Patho Exam 3
1/176
Earn XP
Description and Tags
Patho Block 3 Exam
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
177 Terms
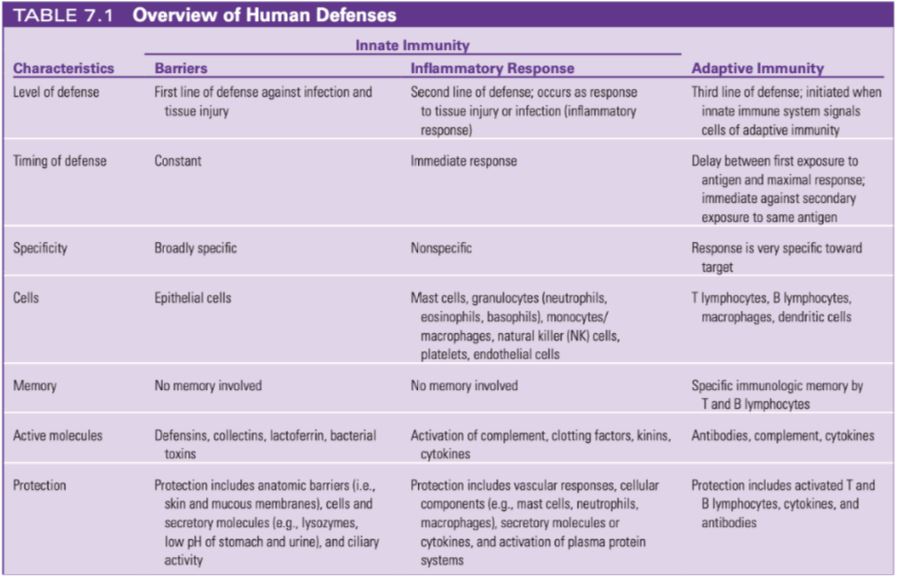
Compare and contrast key components of the first, second, and third lines of defense; timing, specificity; cells involved, memory, and peptides / active molecules involved.
What are the three plasma proteins systems?
Complement system, Clotting (coagulation) system, Kinin System
Complement System
destroys pathogens directly activates every component of inflammatory response.
Clotting (coagulation) system
prevents infection spread by trapping microorganisms at site of inflammation, stops bleeding/ creates clots, framework for repair.
Kinin system
activate and assist inflammatory cells by producing bradykin.
Sequence events in the acute inflammatory response
Initiated by guardian cells located near epithelial surfaces, lymph nodes, or blood vessels
Release of inflammatory mediators
Vascular and cellular responses
Migration of leukocytes, platelets, plasma proteins and other biochemical mediators
Local signs of acute inflammation
Redness (Rubor):
Caused by increased blood flow due to vasodilation.
Heat (Calor):
Also due to increased blood flow and metabolic activity in the inflamed area.
Swelling (Tumor):
Resulting from increased vascular permeability and the accumulation of fluid in the tissues.
Pain (Dolor):
Induced by the release of inflammatory mediators that sensitize pain receptors and pressure on surrounding tissues.
Systemic signs of acute inflammation
Fever
Caused by exogenous and endogenous pyrogens
Acts directly on the hypothalamus
Leukocytosis
Increased numbers of circulating leukocytes
Increase in circulating immature leukocytes (bands)
Increased plasma protein synthesis
Acute-phase reactants
Fatigue and Malaise:
General feelings of discomfort and fatigue due to the body's systemic response to inflammation.
What are the 3 cytokines?
Interleukins, Interferon, Tumor Necrosis Factor-Alpha (TNF-alpha)
Who forms TNF-Alpha?
Activated Macrophages (via secretion)
Mast cells, lymphocytes, and neutrophils to a lesser extent
Who forms Interleukins (IL)?
Macrophages and Lymphocytes as a response to microorganisms or stimulation by inflammation
Who forms Interferons (IFN-alpha, IFN-beta, IFN-gamma)?
Virally-infected host cells
Function of TNF-alpha
Major proinflammatory cytokine
Induces fever
Increases acute phase protein synthesis in the liver
Function of Interleukins (IL)
Regulation of CAMs
Chemotaxis
Production of leukocytes in the bone marrow
Modulation of the innate and adaptive immune responses
Function of Interferons
Prevents viruses from infecting additional healthy cells (does not directly kill viruses)
alpha and beta: induce the production of antiviral proteins in neighboring cells
gamma: increases microbicidal activity of macrophages
Causes of Mast Cell Degranulation
Activated by: physical injury, chemical agents, PRRs, complement, IgE - antibodies
chemicals released in two ways: degranulation, synthesis of lipid-derived chemical mediators
Effects of the released mediators from degranulation
Degranulation
releases histamine
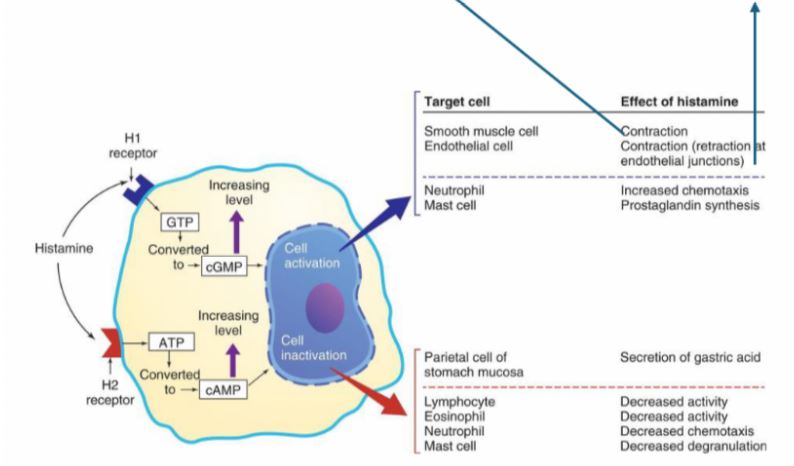
H1 receptor (proinflammatory): causes vasodilation, endothelial cells that line the capillaries are retracted to create space (so leukocytes can squeeze through and infiltrate tissue)
H2 receptor (anti-inflammatory): downregulates release of histamine, negative feedback
can be expressed on same cell, work antagonistically
releases chemotactic factors
neutrophil chemotactic factor attracts neutrophils
eosinophil chemotactic factor of anaphylaxis (ECF-A) attracts eosinophils
cytokines
promote inflammation
active adaptive immune response
Effects of Leukotrienes
similar effect as histamine, later stages of inflammation, made from arachidonic acid
Effects of Prostaglandins
similar effect as histamine, induces pain, made by cyclooxygenase (COX)
meds that inhibit COX: NSAIDs, aspirin, acetaminophen (tylenol)
ouch!
Effects of Platelet-activating factor
blood vessel dilation and platelet aggregation, mediates allergic responses (airway inflammation) and shock
Effect of histamine binding to H1 and H2 Receptors
H1 receptor (proinflammatory)
Histamine binding to H1 causes vasodilation
Endothelial cells that line the capillaries are retracted
• H2 receptor (anti-inflammatory)
- Can be expressed on the same cell
Work antagonistically to each other
Process of Phagocyte Migration
phagocytes arrive
newly expressed CAMs allow for margination on epithelial cells
diapedesis occurs
chemotaxis occurs
migration toward higher concentrations of chemokines
phagocytosis!
Process of Phagocytosis Migration
Opsonization (glue between the phagocyte and the target cell by C3b, making the foreign cell more susceptible to phagocytosis), recognition, and adherence
Engulfment: small pseudopods surround the adherent microorganism
Phagosome formation
Fusion with lysosomal granules: creates phagolysosome
Destruction of the target
Role of Neutrophils in Inflammatory Process
also called polymorphonuclear neutrophils (PMNs)
predominate in early inflammatory responses
ingest bacteria, dead cells and cellular debris
short lived, become components of purulent exudate (pus)
primary roles: removal of debris in sterile lesions, phagocytosis of bacteria in nonsterole lesions
Role of Monocytes in the Inflammatory Process
monocytes become activated and become macrophages.
Role of Macrophages in the Inflammatory Process
Kuppfer cells in liver
Alveolar macrophages in lung
microglia in brain
are either proinflammatory or antiinflammatory
actions are pleiotropic: same molecule may have large variety of different biologic activities, depending on the target cell to which it binds
includes interleukins, interferons, tumor necrosis factor (TNF)
Role of Eosinophils in Inflammatory Process
provide defense against parasites and regulate vascular mediators
help control vascular effects of inflammation
Characteristics of Chronic Inflammation/Differs from Acute
Chronic inflammation: 2+ weeks in duration, usually related to unsuccessful acute inflammatory response
differs b/c inflammatory response doesn’t stop when infection/threat is eliminated, body keeps receiving inflammatory signals
subtler signs/presentation than acute inflammation
periods of getting better then worse, can fluctuate in severity
What is immunity?
Innate and adaptive (body line of defense)
What are immunogens?
Specific antigen that can induce an immune response
What are antigens?
Any substance that can bind to antibody or T cell receptor (an immune receptor)
What are antibodies?
(Immunoglobulins) Protein made by the immune system in response to an immunogen (antigen)
What is Hapten?
Non-immunogenic antigen; must bind with something else to become an immunogen (too small to trigger its own immune response)
Ex. Penicillin is a hapten
What is an immunoglobulin?
AKA Ig and antibody interchangeably, made by B cells
What is an allergen?
triggers an inappropriate immune response
What is an Antigen determinants (epitotes)?
Specific area of the antigen recognized by a particular antibody
Similarities and differences between Cellular and Humoral Immunity
cellular:
T-cytotoxic cells, activated when their receptors detect cellular antigens presented on MHC I molecules that are foreign
primarily protects against viruses and cancer
humoral: B cells and circulating antibodies are primary cells
B cells become activated to become antibody-producing plasma cells
causes direct inactivation of microorganisms or the activation of the inflammatory mediators
primarily protects against bacteria and viruses
similarity: works together to provide immunity and memory
What are the five classes of immunoglobulins (antibodies)?
IgG, IgM, IgE, IgA, IgD
Role and structure IgG
most protective activity against infections, most active/important in vax response
monomer with 4 isotopes
Role and structure IgM
first antibody production in response to antigen (both fetus and adult) with complement activation on mature and immature B cells
Role and Structure IgE
defense against parasitic infections and hypersensitivity reactions in tissues
monomer
Role and Structure IgA
antibody secretions and mucosa, first line of defense against microorganism infection
monomer dimer
Role and Structure IgD
on mature B cells, no bio effector function known
monomer
What are the four stages of a clinical infection?
Incubation, Prodromal Stage, Invasion Period, an Convalescence
Incubation
Period of initial exposure to the infectious agent and the onset of the first symptoms
Microorganisms have entered a person → undergone initial colonization → begun multiplying (not enough at this stage)
May last from several hours to years
Clinical latency- time between exposure and symptoms
Prodromal Stage
Occurrence of initial symptoms, often mild and include a feeling of discomfort and tiredness
Pathogens continue to multiply
Invasion Period
Pathogen is multiplying rapidly, invading farther and affecting tissues at the site of initial colonization and other areas
Immune and inflammatory responses triggered
Symptoms may be specifically related to the pathogen or to inflammatory response
Convalescence
Individual’s immune and inflammatory systems successfully remove the infectious agent (in most cases) → symptoms decline
Disease may be fatal or enter latency phase with resolution of symptoms until pathogen reactivation at a later time
Infectivity
the ability of an organism to infect the host.
Pathogenicity
Ability of an organism to produce disease.
Depends on infectivity, virulence, toxigenicity, etc.
Virulence
the degree of pathogenicity (disease severity)
Can measure by case fatality, hospitalization, etc
Portal of Entry
How the pathogen enters the body
Ex: Open wound: group A strep or Staph Aureus
Infective Dose
The number of organisms required to cause infection
Ex: 10-100 for Shigella and norovirus
Phases of Pathogenesis of Bacterial Infections
Transmission, colonization, invasion, evasion
Transmission
direct transmission: through direct contact with infections of another individual
indirect transmission: contact, respiratory, airborne, ingestion, vector-borne
Colonization
ability of pathogenic microorganisms to survive and multiply within the human body. Bacteria adhere to tissue and stabilizes without symptoms
Invasion
ability of pathogens to cross surface barriers (skin, mucous membranes), also referred to as penetration. Either invading locally or getting into the bloodstream
Evasion
bacteria evades, replicates, cause disease, Bacteria “hide” via various mechanisms
ex: TB evades killing by hiding in host macrophages
Routes of transmission
Contact, respiratory, airborne, ingestion and vector-borne
Contact (Route of Transmission)
- physical touch
direct (person-to-person)
indirect (contaminated fomites), vertical (mother to infant)
Respiratory (Route of Transmission)
direct large droplet nuclei spread or mucus/saliva
Airborne (Route of Transmission)
- indirect small droplet transmission
human-to-human (spreads through air when someone expels droplets)
environmental (spores inhaled like anthrax)
Ingestion (Route of Transmission)
- through direct oral intake
fecal-oral transmission
ingestion of uncooked food
Vector-Borne (Route of Transmission)
-living organisms transmit illness to others by contact
ticks, mosquitos, fleas, bugs, flies
Endotoxin Mechanism
(lipopolysaccharide) heat-stable antigen of gram-negative cell wall, released during lysis (destruction) of bacteria
-elicits the inflammatory response by activating complement via alternative pathway, and induce fever
Exotoxin Mechanism
enzymes that can damage the plasma membranes of host cells, or by entering cells and changing their function
-mainly produced by gram-positive organisms
-usually protein-based and heat-labile
-often may be neutralized by antibodies or inactivated by enzymes
Capsules Mechanism
-a “slime layer” mostly consisting of simple polysaccharides
-an envelope of loose gel surrounding a bacterial cell
- Keeps the bacterium from being phagocytized by the host’s immune cells
Antigenic Variation Mechanism
the altering of a microorganism’s surface antigens to elude detection by the host’s immune system
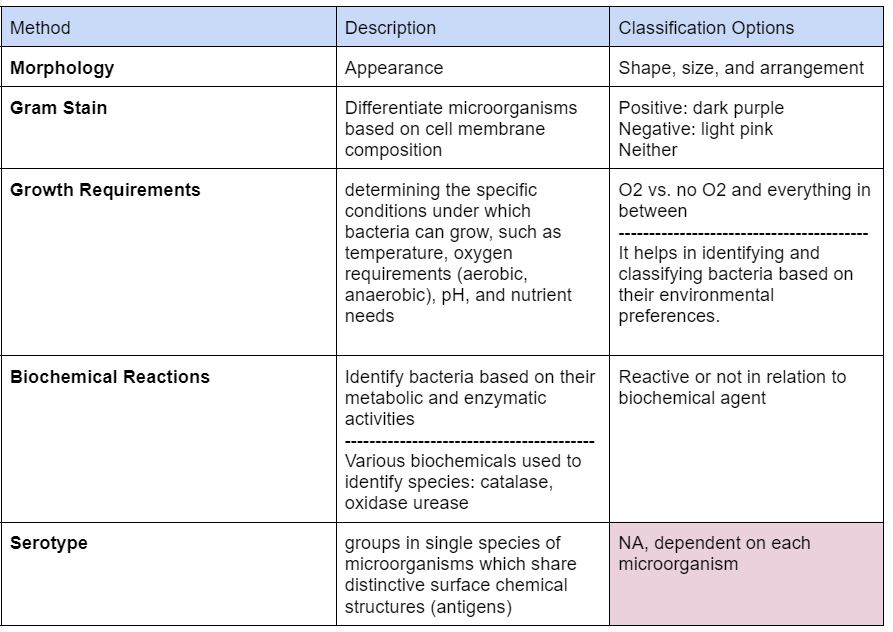
Methods for Classification of Bacteria
Gram Negative Bacteria
thinner cell wall, have outer membrane containing lipopolysaccharides
after last step of counter stain safranin: stains pink
have pilli
ex. E. Coli, Klebsiella, Bacteroides, Brucella
Gram Positive Bacteria
thick peptidoglycan cell wall, no outer lipid membrane
after last step of counter stain safranin: stains blue/purple (retains crystal violet stain)
Bacteria Lacking Cell Walls
instead of rigid cell wall, they have a trilaminar unit membrane
require complex lipid cholesterol in growth medium
Mycoplasma species, ureaplasma species
Acid fast Bacteria
unique cell wall composition: 60% of cell wall comprised of waxy lipid, mycolic acid (making them resistant to ordinary dyes), also made of peptidoglycan & glycolipids
primary stain: carbol fuchsin, binds to mycolic acids in the cell wall
counterstain: methylene blue
non acid-fast: blue
acid-fast: red
ex. mycobacteria, TB
flexible thin walled cells
long, helically coiled, resulting in spiral shaped cells
gram negative, but do not stain well enough for clinical use
T. palladium = syphilis
B. burgdorferi = Lyme disease
Spore-forming Bacteria
produces spores, which are highly resistant, dormant structures
allows bacteria to survive in unfavorable environmental conditions: heat (boiling temp), chemical, radiation resistance, desiccation (dry conditions)
can remain dormant for years until favorable conditions return
has thick layer of peptidoglycan, outer layer that contributes to spore resistance
ex. C. diff, Bacillus anthracis
Obligate Aerobes
require oxygen to survive and multiply
Gather at the top in test (where oxygen concentration is highest)
Facultative Anaerobes
Can toggle between aerobic metabolism if O2 is present, but can switch to anaerobic metabolism if O2 is absent.
Gathers mostly at the top because aerobic respiration generations more ATP, has some at bottom
Obligate Anaerobes
Cannot survive in an oxygen-containing environment
gathered at the bottom in the test (presence of O2 leads to cell death)
Staphylococcus aureus
- gram-positive spherical shape cocci, coagulase positive, creates exotoxin called enterotoxin B, TSST-1
major cause of human infection - sepsis, toxic shock syndrome, food poisoning, cellulitis, skin abscesses, osteomyelitis, endocarditis, pneumonia
MRSA=methicillin-resistant staph aureus
Clostridium difficile
-gram-positive, spore-forming
hospital-acquired infection - diarrhea, pseudomembrane colitis
Escerichia coli
- gram-negative bacteria, gut/urine colonizer, pili is tool of evasion
UTI, bacteremia, sepsis, pneumonia, neonatal meningitis
STEC (shiga toxin-producing E. coli) - dysentery, hemorrhagic colitis, hemolytic uremic syndrome (HUS)
ETEC (enterotoxigenic) - traveler’s diarrhea
Mycobacterium tuberculosis
- weakly gram-positive, acid-positive
TB
Borrelia Burgdorferi
- gram-negative spirochete, non-stainable
Lyme disease, relapsing fever
Normal Flora Means?
AKA the microbiome
assemblage of microbes constituting a microbial community and occupying a specific habitat
protective
varies widely by body site and impacted somewhat by age, sex, diet, nutrition, early development changes, puberty, menopause, etc.
Bacterial Flora in Skin
proptonibacterium
corynebacterium
staph
Bacterial flora in Mouth/ Upper Respiratory Tract
mouth- strep, haemophilus, prevotella, veillonella
anterior nares- propriobacterium, cor
Bacterial flora in gastrointestinal tract and rectum
stool: bacteroides
Bacterial Flora in Genitalia
Vagina: lactobacillus
Bacterial Flora in Eye
Staph epidermidis
Bacterial Flora in Urinary Bladder
urine is normally sterile in young, healthy adults, BUT
asymptomatic bacteriuria is common and expected in elderly, diabetics, & catheterized
Enterococcus
Key Characteristics of Amoeba
Jelly-like cytoplasm
Thin outer plasma membrane
Central granular endoplasm.
----------------------------------------
The endoplasm contains food vacuoles, a granular nucleus, and a clear contractile vacuole.
Food vacuoles are necessary for digestion as there is no mouth/anus.
-----------------------------------------
Make pseudopodia (fake feet) for locomotion
Characteristic of Flagellate
Cell or organism with one or more whip-like appendages called flagella
Characteristic of Ciliate
a coating of cilia on their cell surfaces
----------------------------------------
two types of nuclei within single cells: micronucleus and the macronucleus.
Characteristic of Sporozoa
Single-celled
Parasitic
Non-motile
Spore forming
Helminths
multicellular
complex life cycles
free-living or parasitic
3 subgroups (nematodes, trematodes, cestodes)
Nematodes (roundworms)
various lifecycles
can be transmitted directly person-person
some require soil phase for development
some require egg to mature outside the host
intestinal infections: strongyloidiasis, enterobiasis (pin worm), ascariasis
Trematodes (flukes)
flukes - found in liver, lung, blood
transmission through
eating undercooked fish/crabs (liver flukes)
direct penetration of skin (blood flukes
schistosomiasis
adult flukes in mesenteric or bladder veins
Cestodes (tapeworms)
intestinal infection
attaches to lumen of intestines, feeds off food the host is digesting
ingested through: undercooked pork, beef, fish
Pathogenesis of Toxoplasma gondii (obligatory intracellular parasite)
Pathogenesis: sporozoa
cats shed oocysts in sexual development
ingestion of oocysts, replicates using host system -> release of sporozoites into intestines -> turns into tachyzoites in acute infection
asymptomatic in most people