Endocrine Pancreas, Hyperparathyroidism
1/24
Earn XP
Description and Tags
Flashcards to review key concepts from the Endocrine System lecture, focusing on diabetes mellitus, insulinoma, and hyperparathyroidism.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
25 Terms
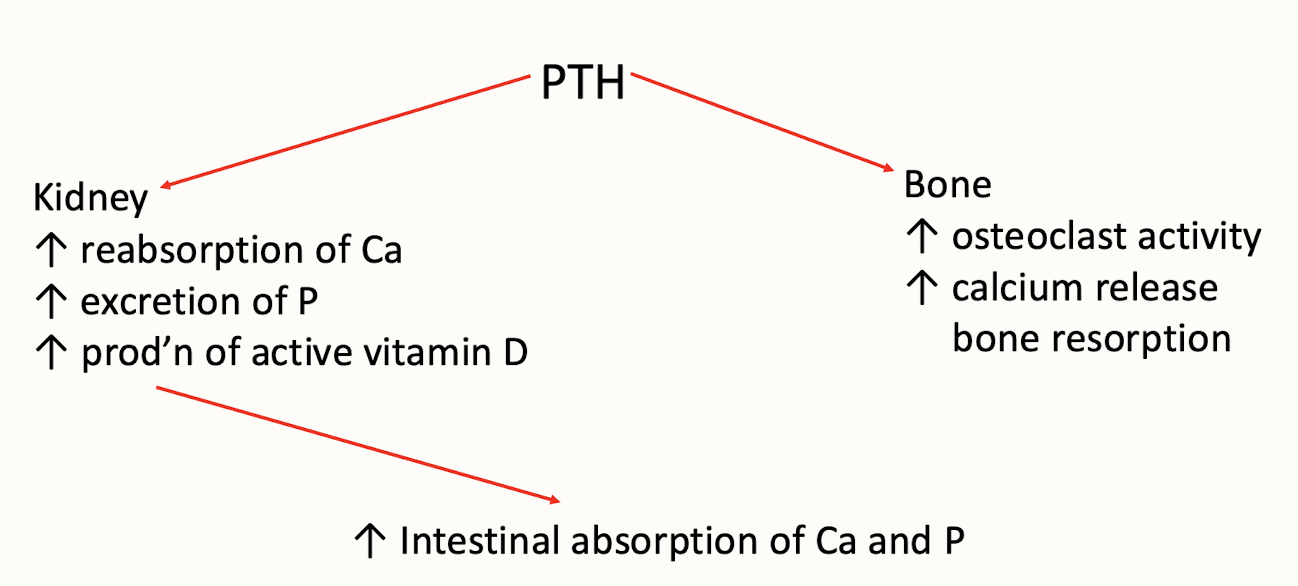
What is the primary function of parathyroid hormone (PTH)?
To maintain calcium balance in the body.
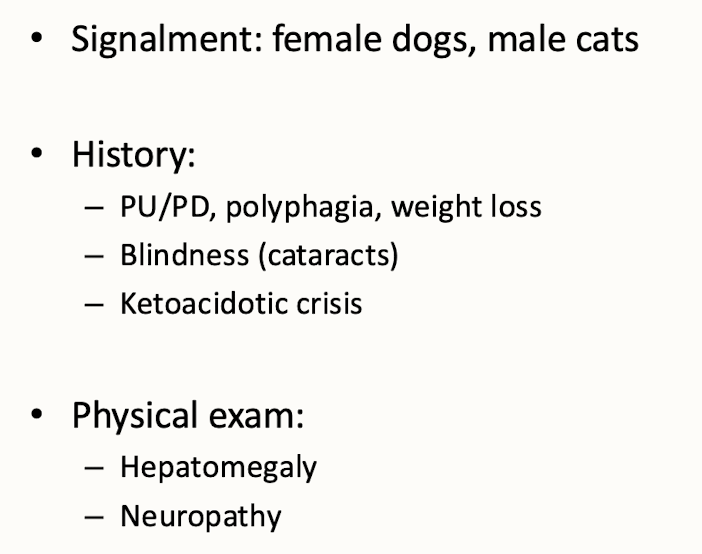
What notable conditions are associated with diabetes mellitus in dogs?
Type I diabetes, characterized by insulin dependence due to loss of β cells (genetics, immune mediated, pancreatitis, obesity)
Pancreatic islet
alpha cell = glucagon
b cell = insulin
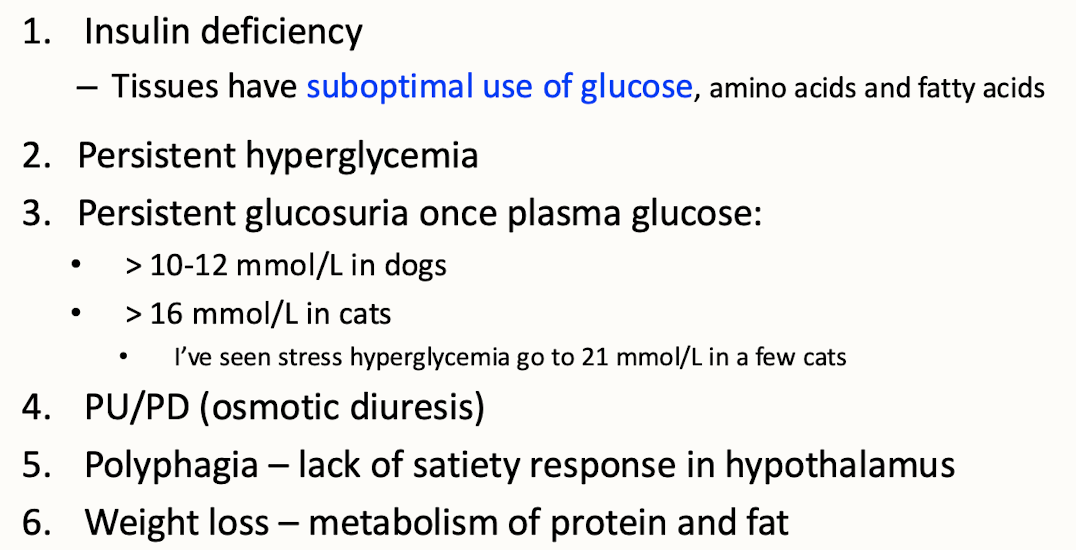
Pathophysiology of insulin dependent diabetes mellitus
Insulin dependent diabetes mellitus, also known as Type I diabetes, results from the autoimmune destruction of pancreatic β cells, leading to insufficient insulin production and persistent hyperglycemia.
Pathogenesis of type 2 diabetes mellitus in cats
Type 2 diabetes mellitus in cats is characterized by insulin resistance, often linked to obesity, leading to inadequate insulin secretion and resulting in hyperglycemia.
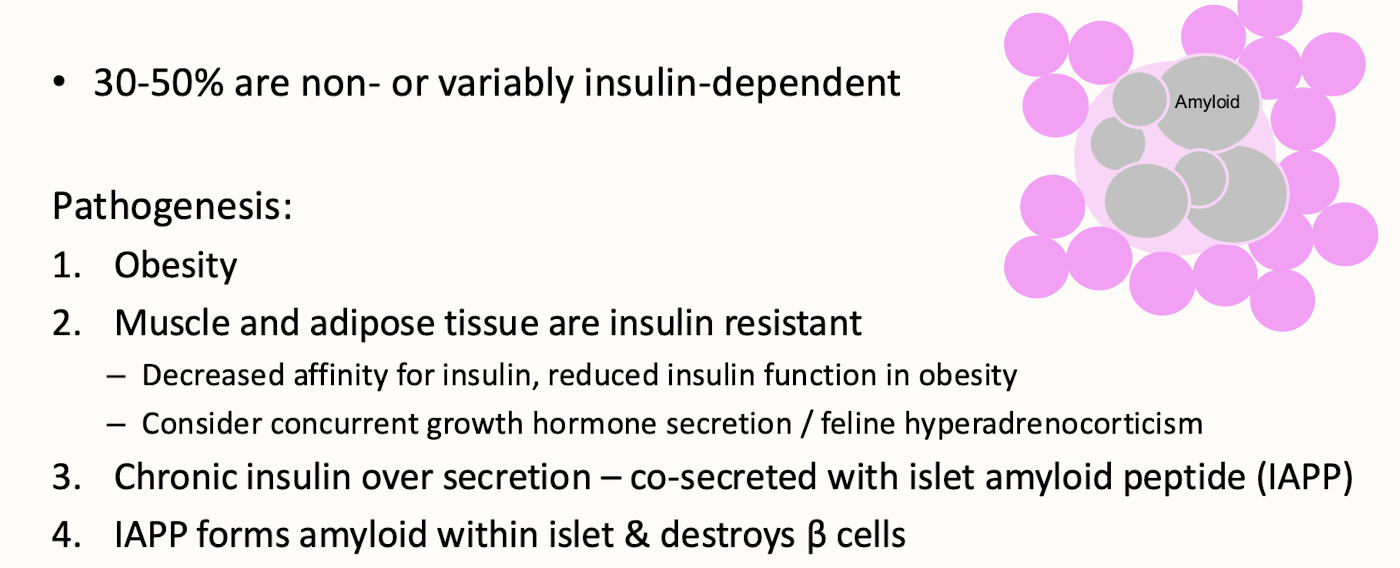
What are the characteristics of Type II diabetes mellitus in cats?
Insulin resistance primarily due to obesity and potentially concurrent hyperadrenocorticism.
Loss of B cell function → less insulin secreted
insulin receptor defective function
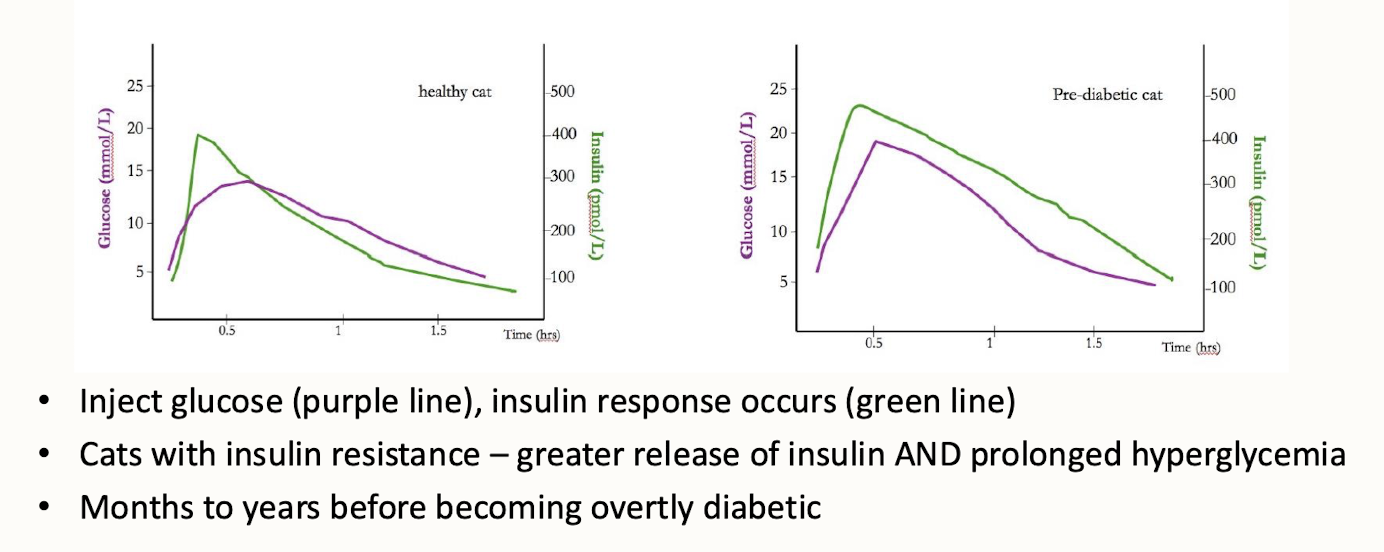
Subclinical aka pre-diabetic cats
are cats that show signs of insulin resistance without having overt diabetes. They often display increased blood glucose levels and may be at risk for developing diabetes if not managed appropriately.
What are common clinical signs of diabetes mellitus in animals?
PU/PD (polydipsia and polyuria), weight loss, and increased appetite (polyphagia).
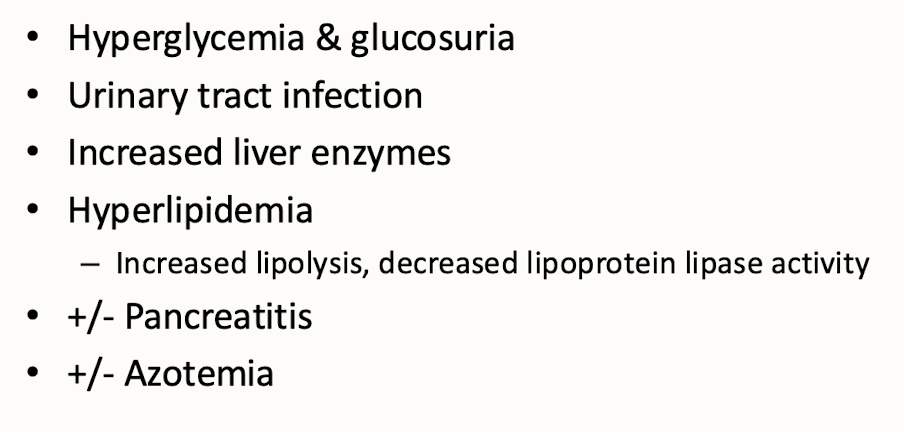
In diagnosing diabetes mellitus, what laboratory findings are important?
Hyperglycemia & glucosuria(stress), hyperadrenocorticism
IV glucose tolerance test
Glycated proteins
hyperglycemia, glucose likes to attach to proteins
serum fructosamine → mainly albumin
hemoglobin test for humans, not animals
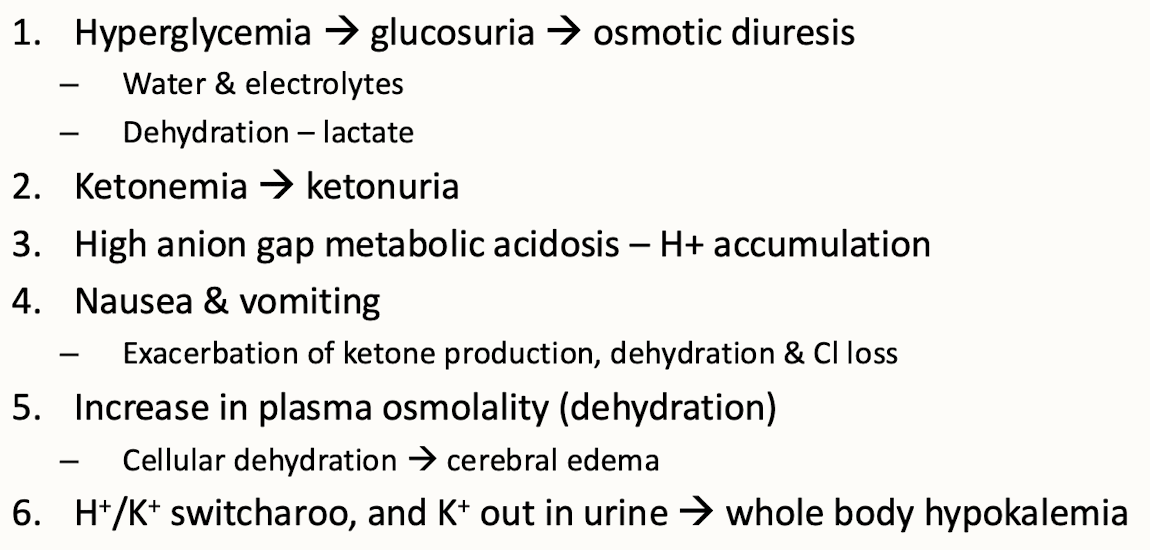
Pathophysiology of diabetic ketoacidosis
is a complex metabolic condition resulting from insulin deficiency and increased counter-regulatory hormones, leading to elevated ketone bodies and acidosis. It often occurs in diabetic patients during periods of stress, infection, or inadequate insulin administration
Acromegaly → hypersomatotropism
is a hormonal disorder resulting from excess growth hormone, often due to a pituitary tumor. This condition causes abnormal growth of bones and tissues, leading to features such as enlarged hands and feet → measure IGF
What is insulinoma and its effect on blood sugar levels?
A tumor of pancreatic β cells that produces insulin, leading to hypoglycemia → causes weakness/seizures
Diagnose insulinoma
typically involves measuring blood insulin levels during fasting and evaluating symptoms of fasting hypoglycemia <3.3 mmol/L
What are common differential diagnoses for hypoglycemia?
Portosystemic shunt (PSS), severe liver disease, hypoadrenocorticism, hepatic or intestinal tumors secreting hypoglycemic substances, and sepsis
What is hyperparathyroidism(not too common) characterized by?
Excess production of PTH leading to elevated calcium levels (hypercalcemia).
Consequences of hyperparathyroidism
Mineralization of kidney tubules, GI problems, weak bones, adenomas palpable more in cats than dogs
weakness, PU/PD
What are potential presentations of hyperparathyroidism in dogs?
Weakness, PU/PD, and signs of renal failure due to mineralization.
What features are indicative of a diagnosis of hyperparathyroidism?
Marked and persistent hypercalcemia and elevated serum PTH concentration.
high normal or inc serum PTH conc
DDx hypercalcemia
includes primary hyperparathyroidism, malignancy, vitamin D toxicity, and kidney disease.
PTH will be low-normal with any other cause of hypercalcemia
What are the complications associated with diabetic ketoacidosis (DKA)?
Hyperglycemia, glucosuria, dehydration, metabolic acidosis, and ketonemia.
What is the role of glucocorticoids in the adrenal system?
To regulate metabolism, immune response, and stress response.
What is a common neoplasm associated with the parathyroid glands?
Adenoma of the chief cells.
What is the relationship between calcium balance and renal function?
PTH promotes calcium reabsorption in kidneys and impacts calcium absorption in intestines.
What are the physiological responses to insulin deficiency in diabetes mellitus?
Suboptimal use of glucose, persistent hyperglycemia, and weight loss.
What clinical signs may suggest diabetic ketoacidosis?
Nausea, vomiting, dehydration, and weakness.
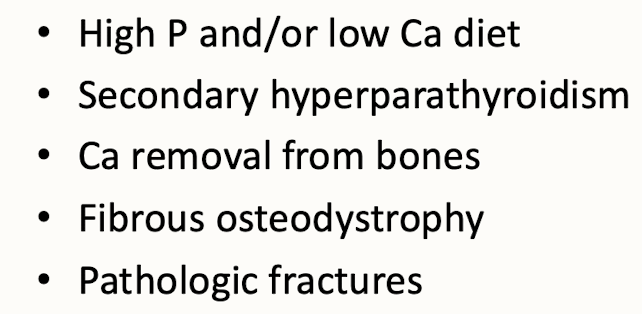
Why is calcium balance important in reptiles and can lead to nutritional secondary hyperparathyroidism?
It affects their bone health and metabolic functions. Nutritional secondary hyperparathyroidism occurs when inadequate calcium leads to excess parathyroid hormone secretion, resulting in weakened bones and other physiological issues.