USMLE CVS
1/76
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
77 Terms
What are 2 types of the coarctation of the aorta?
1.Preductal coarctaion (associated with Turner syndrom)
2. Postductal coarctation
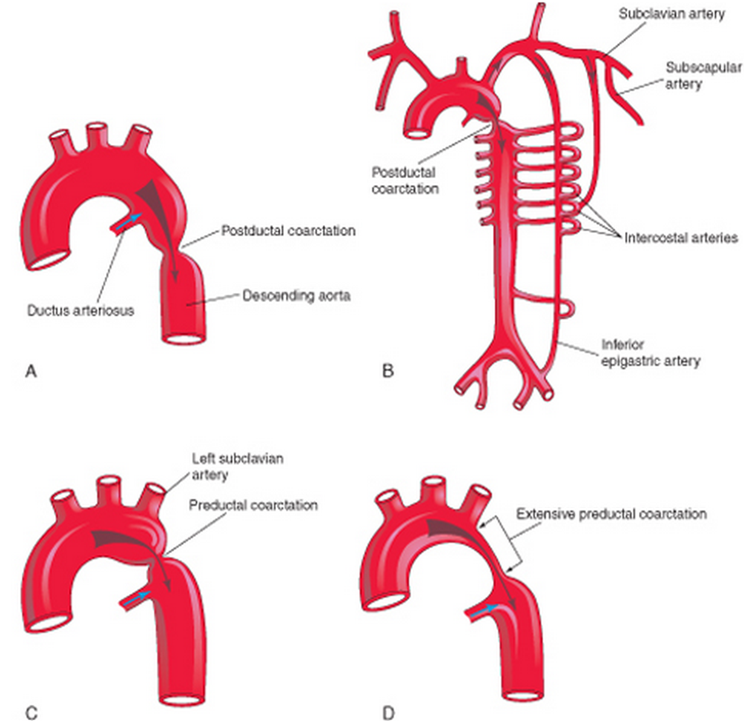
How can you suspect the coarctation of the aorta in a patient?
In an infant - poor weight gain, feeding problems, breathing probems (left ventricle hypethrophy as a reaction to the pressure increased) + hypertensive in the upper body and hypotensive and cyanose with weak pulse in the lower limbs
In adults - hypertensive in the upper body and hypotensive with weak pulse in the lower limbs, as result of the left ventricle hypethrophy - pulmonary hypertension+ costal notching (enlargment of the intercostal arteries, can be seen on X-ray). Dissecting aorta aneurysm + intracerebral hemorrhage.
Velocity
Velocity= Q/CSA (cm/sec), low in capillaries, high in the aorta (turbulence).
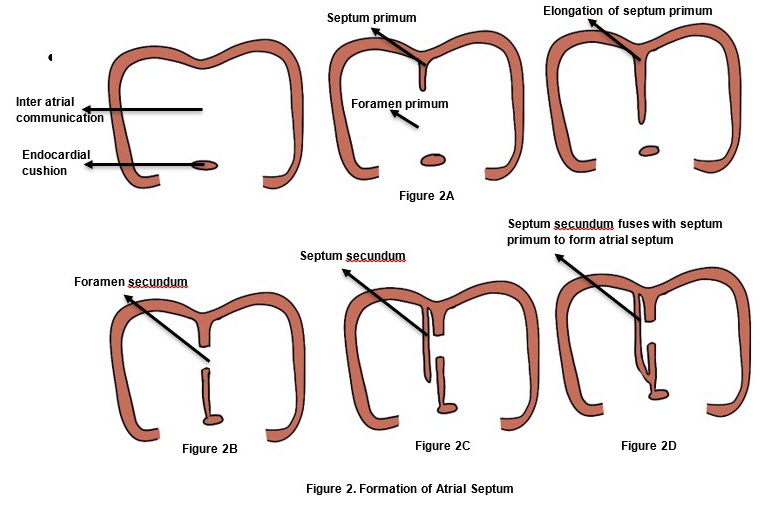
What is the cause of the patent foramen ovale?
Failure of septum primum and septum secundum to fuse after birth (right tp left shunt+paradoxical emboly)
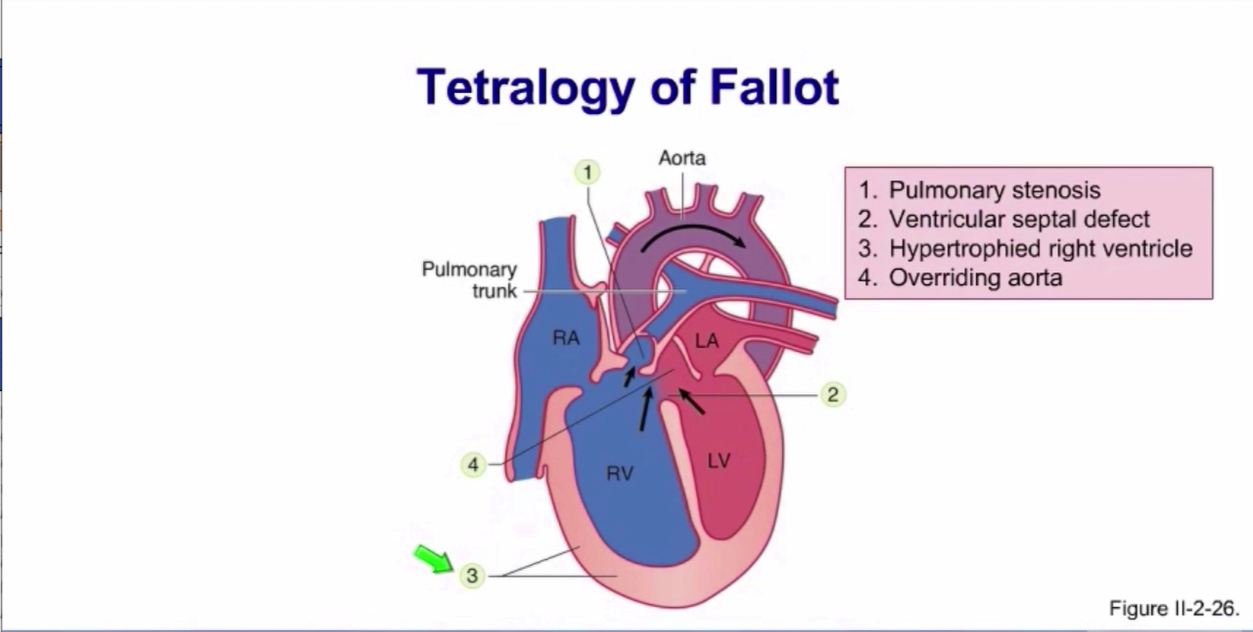
Down Syndrom heart defects?
About 80% have an atrial septal defect or ventricular septal defect with the former being more common. Congenital heart disease can also put individuals at a higher risk of pulmonary hypertension, where arteries in the lungs narrow and cause inadequate blood oxygenation. Some of the genetic contributions to pulmonary hypertension in individuals with Down Syndrome are abnormal lung development, endothelial dysfunction, and proinflammatory genes.Mitral valve problems become common as people age, even in those without heart problems at birth. Other problems that may occur include tetralogy of Fallot and patent ductus arteriosus.
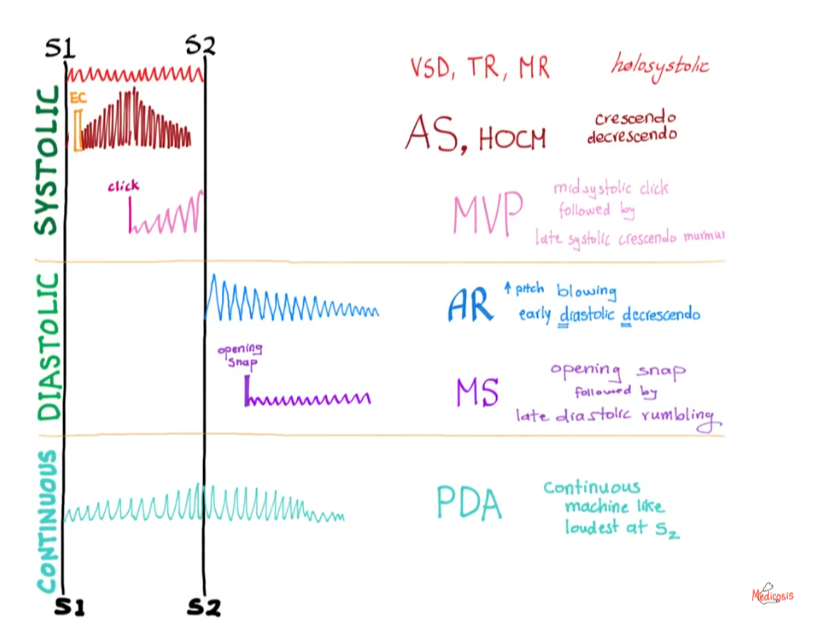
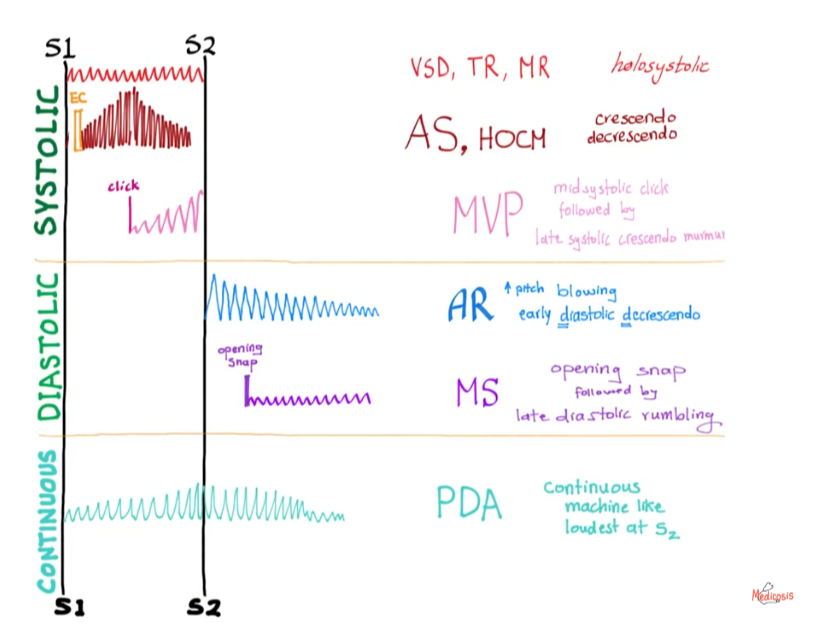
Which conditions are most highly to cause holosystolic heart murmur?
Ventricular septal defect, mitral regurgitation or tricuspid regurgitation.
What embryology defect is present in DeGeorge syndrome?
22q11.2 deletion
Failure to develop 3 and 4 branchial arches - truncus arteriosis, tetralogy of Fallot, thymic hypoplasia, hypoparathyroidism, cleft facial disease
Factors affecting systolic pressure
Factors affecting dyastolic pressure
TPR (direct)
HR (direct)
SV (direct)
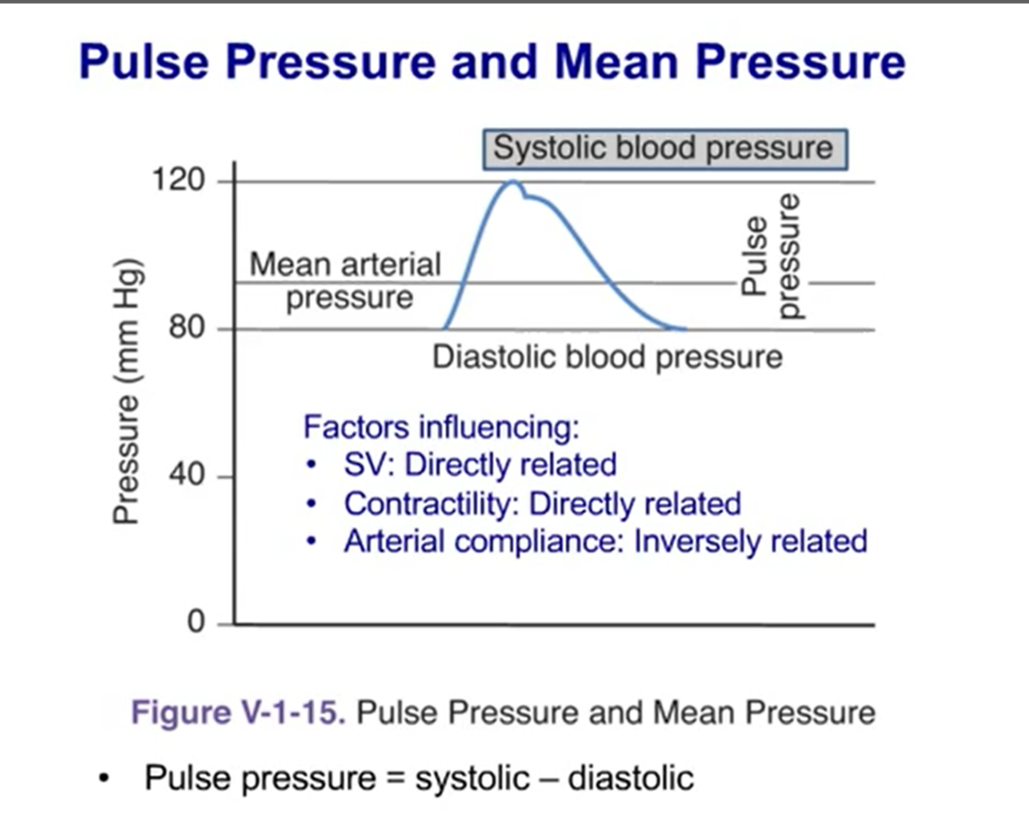
Factors affecting pulse pressure
PP=SV/C
SV (direct) acute and chronic
Compliance(arterial) (inverse) chronic
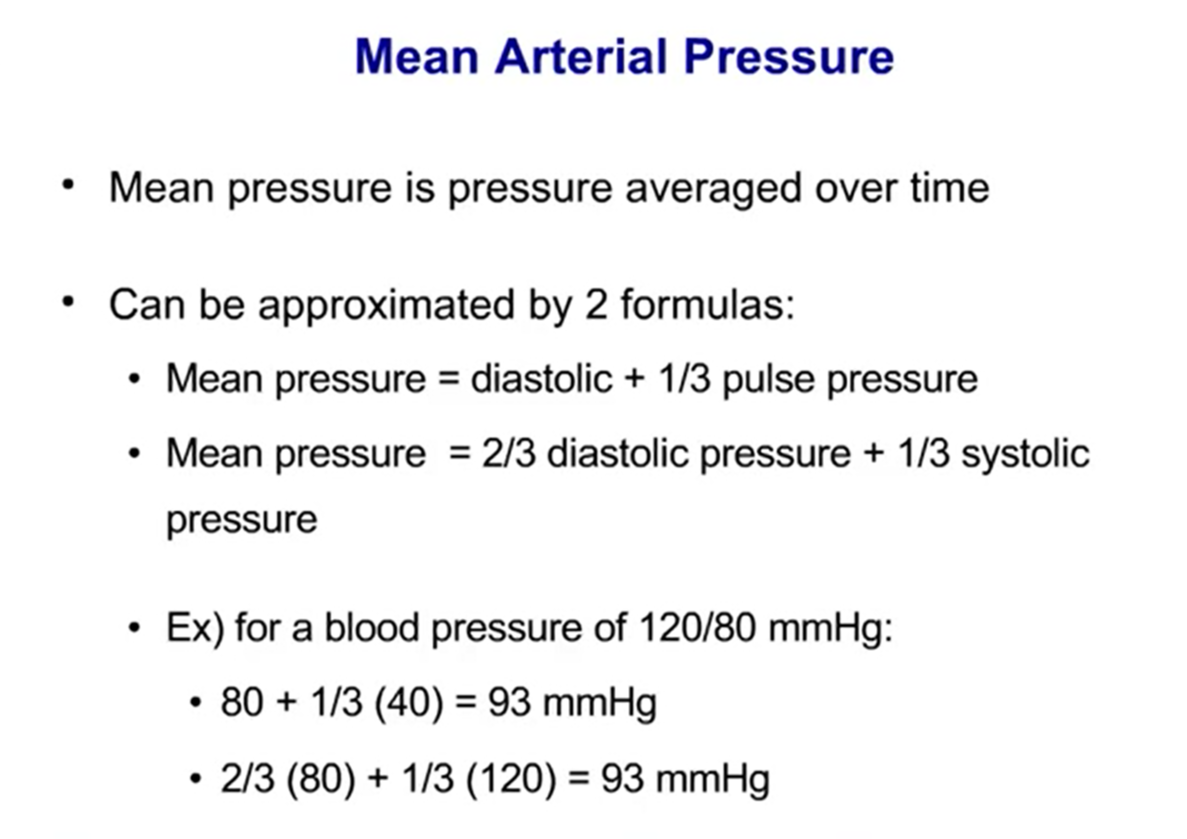
Mean arterial pressure
A normal MAP is about 90 mmHg.
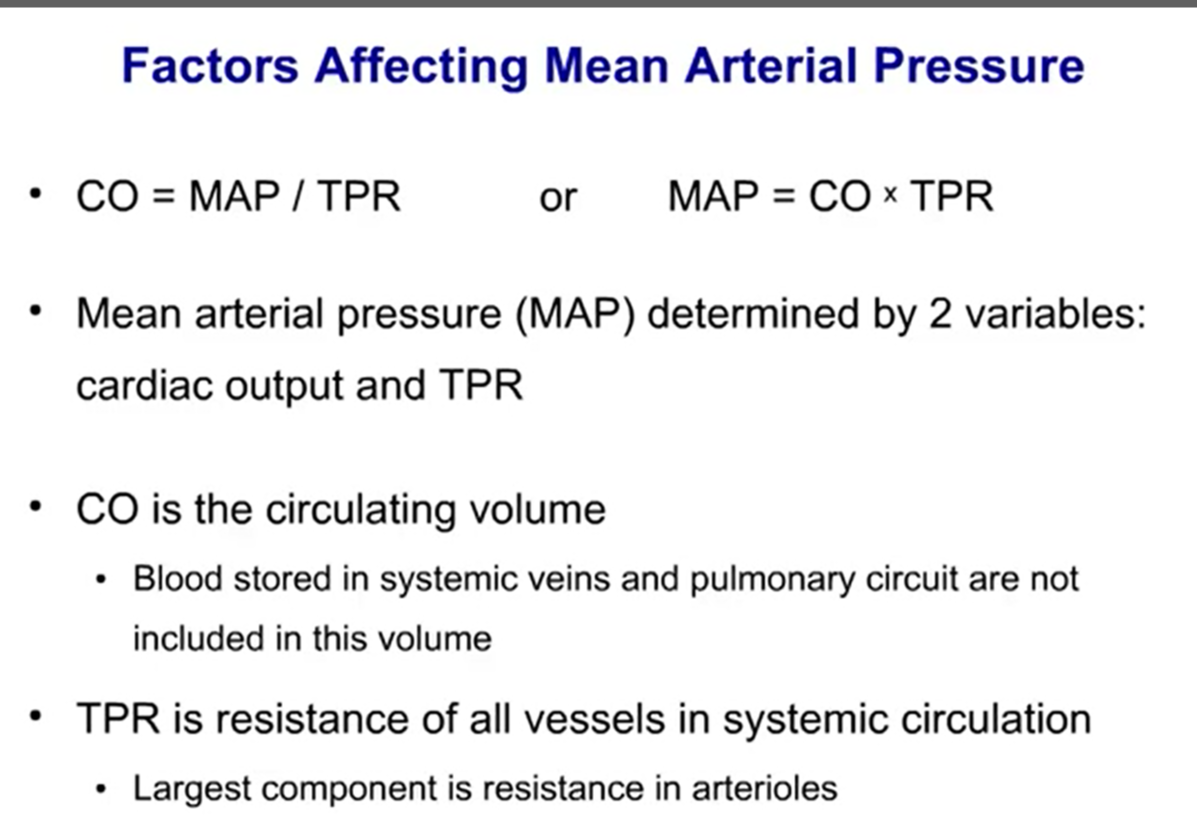
Factors affecting mean arterial pressure
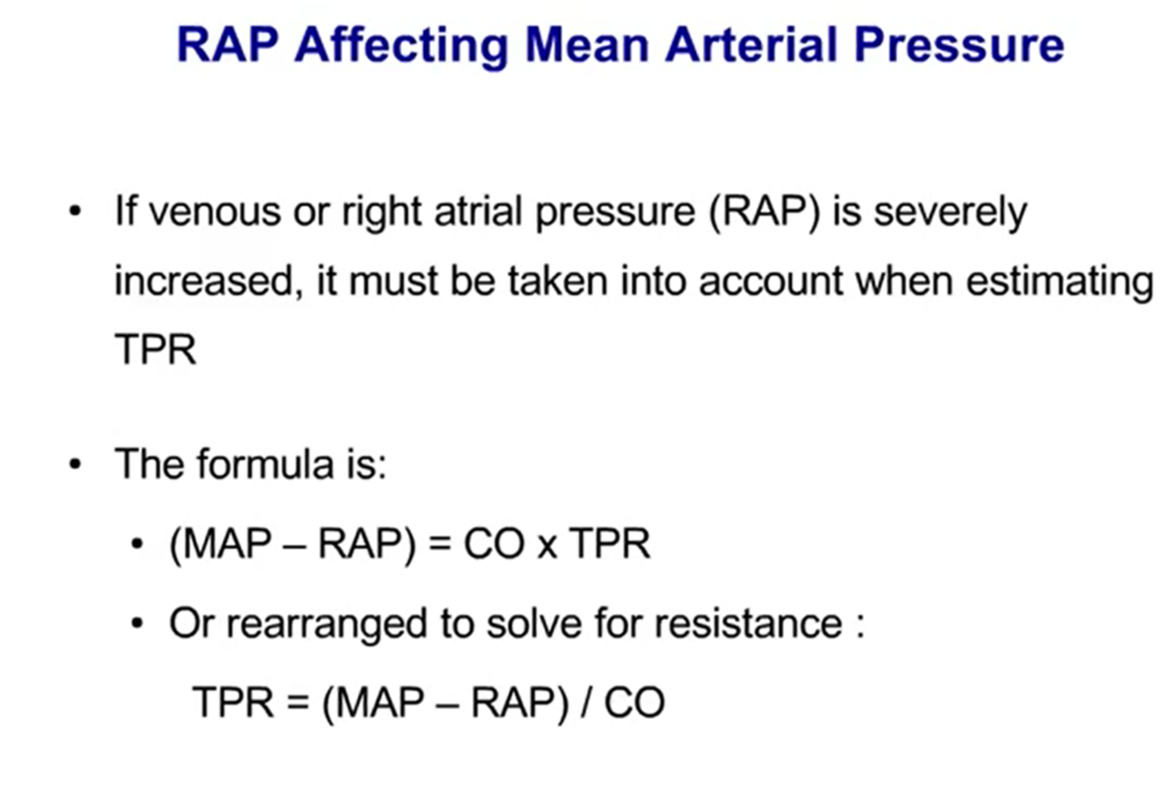
Influence of the RAP on MAP
Aortic regurgitation, type of murmur?
Early diastolic, decrescendo hight-pitched blowing murmur, best heard along the lower left sternal body 2 intercostal space.
Becks triad (cardiac tamponade)
Diminished heart sounds
Decreased arterial pressure
Increased jugular venosus pressure
Effects of the arterial baroreceptors (aortic arch and carotid sinus)
Stimulated by the change (rise) in the intravascular pressure through 9 and 10 nerve to the medulla
Stimulates parasympathetis, inhibits sympathetic (BP increase - symp. decrease, parasym. increase and vice versa)
Activation inhibits ADH
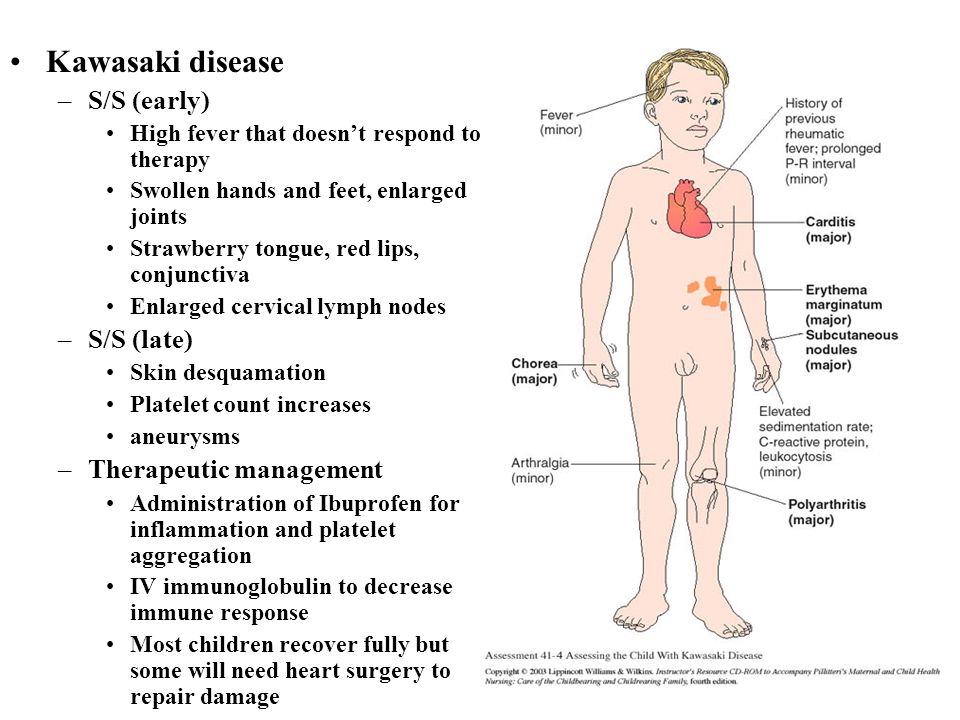
What heart complication might be expected in the person with Kawasaki syndrom?
Coronary artery aneurysms (20%)
The Poiseuille equation
Q=P1-P2/R, P=QR, pressure, flow, resistance (for arterial circuit)
Effects of the length,viscosity and radius on the resistance
R=8ņ (viscosity)*length/пr4
the greater radius the less resistance ( TPR the most in arterioles)
length is constant, 50% reduce in length - 50% reduce resistance
the greater the viscosity the greater the resistance
Reynold’s number
Diameter*velocity*density/viscosity
>2000 - turbulent flow
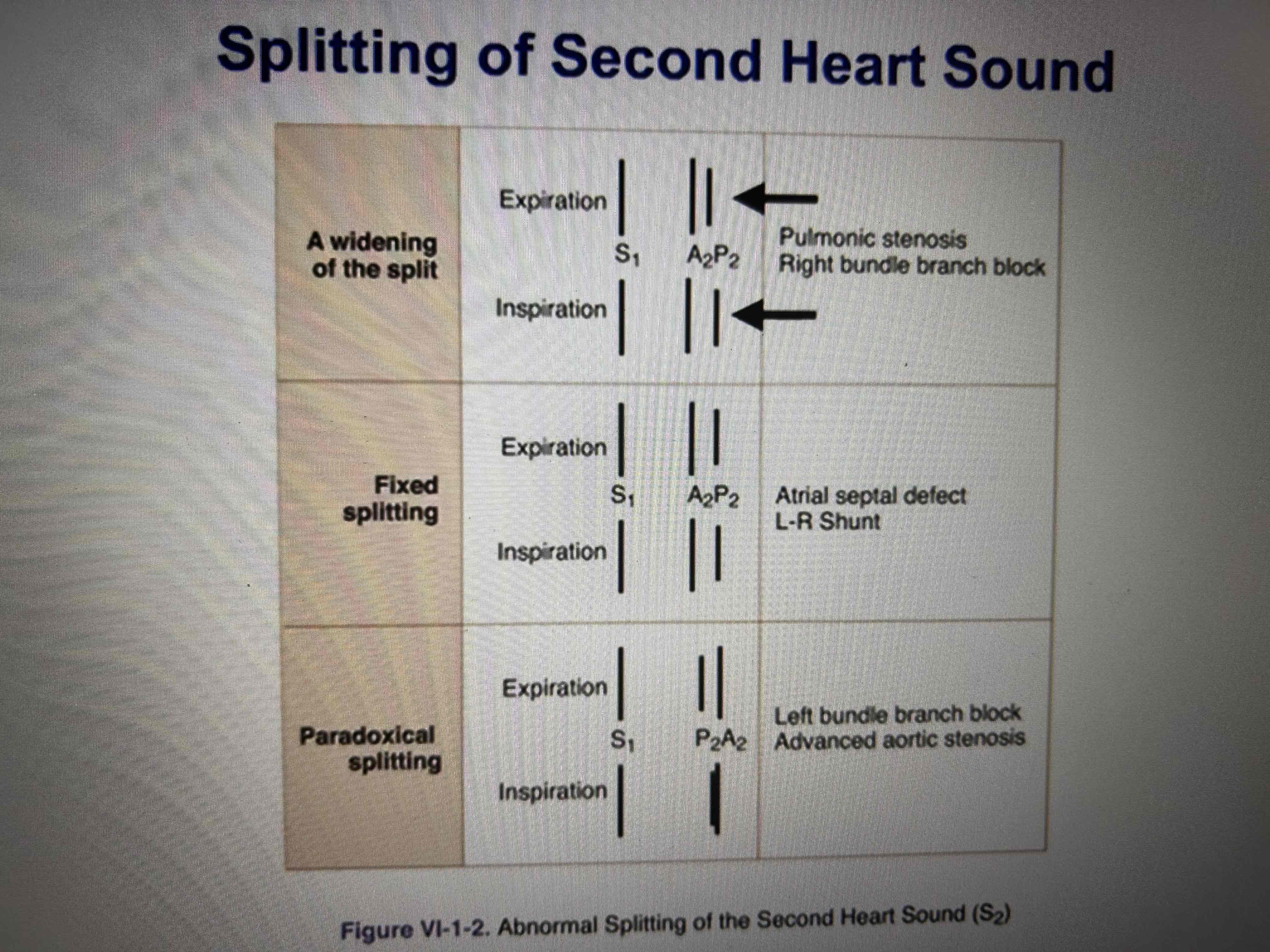
Most common adult congenital heart disease?
Atrial septal defect
1.Midsystolic ejection murmur at the pulmonic area
2.Fixed spitting of S2
3. Prominent right ventricular cardiac impulse
4.Right atrial and ventricular hyperthrophy
Pericarditis
Sharp stabbing pain that varies with breathing
Often positional and relieved by leaning forward
Diffuse ST elevations with upright T-waves
The most common reason for aortic stenosis?
Bicuspid aortic valve (systolic click)
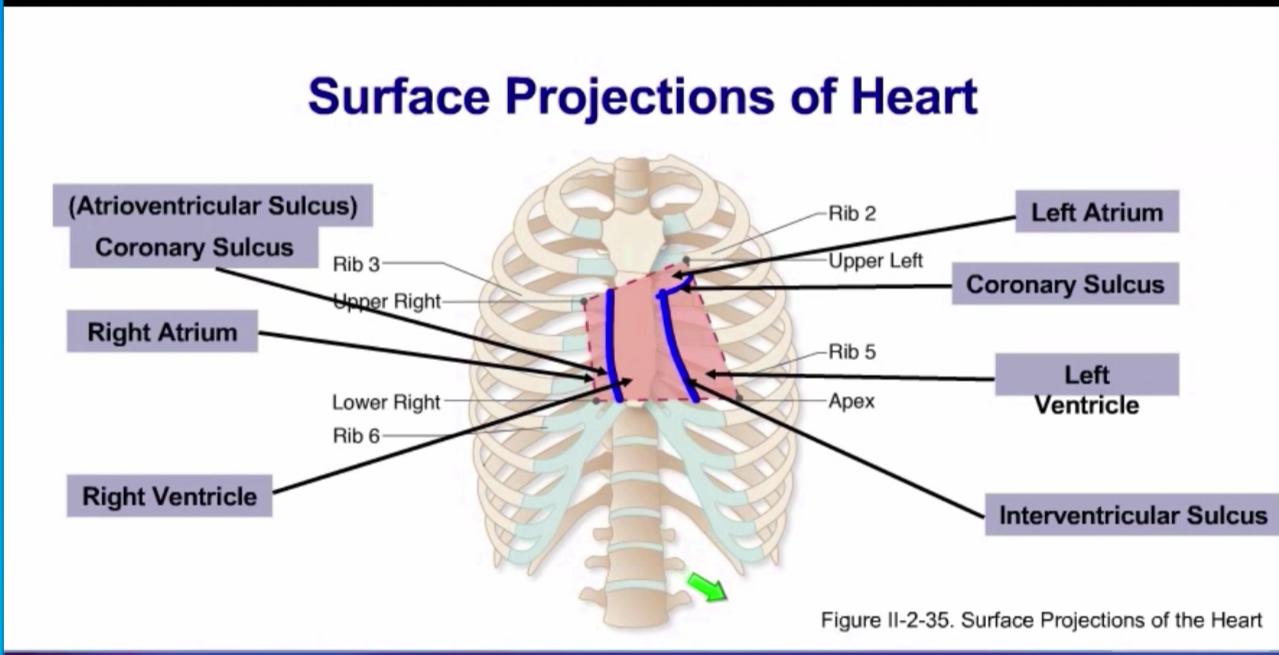
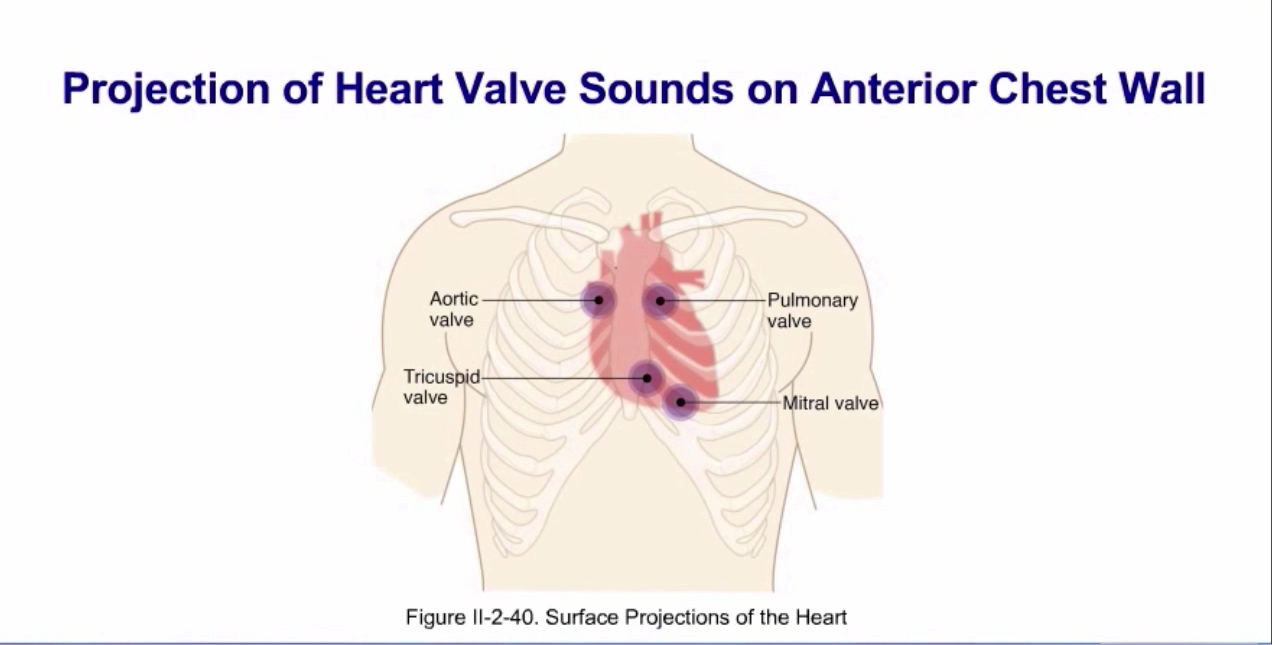
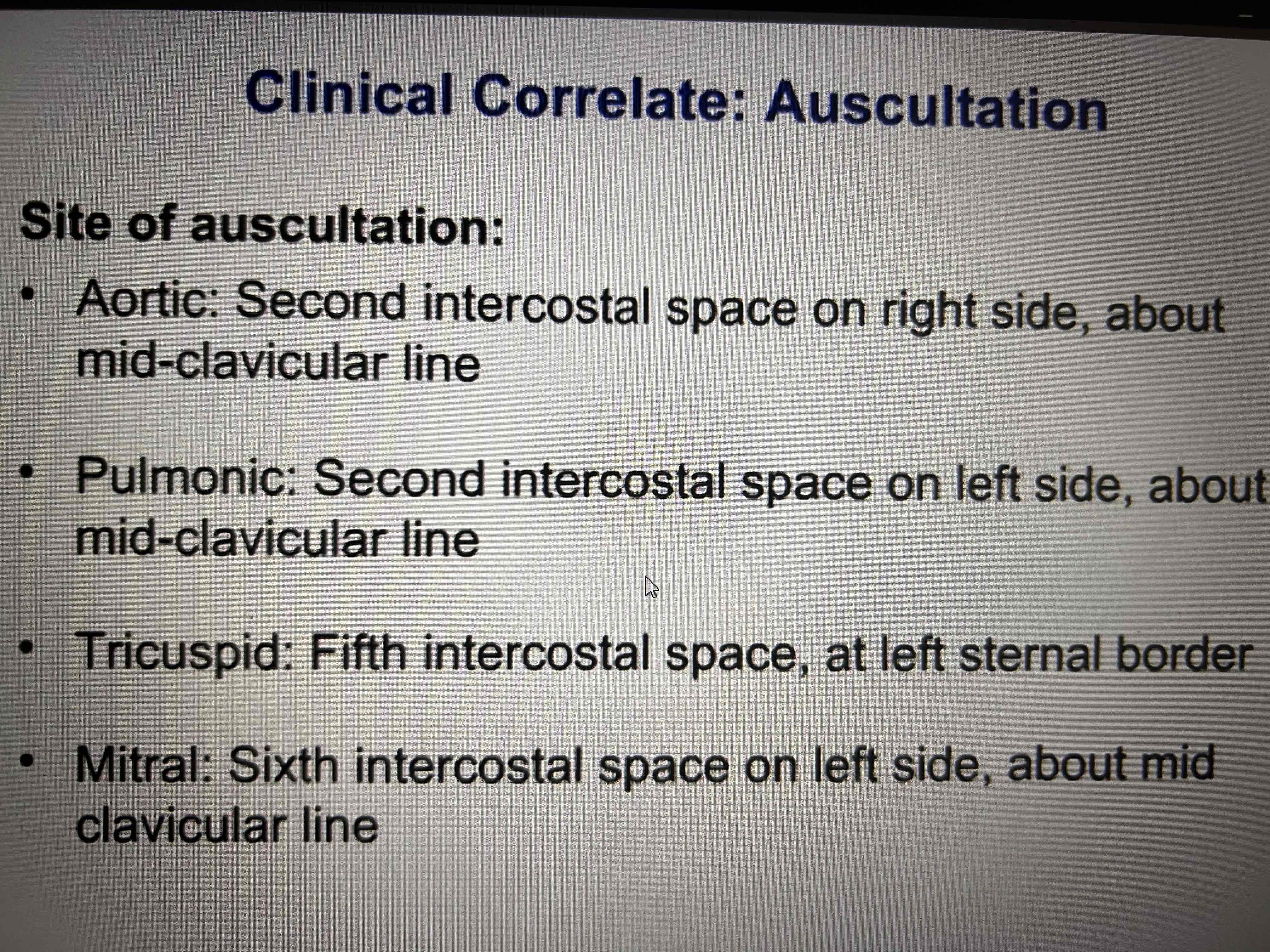
Surface projections of the heart
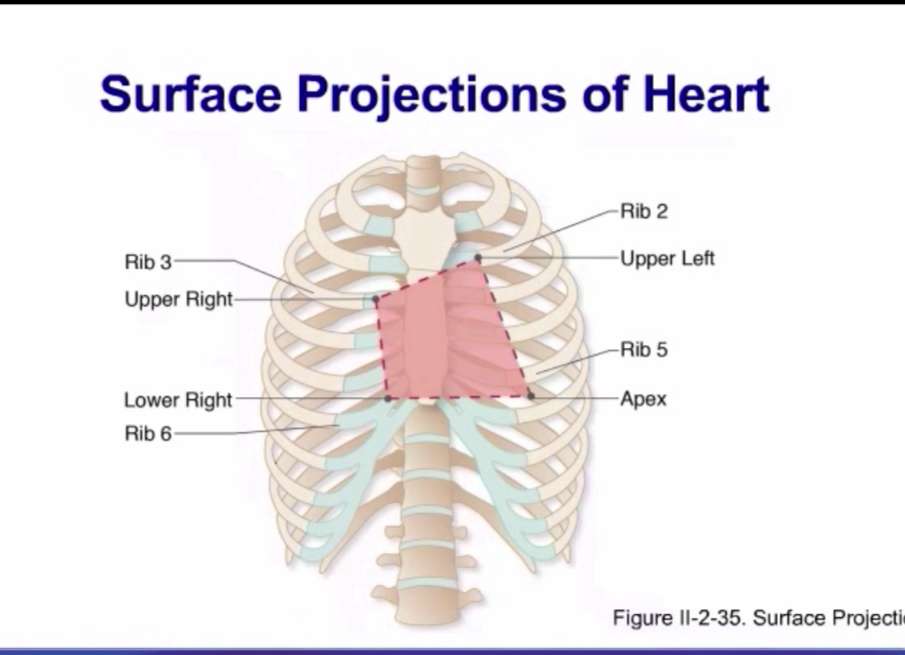
Heart chambers projections on the chest wall
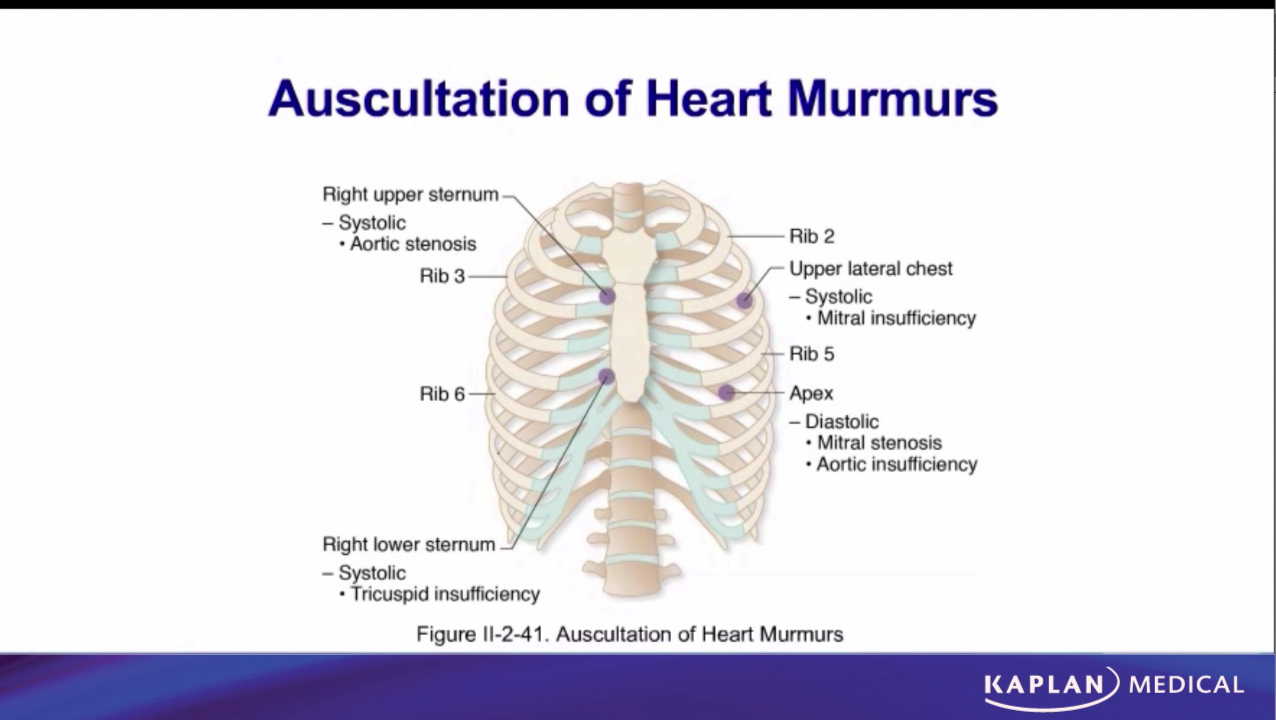
Murmurs projections
+tricuspidal stenosis - 5 intercostal space on the left
dyastolic murmurs - tricuspial, mitral stenosis + aortic and pulmonary valves insufficiency
systoic murmurs - tricuspial, mitral insufficiency+ aortic and pulmonary valves stenosis
Projections of the normal heart sounds
Embryology tissue of the heart
splanchnic mesoderma 3,5-4 weeks of development + migration of the neural crest cells - heart tube (truncus arteriosus, bulbus cordis, primitive ventricle, primitive atrium, sinus venosus)
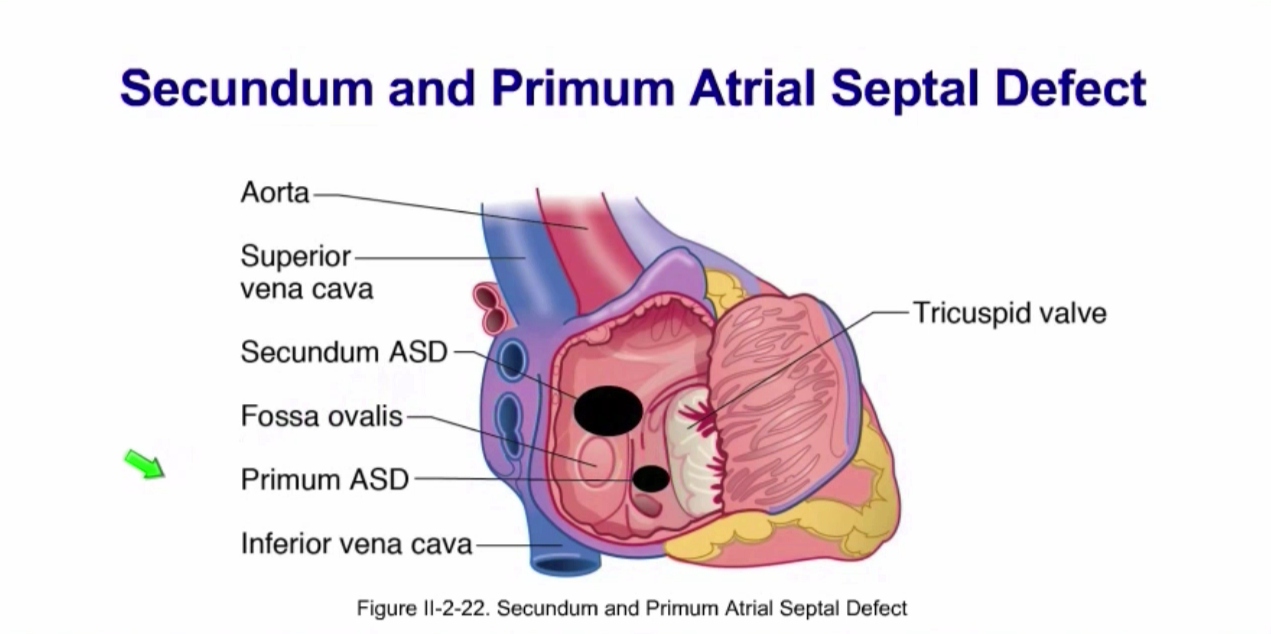
Types of the atrial septum defects
Primum ASD (less common, endocardial cushion defect, might be associated with atrioventricular septum defect (membranosus part) and defect of the atrioventriculat valves)
Secundum (more common, excessive apoptosis)
If too sever might evolve into Eisenmenger complex (pulmonary hypertension + right to left shunts). The same is with the ventricular septal defect.
3 cyanotic congenital heart abnormalities (aorticopulmonary septum defects)
Truncus arteriosus (no APS)
Tetralogy of Fallot ( APS more on the right side)
Transposition of great vessels (does not goes spiral)
Compliance
C=V/P, mostly for venosus system
Wall tension (LaPlace relationship)
T is directly proportional to Pr (pressure, radius)
Aortic aneurysm (due to high velocity) increase wall tension - might burst
Dilated heart failure - increased wall tension
Systolic performance (pressurises and ejects) is determined by?
Preload
Contractility
Afterload
Preload
Load or prestretch on ventricular muscle at the end of diastole.
LV preload - LVEDV (60-110 ml/m2), LVEDP (3-12 mmHg) (Directly measured in the ventricle ); CVP (4-12 cmH2O/3-8 mmHg), PCWP (estimates left atrial pressure) (4-12 mmHg), RAP (2-6 mmHg) ( measured in the venous system)
Contractility and heart rate effects on the heart
Systolic interval decreased: contractility effect
Diastolic interval decreased: heart rate effect
Afterload is increased?
Aortic pressure is increased
SVR is increased
Aortic stenosis
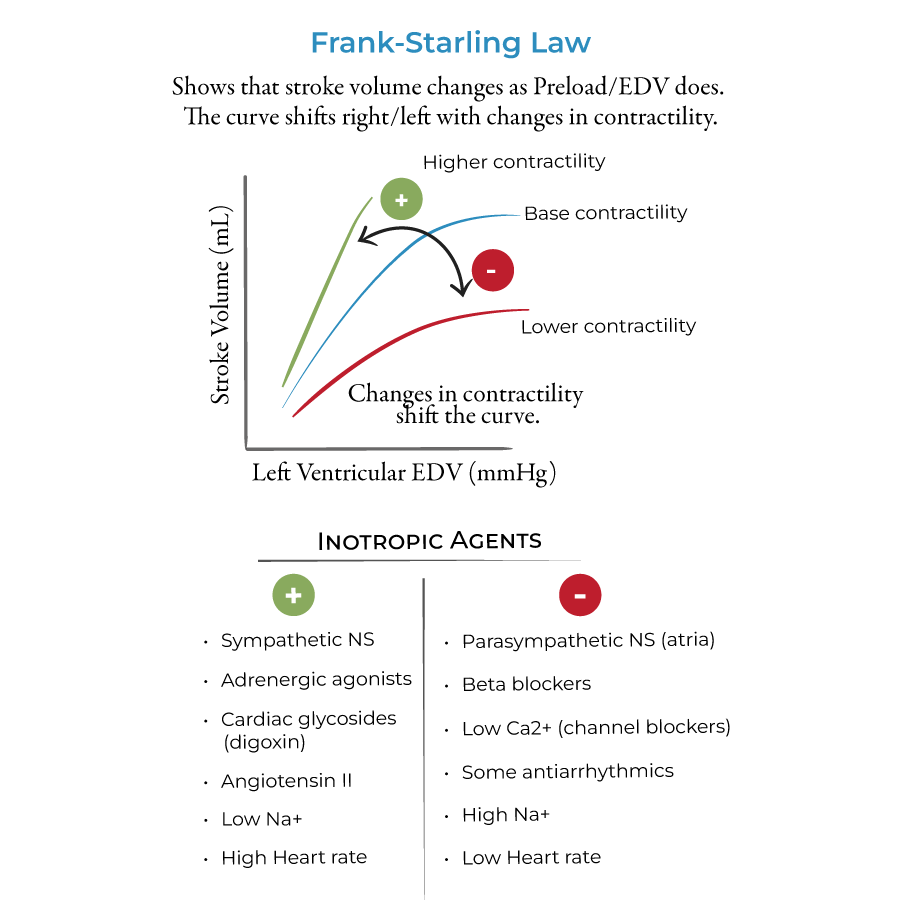
Frank-Starling curve
Rise in ventricular performance as preload increases
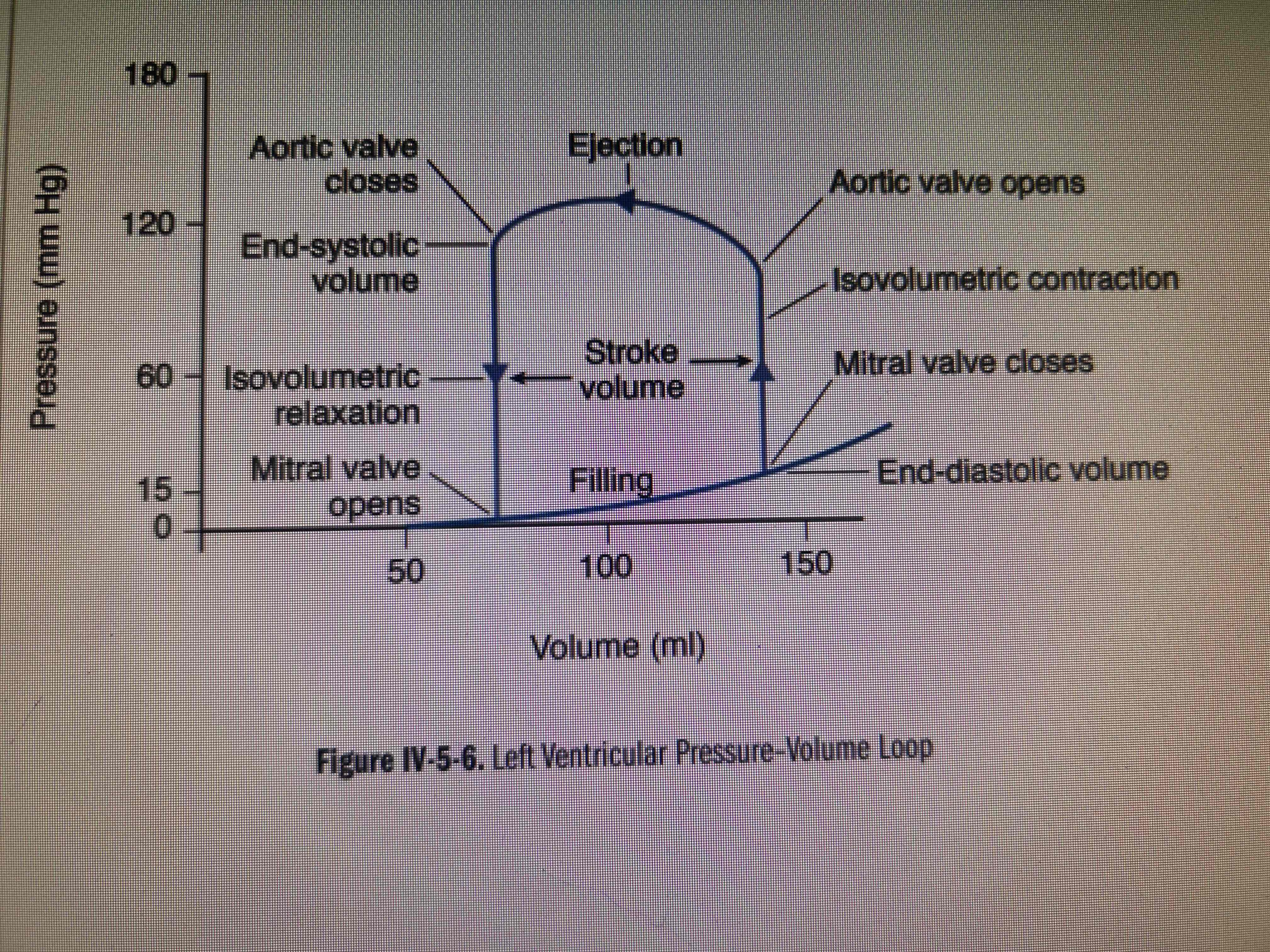
Ventricular volumes
End-diastolic volume
End-systolic volume
Stroke volume = EDV - ESV
Ejection fraction = SV/EDV more than 55% in a normal heart
Pressure overload
Increased contractility, increased performance-normal CO(initially)
Chronically- concentric hypertrophy, increase in wall thickness.
Decreased compliance, diastolic dysfunction followed by systolic dysfunction
Volume overload
Well tolerated if developed slowly
Chronically- eccentric hypertrophy, compliance is not compromised, diastolic function is maintained
Systolic dysfunction
Cardiomyopathy
Dilated (diastolic function remains intact, increased sympathetic stimulation, systolic dysfunction, mitral and tricuspidal failure)
Restrictive - decreased ventricular compliance with diastolic dysfunction and a decrease in a ventricular cavity size (increased filling pressure, ventricular hypertrophy +-, systolic close to normal
Hypertrophic (septal or left ventricular hypertrophy is unrelated to a pressure overload, diastolic dysfunction due to muscle stiffness, HOCM. Сrescendo-decrescendo systolic murmur heard best at the apex
Factors that cause vasoconstriction
Norepinephrine (binds alpha-1-receptors to activate Gq (heterotrimeric G protein alpha, activate beta-type phosholipase C-release Ca into cytoplasm, activate protein kinase C)- vasoconstriction, releases from sympathetic postganglionic neurons.
Epinephrine released from the adrenal medulla activates alpha-1-receptors.
Angiotensin 2 via the AT1 receptor (Gq)
Arginine vasopressin (AVP, ADH) via the V1 receptor (Gq).
Vasodilation mechanisms
Decreased sympathetic activity
NO released from the vascular endothelium
Adenosine, CO2, K+, H+
EPI stimulates vascular beta-2-receptors (Gs-cAMP)
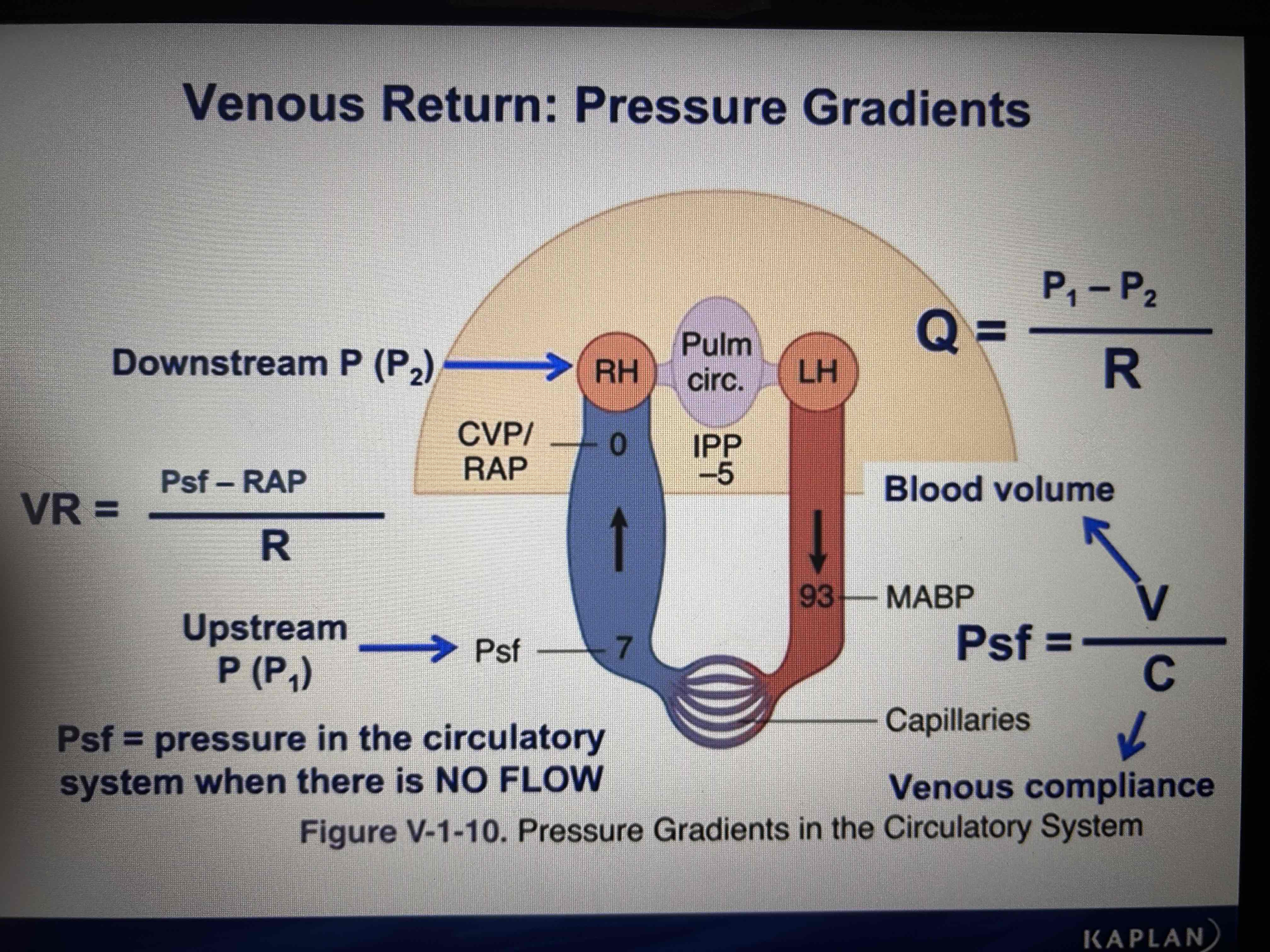
Venous return
Determines preload
Pressure flow resistance
RAP is downstream pressure for VR, mean systemic filling pressure (Psf) - upstream pressure
Increase in blood volume increases Psf and VR
Decrease in blood volume decreases Psf and VR
Decrease in venous compliance (sympathetic stimulation, muscle pump) increases Psf and VR
Increase in compliance (sympathetic inhibitions, venodilators, alpha block) decreases Psf and VR
Determinants of the CO
HR
Contractility
Afterload
Preload
CO
CO=HR*SV
High HR decreases filling time for the ventricles - can decrease SV
Exercise - sympathetic activation: decreases systolic intervals, increases contractility, venoconstrict, increases conduction velocity, skeletal muscle pump - maintain SV.
Contractility
Direct relation between CO
Afterload to CO
Inverse relation between afterload and CO
Preload in CO
Direct relation between preload and CO
VR determines preload
CO/VR curve
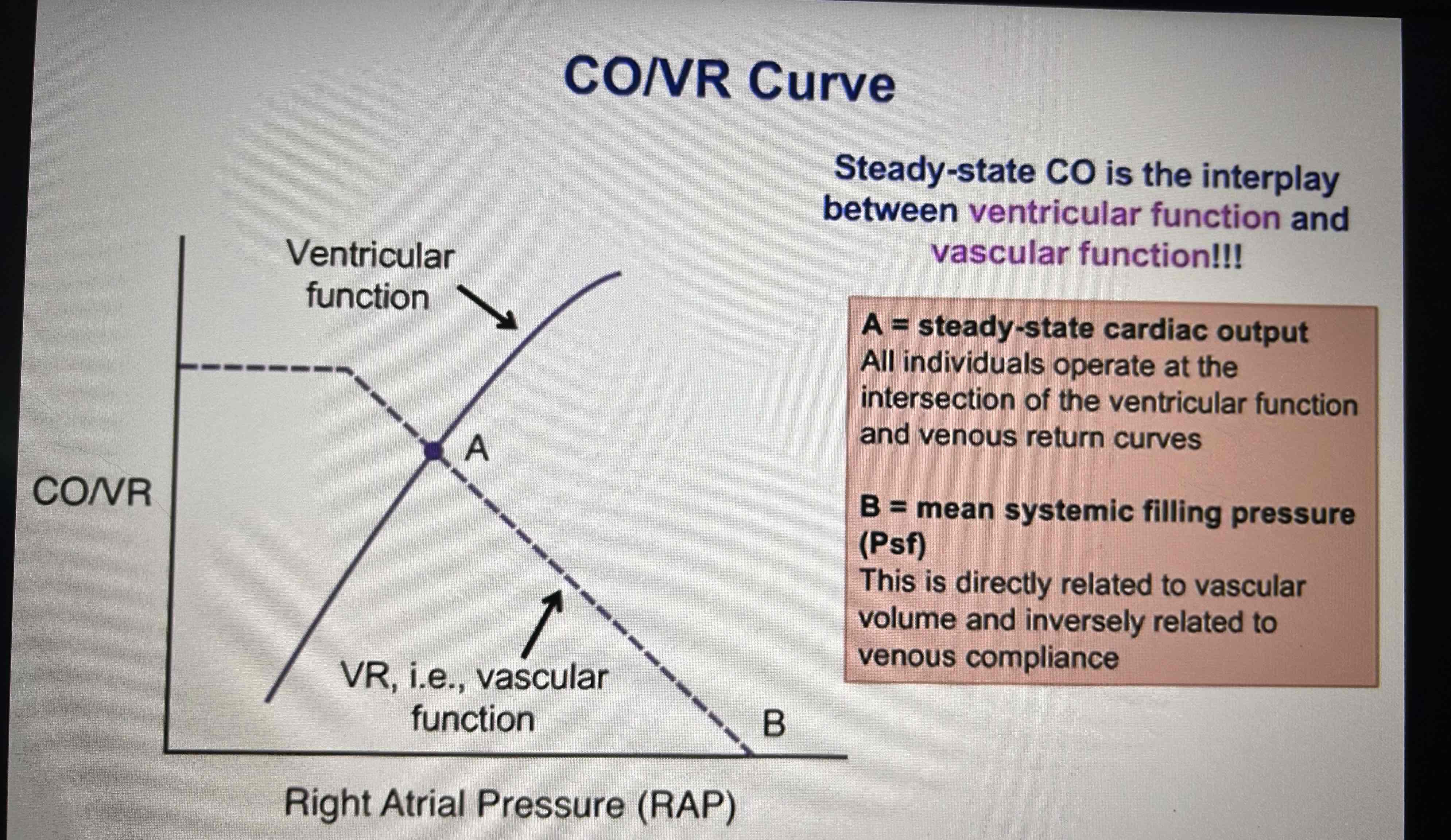
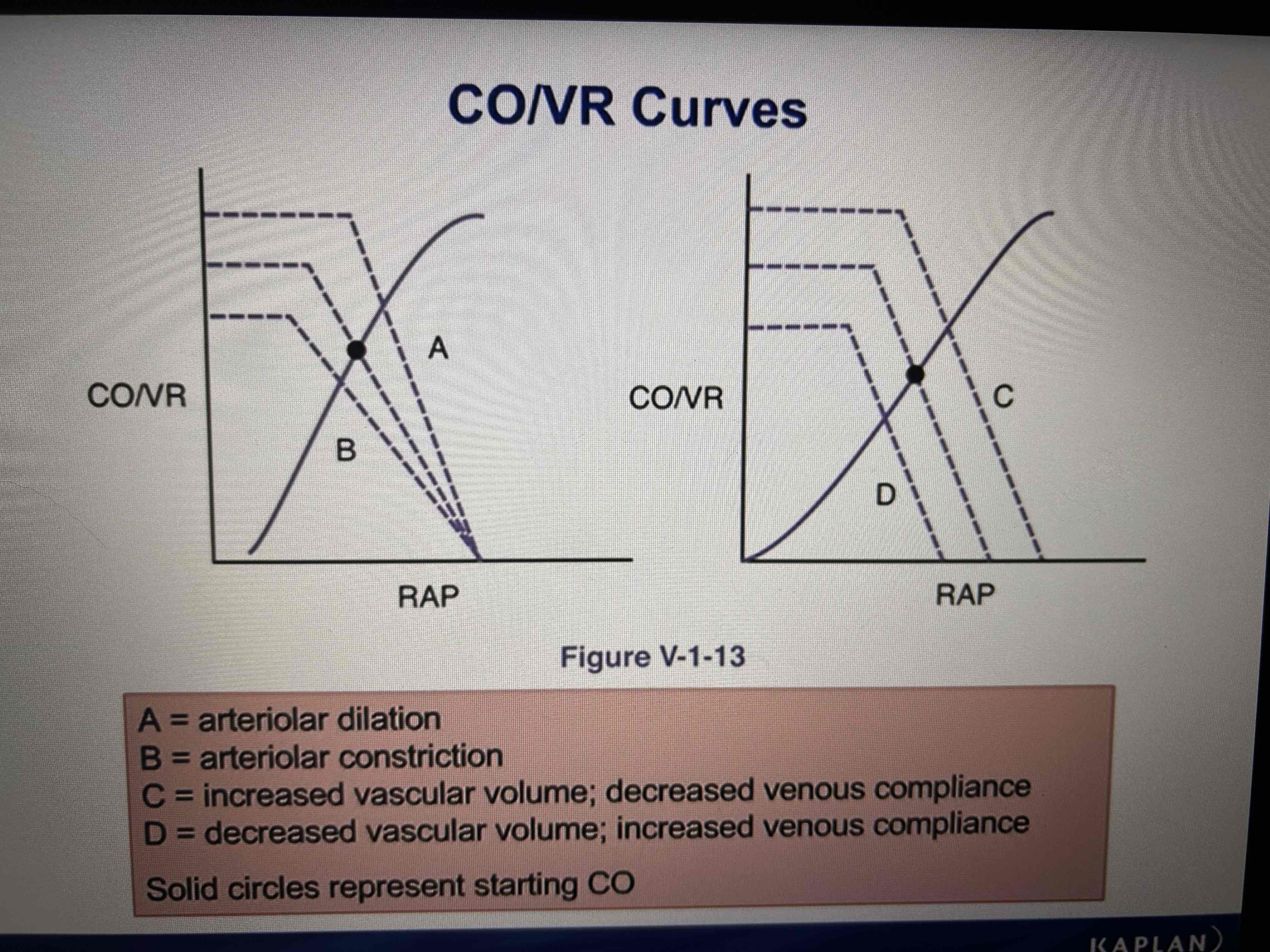
Resistance in CO
If arterioles vasodilate VR increases
Arteriolar vasodilation decrease afterload
If arterioles vasoconstrict VR falls, CO falls (F-S curve)
Arteriolar vasoconstriction increases afterload

Psf: increasing vascular volume
Increase vascular volume (infusion, RAAS) of decreasing venous compliance (sympathetic stimulation, muscle pump, exercise, lying down) increases Psf
Increases CO (F-S)
Psf: decreasing vascular volume
Decreasing vascular volume Haemorrhage, burn trauma, vomiting, diarrhea) or increasing venous compliance ( inhibit sympathetics, alpha block, venodilators, standing up right) decreases Psf
Reduce CO (F-S)
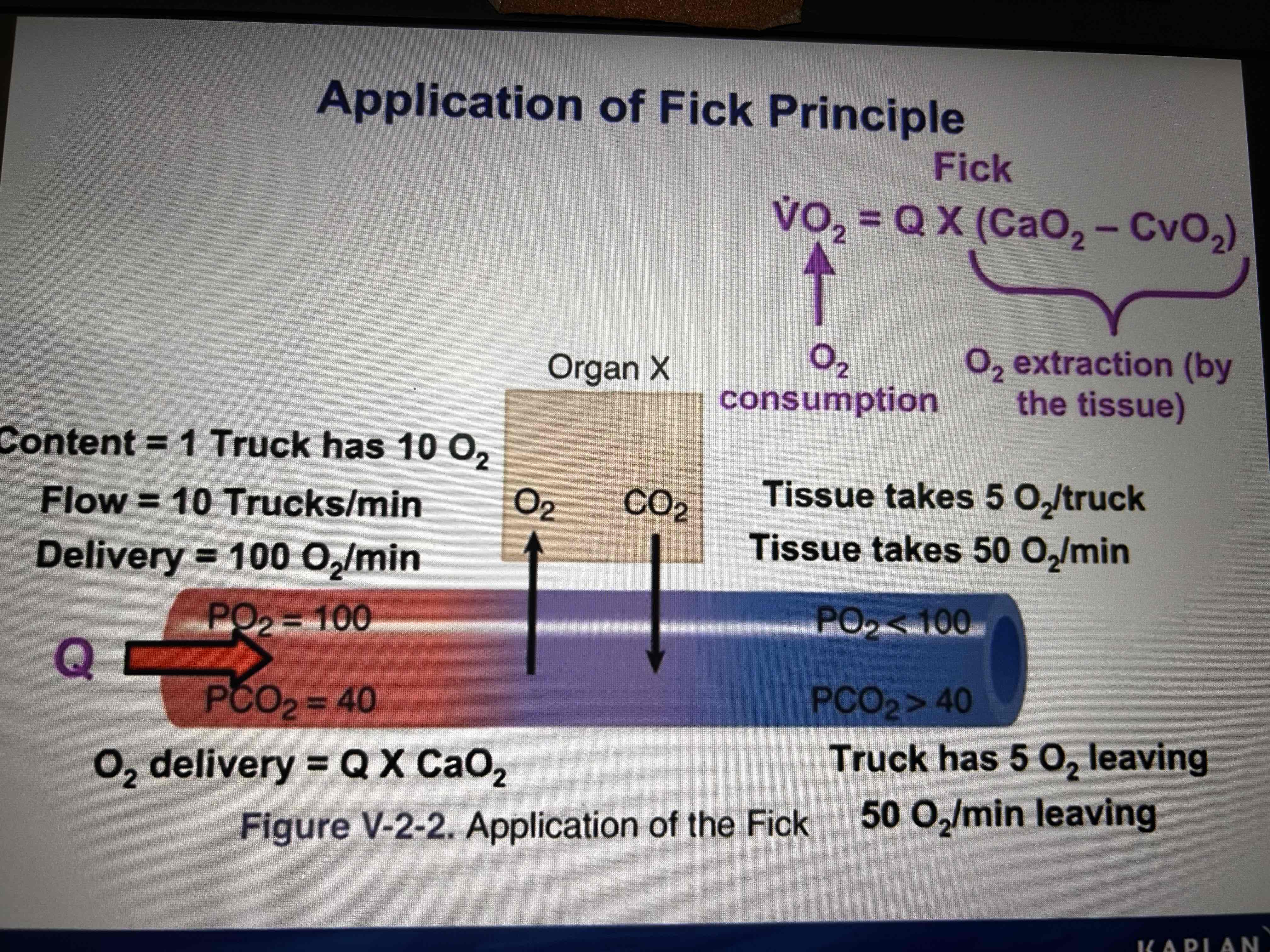
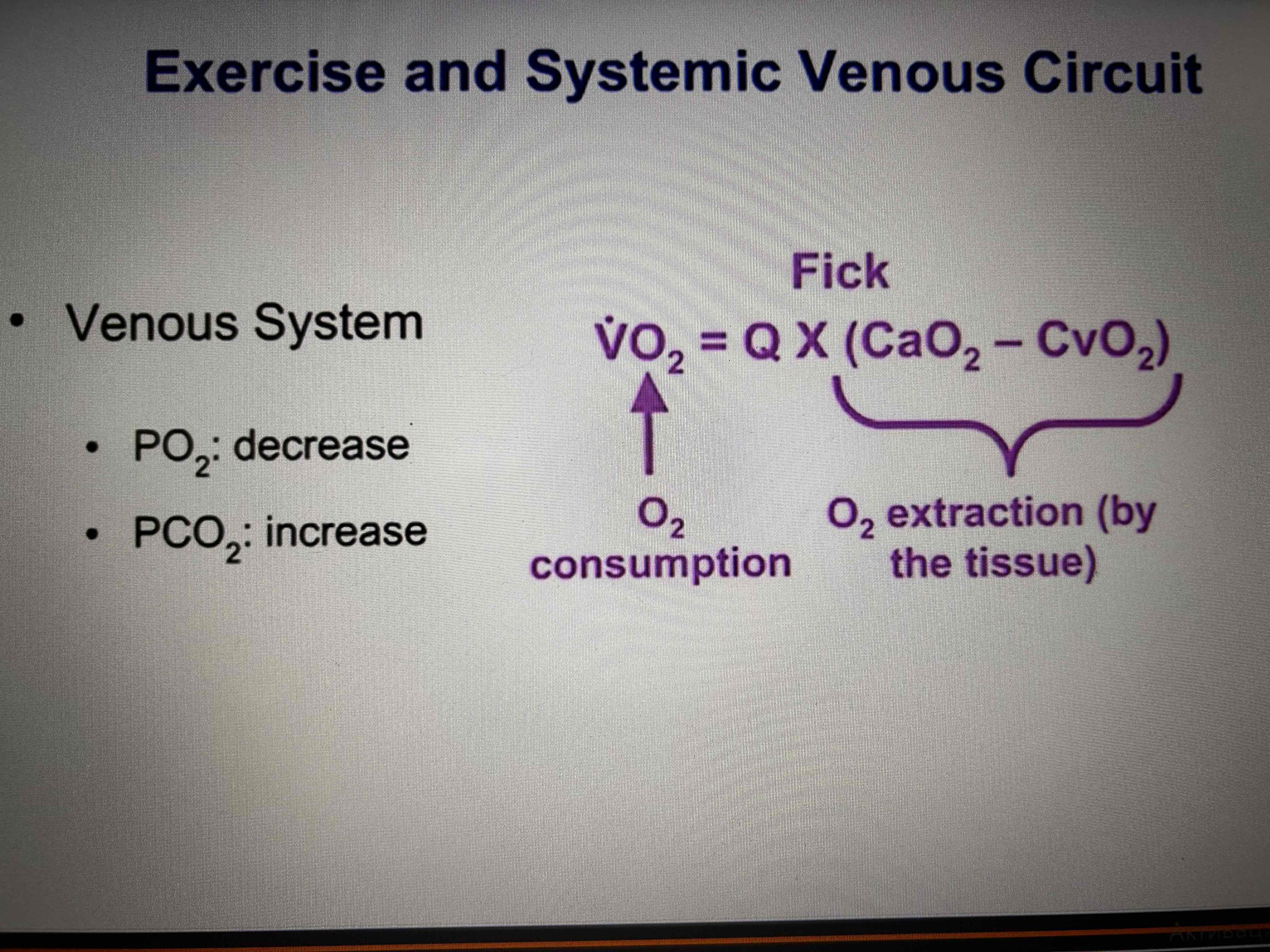
Fick principle of blood flow
Used to calculate blood flow
Flow=uptake (consumption)of oxygen/A-V (oxygen content difference across the organ
Can calculate oxygen consumption (VO2)
VO2=CO*(CaO2 (total arterial oxygen content )-CvO2 (total venous oxygen content))
Pulmonary venous O2 content - 0,2 ml O2 per ml blood
For any given O2 consumption, a decrease in delivery results in increased lactic acid production and possible hypoxia damage, decrease in the amount of the venous O2
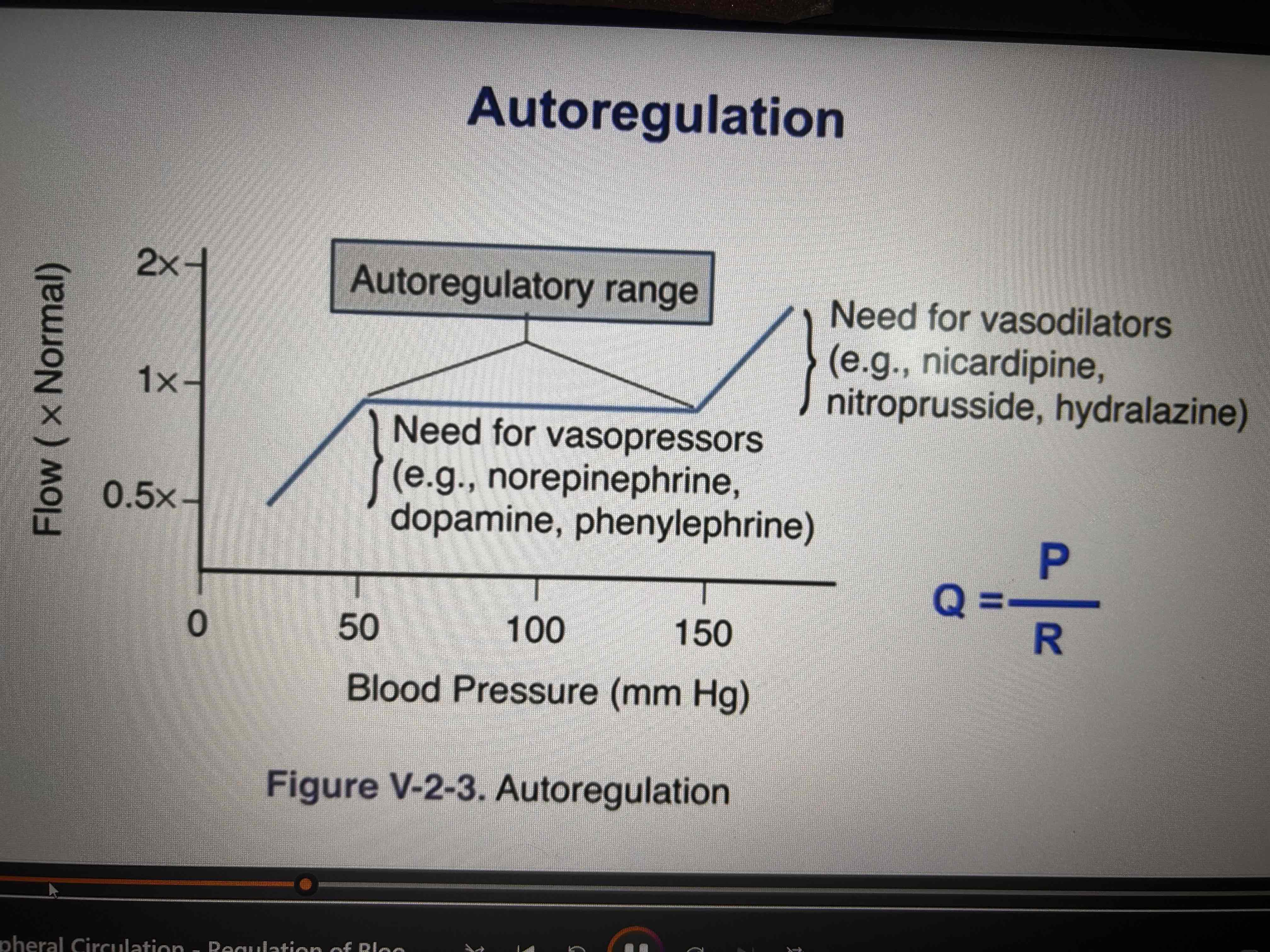
Intrinsic blood flow regulation
Metabolic mechanism (flow is regulated by constricting and dilating smooth muscle around arterioles)
tissue produces a vasodilators metabolite that regulates flow (K, H, CO2, adenosine) - dilation of arteriolew when concentration increases and vice versa
Myogenic mechanism
arteriolar stretch and surrounding muscles ( change in pressure)
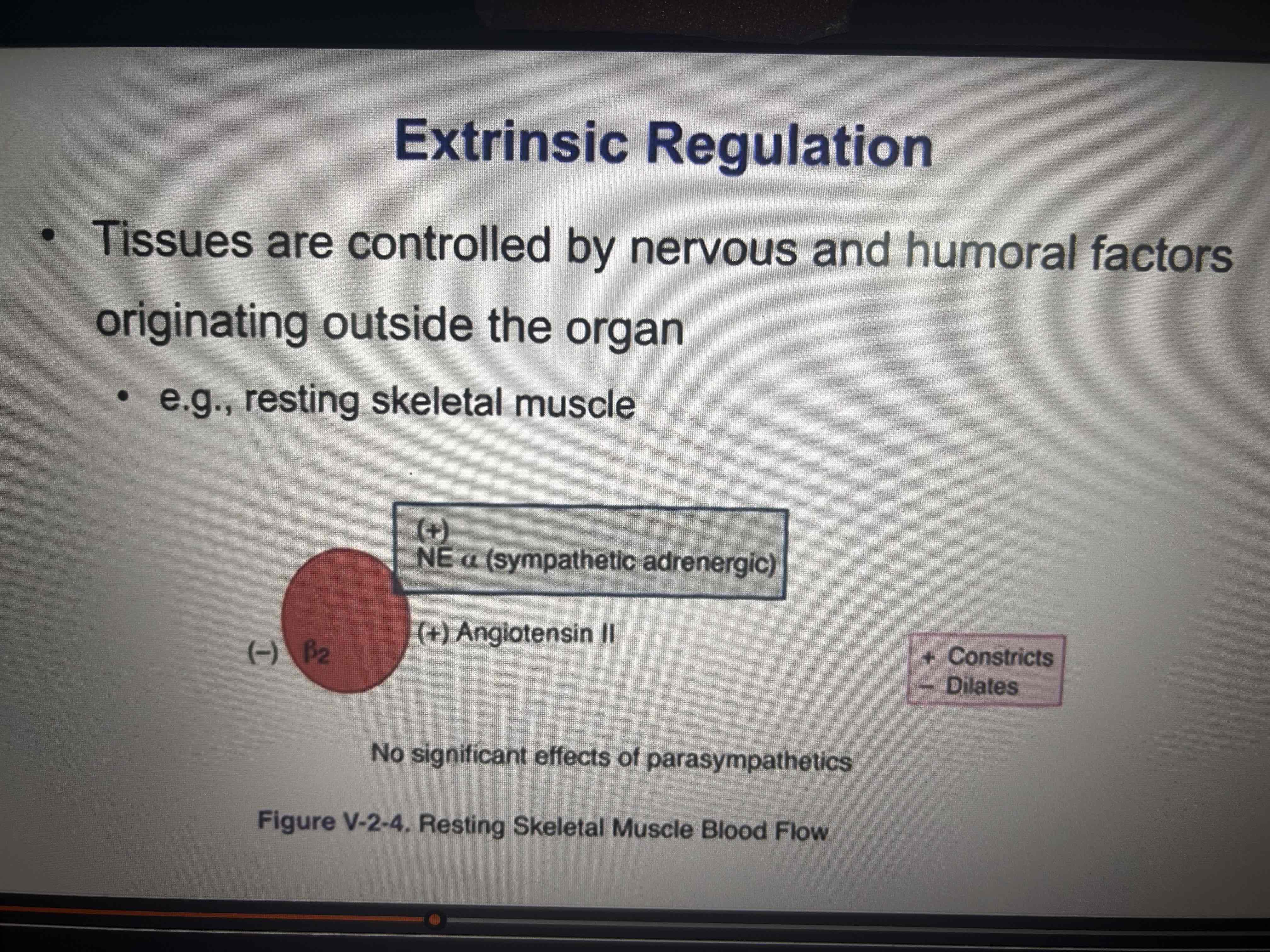
Extrinsic regulation
EPI can cause vasodilation via B2 receptors
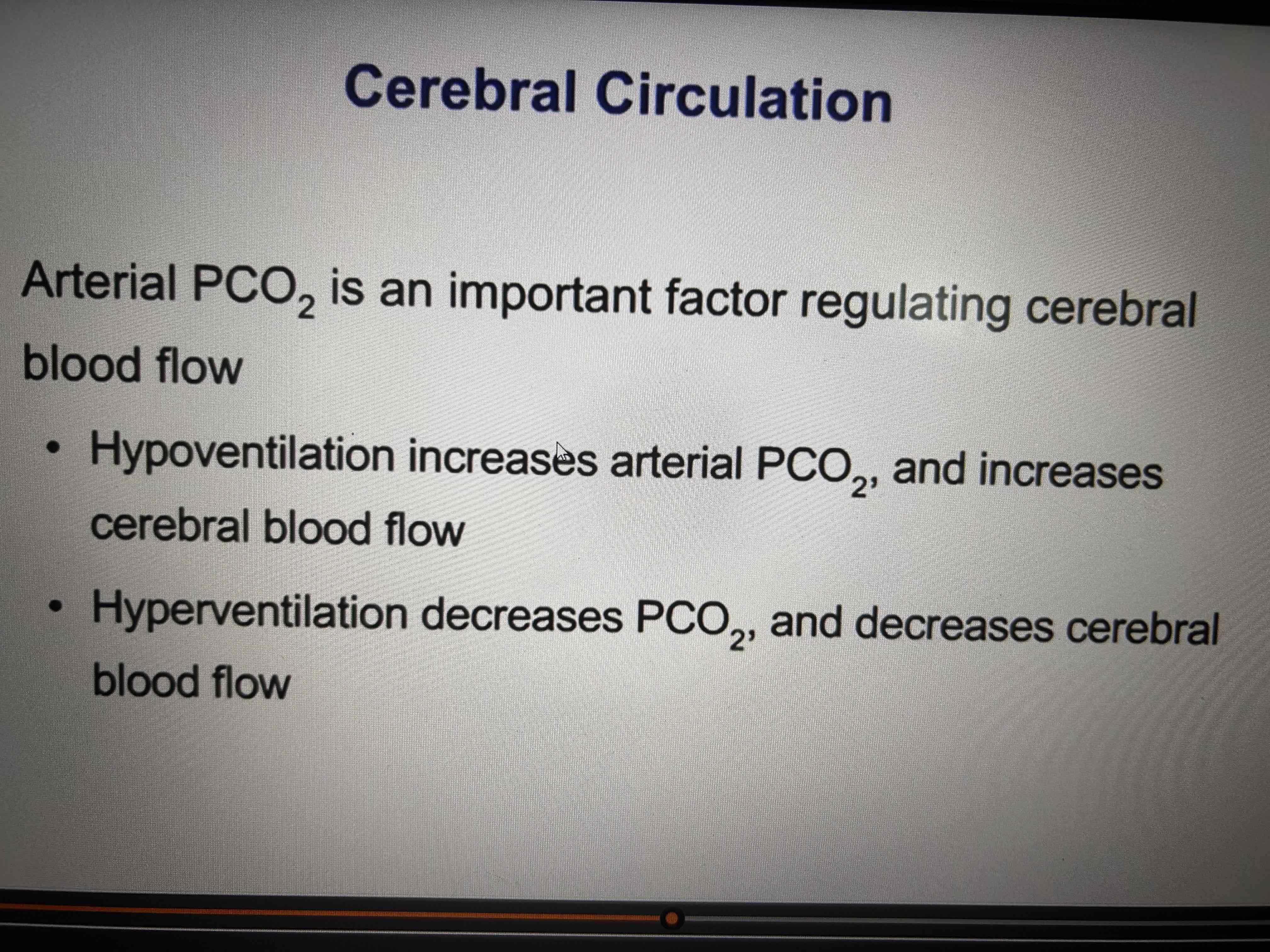
Cerebral circulation
If arterial PO2 is normal or above cerebral blood flow is regulated via arterial PCO2
A large decrease in arterial O2 increases cererbal flow (high attitude pulmonary edema)
Baroreceptors don’t affect flow
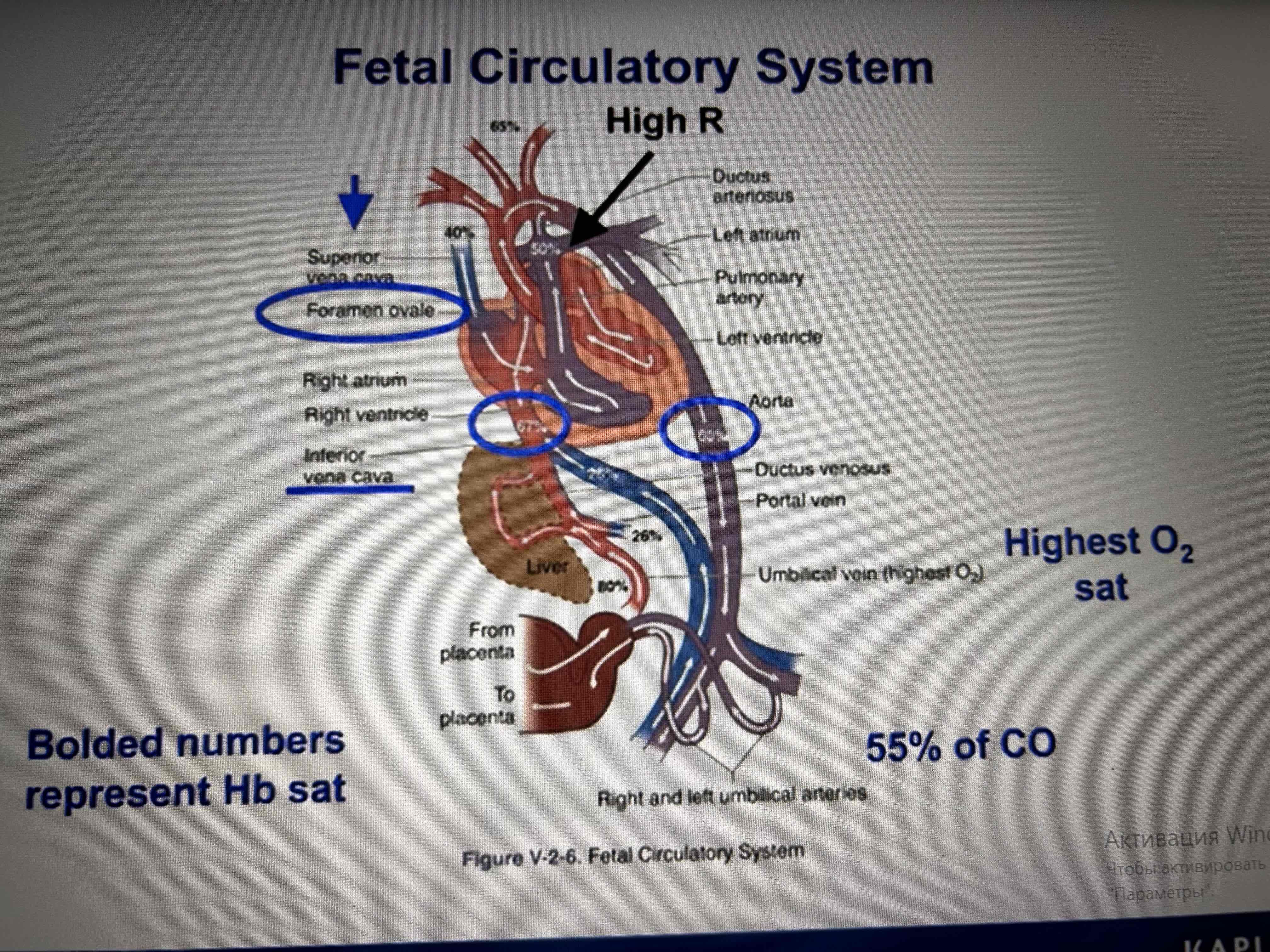
Fetal circulation system
55% of CO goes to the umbilical cord, highest O2
Fetal Hb has a very hight affinity to O2
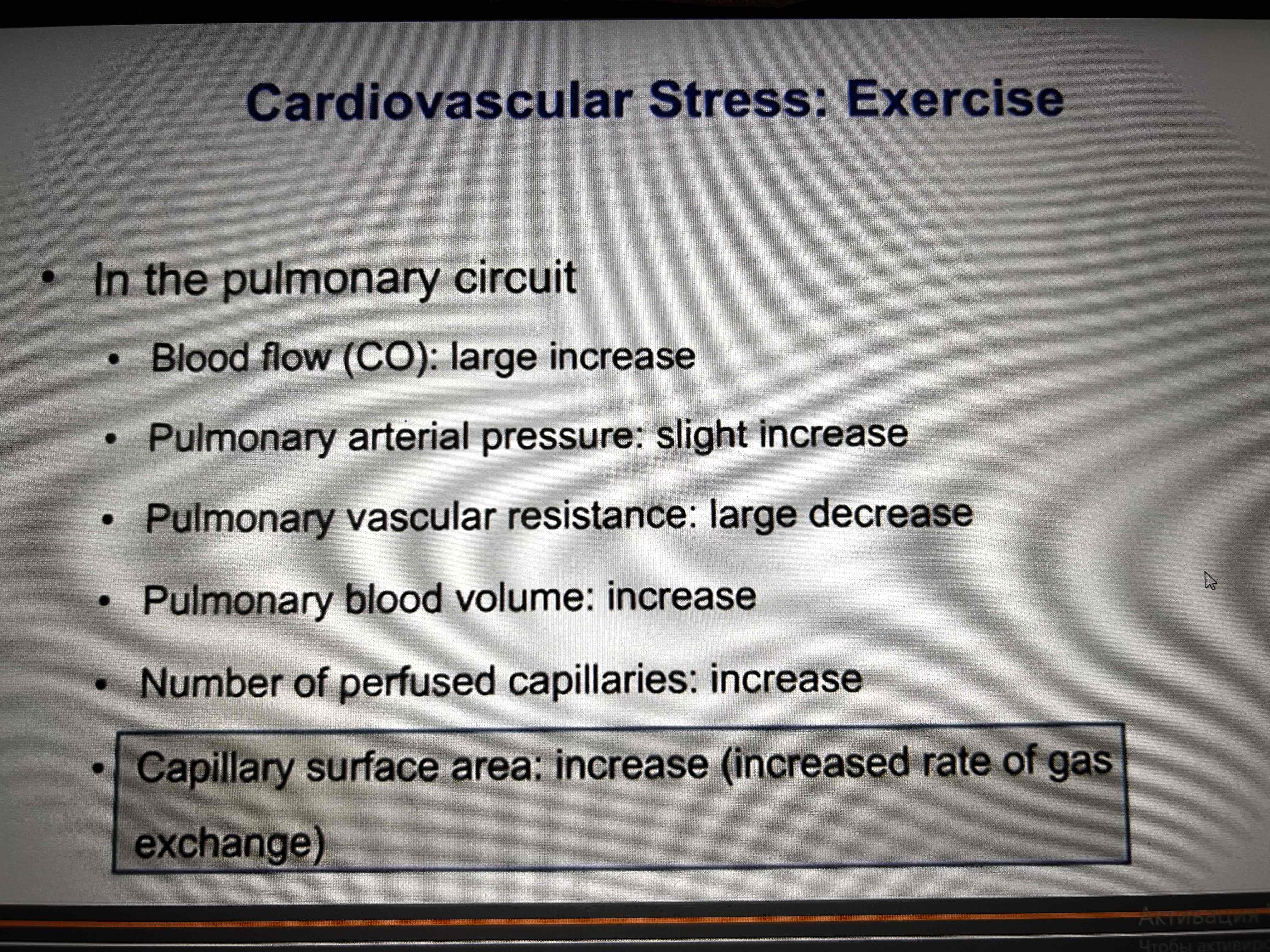
CVS stress: exercise
In the arterial system:
PO2 normal, Hb fully saturated
PCO2 normal
Oh stable or decrease due to production of lactic acid
MAP slight increase
Temperature slight increase
TPR large decrease, dilation of the skeletal muscle
Exercise and systemic venous circulation
Normal cardiac cycle
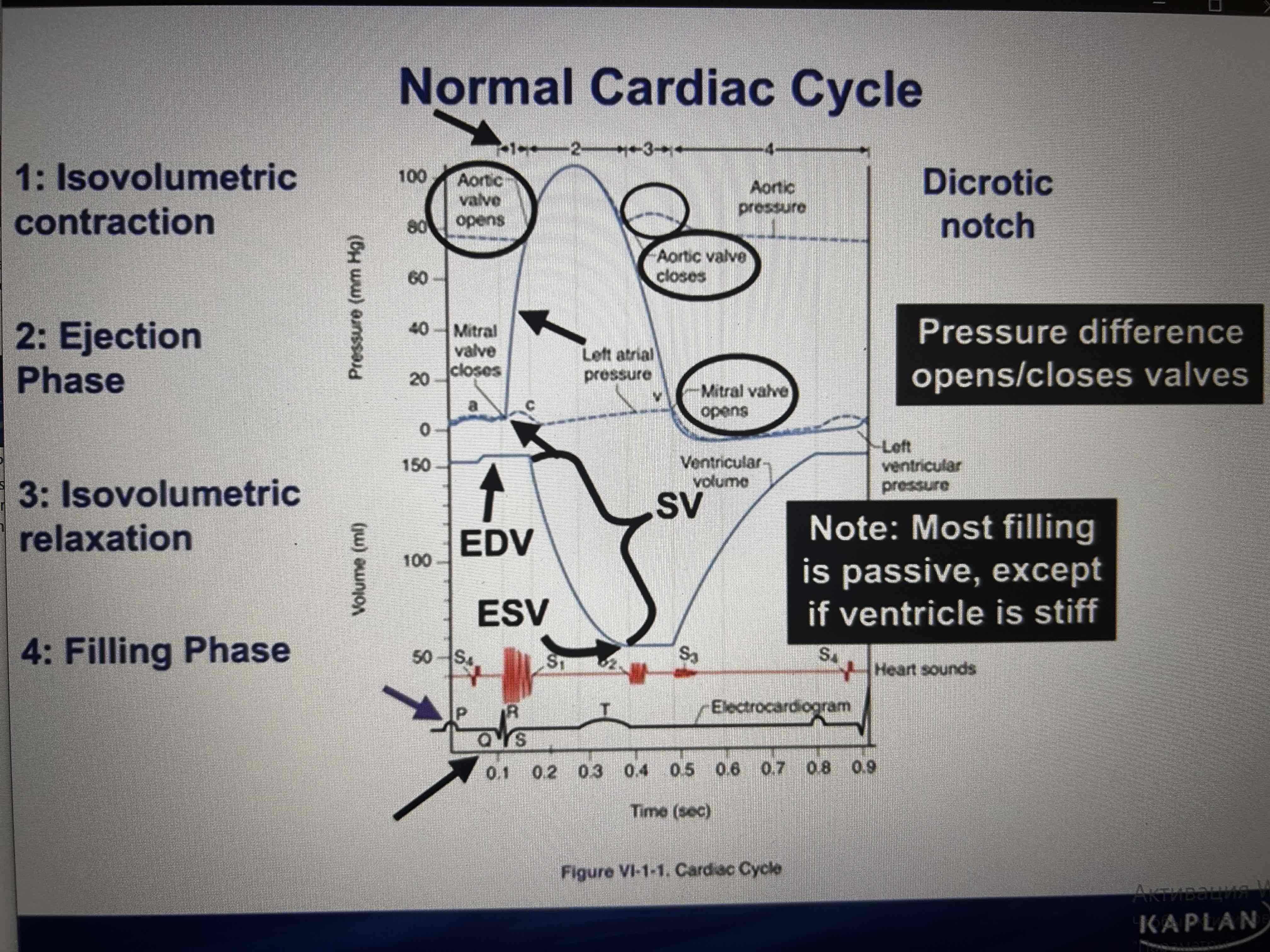
Heart sounds
S1-mitral and tricuspid valves closure
S2- closure of the aortic and pulmonic valves ( during inspiration-physiological splitting, right heart delayed)
Heart sounds
S3-After opening of the AV valves during rapid filling of ventricle. Normal in kids. Pathological - volume overload.
S4 - atrium contracts against a stiff ventricle ( concentric hypertrophy, aortic stenosis, MI)
Auscultation
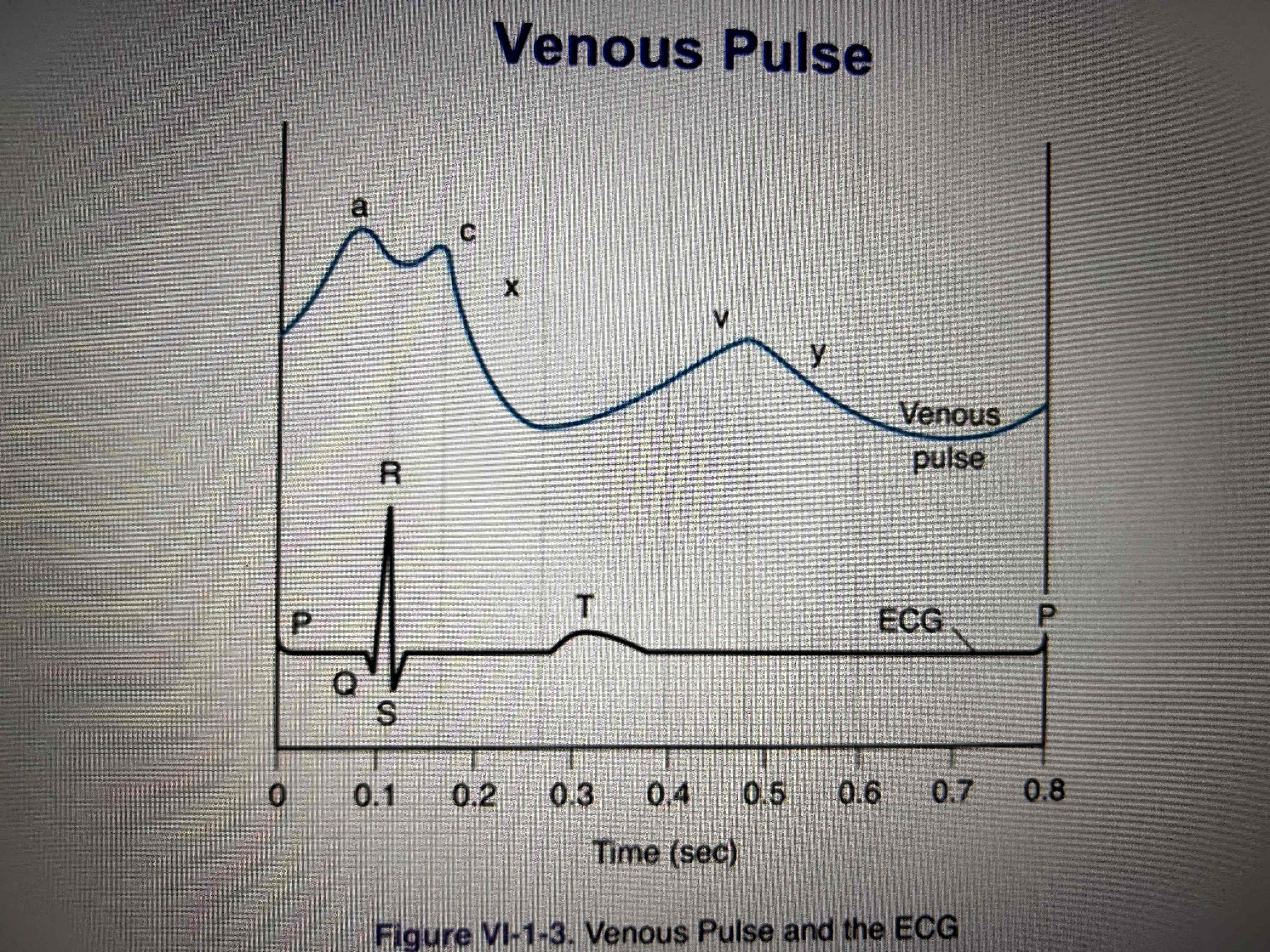
Venous pulse
a-atrial systole
c-bulging of the tricuspid valve
x-atrial diastole
v-venous return during systole of the ventricle
y-opening of the tricuspid valve
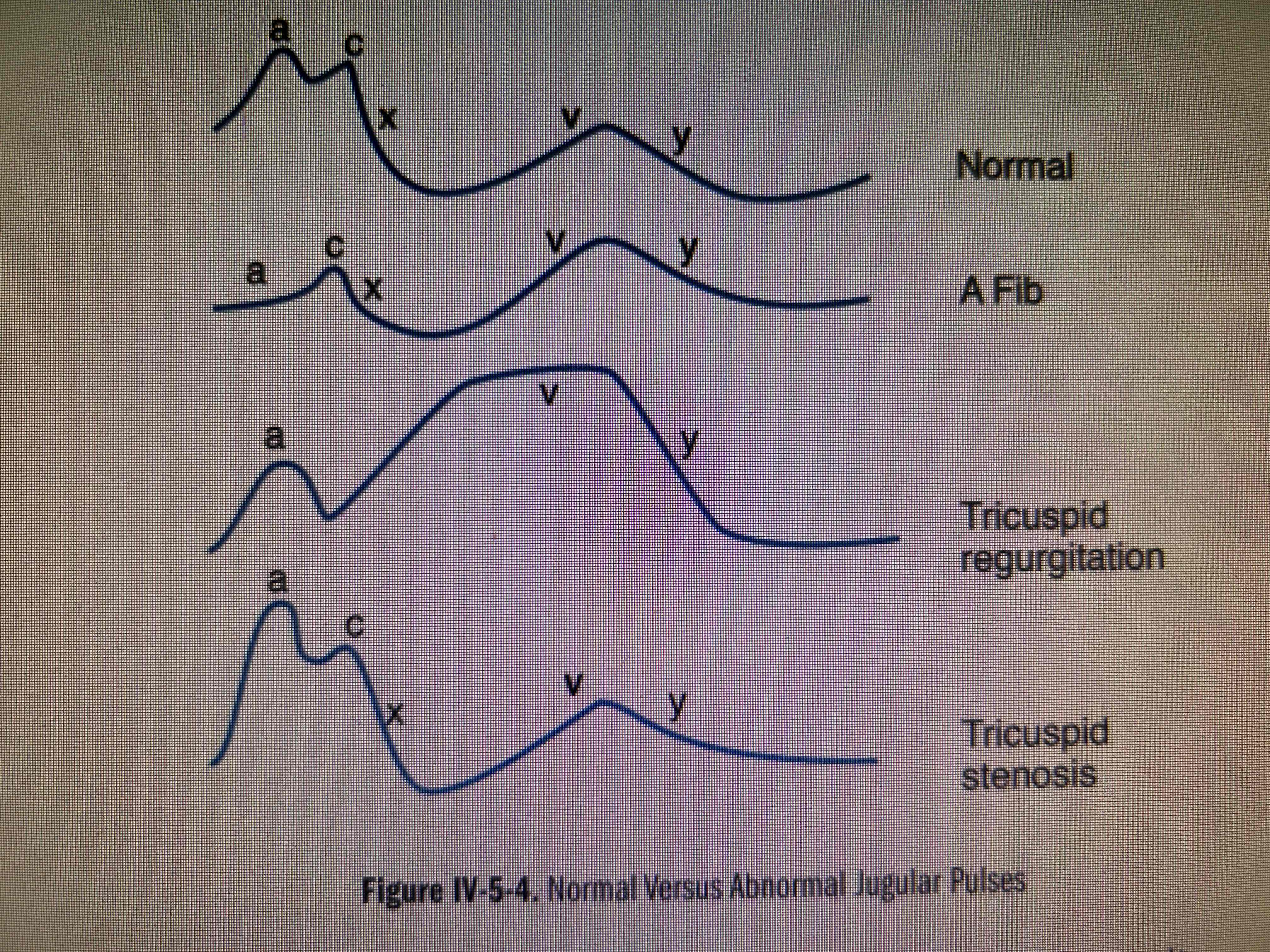
Abnormal venous pulses
Pressure-volume loops
S3 heart tone
Volume overload, appears in diastole due to high ventricle compliance, can be heard at children, pregnant women in normal, in pathology indicates heart failure due to volume overload (severe regurgitation, VSD). Gallop rhythm.
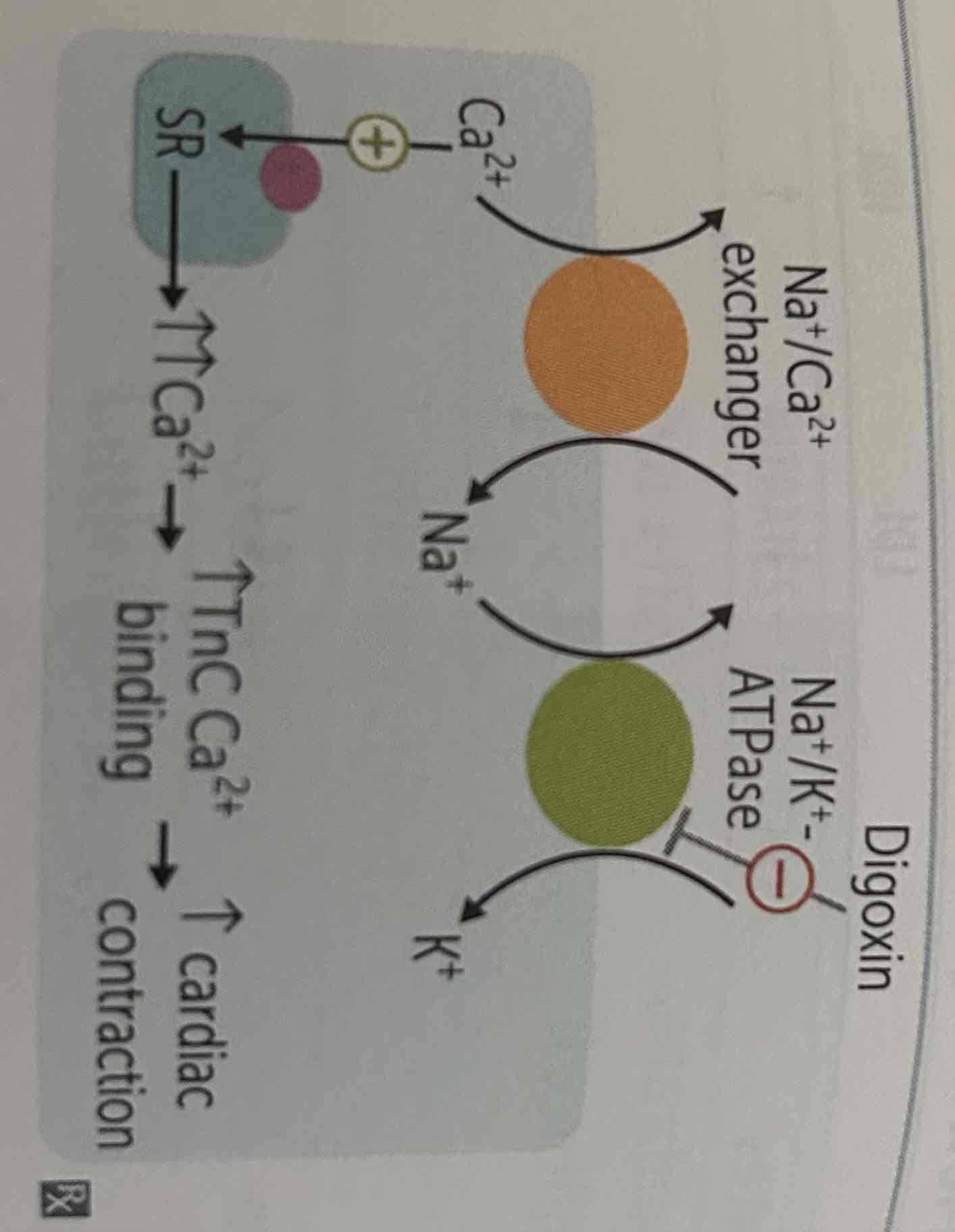
Digoxin
Na/K ATPase inhibitor - increases contractility
Adverse effects: hyperkalemia, nausea, vomiting, diarrhoea, blurry yellow vision, arrhythmias, AV block
Hydralazine
Increases cGMP-smooth muscle relaxation ( arterioles vasodilation is more the veins - afterload reduction). Prevents oxidation of nitric oxide and thereby lowering systemic vascular resistance and mean arterial pressure.
Can be used in pregnant women (sever hypertension, HF), can be administered with B-blockers to prevent reflex tachycardia
Side effects- tachycardia, agina, drug-induced lupus(+procainamide, isoniazide, methyldopa)
Alpha receptors
There are two types of alpha-adrenergic receptors; alpha-1 and alpha-2. Both are G-protein coupled receptors (GPCR); however, the downstream effects of the two are different. The alpha-1 receptor is of the Gq type, resulting in activation of phospholipase C, increasing IP3 and DAG, and ultimately increasing the intracellular calcium concentrations leading to smooth muscle contraction and glycogenolysis.The alpha-2 receptor acts as an allosteric inhibitor through Gi function, leading to an inhibition of adenylyl cyclase, decreasing the formation of intracellular cAMP. It also leads to a reduced amount of cytoplasmic calcium, which decreases neurotransmitter release and central vasodilation.Epinephrine and norepinephrine have relatively equal affinities for both types of alpha-receptors, with other drugs used in shock having a higher selectivity for the alpha-1 receptor.
Mitral stenosis murmur
Mid-diastolic rumble with an opening snap at the apex, loud S1. Better heard at the apex.
Beta-receptors
1- fat, heart, kidney ( raise contractility, heart rate, conduction)
2-arterial and bronchus smooth muscle (relaxation)
Equilibrium potentials of important ions
K-95mV
Na+70mV
Cl-76mV
Ca+125mV
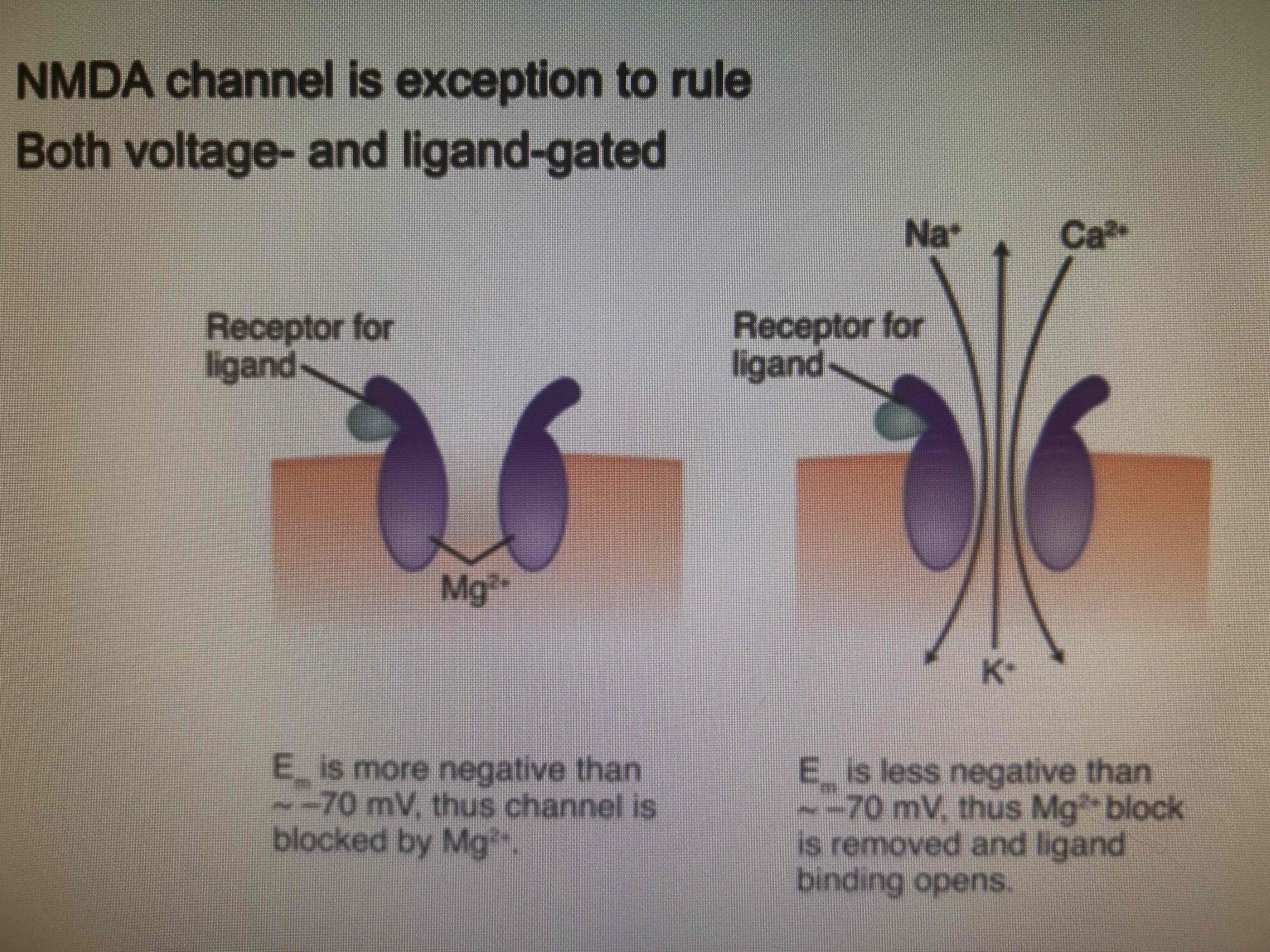
The only receptor both voltage and ligand-gated
NMDA
Ligands-aspartate and glutamate
Memory and pain transmission
Pulmonary regurgitation murmur
Diastolic, decrescendo murmur best heard at the left second intercostal space, increasing with inspiration