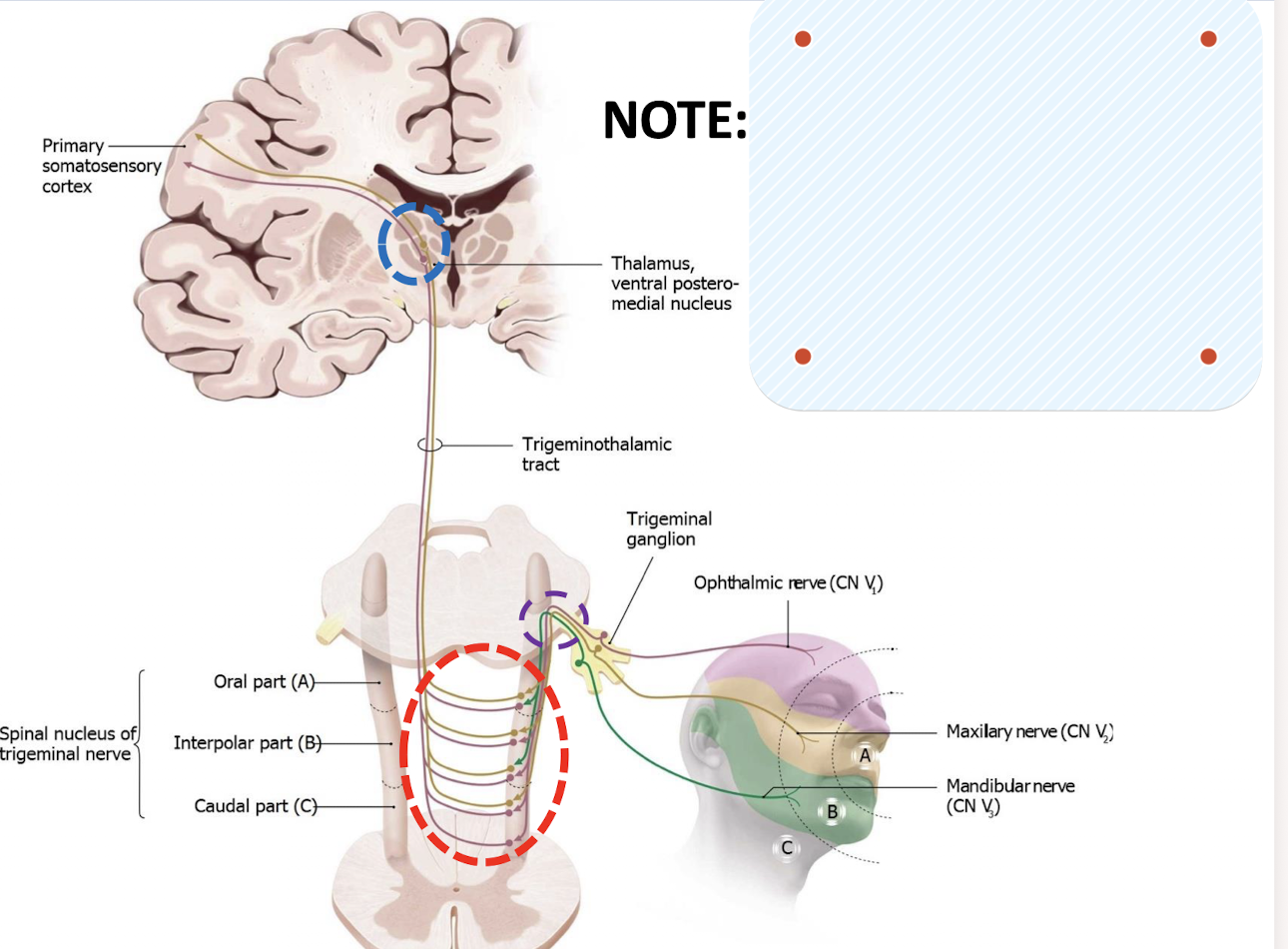
It shows how touch and pain signals from the face travel to the brain:
pain (and temperature) sensation from the left side of your face is processed by the right side of your brain.
The trigeminal nerve (CN V) carries sensory info (like pain and temperature) from the face.
When these fibers enter the brainstem, they descend first (that’s the “anomalous initial descent” part).
Then they decussate (cross over) to the contralateral side — meaning left → right or right → left.
From there, they ascend to the thalamic relay nuclei, which send the information to the somatosensory cortex on the opposite side.
Describe the symptoms of Trigeminal Neuralgia (Tic doloureux).
Lancinating (sharp stabbing pain) ; paroxysmal pain (sudden bursts of intense pain that goes quickly); intermittent; unilateral (one side of the face); disabling PAIN
What frequently triggers the pain in Trigeminal Neuralgia?
Moving the mandible; smiling or yawning; or by cutaneous or mucosal stimulation
What demographic experiences Trigeminal Neuralgia and what divisions of the nerve is it frequently found in
Almost always adults, often seniors. usually within the 2nd or 3rd divisions (maxillary and mandibular)
What is the suspected etiologies of Trigeminal Neuralgia
Demyelination or compression of the sensory root endocranially (often by the superior cerebellar artery)
postherpetic neuralgia
tongue piercing
idiopathic
What are the treatment options for Trigeminal Neuralgia?
Analgesics; anticonvulsants; surgical decompression; rhizotomy; gamma knife ablation
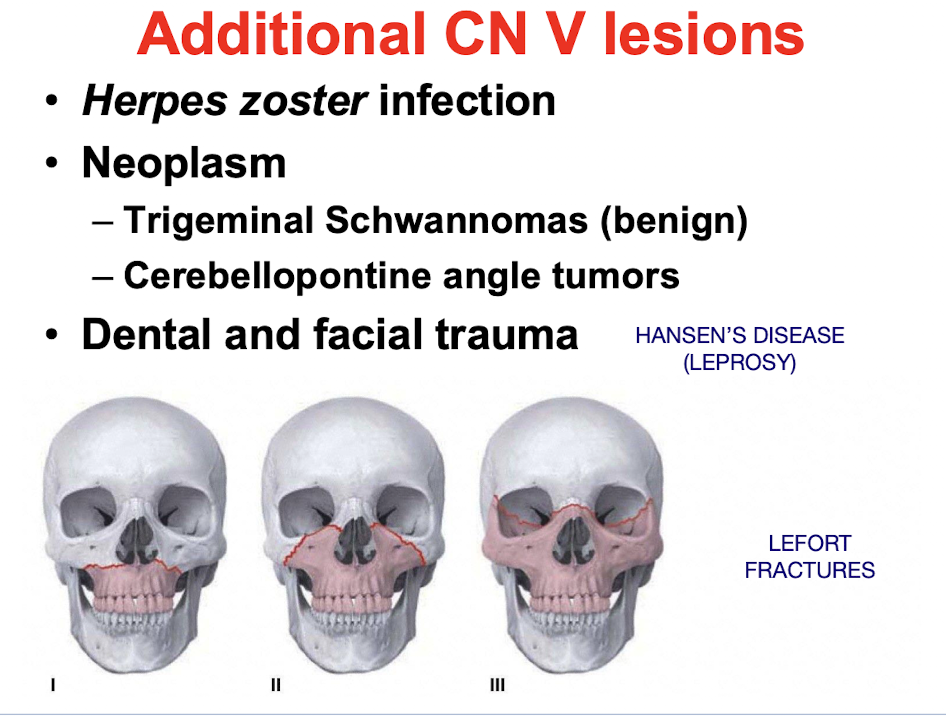
What are some other CN V lesions (not trigeminal neuralgia/ tic doloureux)
Herpes Zoster Infection
Neoplasm
Trigeminal schwannomas (benign)
cerebellopontine angle tumors
Dental and facial trauma
Hansen’s disease (leprosy)
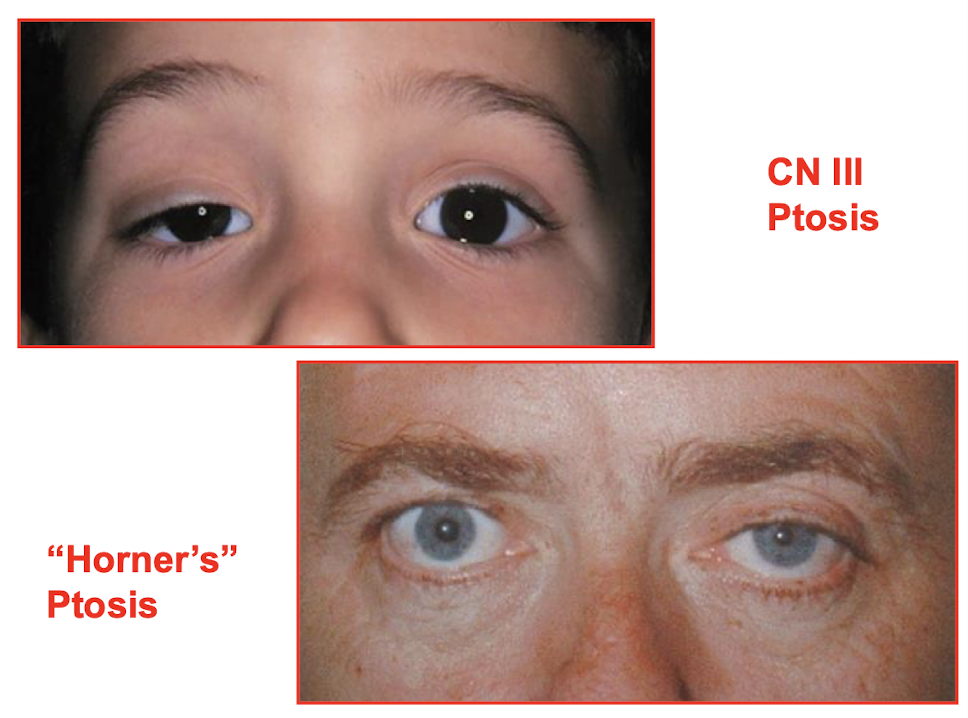
Which two muscles are responsible for raising the upper eyelid; and how do they differ in innervation and muscle type?
LEVATOR PALPEBRAE SUPERIORIS (skeletal muscle; innervated by CN III OCULOMOTOR runs from the orbital roof to the deep surface of the upper eyelid); and the SUPERIOR TARSAL MUSCLE (SMOOTH muscle; innervated by sympathetics).
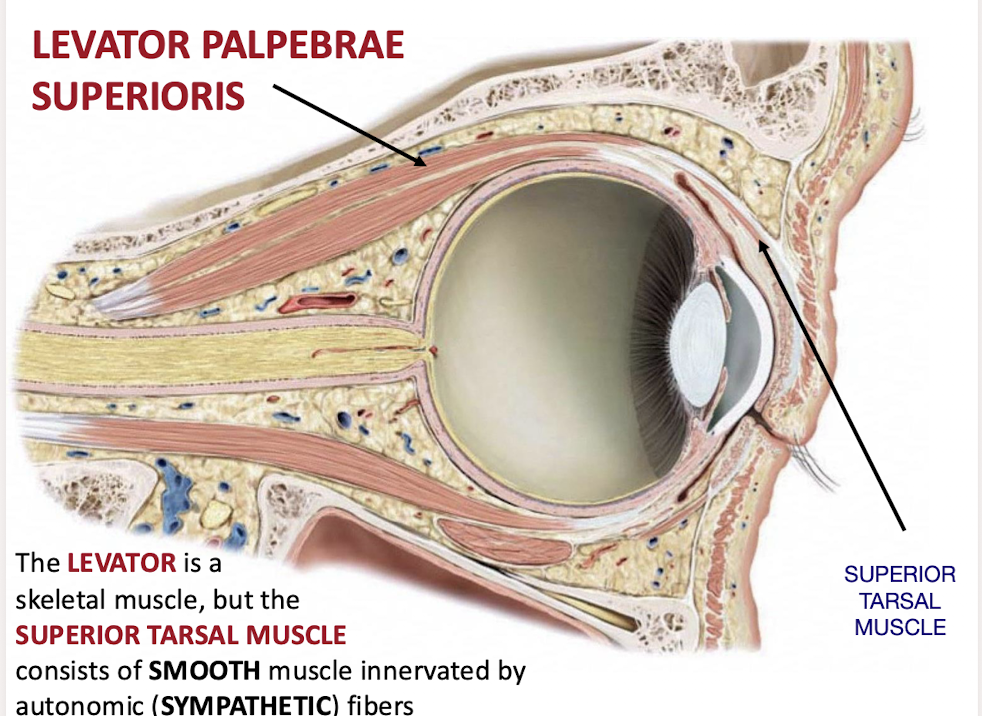
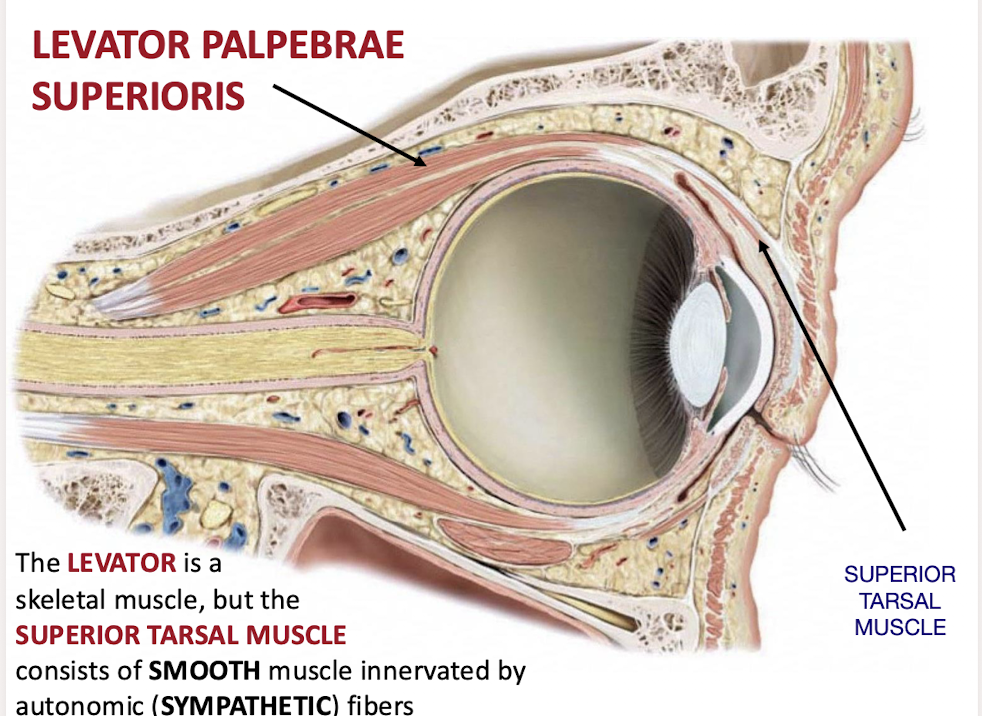
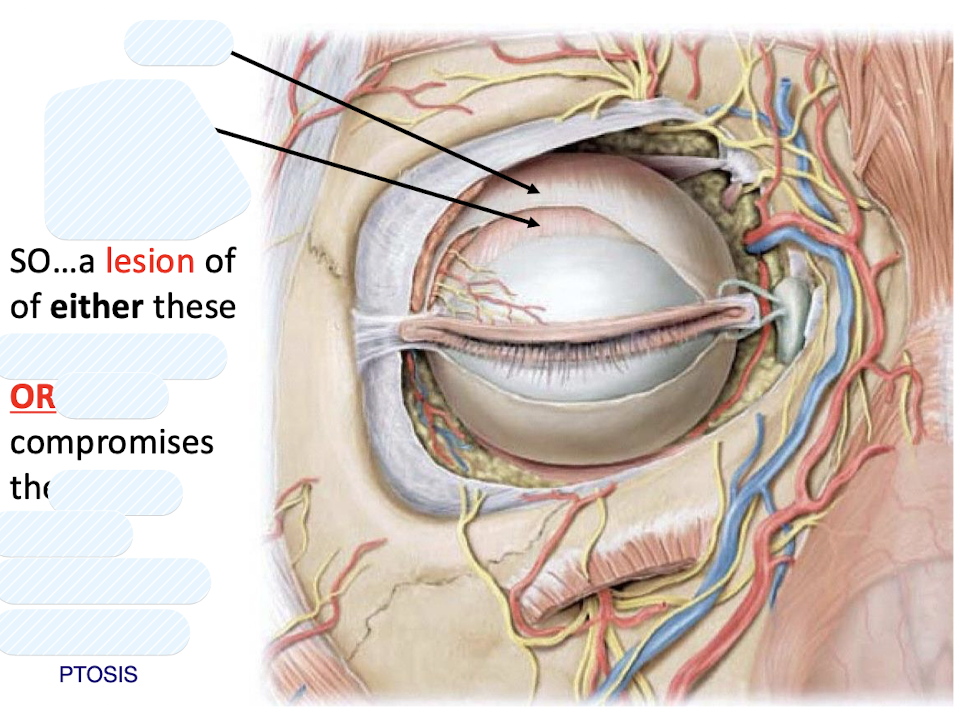
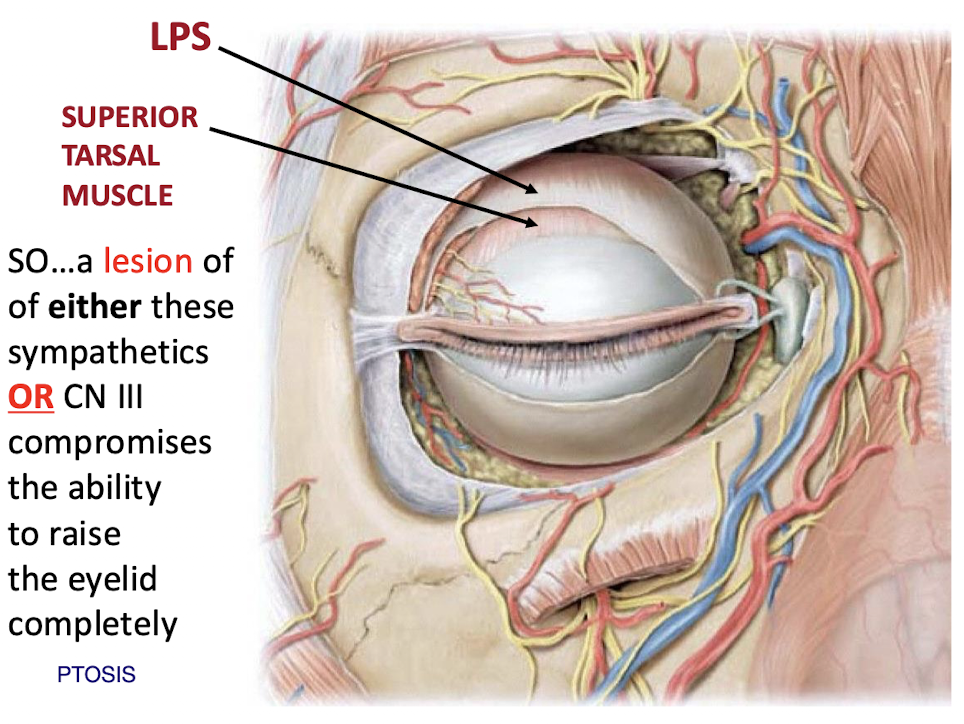
A patient presents with PTOSIS; what two distinct neurological lesions could be the cause?
A lesion of either the sympathetic innervation (“Horner’s” Ptosis) OR CN III (“CN III Ptosis”)