Drugs Acting on ANS
1/43
Earn XP
Description and Tags
Drugs acting on ANS Part I
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
44 Terms
What are the three main divisions under ANS?
enteric, parasympathetic, sympathetic
How does a preganglionic neuron differ from a postganglionic neuron?
Preganglionic neuron: The cell body is located within the CNS. These neurons emerge from the brainstem or spinal cord and synapse in autonomic ganglia. The ganglia function as relay stations between the preganglionic neuron and the postganglionic neuron.
Postganglionic neuron: The cell body originates in the ganglion, is generally nonmyelinated, and terminates on effector organs such as visceral smooth muscle, cardiac muscle, and exocrine glands
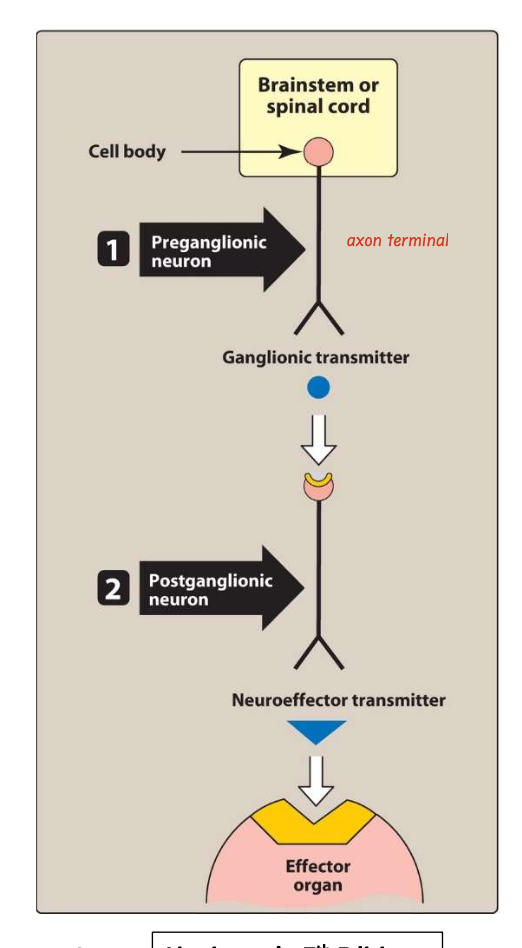
The ANS carries nerve impulses from the CNS to the effector organs via two types of efferent neurons?
preganglionic and postganglionic neurons
what is the ANS known for and its fans?
know as involuntary nervous system
regulates everyday requirements of vital body functions
what are autonomic drugs?
Drugs that produce their primary therapeutic effect by mimicking or altering the functions of the ANS
how do autonomic agents act?
By stimulating portions of the ANS or by blocking the action of the autonomic nerves.
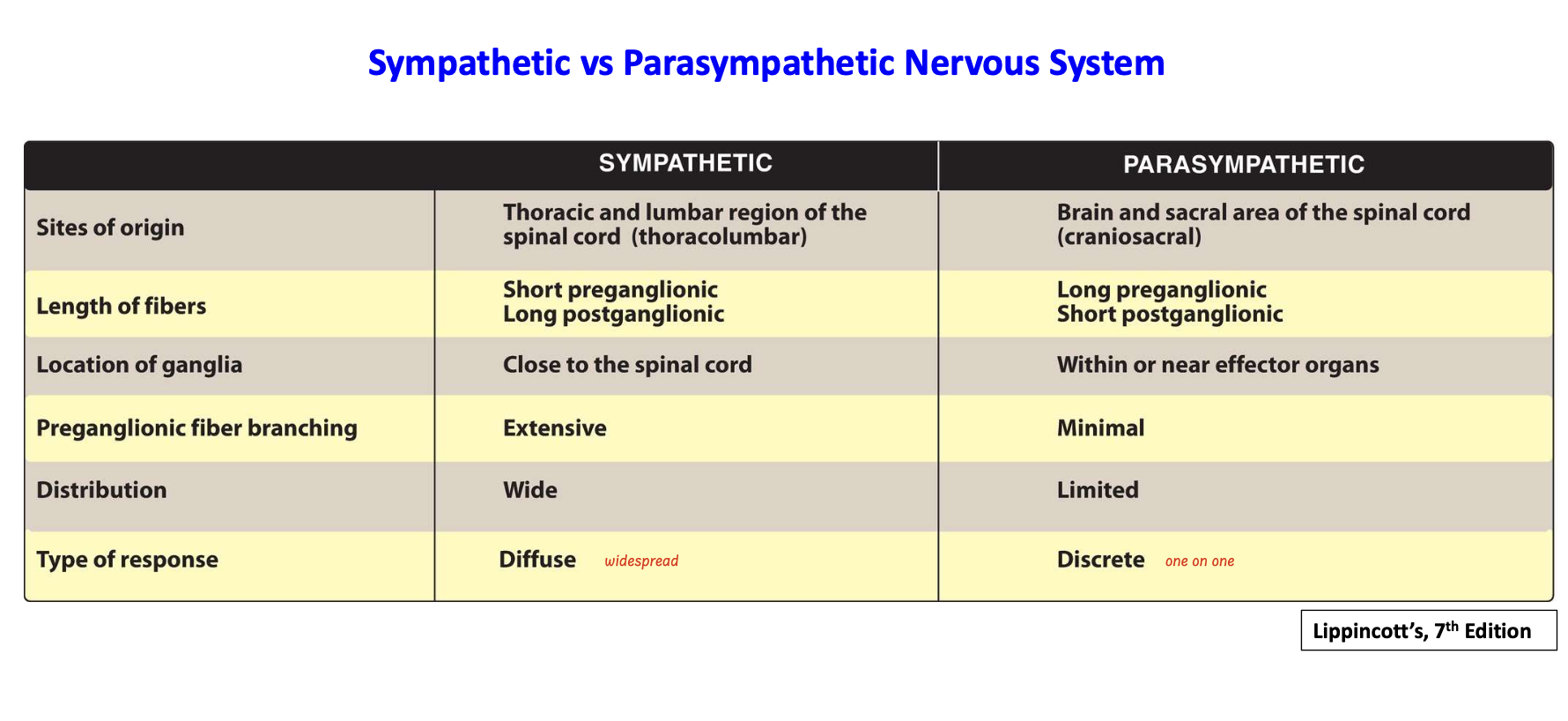
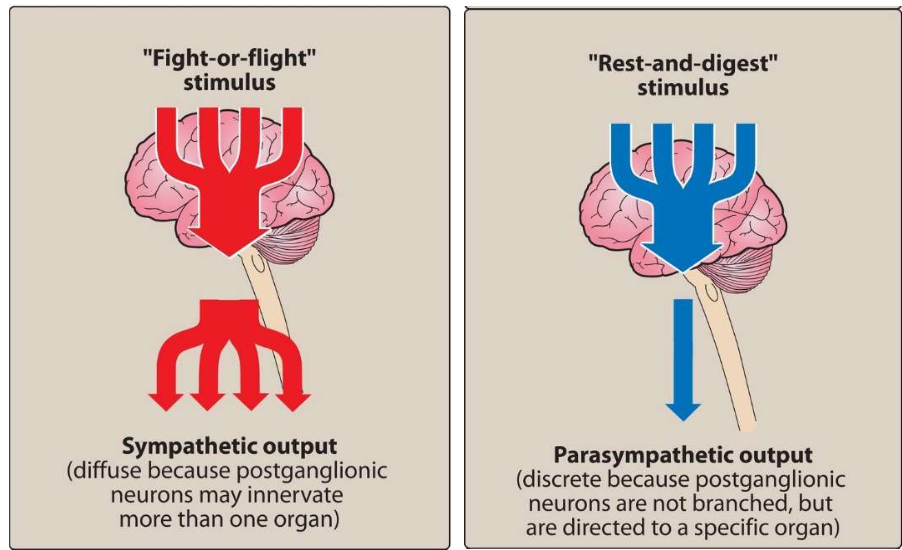
Differentiate between sympathetic and parasympathetic system
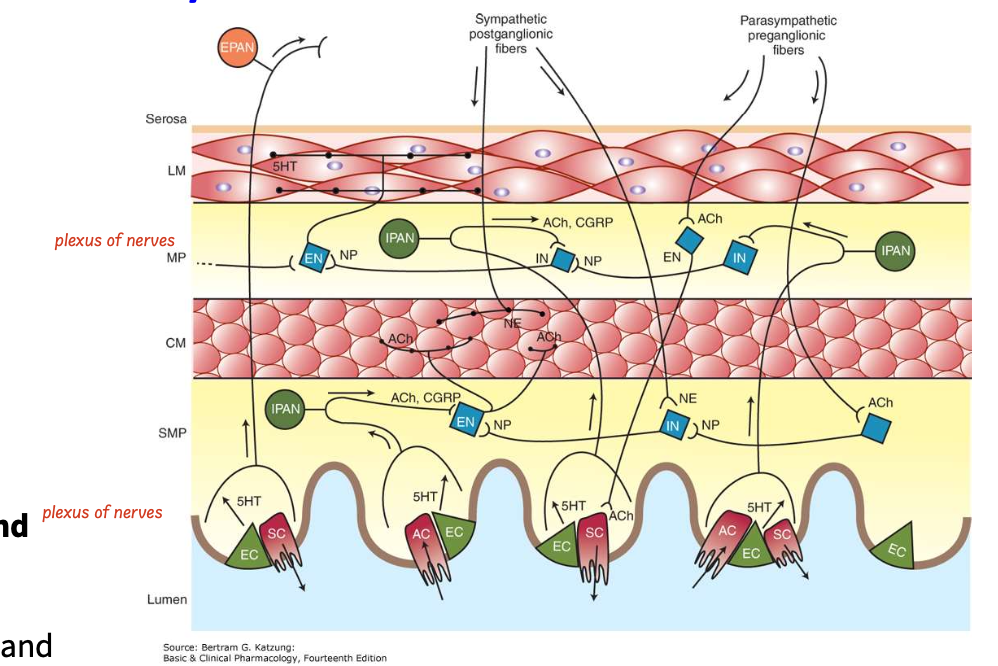
What are the key features of enteric nervous system?
third division of the ANS
Nerve fibers innervate the GI tract, pancreas, and gallbladder
Functions independently of the CNS
Controls motility, exocrine and endocrine secretions, and microcirculation of the GI tract
Modulated by input from both sympathetic and parasympathetic systems
Sends afferent impulses to sympathetic ganglia and the CNS
What are the sympathetic and parasympathetic actions on the eye,lacrimal glands, heart, bronchioles, bladder and GIT?
Eye
Sympathetic: contraction of the iris radial muscle (pupil dilates)
Parasympathetic: contraction of the iris sphincter muscle (pupil contracts), Contraction of the ciliary muscle (lens accommodation for near vision)
Lacrimal Glands
parasympathetic: stimulation of tears
Heart
Sympathetic: ↑ heart rate and ↑ contractility
Parasympathetic: ↓ heart rate and ↓ atrial contractility (M2)
Bronchioles
Sympathetic: Dilation
Parasympathetic: Constriction, increased secretions
Bladder
Sympathetic: Detrusor relaxation, contraction of the sphincter and the trigone
Parasympathetic: Detrusor contraction, relaxation of the sphincter and the trigone
GIT
Sympathetic: ↓ muscle motility and tone, contraction of sphincters, secretion
Parasympathetic: ↑ muscle motility and tone
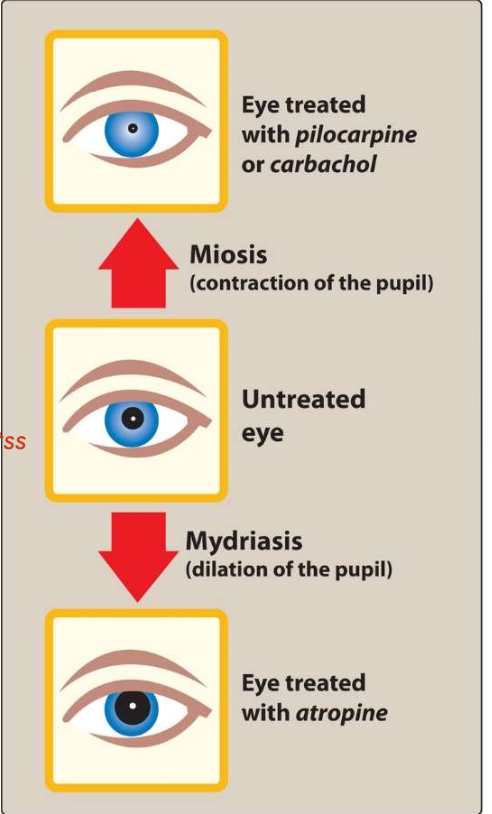
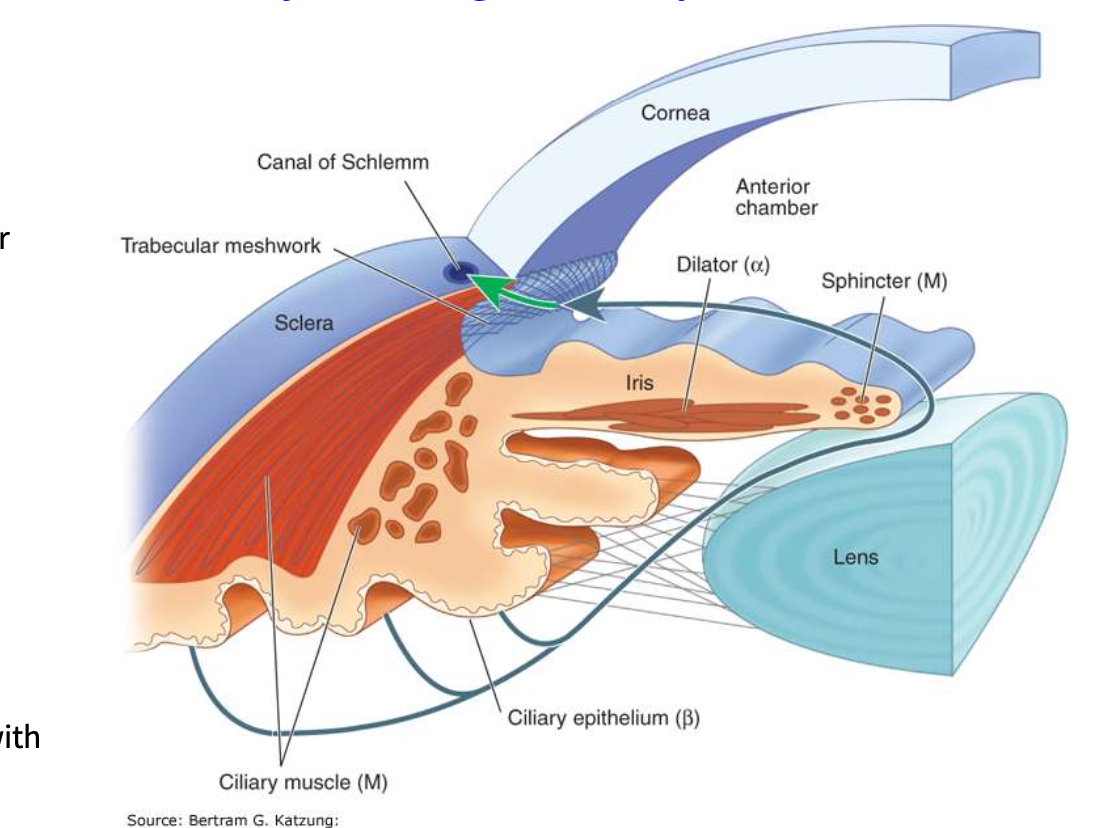
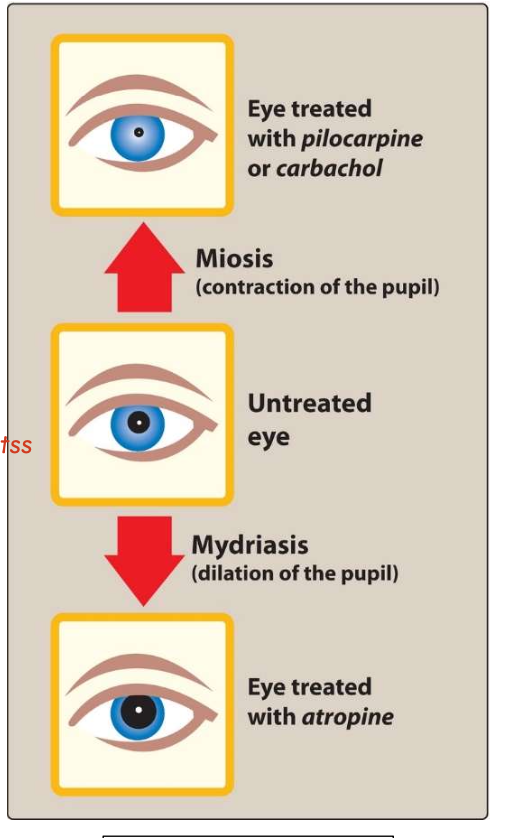
What are the consequences of stimulation/blockade of ANS receptors in the eye?
α1 stimulation in iris dilator → induces contraction→ mydriasis
M3 stimulation in iris sphincter → induces contraction→ miosis
M3 stimulation in ciliary muscle → induces contraction→ accommodation
β-adrenoceptor stimulation → ciliary muscle relaxation → restoration of normal lens shape
β-adrenoceptor blockade (associated w ciliary epi) → ↓ aqueous humor secretion → ↓ IOP
What is the main role of the sympathetic and parasympathetic system on the body?
Sympathetic system: Adjusts body responses to stress (trauma, fear, hypoglycemia, cold, exercise), ↑ heart rate, ↑ BP, dilates pupils and bronchioles, ↓ GI motility, and mediates the fight-or-flight response
Parasympathetic system: Maintains body homeostasis, essential bodily functions like digestion and elimination and opposes sympathetic actions
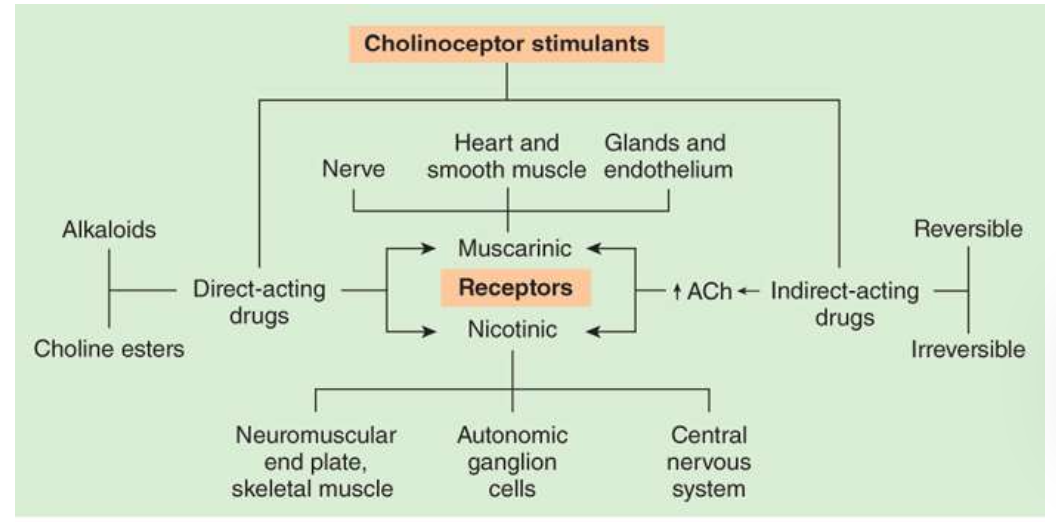
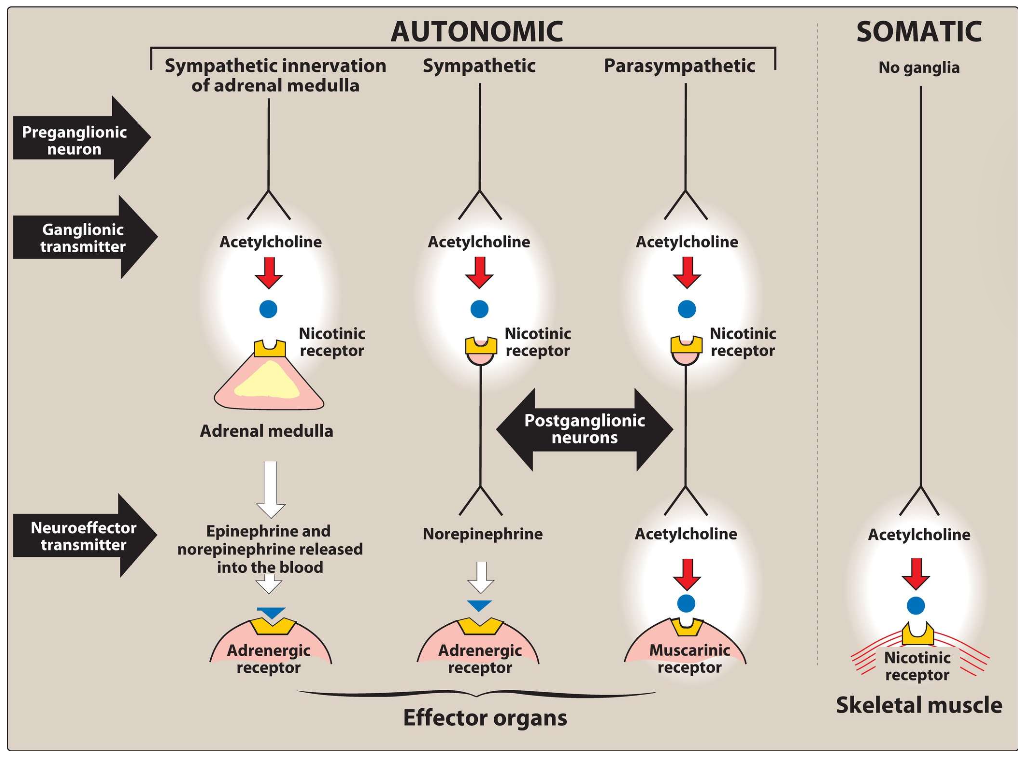
study this picture
Know this well
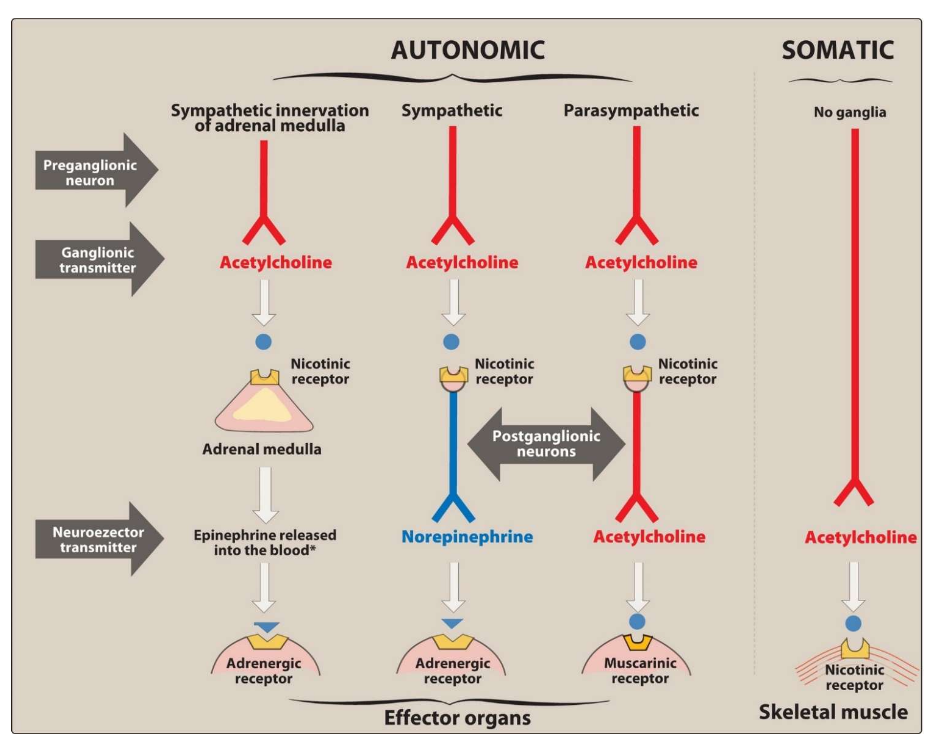
Differentiate between a cholinergic and adrenergic neuron
Cholinergic neuron: Uses acetylcholine as its neurotransmitter
Adrenergic neuron: Uses norepinephrine as its neurotransmitter
Fxn of acetylcholine
Mediates the transmission of nerve impulses across autonomic ganglia in both the sympathetic and parasympathetic nervous systems
The autonomic nerve fibers can be divided into two groups based on the type of neurotransmitter release
If transmission is mediated by acetylcholine, the neuron is termed cholinergic
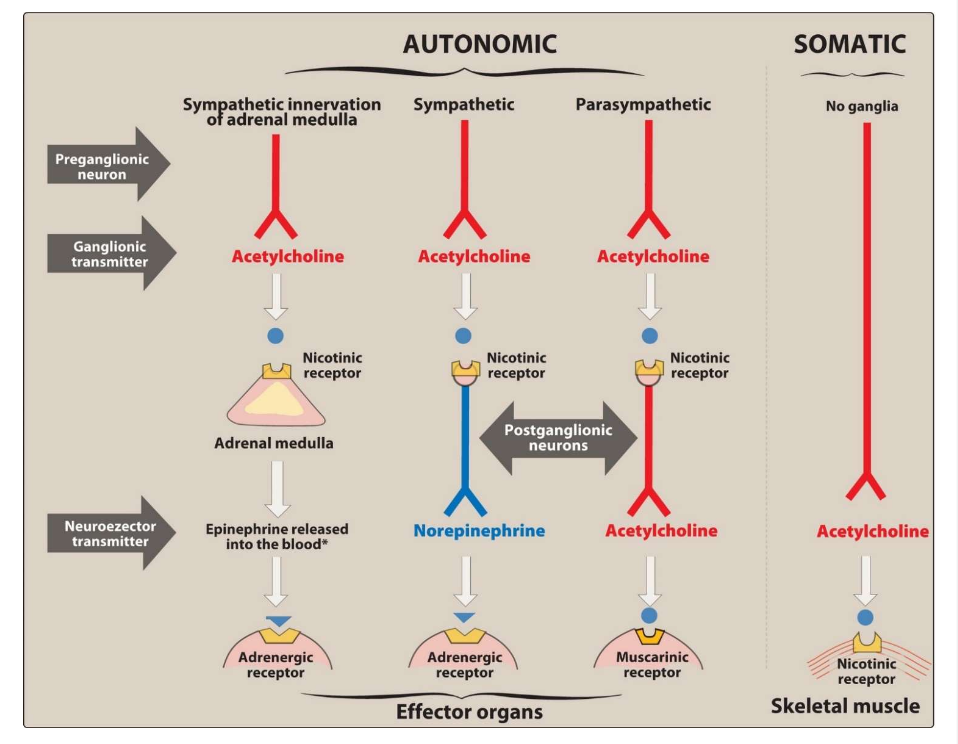
Fxn of norepinephrine (noradrenaline)
When norepinephrine is the neurotransmitter, the fiber is termed adrenergic
In the sympathetic system, norepinephrine mediates the transmission of nerve impulses from autonomic postganglionic nerves to effector organs.
What is the main rate-limiting step in the synthesis of catecholamines? Name the enzyme involved (COULDN’T FIND ANS ON SLIDE)
The rate-limiting step in catecholamine synthesis is the conversion of tyrosine to DOPA, catalyzed by tyrosine hydroxylase
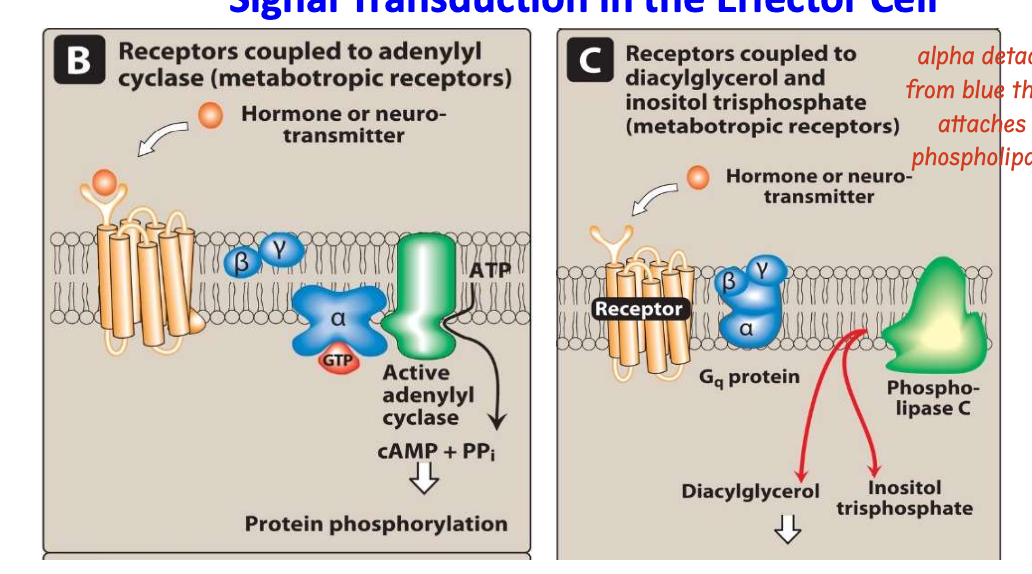
Differentiate between ionotropic and metabotropic receptor. What are the two main second messenger systems?
Ionotropic receptors: Post-synaptic cholinergic nicotinic receptors in skeletal muscle cells are directly linked to membrane ion channels
Metabotropic receptors: they mediate the effects of ligands by activating a second messenger system inside the cell (G-protein coupled receptors that activate intracellular second messengers)
Second messenger systems:
Adenylyl cyclase system
Calcium/phosphatidylinositol system
what are cholinergic receptors further classfied as
nicotinic or muscarinic
what does the binding of neurotransmitters do to ionotropic receptors
directly affexts ion permeability
The binding of chemical signals to receptors activates enzymatic processes within the cell membrane, resulting in cellular responses such as:
Phosphorylation of intracellular proteins or
Changes in the conductivity of ion channels
The receptors in the ANS effector cells are classified as what? Also, what binds to these receptors?
The receptors in the ANS effector cells are classified as adrenergic or cholinergic based on the neurotransmitters or hormones that bind to them.
Epinephrine and norepinephrine bind to adrenergic receptors
Acetylcholine binds to cholinergic receptors
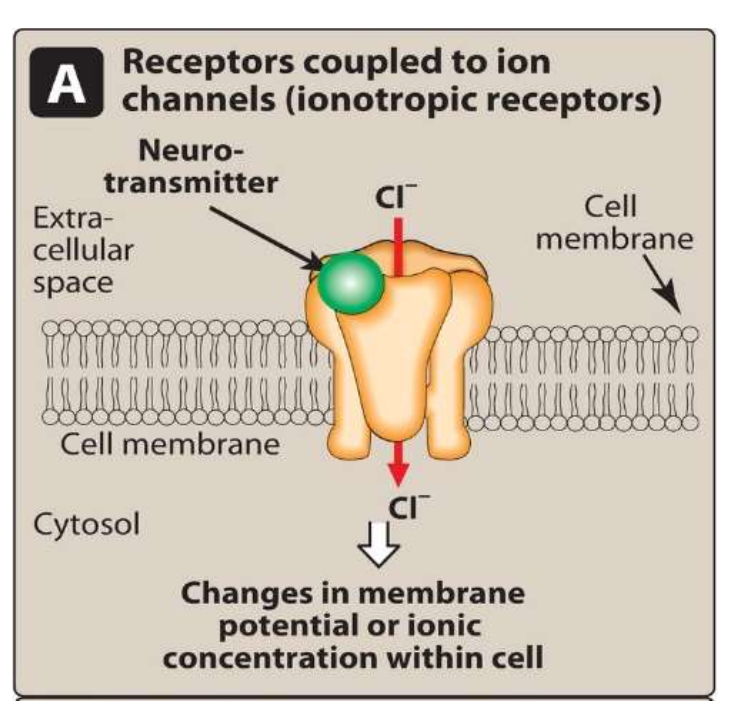
Briefly outline the steps involved in neurotransmission at cholinergic neurons
Synthesis of ACh
Storage of ACh
Release of ACh
Binding of ACh to receptor
Degradation of ACh in synaptic cleft
Recycling of choline
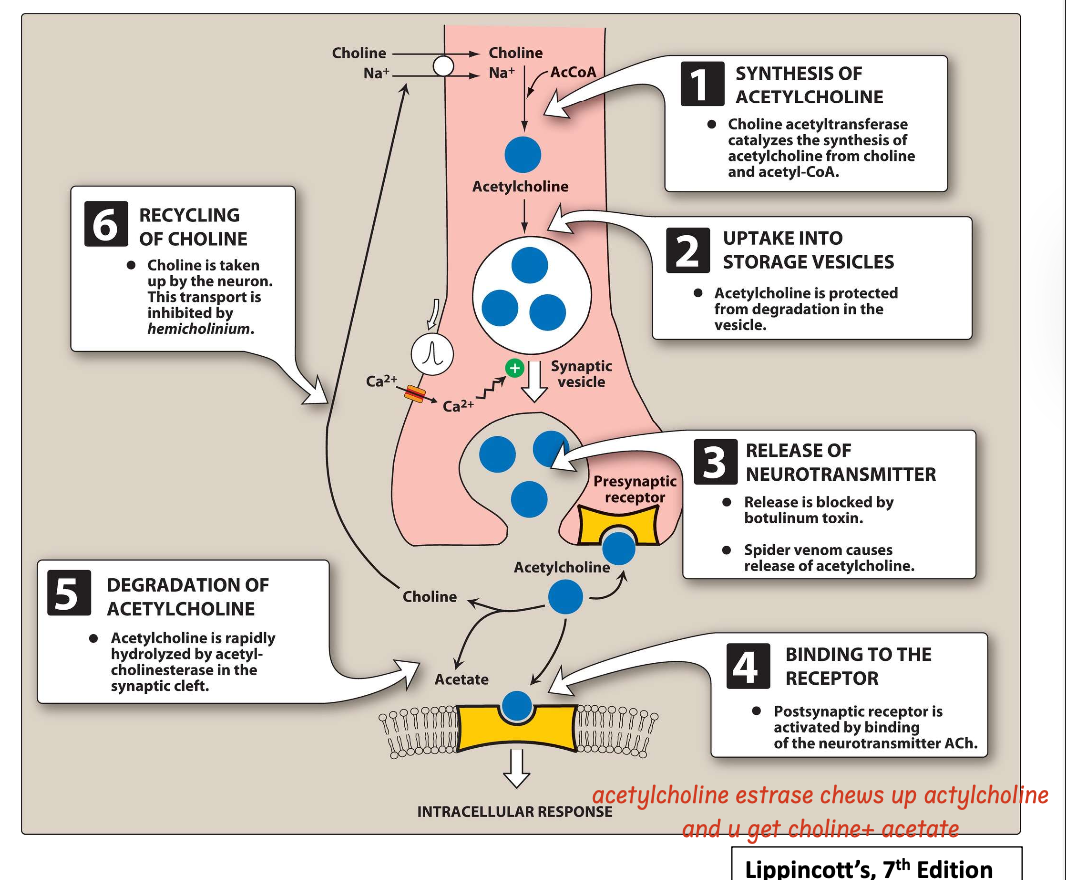
What are the two main cholinergic receptors and how do they differ from each other?
Nicotinic receptors: Ionotropic, ligand-gated ion channels
Muscarinic receptors: Metabotropic, G-protein coupled receptors
Note: Cholinoceptor stimulants are classified pharmacologically by their spectrum of action, depending on the type of receptor— muscarinic or nicotinic—that is activated.
Cholinomimetics are also classified by their mechanism of action:
Some bind directly to (and activate) cholinoceptors
Others act indirectly by inhibiting the hydrolysis of endogenous acetylcholine
what group of drugs mimic acetylchline (cholinometics)?
Acetylcholine-receptor stimulants and cholinesterase inhibitors make up a large group of drugs that mimic acetylcholine (cholinomimetics)
Acetylcholine is used as a neurotrasnmitter by:
Preganglionic fibers terminating in the adrenal medulla
Autonomic ganglia (both parasympathetic and sympathetic)
Postganglionic fibers of the parasympathetic division
Postganglionic sympathetic division of sweat glands.
Cholinergic neurons innervating the muscles of the somatic system
Neurons in the central nervous system (CNS)
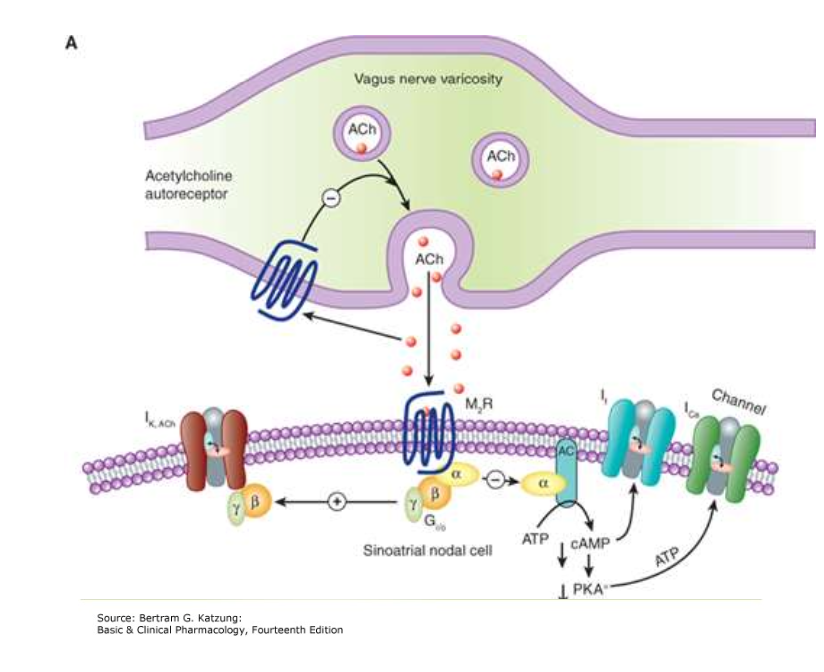
Give the location of M2 and M3 receptors and their associated G protein
M2 receptors: Heart, nerves, smooth muscle — Gi/o protein
M3 receptors: Glands, smooth muscle, endothelium — Gq/11 protein
What are cholinergic agonists? How are they classified?
Cholinergic agonists are drugs that mimic acetylcholine by binding directly to cholinoceptors (muscarinic or nicotinic).
They are classified as:
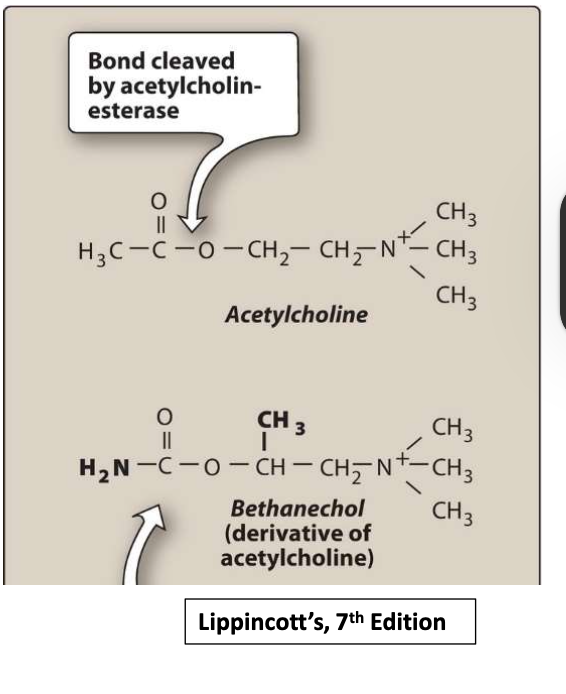
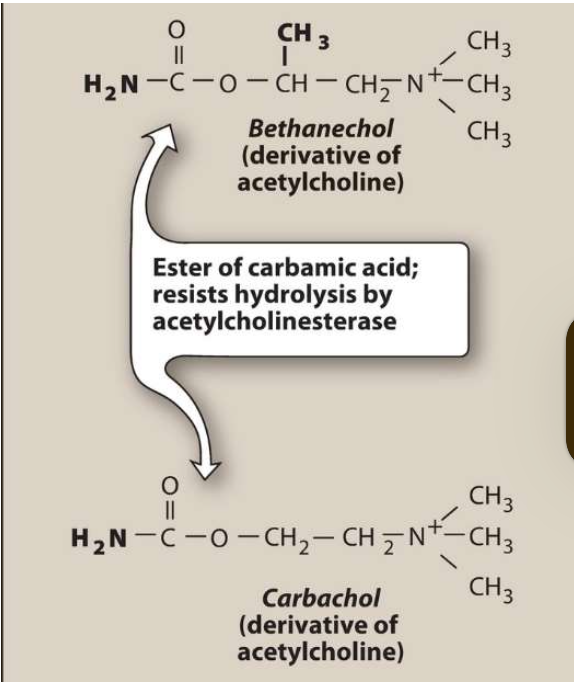
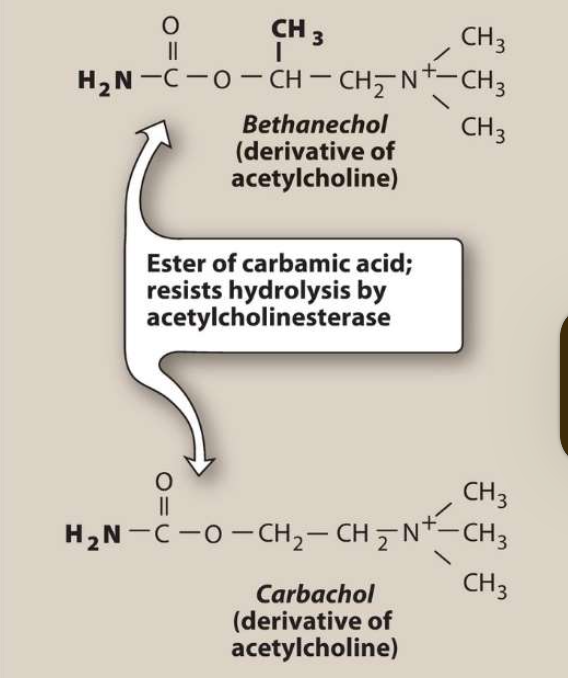
Choline esters- includes endogenous Ach and synthetic esters of choline, such as carbachol and bethanechol,
Naturally occurring alkaloids, such as nicotine and pilocarpine
what is a key characteristic of direct acting cholingeric drugs
have longer duration of action than Ach
what drugs are considered “more therapeutically useful” and what do they typically bind too?
More therapeutically useful drugs (pilocarpine and bethanechol) preferentially bind to muscarinic receptors
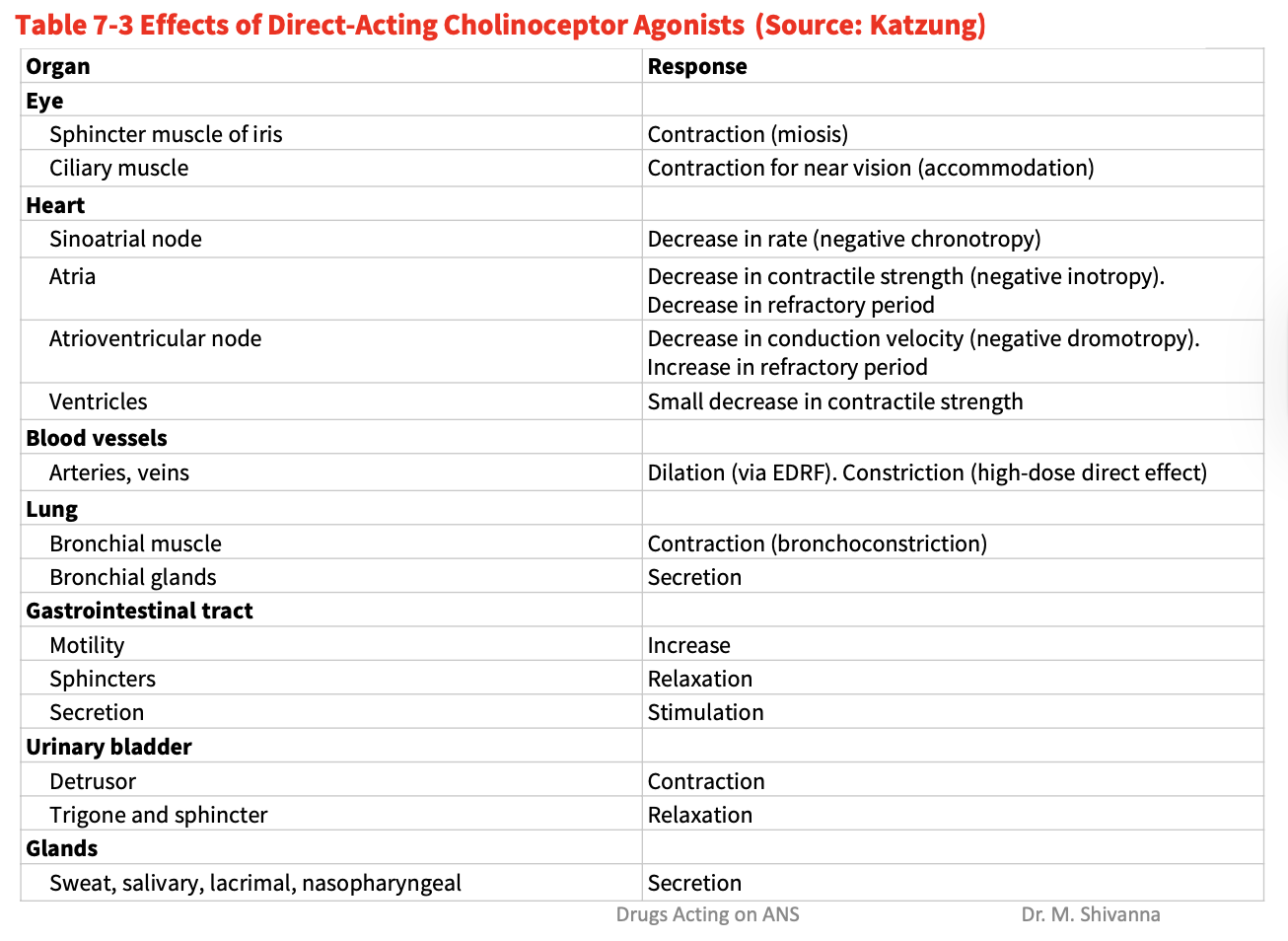
What is the influence of acetylcholine on the heart, blood pressure, bladder, eye and secretions?
Heart: Decreases heart rate and cardiac output (Acetylcholine mimics vagal stimulation, so when given IV, it slows SA node firing, causing bradycardia and decreased cardiac output)
Blood pressure: Causes vasodilation and decreases BP (cuz Injection of acetylcholine lowers blood pressure indirectly by activating M3 receptors on endothelial cells, which release nitric oxide, causing smooth muscle relaxation and vasodilation)
Bladder: Contracts detrusor muscle → urination
Eye: Causes miosis and accommodation (involved in stimulation of ciliary muscle contraction, topical for near vision and constriction of the sphincter muscle causing miosis)
Secretions: Increases salivary, gastric, intestinal and bronchial secretions and also increases intestinal motility
What is the adverse effect of direct acting cholinergic agonists on blood pressure, lungs, salivary and sweat glands and GIT? (DK ANS TO THIS)
Blood pressure: Decreased BP (FC THIS)
Dilation (via EDRF). Constriction (high-dose direct effect)
Lungs: Bronchoconstriction in bronchial muscle, secretion in bronchial glands (maybe even bronchospasm FC this)
Salivary & sweat glands: Excessive secretion
GIT: Abdominal pain, diarrhea, increased motility
What is the adverse influence of pilocarpine on the eye?
Pilocarpine causes blurred vision, night blindness, brow ache, and spasm of accommodation
Potent stimulator of secretions such as sweat, tears, and saliva,
Give the therapeutic applications of pilocarpine
Treatment of open-angle and angle-closure glaucoma to lower IOP in emergency
Reversal of atropine-induced mydriasis
Treatment of xerostomia (promotes salivation to dry mouth) resulting from irratiation of head and neck
Oral tablets useful in treatment of Sjögren syndrome (characteritized by dry mouth and lack of tears)
know this chart
what is instilled into eye during opthalmic surgery
Ach (1% solution) is instilled into the anterior chamber of the eye to produce miosis during ophthalmic surgery
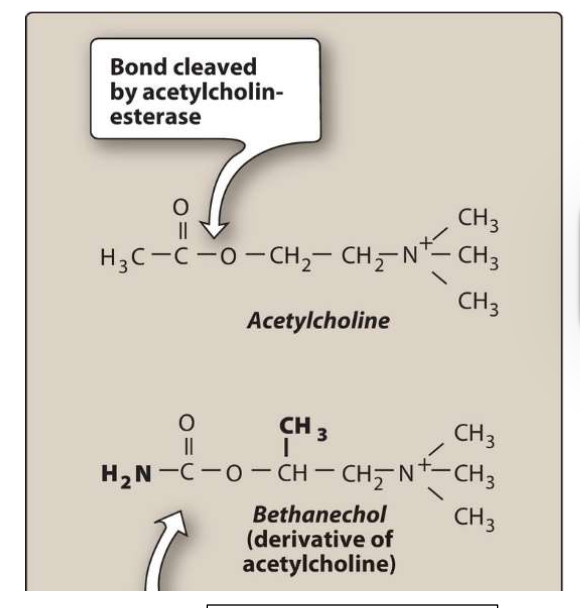
Give the characterisitcs of Bethanechol
Carbamoyl ester, structurally related to ACh
Not hydrolyzed by acetylcholinesterase (AChE), but inactivated through by other esterases
No nicotinic action but strong muscarinic activity
Acts mainly on smooth musclature (bladder + GI tract)
Duration of action ≈ 1 hour
Actions of bethanechol
Directly stimulates muscarinic receptors, causing increased intestinal motility and tone
It also stimulates the detrusor muscle of the bladder stimulating urination.
therapeutic uses of Bethanechol
To stimulate the atonic (acontractile) bladder in postpartum or
postoperative, nonobstructive urinary retention.
Neurogenic atony (bladder function related to neurological
damage)
Megacolon (abnormal dilation of the colon accompanied by paralysis
of peristalsis).
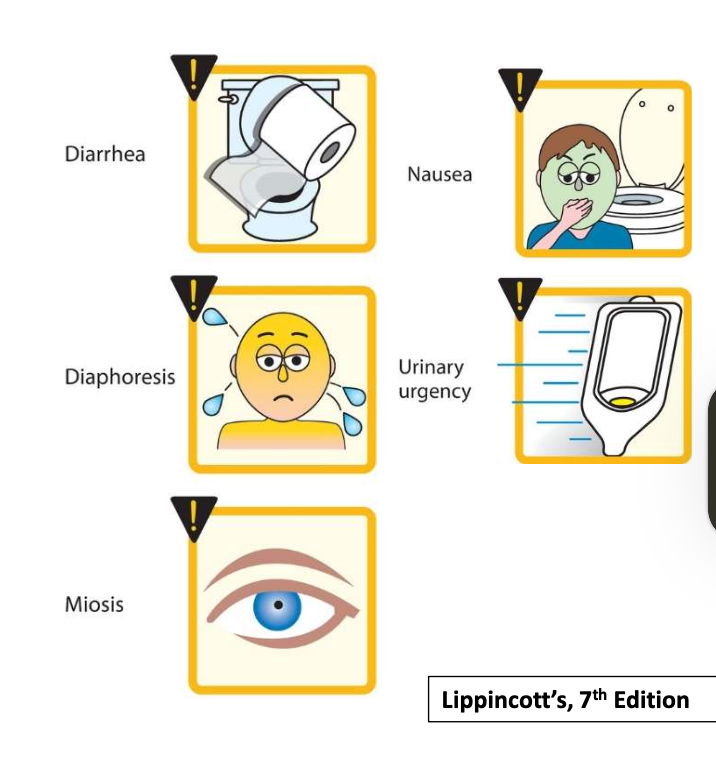
Adverse effects of bethanechol
Sweating
Salivation
Flushing
Decreased blood pressure (with reflex tachycardia)
Nausea
Abdominal pain
Diarrhea and bronchospasm
Key characterisitcs of Carbachol (Miostat)
Has both muscarinic and nicotinic actions.
An ester of carbamic acid and a poor substrate for AChE.
Biotransformed by other esterases, but at a much slower rate.
Actions of Carbachol (Miostat)
Strong effects on cardiovascular + GI system (cuz of ganglionic activity → First stimulates, then depresses these systems)
Nicotinic action causes epinephrine release from the adrenal medulla
mimics effect of ACh in the eye causes miosis (pupil constriction) + spasm of accommodation
Due to accomodation spasm, vision becomes fixed at one distance making it impossible to focus
Therapeutic uses of Carbochol and Adverse effects
Therapeutic uses of Carbachol
Intraocular use provides miosis for eye surgery
Lowers intraocular pressure in the treatment of glaucoma.
Adverse effects
Few adverse effects with ophthalmologic use due to lack of systemic penetration
Characterisitics of Pilocarpine (Pilocar)
Stable to hydrolysis by AChE
Uncharged and can penetrate the CNS at therapeutic doses
Exhibits muscarinic activity and is used primarily in ophthalmology