(4) Skull / (5) Jaws & Teeth / (6) Chewing & Swallowing
1/92
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
93 Terms
How many bones are there in the skull and what regions and what regions can it be divided into?
22 bones in adult cranium
6 bones of middle ear and mandible
Neurocranium is the region of the skull protecting the brain
Viscerocranium is the region that forms the face
Describe the neurocranium
forms the shape of the head
protects the brain
protects the organs controlling the 5 senses
allows neurovascular passage between intracranial and extracranial anatomy
Describe the viscerocranium
forms the shape of the face
forms the cavities of the anterior skull (orbit, oral, and nasal cavities)
protects the delicate structures of the cavities
protects the neurovascular structures of the face
provide surface attachments for the facial muscles
bones here tend to be smaller and more delicate
What are the 2 sets of paired bones in the neurocranium?
The parietal and temporal bones
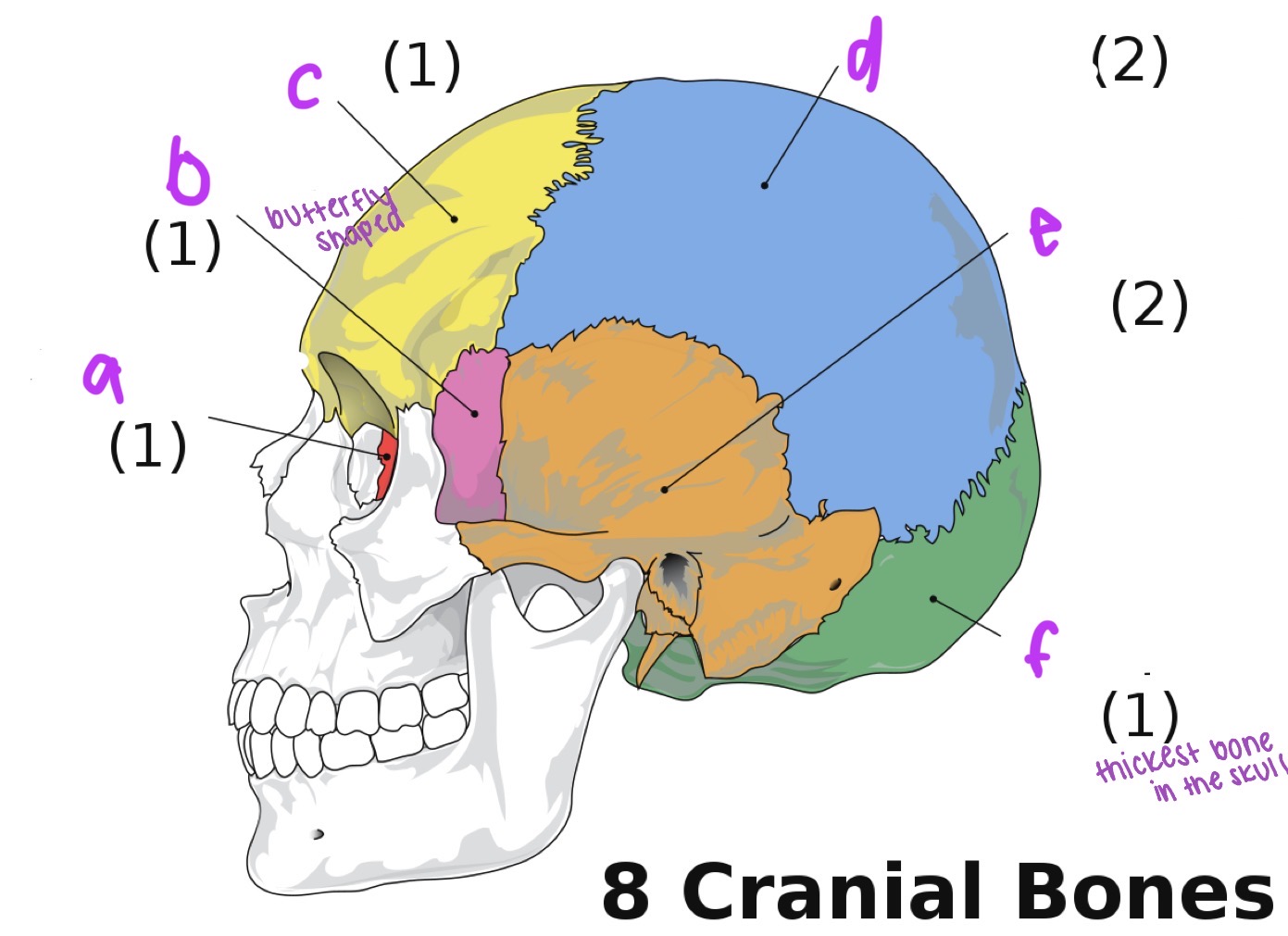
Label the neurocranial bones
a. ethmoid
b. sphenoid
c. frontal
d. parietal
e. temporal
f. occipital
What is the dorsal (top) part of the skull called?
Calvarium
What is the ventral (bottom) part of the skull called?
Cranial base
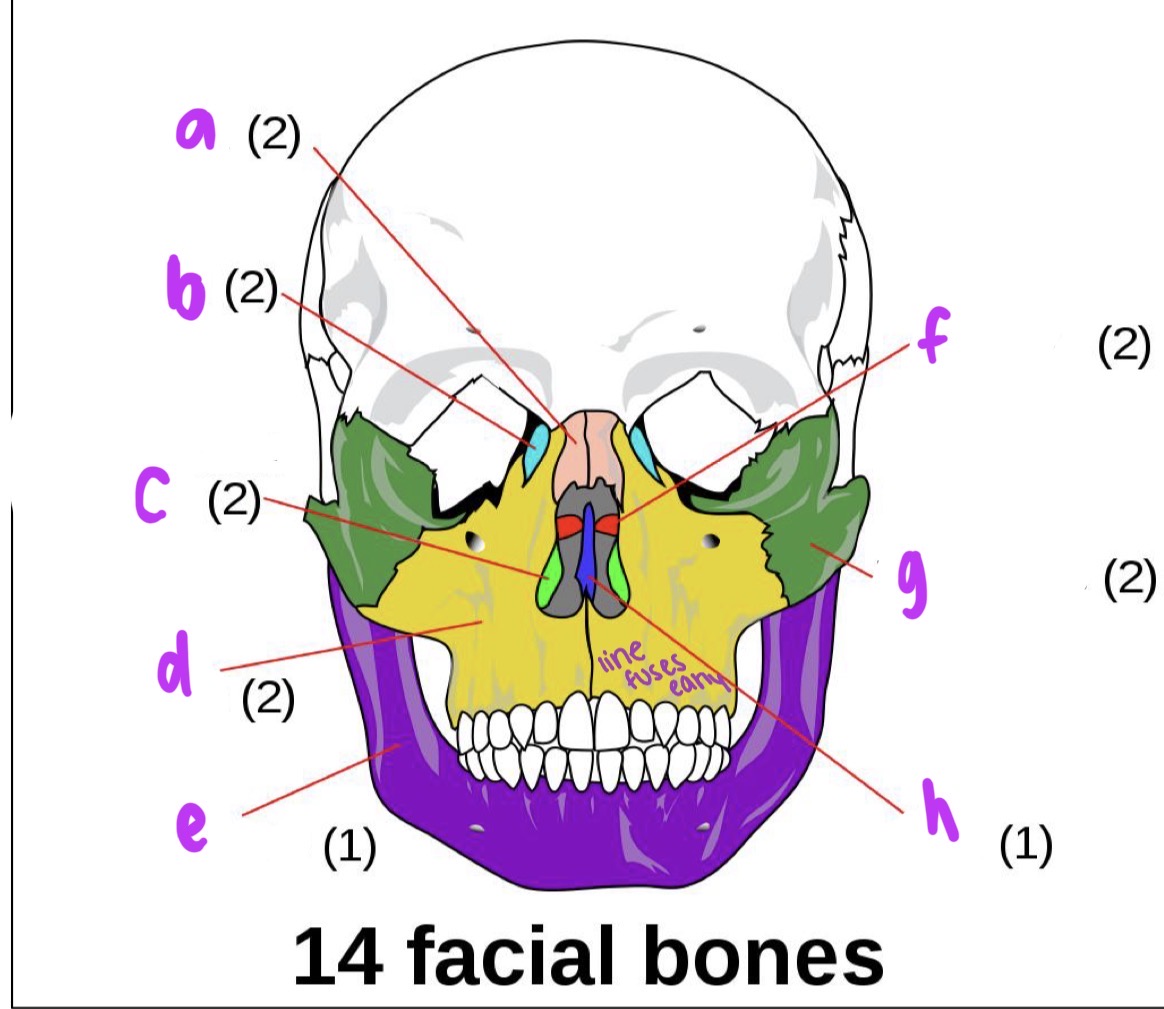
Label facial bones
a. nasal
b. lacrimal
c. inferior nasal concha
d. maxilla
e. mandible
f. palatine
g. zygomatic
h. vomer
At birth how many bones is the skull comprised of?
45
What are cranial sutures?
Bony articulations that exist between bones of the skull
Bones almost connect with each other, separated by fibrous tissue compromised mainly of cartilage
Starts as a series of ossification centers around a fetus brain → allow for rapid growth
Brain growth slows and the ossification centers become sutures which fuse together mostly during adulthood and can be obliterated with age
What are the 4 major cranial sutures and what do they seperate/connect?
Sagittal: middle part, separates 2 parietal bones and joins frontal bone and occipital bone
Coronal: crown, over the top. separates forehead from everything else. connects frontal bone and two parietals
Squamous: “squashed” on the side of the head
Lambdoid: “last”, back of the skull
What is the order of obliteration of cranial sutures, first to last?
Sagittal first, followed by coronal, then lambdoid
What is the metopic suture and metopism?
Metopic suture divides the frontal bone in infants
It fuses between 3 and 9 months and usually obliterated by age 7
Occasionally the suture line remains in adulthood which is known as metopism, this is found in about ~6% of the population
What does fossa mean?
Pit, cavity, depression
Anterior cranial fossa
compromised of the frontal bone, ethmoid bone, and sphenoid bone
accommodates frontal lobe
shallowest of the cranial fossa
has the ethmoid bone
the cribriform plate of the ethmoid bone allows the transmission of the olfactory fibers
Middle cranial fossa
comprised of sphenoid bone and two temporal bones
accommodates the pituitary gland and the temporal lobes
the pituitary gland sits in a depression in the sphenoid bone known as sella turcica
Posterior cranial fossa
comprised of the occipital and two temporal bones
accommodates the brain stem and cerebellum
the deepest of the cranial fossa
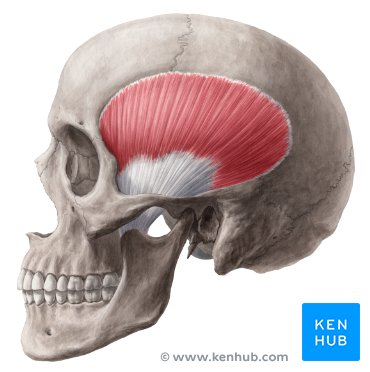
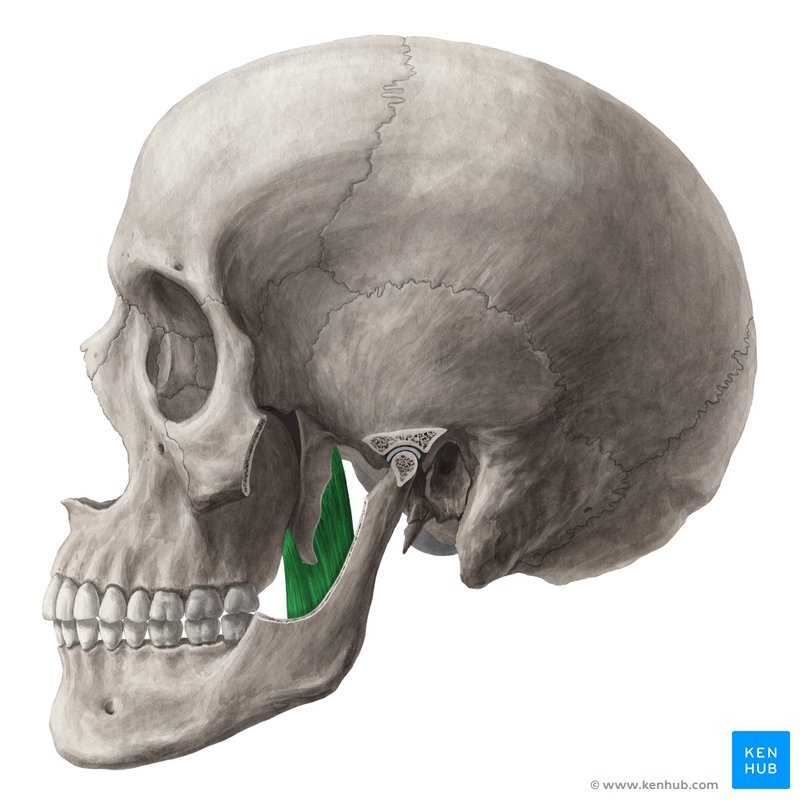
Temporal fossa
a shallow depression on the temporal region of the skull
forms one of the largest landmarks of the skull
comprised of the parietal, temporal, frontal, and sphenoid bones
mainly occupied by the temporalis muscle
Define foramen and fissure and state their role
foramen: an opening, hole, or passage usually through a bone
fissure: a slit like groove
they transmit major nerves and blood vessels
Major foramina
supraoribital foramen: located in the frontal bone, it allows passage of the supraorbital vein, artery, and nerve in orbit
optic foramen: located in sphenoid, it allows the passage of the ophthalmic artery and nerve from the optic canal into the orbit
foramen magnum: located in the occipital bone, it allows the passage of the spinal and vertebral arteries and the spinal cord to pass from the skill into the orbit
foramen magnum: located in the occipital bone, it allows passage of ophthalmic artery and nerve from the optic canal into the orbit
foramina of cribriform plate: located in the ethmoid bone, allows the passage of the olfactory nerve
foramen rotundum: located in the sphenoid bone, it allows the passage of the maxillary nerve
internal acoustic meatus: located in the temporal bone, allows passage of vestibulocochlear and facial nerves
Superior and inferior orbital fissures
Superior:
located in the sphenoid bone, transmits many nerves including the oculomotor and nasociliary nerves, as well as superior ophthalmic vein
Inferior
transmits the zygomatic branch of maxillary nerve, the inferior ophthalmic vein, sympathetic nerves
Non-metric traits of the skull
cannot be measured- either there or not
not considered pathological although their existence may impact upon anatomical function
examples are additional facets, foramina, and facets such as supraorbital notches, zygomaticofacial foramen, and wormian bones
Biparietal thinning of the skull
aka biparietal osteodystrophy
parietals can eventually become so thin that holes appear
incidence increases with age
may be related to osteoperoisis
affects females more
the dipole (spongy inner bone) thins, followed eventually by the cortical (outer) bone
Craniosynostosis
birth defect where bones in a baby’s skull fuse together too early
if this happens before brain is fully developed it ca slow the growth of the brain, compress it
severity is variable but it can result in blindness, seizures, or brain damage
genetic in origin
causes early death but modern day interventions can stop this
Hydrocephaly
excess buildup of CSF in cavities (ventricles) deep within the brain
can cause an increase in the size of the neurocranium (macrocephaly)
viscerocranium usually unaffected
can be present at birth (congenital) or the result of injury/illness
What are some of the most vulnerable parts of the brain?
the middle cranial fossa is the most vulnerable part of the skull as the bones are thin and there are multiple foramina → more likely to die from these injured
the oribital roof and nasal bones are also vulnerable → risk of infection entering brain
Describe the upper jaw
part of the viscero-craniumn
known as the maxilla
comprised of 2 bones
together with the 2 palatine bones, forms the hard palate
holds and supports the upper teeth
helps shape middle of the face
shapes the floor of nasal cavity, allowing normal airflow
Describe the mandible
part of viscero-cranium
single u-shaped bone
largest bone in skull
insertion point for many of the muscles involved with facial expression
holds and supports the lower teeth
shapes and contours lower 3rd of the face
holds tongue
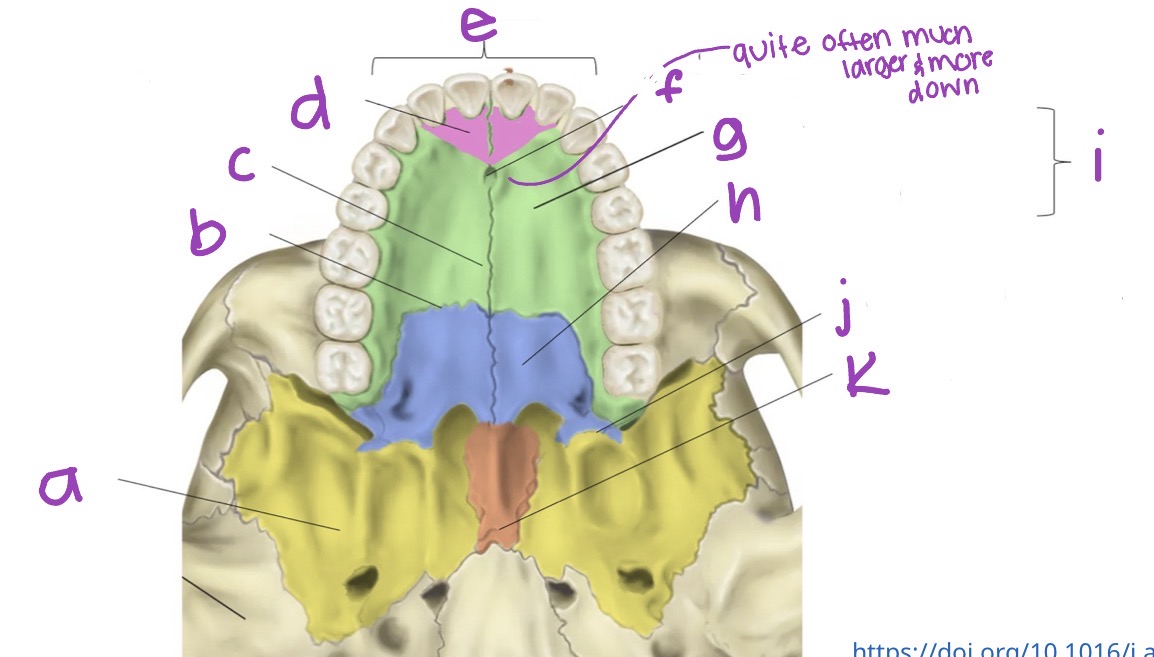
Label hard palate
a. sphenoid bone
b. transverse palatine suture
c. median palatine suture
d. primary hard palate
e. alveolus
f. incisive fossa
g. palatine process of maxilla
h. palatine bone
i. secondary hard palate
j. pyramidal process of palatine bones
k. vomer bone
What does the primary palate of the jaw refer to
lips
nasal sill
alveolus
hard palate anterior to the incisive foramen
What does the secondary palate of the jaw refer to
hard palate posterior to the incisive foramen and soft palate
What is the incisive fossa (aka incisive foramen) ?
Opening for the 2 incisive canals that run either side of the maxilla. They connect the hard palate to the nasal cavity. Carriers branches of the nasopalatine nerve and the terminal ends of the greater palatine vessels
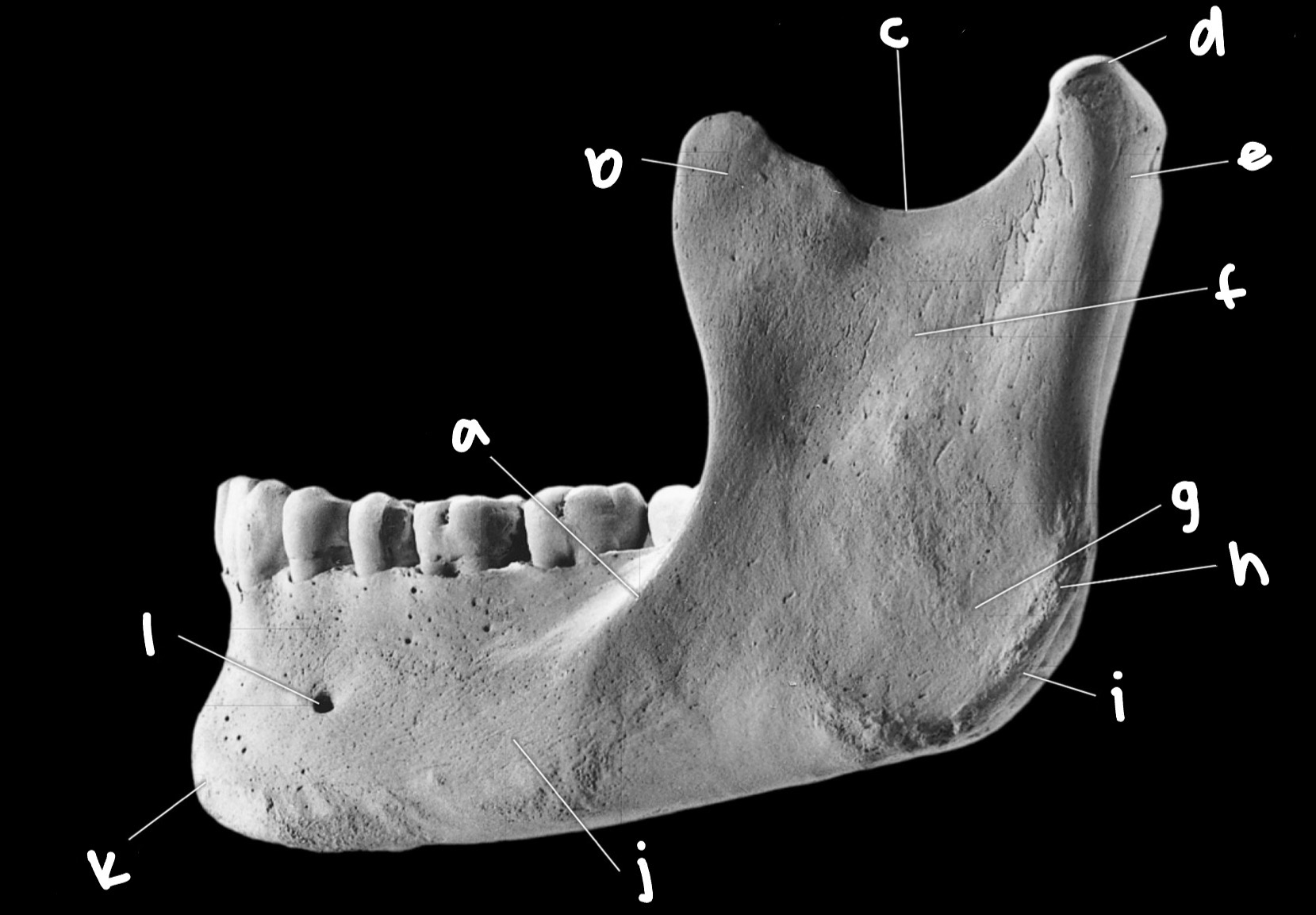
Mandibular features slide 8
a. oblique line
b. coronoid process
c. mandibular notch
d. mandibular condyle
e. condylar neck
f. ramus
g. masseteric fossa
h. masseteric tuberosity
i. gonial angle
j. body
k. mental protuberance
l. mental foramen
Mental foramen
Part of mandibular canal. Carries the inferior alveolar nerve and the mental vessels. These enter through the mandibular foramen on the medial aspect of the mandible
Masseteric fossa and tuberosity
Attachment points for the masseter muscle
Gonial angle and mental protuberance
Important for facial symmetry
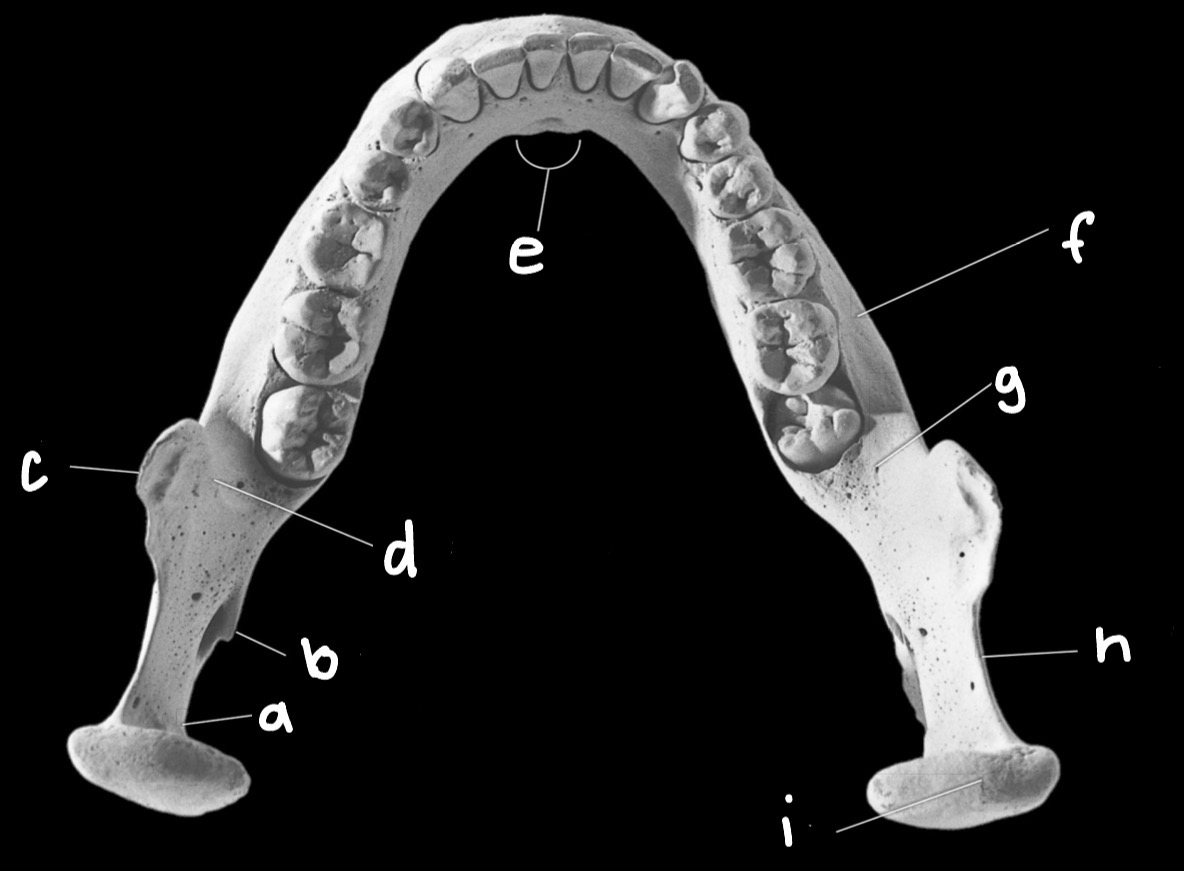
Label Mandibular features
a. condylar neck
b. lingula
c. coronoid process
d. endocoronoid ridge
e. mental spines
f. body
g. extramolar sulcus
h. mandibular notch
i. mandibular condyle
Mental spines
attachments for the intrinsic tongue muscles
Mandibular notch
allows for the passage of the masseteric nerves and vessels
Mandibular condyle
vital to functioning of TMJ
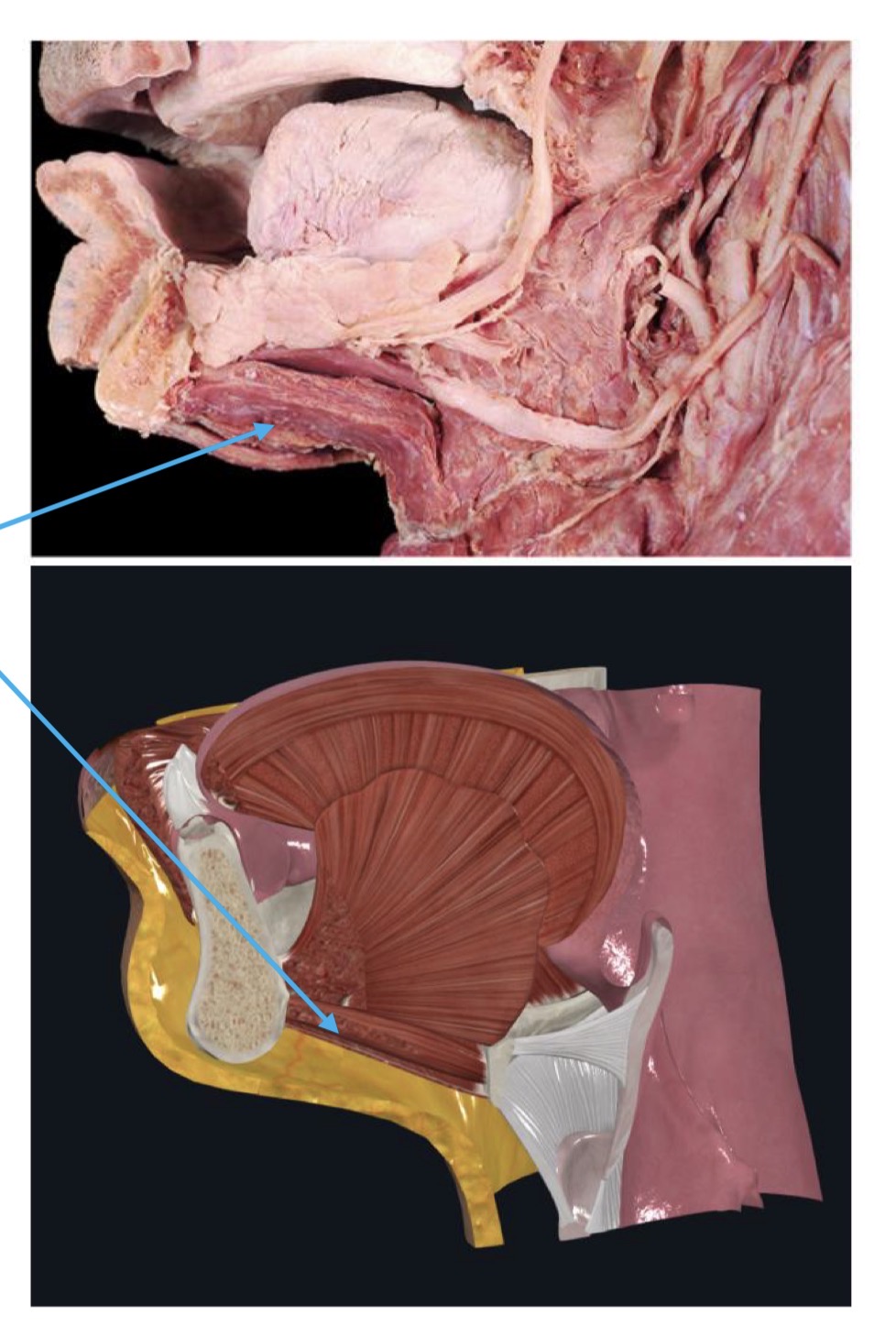
Temporomandibular joint (TMJ)
consists of articulations between 3 surfaces: head of mandible (mandibular condyle) and the articular tubercle and the mandibular fossa in the temporal bone
unique mechanism as surfaces never actually touch each other, being separated by a disc
movement:
produced by muscles of mastication, and hyoid muscles
allow for protrusion and retraction, elevation and depression
What features of the mandible are s*xually dimorphic?
The gonial angle, projection of the mental protuberance, and the extent of the gonial eversion
Anatomical functions of the teeth
Digestion (chewing, swallowing)
only part of the skeleton that interacts directly with the environment
they seize and masticate (chew) food
incisors bite food into smaller pieces
canines grasp food and tear it off
premolars and molars chop/crush these pieces further before swallowing
breaking down food into smaller bolus is important for digestion
Speech
make words by controlling airflow out of the mouth
(th → tongue brushes against upper row of teeth)
(f / v → pressing lower lip to upper teeth)
Facial structure
help maintain natural alignment of jawbone and facial muscles
Dentition of teeth
formed deep within jaw
erupt through gum tissue once nearly complete
do not change with age
shape of tooth is only altered by attrition, breakage, cultural mods, or demineralization
enamel is outer layer of tooth and the hardest tissue in the human body
Adult teeth classifications
8 incisors (thin cutting edges)
4 canines (single prominent cones)
8 premolars (bicuspids)
12 molars (tricuspid or more)
32 total
Deciduous (children) teeth classifications
8 incisors
4 canines
8 molars
20 in total
Dental eruption
3rd molars usually erupt ~17-25 years
lower M3s usually erupt slightly earlier
eruption often begins earlier in females
by ~ age 25 you cannot use dental eruption to age a skeleton
Malocclusion and its 2 most severe forms
misalignment of the teeth
difference between size of upper and lower jaw or between jaw and tooth size
usually inherited but can be from trauma, tumors, poor dental habits, childhood habits
most severe forms:
retrognathism (overbite) → used to be called prognasis
prognathism (underbite)
Cleft palate
developmental defect in hard palate
caused by arrested development of the maxilla during embryogenesis
results in communication between oral and nasal cavities
can cause hearing problems (bc of infections), issues with dental development, and speech problems
causes unclear
Mandibular tori
Bony growths on the lingual surface of the mandible , also known as protrusion or a hyperostosis
Torus palatinus
bony growth midline on the hard palate
Non-metric dental traits (NMDTs)
carabelli’s cusps
shove-shaped teeth
peg-shaped teeth
additional grooves, ridges, and roots
supernumerary teeth
congenital absence of teeth
Plaque and caries
plaque
soft, thin film of bacteria, mucin, dead epithelial cells, and food debris that develops on tooth surface
eventually soft plaque mineralizes to become calculus (hard plaque or tartar)
caries
caused by acids produced by bacteria in plaque. damages the enamel of the tooth eventually causing a pit of cavity
if left caries can lead to pain, infection, and tooth loss
Periodntal disease
gum disease
causes inflammation of tissues surrounding the teeth
bacteria break down the tissues surrounding the teeth faster than the body can replace them
in advanced stages can lead to abscesses and tooth loss
Dental abscesses
caused by a buildup of pus in the gum or tooth
can spread to the surrounding bone and to other areas of the body through the blood stream
if untreated can lead to sepsis
Causes of dental wear
erosion
acids from foods
stomach acid
attrition
tooth to tooth contact
abrasion
over brushing, eating coarse foods
occupational habits
holding items in teeth
environmental dust
What are the primary bones involved in mastication (chewing)?
maxilla - fixed
mandible - movable
temporal bones - enabled movement
What is the temporomandibular joint?
modified hinge joint that connects the jawbone to the skull, allowing for movement during chewing and speaking
modified hinge synovial joint
fibrous capsule and ligament
articular cartilage and disc
What are the anatomical boundaries of the temporomandibular joint and what movements does it permit?
anatomical boundaries
mandibular fossa
articular tubercle of the temporal bone
mandibular head
permits movement in multiple planes
elevation - close mouth
depression - open mouth
protrusion - forward movement
retraction - backward movement
lateral movement - side to side
What innervates the muscles of mastication?
Mandibular division of the trigeminal nerve (CN V3)
Muscles of Mastication: Origin, Insertion, & Action of Temporalis
Origin: temporal fossa floor
insertion: tip and medial surface of coronoid process
action: elevates and retrudes jaw
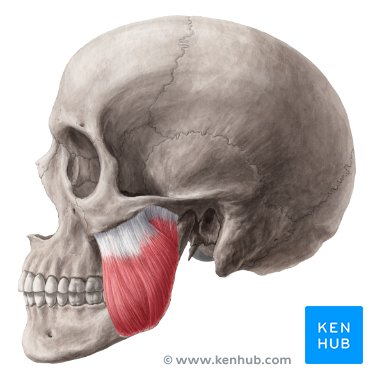
Muscles of Mastication: Origin, Insertion, & Action of Masseter
origin: maxillary process of zygomatic bone and zygomatic arch
insertion: angle and lateral ramus of mandible
action: elevates jaw (+ superior fibers protrude)
Muscles of Mastication: Origin, Insertion, & Action of Lateral Pterygoid
origin: infratemporal surface/crest of sphenoid and lateral surface of lateral pterygoid plate
insertion: joint capsule, articular disc, neck of condyloid process of mandible
action: acting bilaterally, protrudes and depresses chin. acting unilaterally, swings contralaterally
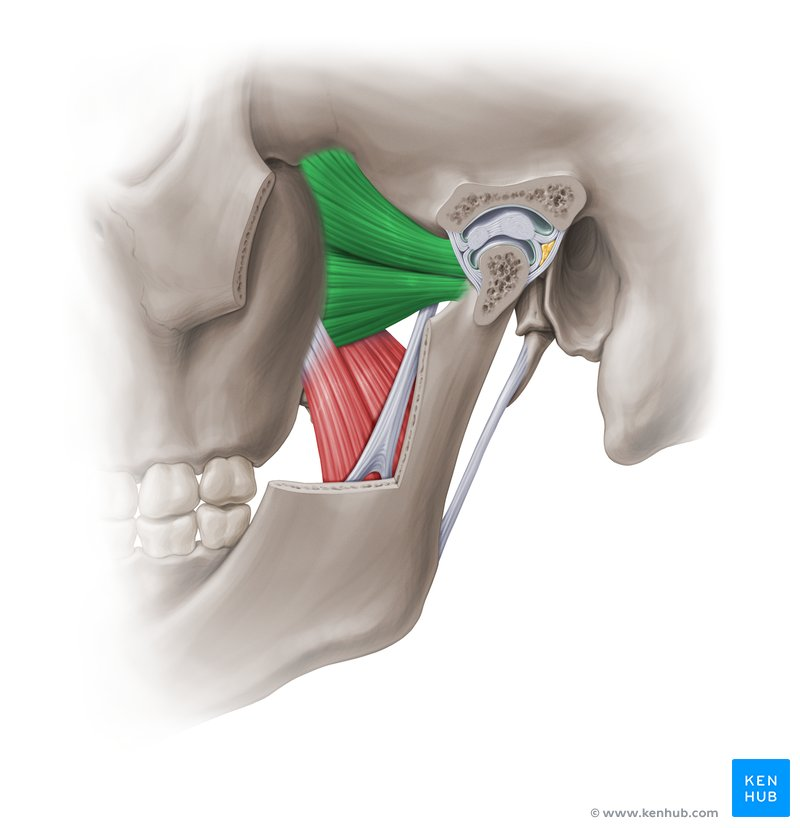
Muscles of Mastication: Origin, Insertion, & Action of Medial Pterygoid
origin: medial surface of lateral pterygoid plate, pyramidal process of palatine bone, tuberosity of maxilla
insertion: medial surface of ramus of mandible
action: elevates jaw with masseter contributes to protrusion and small lateral movements when working unilaterally
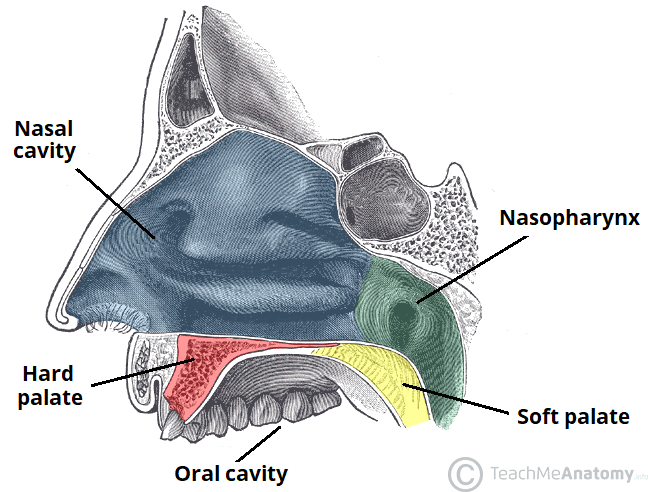
Describe the oral cavity
start of the digestive tract
extends from the oral fissure to the pharynx
anatomical boundaries
roof - hard and soft palates
walls - cheeks and lips
floor - muscle
lined with stratified squamous epithelium
contains teeth, tongue (fills most of the cavity), gingivae, palate and tonsils
Oral cavity floor
mylohyoid muscle
covered with non- keratinized stratified squamous epithelium
innervated by the mandibular division of the trigeminal nerve (CN V3)
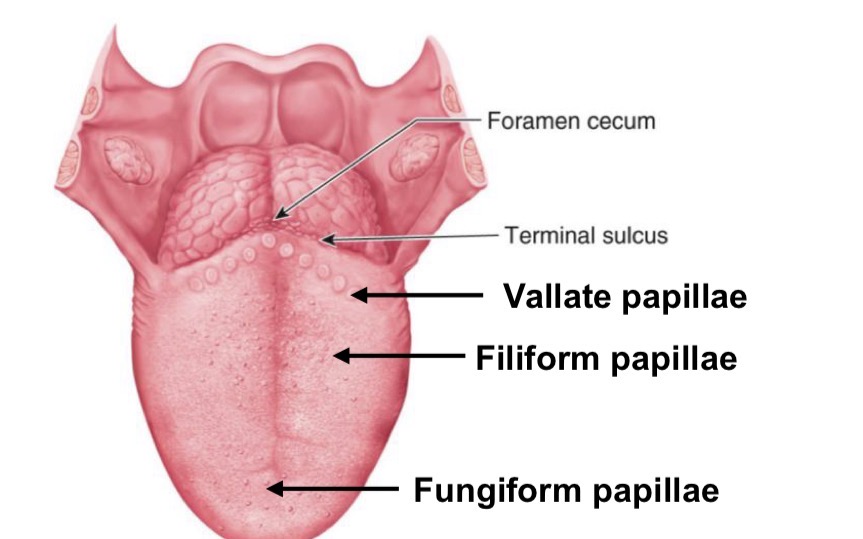
Dorsal surface of the tongue
rough with dull appearance
para-keratinized stratified squamous epithelium
anterior part in oral cavity
posterior part in oropharynx
lingual tonsils underly the epithelium of the posterior third (lymphoid tissue)
insert imagef from slide 10
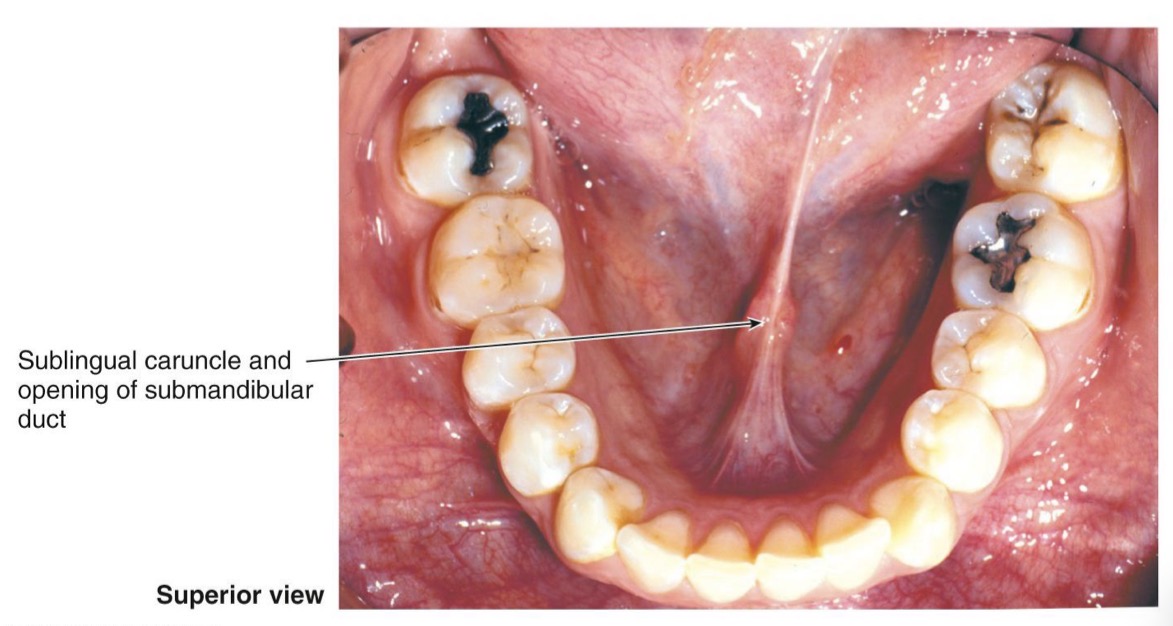
Ventral surface of tongue
smooth and shiny appearance
non-keratinized stratified squamous epithelium
sublingual caruncle and opening of submandibular duct
insert image from slide 10
Muscles of the tongue: Intrinsic vs Extrinsic
Intrinsic: alter tongue shape
originate and insert within the tongue
superior and inferior longitudinal fibers
transverse fibers
vertical fibers
extrinsic: alter tongue position
originate outside the tongue but insert within the tongue
Muscles of the Tongue: Origin, Insertion, & Action of Genioglossus
origin: genial tubercle of mandible
insertion: tip and body of tongue
action: depresses center of tongue, protrudes tongue, deviates tongue
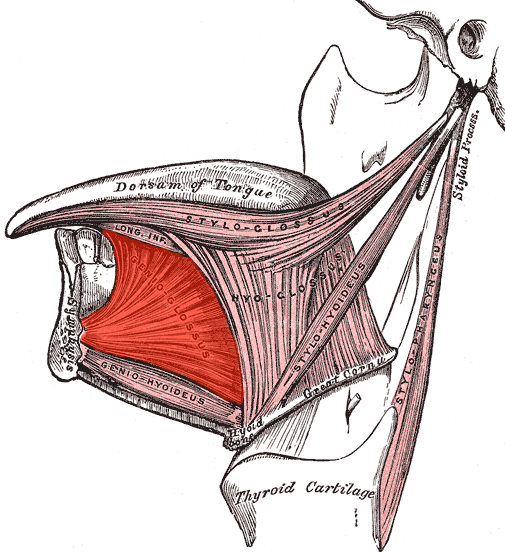
Muscles of the Tongue: Origin, Insertion, & Action of Hyoglossus
origin: hyoid bone
insertion: inferolateral aspect of tongue
action: depresses and retrudes tongue
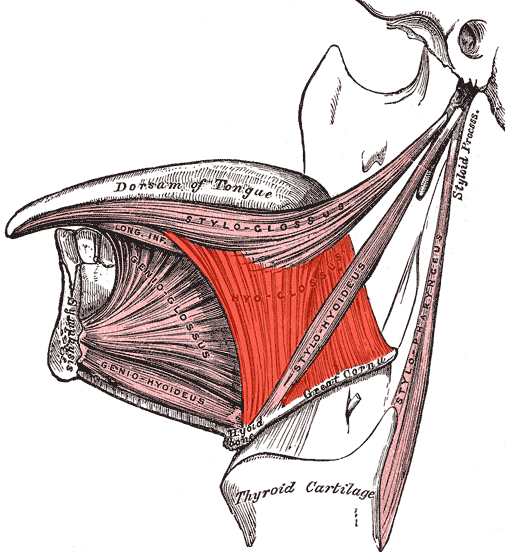
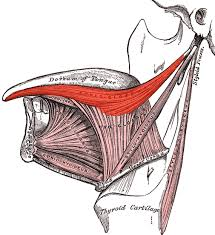
Muscles of the Tongue: Origin, Insertion, & Action of Styloglossus
origin: styloid process of temporal bone
insertion: posterolateral aspect of tongue
action: retrudes tongue and curls sides
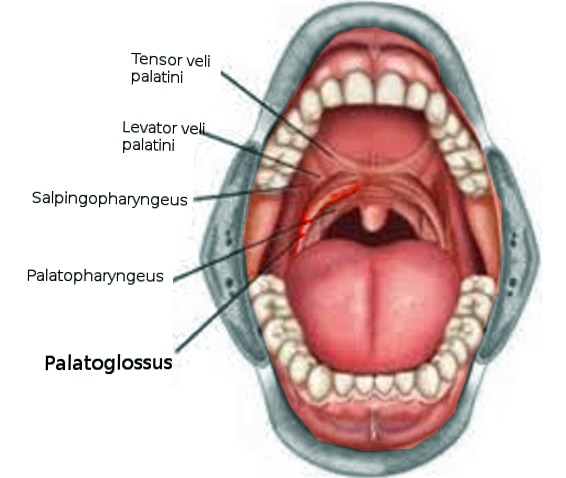
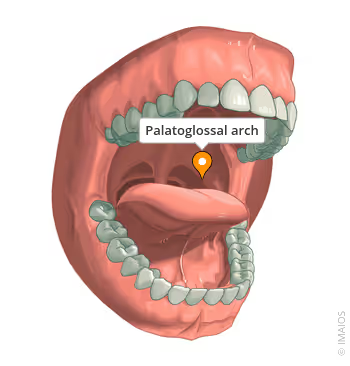
Muscles of the Tongue: Origin, Insertion, & Action of Palatoglossus
origin: palatine aponeurosis
insertion: posterolateral aspect of tongue
action: elevates back of tongue/ depresses soft palate
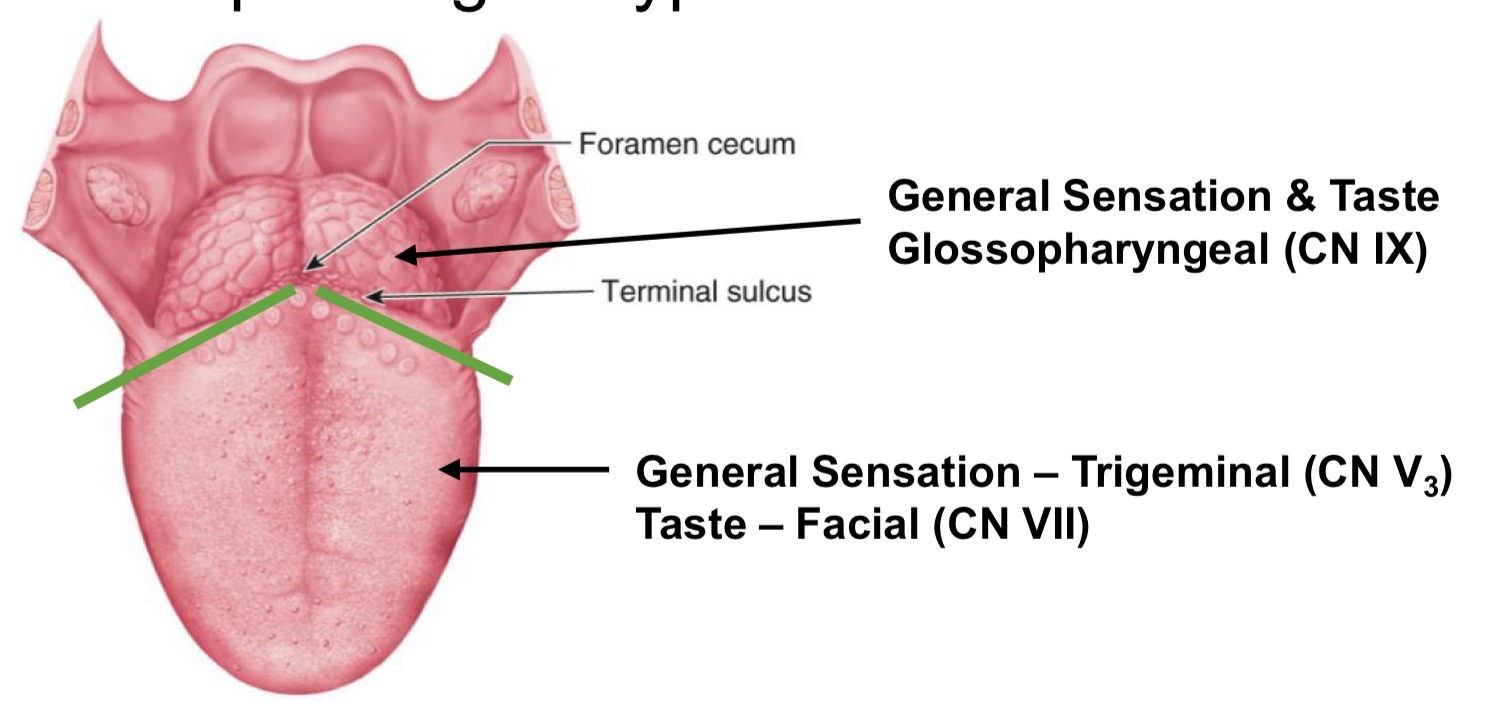
Neurovasculature of the tongue
motor
hypoglossal (CN XII) for most
palatoglossus innervated by Pharyngeal plexus (CN X)
arterial supply
lingual branch of external carotid artery
sensory
differs depending on type and location (insert pic from slide 12)
venous drainage
lingual vein > internal jugular vein
Salivary glands function
produce saliva which drains into oral cavity
serous fluid that washes oral cavity
mucin for lubrication
amylase for carbohydrate digestion
lysozyme as an antibacterial
immunoglobin A for defense
high pH to reduce acidity and prevent tooth decay
Salivary gland’s accessory organs
parotid x 2
sublingual x 2
submandibular x 2
and more minor glands: labial, buccal, palatal, lingual
Parotid gland
largest
posterior to mandible
duct opens opposite second molar
facial nerve and vessels pass through it
serous saliva
parasympathetic innervation- glossopharyngeal (IX)
Submandibular gland
wraps around mylohyoid
duct opens at the sublingual papilla
serous and mucosal saliva (3:2)
parasympathetic innervation - Facial (VII)
Sublingual gland
located in the floor of the mouth (sublingual fold)
multiple ducts open into the sublingual fold
serous and mucosal saliva (1:3)
parasympathetic innervation - Facial (VII)
Oral cavity roof - anterior hard palate
Bony skeleton
palatine processes of the maxillae
horizontal processes of palatine bones
mucosa
oral surface - keratinized stratified squamous epithelium
nasal surface - respiratory epithelium
underlying lamina propria - contains blood vessels and nerves
transverse palatine folds *rugae)
assist with manipulation of food during mastication
sensory innervation
maxillary division of the trigeminal nerve (CN V2)
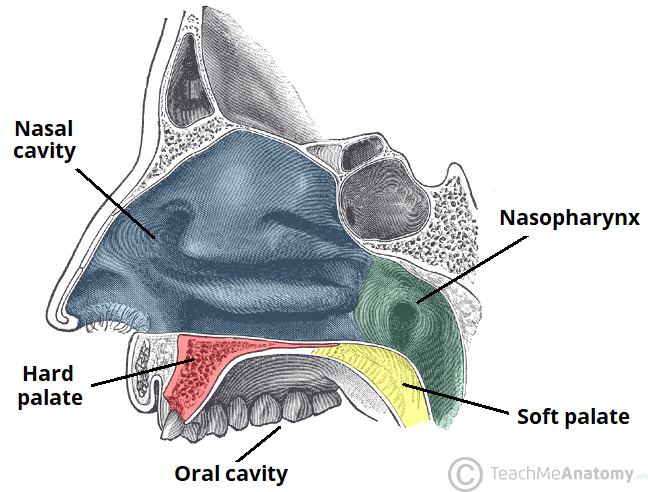
Oral cavity roof - posterior soft palate
suspended from hard palate and ends at the uvula
mucosa
non-keratinized stratified squamous epithelium
underlying lamina propria - contains blood vessels and nerves
Muscles of the soft palate and why they are important
levator veli palatini, tensor veli palatini, palatoglossus, palatopharyngeus
most are innervated by pharyngeal plexus (CN X) for most, mandibular division of the trigeminal nerve (CN V3) for the tensor veli palatini
prevents food bolus from entering nasal cavity
prevents food bolus from re-entering oral cavity
protects the airway when swallowing
allow expansion during swallowing
regulates air entering the nose during phonation
facilitate movement of air through pharynx
Pharynx
the oropharyngeal isthmus connects the oral cavity and pharynx
anatomical boundaries:
superior - soft palate
inferior - posterior 3rd of the tongue
lateral - palatoglossal arch
pharynx is a musculomembranous tube
extends from the base of the skull to the esophagus
anterior openings - nose, mouth, larynx
3 divisions
Nasopharynx
extends from the nasal choanae to the tip of the soft palate
contains the ostium of the auditory (eustachian) tube
additional tonsils
mucosa
lined by pseudostratified ciliated columnar epithelium
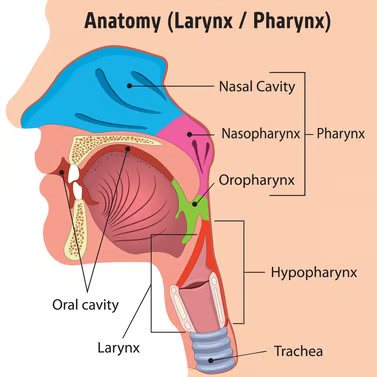
Oropharynx
extends from tip of the soft palate to the superior aspect of epiglottis
extends anteriorly from the oropharyngeal isthmus
contains folds and tonsils
mucosa
lined by non-keratinized stratified squamous epithelium
Laryngopharynx
extends from epiglottis to the esophagus
laryngeal inlet located anteriorly and bounded by epiglottis
posterior 1/3 of tongue runs vertically in the anterior wall
mucosa
lined by non-keratinized stratified squamous epithelium
Muscles of the pharynx
constrictor muscles
3 pairs of overlapping muscles
contract sequentially to push food bolus into esophagus
all innervated by pharyngeal plexus (CN X)
longitudinal muscles
shorten and widen pharynx
elevate pharynx and larynx
open the auditory tube
Esophagus
muscular tube which extends from laryngopharynx to the stomach (C6-T10)
passes through
neck, thorax, and abdomen
diaphragm at esophageal hiatus (T10)
lower esophageal sphincter prevents reflux
smooth muscle innervated by the autonomic nervous system
upper portion continuous with inferior constructor
lower portion continuous with muscle of stomach
Histology of Esophagus
Mucosa
non-keratinized stratified squamous epithelium
lamina propria
muscularis mucosa- longitudinally arranged fibers
Submucosa
contains mucous glands, blood vessels, lymphatics & nerves
Muscularis externa
inner circular fibers
outer longitudinal
Adventitia
the esophagus is extraperitoneal therefore it is covered with an adventitia
Neurovasculature and Lymphatics of upper 3rd trunk/head
supplied by inferior thyroid artery from subclavian artery
drains into inferior thyroid vein then brachiocephalic vein
lymph drains into deep cervical nodes
Neurovasculature and Lymphatics of middle 3rd trunk/head
supplied by descending aorta
drains into azygos veins then superior vena cava
lymph drains into superior and posterior mediastinal nodes
Neurovasculature and Lymphatics of lower 3rd trunk/head
supplied by celiac trunk from left gastric artery
drains into left gastric veins then portal system
lymph drains into celiac nodes
Innervation of trunk/head
Parasympathetic - vagus nerve (CN X)
Sympathetic - sympathetic trunks/ chains