ch20-Fluid and Electrolyte Balance
1/66
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
67 Terms
what does fluid balance depend on?
blood pressure
where is first quick neural response?
in medulla, slower hormonal response via the kidneys;
what senses behavioral responses?
osmoreceptors
what does cardiovascular system integrate with?
integrates with the kidneys to return homeostasis
what do kidneys do?
conserve volume
how is water balanced?
kidney medulla creates concentrated urine
what is osmolarity determined by?
•the kidneys in order to maintain homeostasis.
how do nephrons control osmosis?
Varying osmolarity in the kidney
Varying permeability to water and solutes
what does osmolarity happen through?
through the nephron; as isosmotic filtrate go down into the concentrated medulla, water is reabsorbed into the kidney interstitial.
s1 of osmolarity?
Fluid becomes more concentrated in the descending limb.
s2 of osmolarity?
Reabsorption of solute; In the thick ascending loop of henle, water can not leave the tubule, no aquaporins, only solutes. As the nephron moves towards the cortex, the osmolarity decreases. Therefore to equalize, solute leave the tubule; the solution becomes hyposmotic.
s3 of osmolarity?
Permeability to water and solutes is regulated by hormones; At this point, a lot of the water and solutes have left.
Now permeability to water and solutes is under, in part, hormonal control.
what is released by pituitary?
Vasopressin, released by the pituitary in response to stretch and osmolarity sensors, adds aquaporins
s4 of osmolarity?
Urine osmolarity depends on reabsorption in the collecting duct.
what does vasopressin increase?
aquaporins
what happens at maximal vasopressin?
collecting duct is permeable to water
Without vasopressin, will the urine be dilute? will water reabsorb?
yes; no
what does vasopressin bind to?
vasopressin, binds to receptors on the nephron epithelium causing aquaporins to be added to epithelium and water to freely pass through it to the capillary.
what controls permeability?
Vasopressin controls permeability in the distal tubule collecting duct.
What stimuli controls vasopressin secretion?
Plasma osmolarity (most potent)
Blood volume
Blood pressure
what do osmoreceptiors sense?
osmolarity
what are stretch sensitive?
osmoreceptors are stretch-sensitive receptors in the hypothalamus
what do baroreceptors do?
Baroreceptors in atria, aorta and carotid sense pressure
how do osmoreceptors work?
osmoreceptors are stretch-sensitive linked to actin (ECM), when cell shrinks due to a concentrated fluid, the receptors get pulled and open cation channels, leading to cell depolarization – increased firing – vasopressin release
s1 of vasopressin release?
AVP is made and packaged in cell body of neuron.
s2 of vasopressin release?
Vesicles are transported down the cell.
s3 of vasopressin release?
Vesicles containing AVP are stored in posterior pituitary
s4 of vasopressin release?
AVP is released into blood.
what triggers vasopressin?
Activated sensory neurons trigger vasopressin (AVP) release
In adults, vasopressin is also released according to our circadian rhythm, with increase secretion during the night. Why would this be beneficial?
More water reabsorption from the nephron
How would the plasma vasopressin vs. plasma osmolarity plot look:
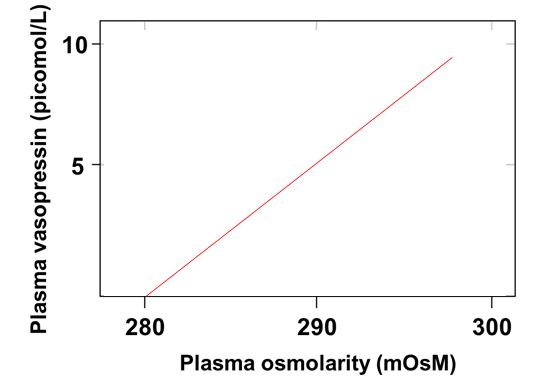
As osmolarity increases, vasopressin is released into the blood, in attempt to increase the water content of the blood and bring down the osmolarity to normal (280).
What maintains creates the concentration gradient in the medulla?
The close anatomical association with the capillary.
What creates the concentration gradient in the medulla?
the loop of Henle and urea recycling
Why doesn’t the osmolarity reduce when water leaves the nephron on the descending loop of Henle?
Water only leaves in the decending part. In the acending limb, the tubule is impermeable to water while actively transporting ions out of the tubule, causing the osmolarity of the capillary to increase.
Ascending loop of Henle?
Not permeable to water, concentrated filtrate; Active transport of ions creates dilute filtrate
how does it ascending loop of henle work?
NKCC symporter uses energy stored in sodium gradient to transport K, and 2 Cl from the lumen to epithelial cell.
Na-K-ATPase removes Na from cells on basolateral side, while K and Cl leave by cotransporters or channels.
s1 of ah?
1200 mOsm entering ascending loop of Henle
s2 of ah?
Salt reabsorption
s of ah?
Water cannot follow solute.
s4 of ah?
100 mOsM leaving the loop
what is normal plasma sodium?
Normal plasma sodium is 135-145 mOsm
what is potassium balance?
K+ falls below 3 meq/L or above 6 meq/L excitable tissues of the muscle and nerve begin to show altered function.
what is hypokalemia?
(low K+) – muscle weakness, difficult to depolarize
what is hyperkalemia?
more dangerous, depolarization makes excitable tissues more excitable, cells are then unable to repolarize fully. Can lead to life threating arrhythmias
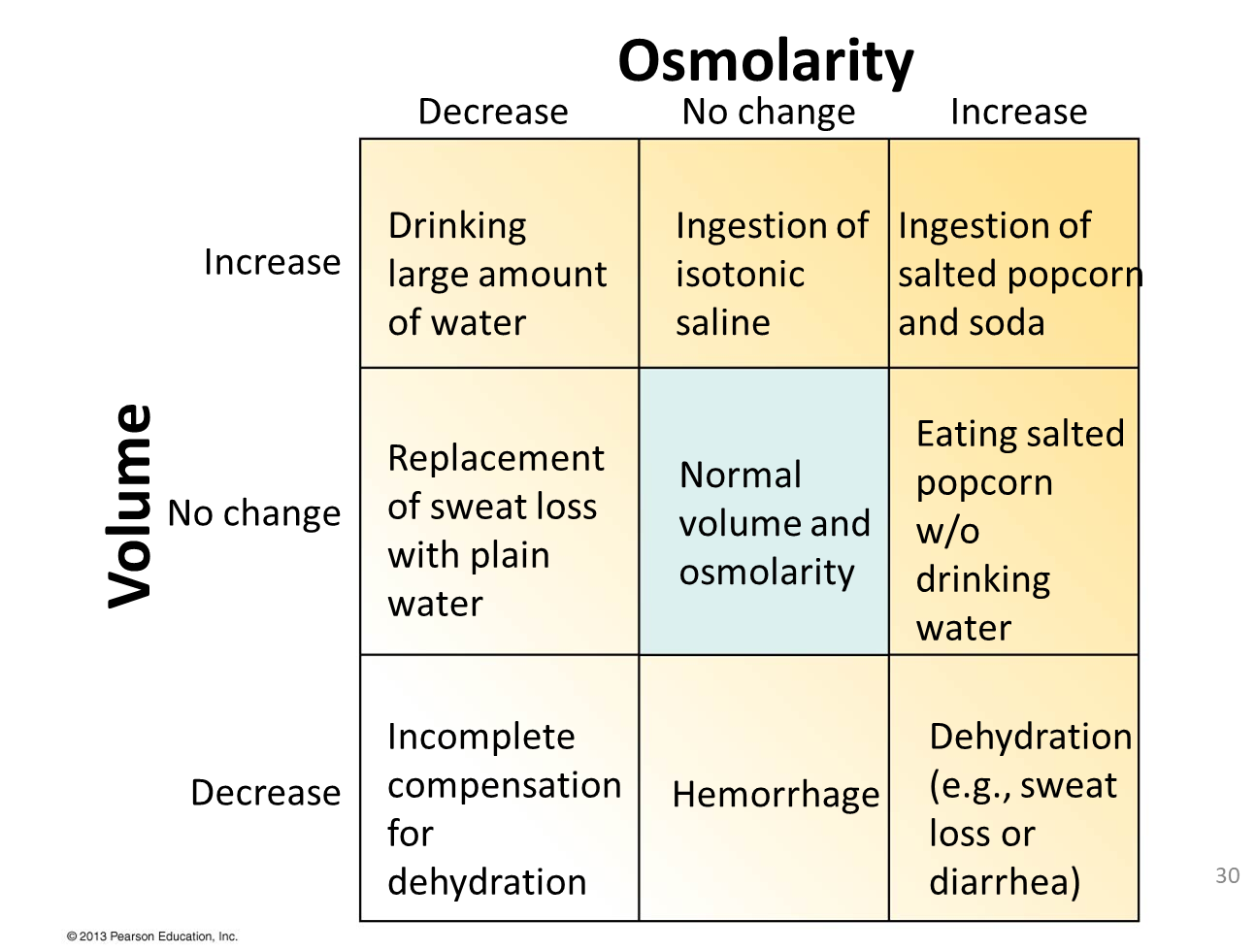
What would be the kidneys response to these disturbances in volume and osmolarity?
what are causes of dehydration?
Prolonged exercise
Water loss from lungs may double, sweat can increase from 0.1 L to up to 5 L
Sweat is hyposmotic (fluid left behind becomes hyperosmotic)
Diarrhea
Decreases blood volume, if severe can reduce blood pumped to brain
Water loss can lead to cell shrinkage and disruption in function
what are goals of dehydration?
conserve fluid
Increase BP
Increase volume and reduce osmolarity (thirst)
how is dehydration controlled?
Carotid and aortic baroreceptors signal the medulla: cardiovascular control center, sympthatic response increases.
Increasing HR, CO, constricting arterioles
what does dehydration do?
Dehydrations increases the omolarity. Vassopressin increases water reabsorption. Thirst (mechanisms still unknown)
what does decrease in BP do?
Decrease in BP decreases flow, decreasing GFR
Lower flow against the macula densa triggers paracrine response and renin release.
what does renin do?
Renin converts inactive plasma protein angiotensinogen to ANGI, than angiotensin converting enzyme (ACE) on the endothelium of blood vessels converts ANG1 to ANG2.
what restores homeostasis?
All together restore homeostasis
what is CNS depression?
patients go into coma, or respiratory centers can cease to function
what is Aljalosis?
sustained contractions, paralyze respiratory muscles
what are pH disturbances?
Associated with K+ disturbances (H+-K+-ATPase antiporter)
what does acidosis do?
Acidosis: excrete H+ conserve K+
what does alkalosis do?
Alkalosis: excrete K+ conserve H
normal ph of plasma?
Normal pH of plasma is 7.38–7.42
Urine is 4.5 – 8.5
what is closely regulated?
H+ concentration is closely regulated
Changes can alter three-dimensional structure of proteins (effecting hydrogen bonds)
Normal plasma is 0.00004 meq/L (compared to Na+ which is 135 meq/L)
what do buffers do?
Moderate changes in pH
Combine with or release H+
Cellular proteins, phosphate ions, hemoglobin, bicarbonate
what does ventilation do?
Rapid response
Corrects 75% of disturbances; can also cause them
what is renal regulation?
Receptor-mediated endocytosis
Directly by excreting or reabsorbing H+
Indirectly by changing in the rate at which HCO3– buffer is reabsorbed or excreted
what is respiratory acidosis?
CO2 increases, the reaction shifts to the right, creating on additional H+ and one HCO3-
Asthma, chronic obstructive pulmonary disease, fibrosis
what is respiratory alalosis?
CO2 decreases; Less common. Excessive ventilation – anxiety attack, breath into bag
ph homeostasis with ventilation?
Hb buffers free hydrogen ions.
Ventilation can compensate for pH disturbances
what is metabolic acidosis?
H+ increases, the reaction shifts to the left, creating on additional CO2 and H2O
Lactic acid from anaerobic metabolism, excessive breakdown of fats, low-carb diet
what is metabolic alkalosis?
H+ decreases; excessive vomiting, taking antacids