Human Biology Sem 1 Exam
1/123
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
124 Terms
Homeostasis
Maintenance of a stable internal environment within cells.
Why do the ventricles have higher pressure during atrial filling?
During atrial filling chambers contract, causing blow flow into the arteries.
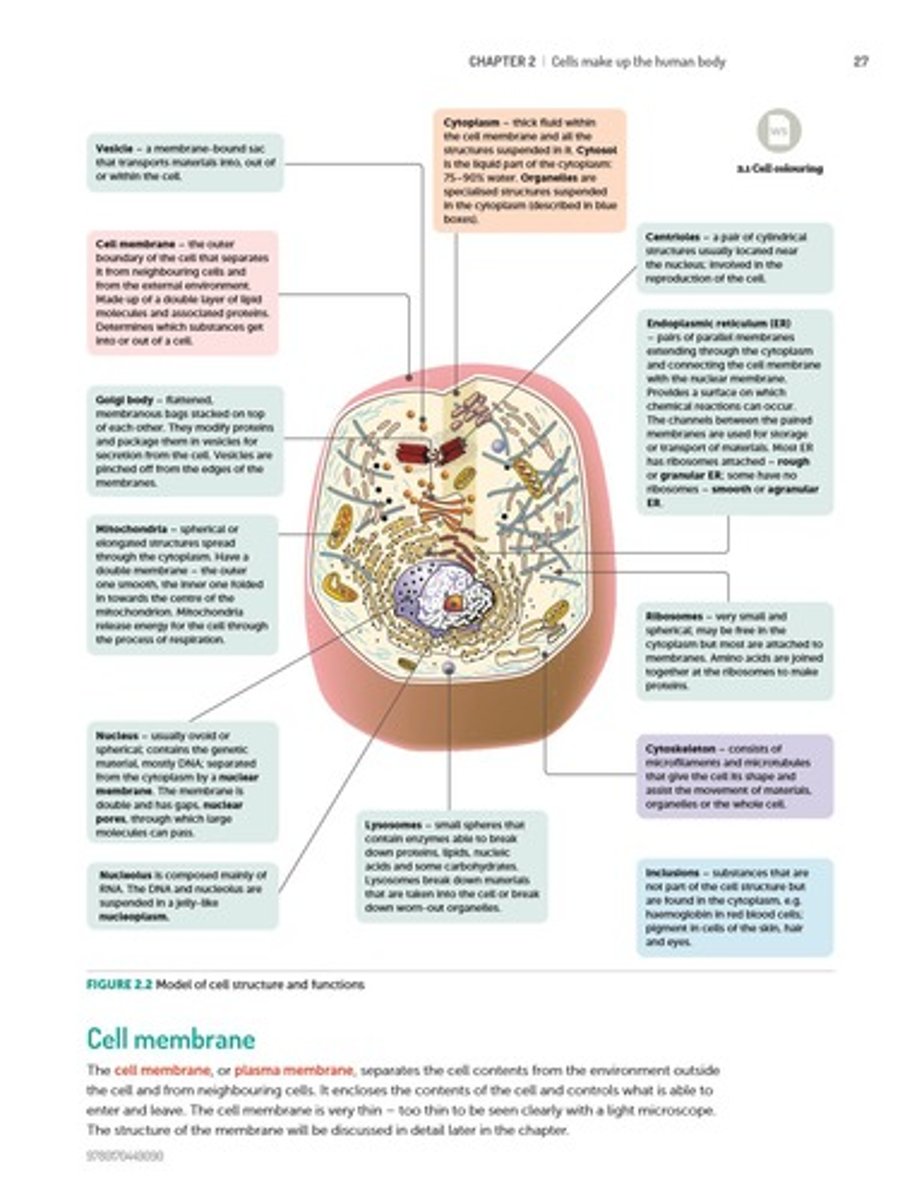
Cell membrane
The outer boundary of the cell.
Organelles
Structures suspended in the cytoplasm that carry out particular functions.
Cytosol
The liquid part of the cytoplasm.
Cytoskeleton
Internal scaffolding of protein fibres within the cytoplasm.
Inclusions
Chemical substances occurring as granules or liquid droplets in the cytoplasm.
Diffusion
Movement of molecules from high to low concentration.
Cytoplasm
Those parts of the cell within the cell membrane, except for the nucleus.
Osmotic Pressure
The amount of force applied to a solution that prevents solvent from moving across a semipermeable membrane.
Osmosis
Diffusion of water across a semi-permeable membrane.
Facilitated Diffusion
Uses carrier proteins for passive transport.
Hypotonic Solutions
Has a lower concentration of solutes compared to another solution it is being compared to.
Organization Levels
Cells → Tissues → Organs → Organ Systems → Organism.
Differentiation
Process where cells become specialized for specific functions.
Epithelial Tissue
Covering/lining tissue; thin & flat or cylindrical or cuboidal; tightly packed cells; acts as coverings; found in the outer layer of skin and lines inside of organs.
Connective Tissue
Separated from each other by large amounts of material not made up of cells (matrix)
Examples of connective tissue
Blood, bones, tendons, ligaments, cartilage
Nervous Tissue
Made of neurons- nerve cells
Muscular Tissue
Responsible for movement of body parts
Skeletal Muscle
Long & thin, striated, voluntary muscle with peripheral nucleus
Involuntary Muscle (Smooth Muscle)
Long & thin, non-striated, non-voluntary muscle with central nucleus
Cardiac Muscle
Long & thin, striated, non-voluntary muscle with central nucleus
Metabolism
The chemical processes that occur within a living organism in order to maintain life
Anabolism
Building complex molecules from simpler ones (requires energy)
Catabolism
Breaking down complex molecules into simpler ones (releases energy)
Nutrients
Organic (e.g., carbohydrates, proteins, lipids) and inorganic (e.g., water, minerals)
Enzymes
Catalysts that allow reactions to occur at normal body temp
Activation Energy
Energy required to start a reaction
Substrate
Molecule on which an enzyme acts
Lock-and-Key Model
Substrate fits enzyme like a key in a lock
Induced Fit Model
Enzyme adjusts shape to fit substrate
Cellular Respiration
Process by which organic molecules are broken down to produce energy in the form of ATP
Glycolysis
Breaks down glucose & produces 2 ATP molecules & 2 pyruvic acid molecules
Aerobic Respiration
CR with oxygen, occurs in the mitochondria, producing up to 36 ATP molecules
Anaerobic Respiration
CR without oxygen, occurs in the cytoplasm, producing lactic acid if no oxygen is present
ATP/ADP Cycle
ATP stores energy; breaking its bonds releases energy for cellular processes
Respiratory System
Composed of the nose, pharynx, larynx, trachea, bronchi, bronchioles, and lungs
Inspiration
The diaphragm and external intercostal muscles contract, expanding the chest cavity and creating a lower pressure within the lungs. The thoracic cavity and lung volume increase.
Expiration
The diaphragm and intercostal muscles relax, causing the chest cavity to decrease in size and the lungs to deflate.
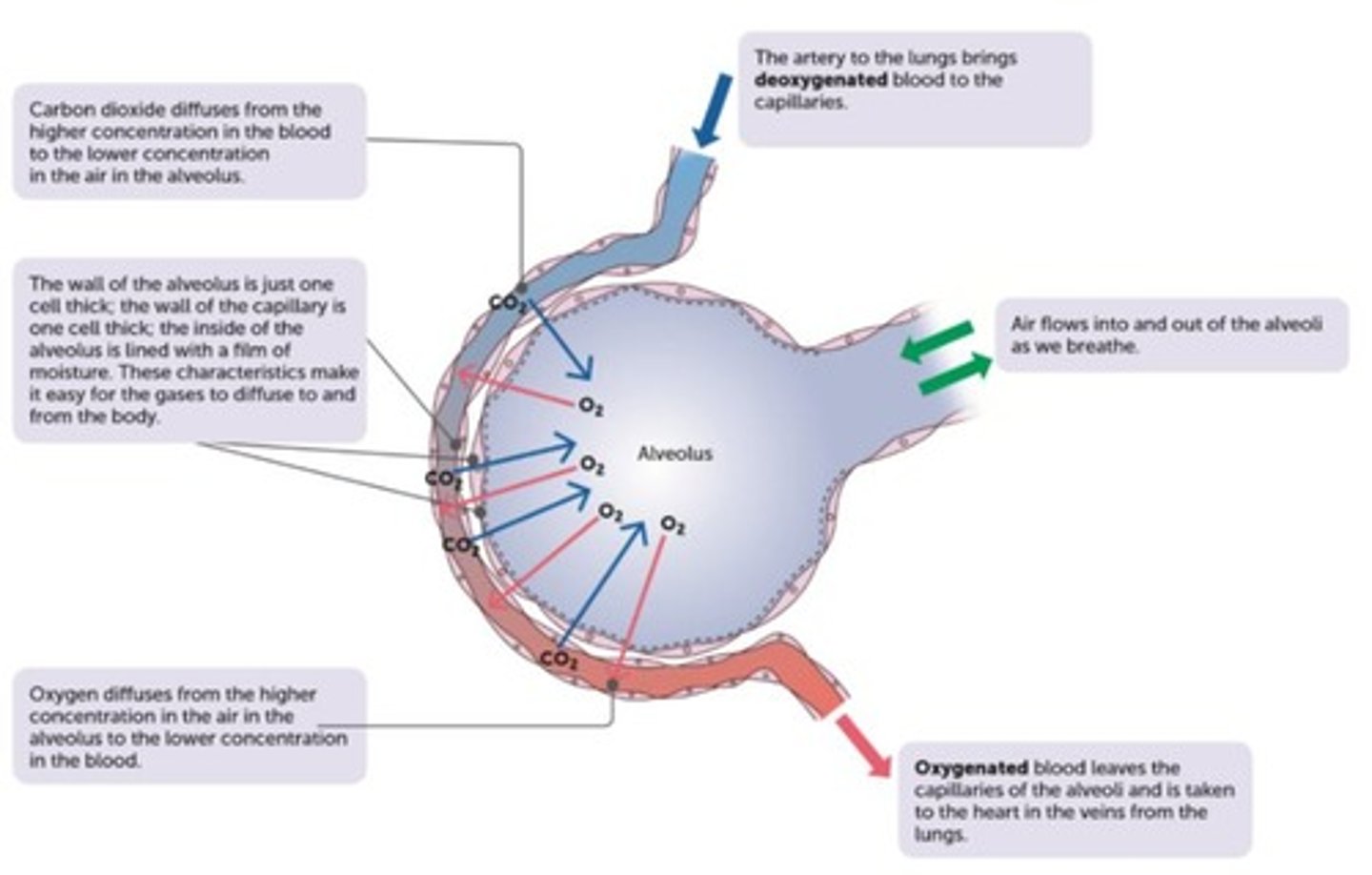
Gas Exchange (GE)
Exchange of oxygen and carbon dioxide in the lungs.
Where does GE occur?
Between the alveoli and surrounding capillaries.
When does GE occur?
All the time except when alveoli are damaged by respiratory conditions like - emphysema, cancer, TB (tuberculosis).
Why does GE occur?
It allows oxygen to enter the blood supply and be delivered to the cells to be used in the process of cellular respiration.
How does GE occur?
Due to structural adaptations and a concentration gradient
Structural Adaptations
Alveoli give the lungs a large surface area to increase the rate of GE.
Continuous flow of blood
Each alveolus is well supplied with blood vessels (capillaries) with a continuous flow of blood.
Movement of air
Movement of air in & out of lungs by the intercostal muscles and diaphragm also maintain the O2/CO2 concentration gradient.
Alveolus and capillary thickness
Alveolus and capillary are only one cell thin, so O2/CO2 do not have far to diffuse.
Lung positioning
The lungs are positioned deep inside the body to prevent evaporation of moisture that lines the alveolus.
Thin layer of moisture
Thin layer of moisture between alveolus and capillaries increases the rate of GE.
Concentration Gradient
There must be a concentration gradient so the gases can diffuse across the alveoli and capillary wall.
Oxygen movement
O2 moves from high concentration in alveoli into low concentration in blood.
Carbon dioxide movement
CO2 moves from high concentration in blood to low concentration in alveoli.
Effects on GE
Diseases like emphysema, lung cancer, asthma, and infections impair gas exchange by damaging lung tissue or narrowing airways.
Components of CS
Made up of blood, heart and blood vessels.
Function of CS
Transport nutrients, oxygen, water, white blood cells, hormones to every cell in the body.
Maintenance by CS
Maintain pH, maintain body temp, maintain H2O/ion (electrolyte) concentration.
Protection by CS
Against disease/invading microorganisms, blood clotting to prevent blood loss.
Blood composition
Plasma, erythrocytes, leucocytes, and thrombocytes.
Plasma
A solution primarily composed of water, containing dissolved solutes such as glucose and electrolytes.
Erythrocytes (Red Blood Cells)
Exhibit a biconcave disc shape, lacking a nucleus to enhance flexibility and facilitate passage through capillaries.
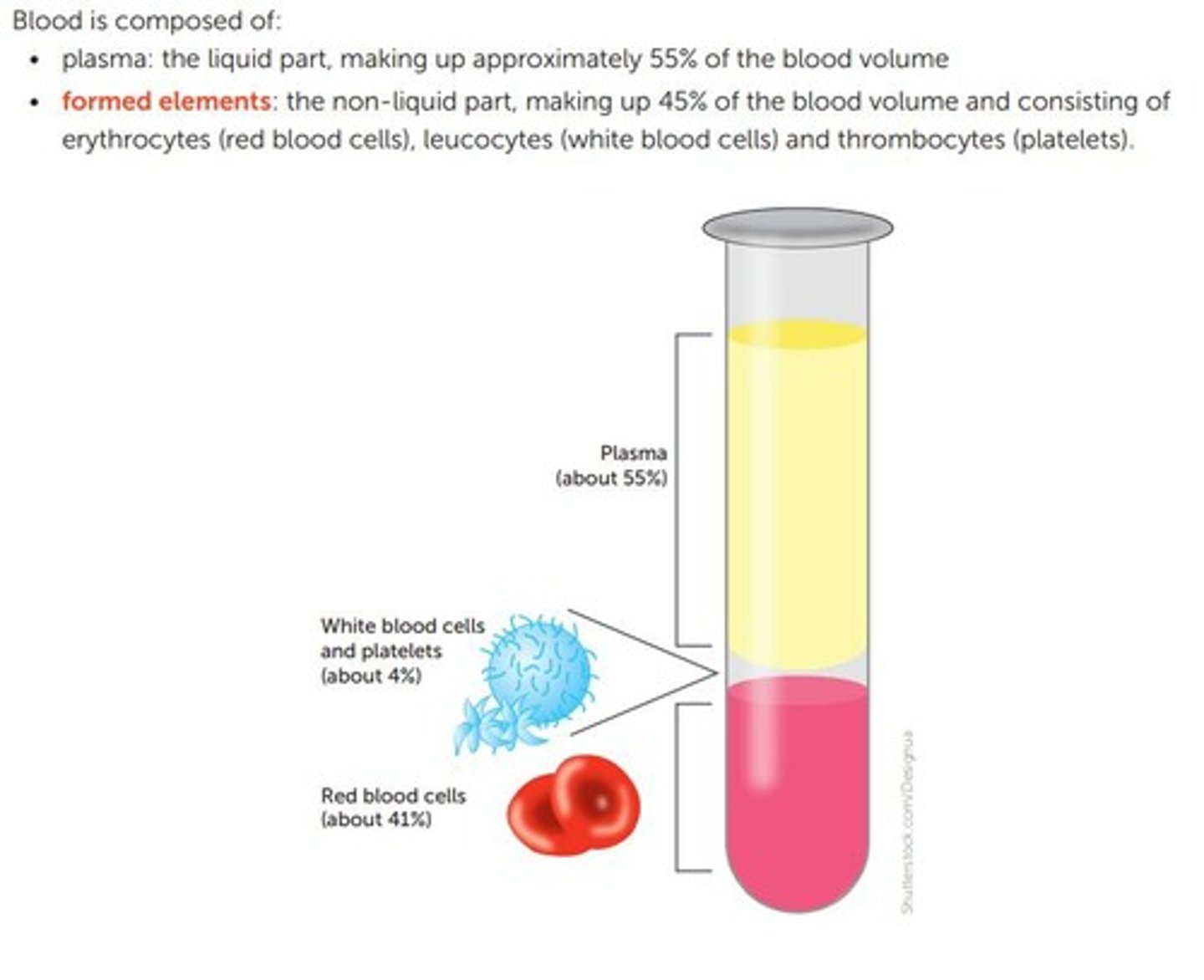
Leucocytes (White Blood Cells)
Essential for immune defence mechanisms, representing about 1% of blood volume.
Thrombocytes (Platelets)
Small, anucleate cell fragments that adhere to damaged endothelium and initiate the coagulation cascade.
Blood Clotting
Also called coagulation, it is the process that occurs when there is injury or damage to blood vessels.
Haemostasis
The process of stopping bleeding.
Clot
A plug of platelets, WBCs, RBCs, and plasma trapped in fibrin.
Fibrin
A protein in the form of threads that form a mesh to create a clot (thrombus) and keeps the clot attached to the wall of the blood vessel.
Vasoconstriction
The constriction (narrowing) of blood vessels at the injury site to reduce blood flow to the area.
Vasoconstrictors
Chemicals released by platelets that cause vasoconstriction.
Clotting Factors (CF)
Chemical substances in the blood that strengthen and reinforce the clot, releasing fibrin.
Clot Retraction
The process where fibrin contracts and pulls the edges of the blood vessel together.
Serum
The fluid that is squeezed out during clot retraction.
Scab Formation
The process of a dried-out clot forming over a wound.
Oxygen (O2) Transport
3% of O2 is transported in plasma, while 97% is combined with haemoglobin (oxyhaemoglobin).
Haemoglobin
A protein in RBCs that binds oxygen in the lungs and releases it in tissues.
Carbon Dioxide Transport
About 70% of carbon dioxide is converted to bicarbonate ions in RBCs and transported in plasma.
Flow of Blood through the Heart
The right atrium receives blood from the body and passes it to the right ventricle, which pumps blood to the lungs; the left atrium receives blood from the lungs and passes it to the left ventricle, which pumps blood to the body.
Arteries and Arterioles
Have thick, muscular, and elastic walls to withstand and regulate high-pressure blood flow from the heart to tissues.
Veins and Venules
Have thinner walls and valves to prevent backflow, carrying low-pressure blood back to the heart.
Capillaries
Very thin walled (one cell thick) to allow efficient exchange of gases, nutrients, and wastes between blood and tissues.
Blood flow
Fastest and under highest pressure in arteries, slows in capillaries for exchange, and returns at low pressure in veins.
Cardiac Cycle Phases
Diastole (heart muscle relaxes, and chambers fill with blood) and Systole (heart muscle contracts and pumps blood out to the arteries).
Cardiac Output
The volume of blood the heart pumps per minute, calculated as heart rate × stroke volume.
Blood Types
Determined by specific antigens on the surface of red blood cells, classified by the ABO system and the Rh factor.
Type A Blood
Has A antigens and anti-B antibodies.
Type B Blood
Has B antigens and anti-A antibodies.
Type AB Blood
Has both A and B antigens, no anti-A or anti-B antibodies.
Type O Blood
Has no A or B antigens, but has both anti-A and anti-B antibodies.
Rh Factor
Determines if blood type is Rh-positive (+) or Rh-negative (-), based on the presence of the Rh antigen.
Universal Donor
O negative blood type
Universal Recipient
AB positive blood type
Lymphatic System Functions
To collect fluid that escapes from blood capillaries and return it to the circulatory system, and to defend the body against pathogens.
Lymph
Excess fluid from the blood, originally plasma, then interstitial fluid, then lymph.
Oedema
Swelling caused by the accumulation of fluid between cells.
Mechanical Digestion
Physical breakdown of food, including chewing and churning.
Chemical Digestion
Enzymes break complex molecules into simple ones.
Stages of digestion
Ingestion, Mastication, Mechanical digestion, Chemical digestion, Peristalsis, Segmentation, Absorption, Elimination.
Digestive System Structure
A tube (alimentary canal) with organs (mouth, oesophagus, stomach, intestines) and glands (salivary, pancreas, liver, gall bladder) that aid digestion and absorption.
Mouth
Ingestion, chewing (teeth), saliva (amylase) starts starch digestion.