Pharmacokinetics
0.0(0)
Card Sorting
1/113
Earn XP
Description and Tags
Last updated 4:12 PM on 1/27/23
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
114 Terms
1
New cards
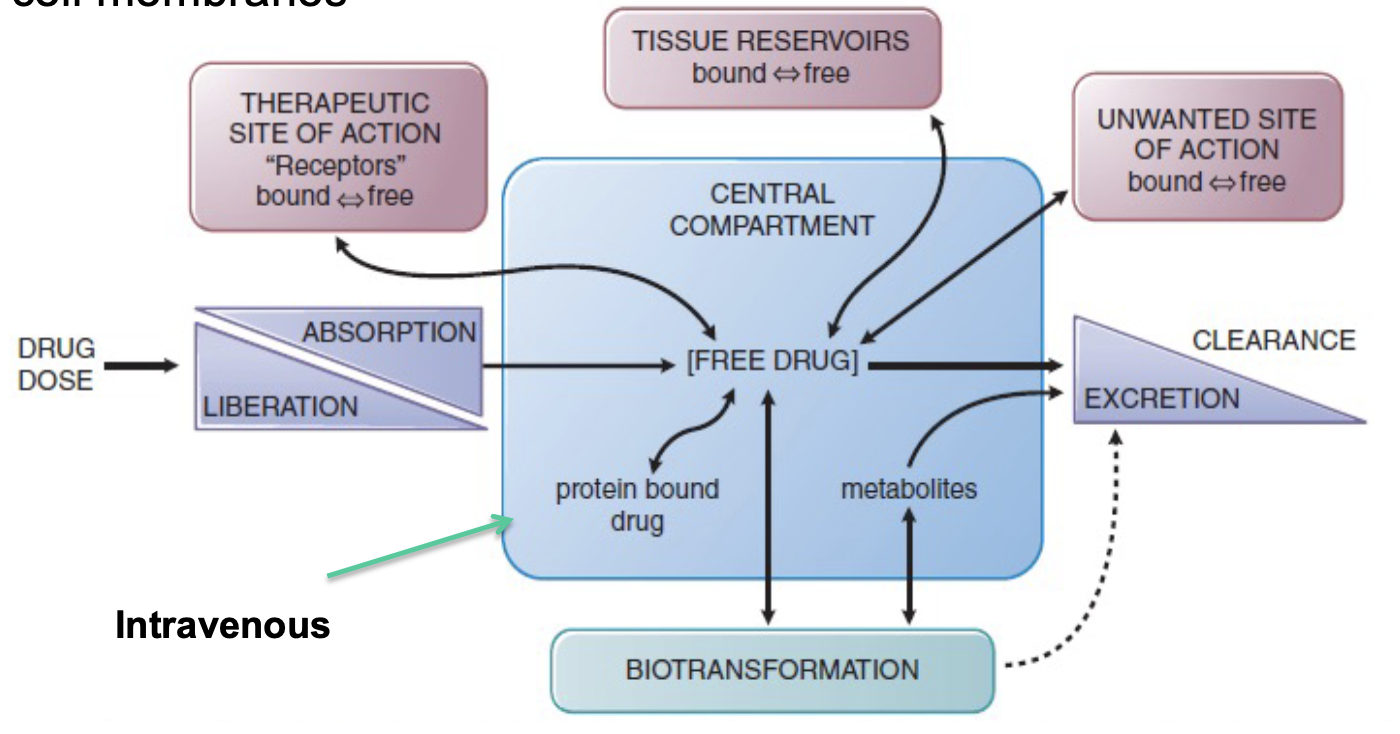
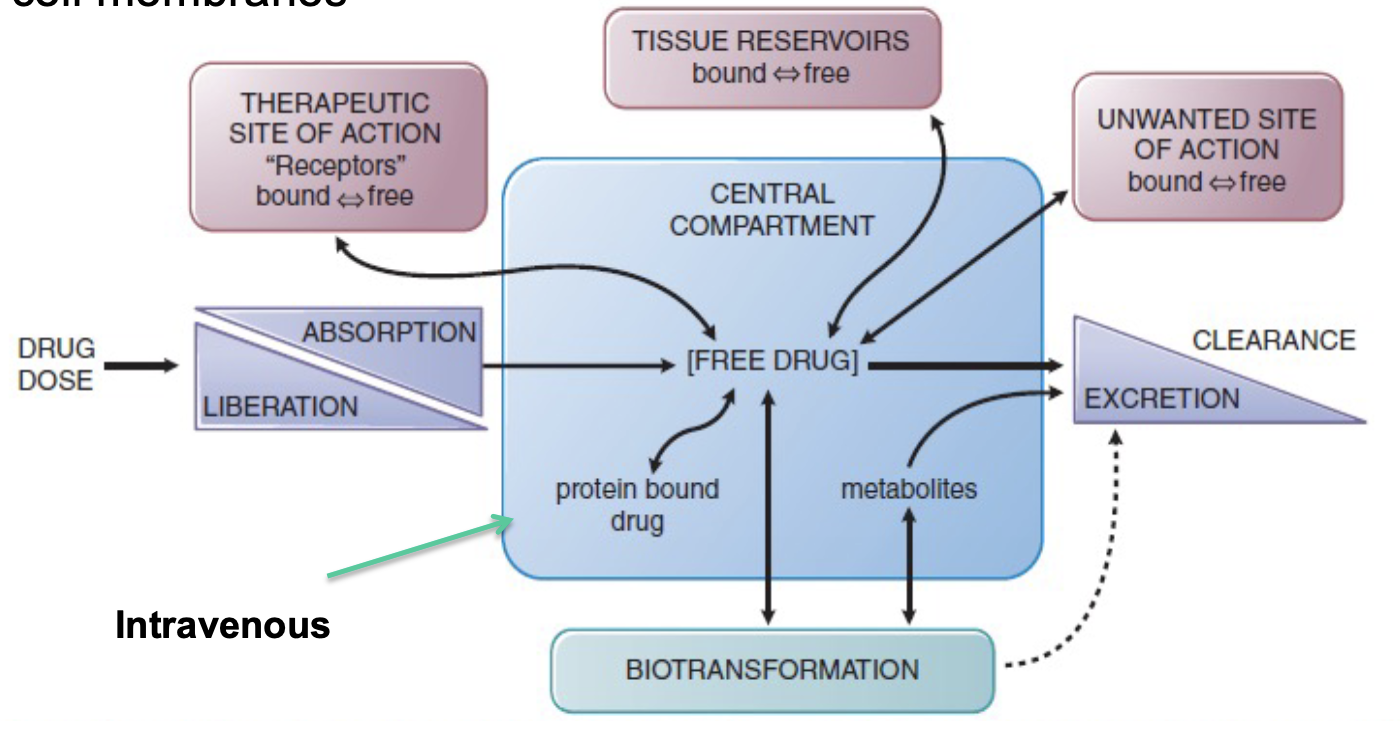
Where are most drugs administered and moved to?
* into one body compartment
* to the site of action where they produce effects
* to the site of action where they produce effects
2
New cards
Drugs must ______ various barriers that separate compartments ie. cell membranes
permeate
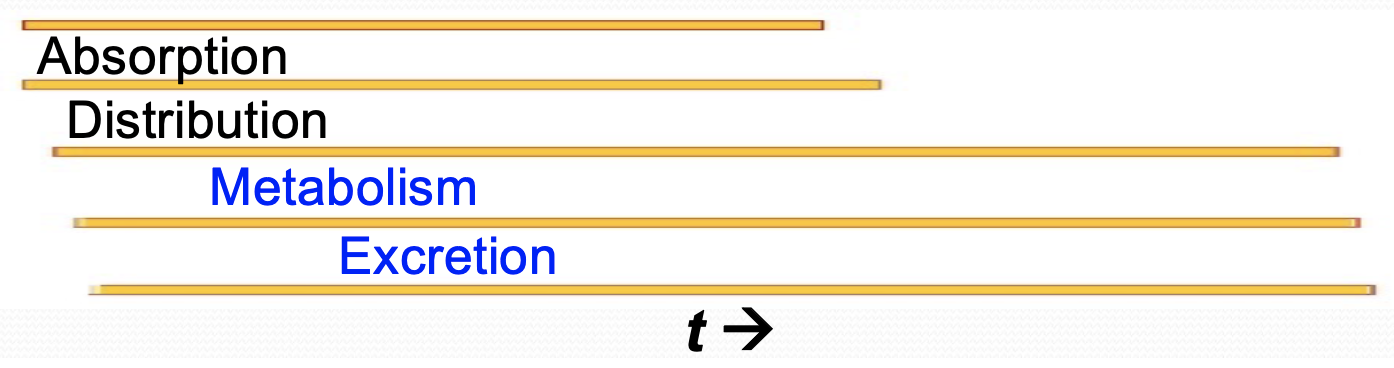
3
New cards
The absorption, distribution, metabolism, and excretion of a drug involves
transport across cell mebrnes, which is affected by several drug characteristics
4
New cards
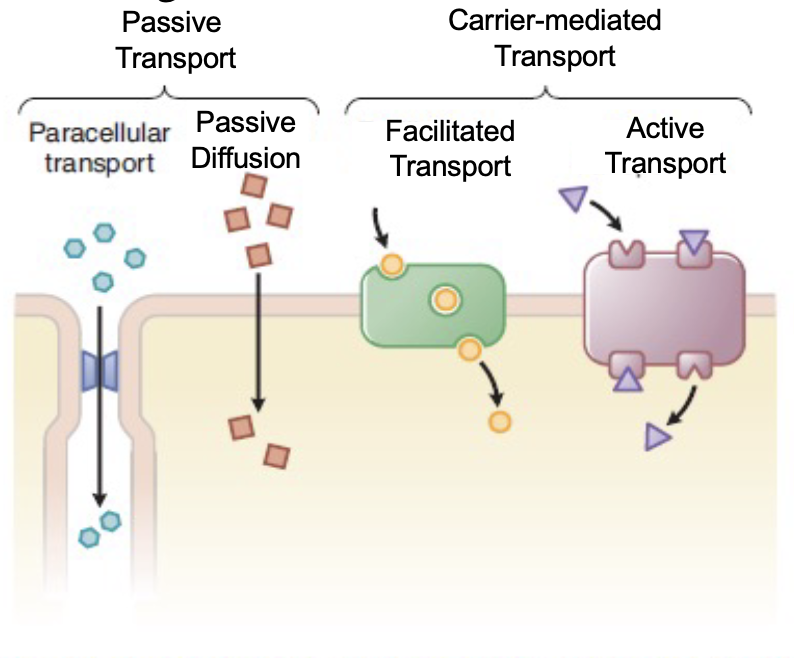
Passive transport includes
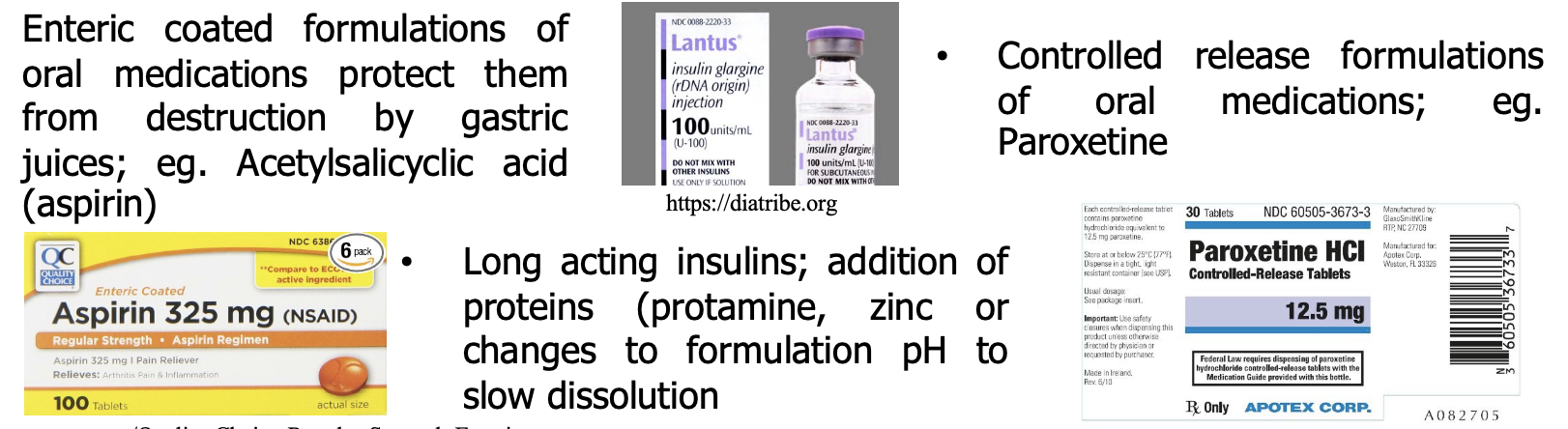
* paracellular transport
* passion diffusion
* passion diffusion
5
New cards
What is passive diffusion
of a drug thru cell membranes is generally limited to unbound(free) drug
* large lipophilic drugs typically pass thru membranes
* thru cell mebranes dominates transport for most drugs
* large lipophilic drugs typically pass thru membranes
* thru cell mebranes dominates transport for most drugs
6
New cards
What is paracellular
passage of molecules thru intercellular gas
* transfer in the capillary endotherlium is limited only by blood flow
* some. capillaries have “tight” intercellular junctions, limiting flow
* transfer in the capillary endotherlium is limited only by blood flow
* some. capillaries have “tight” intercellular junctions, limiting flow
7
New cards
Carrier-mediated transport includes
* facilitated transport
* active transport
* active transport
8
New cards
What are a 4 drug characteristics that involve transport across cell membranes
* molecular size & structural feature
* degree of ionization
* relative lipid solubility of ionized/non-ionized forms
* affinity and binding to serum and tissue protein
* degree of ionization
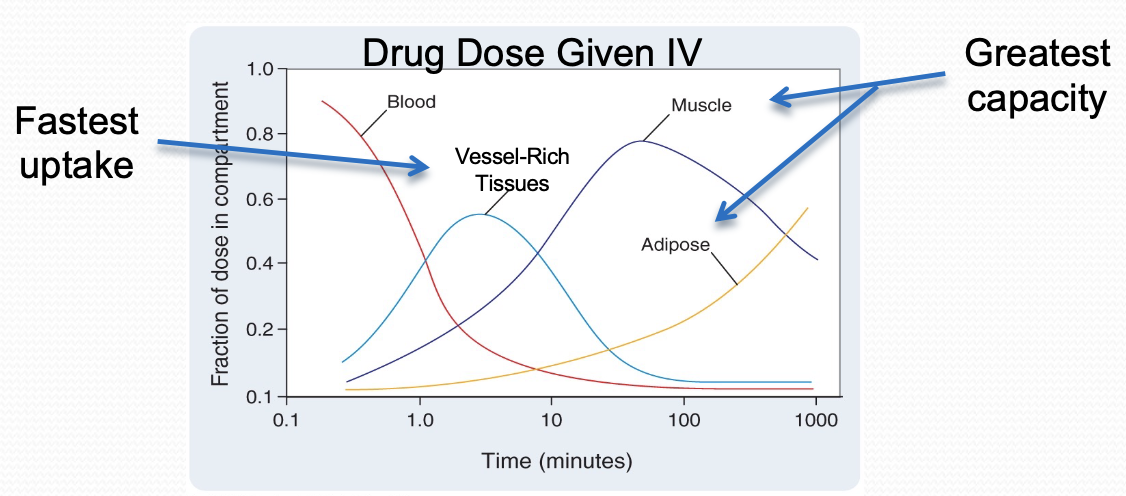
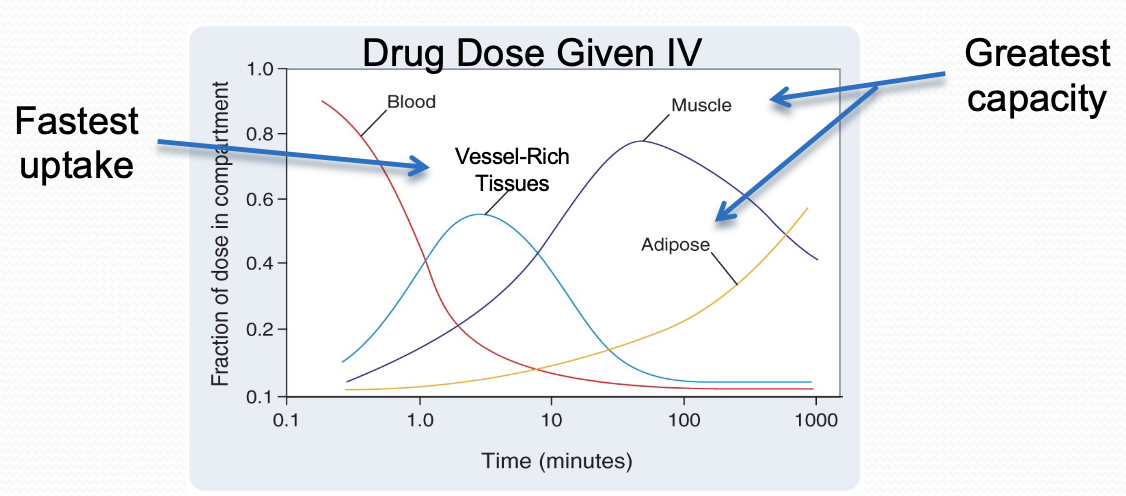
* relative lipid solubility of ionized/non-ionized forms
* affinity and binding to serum and tissue protein
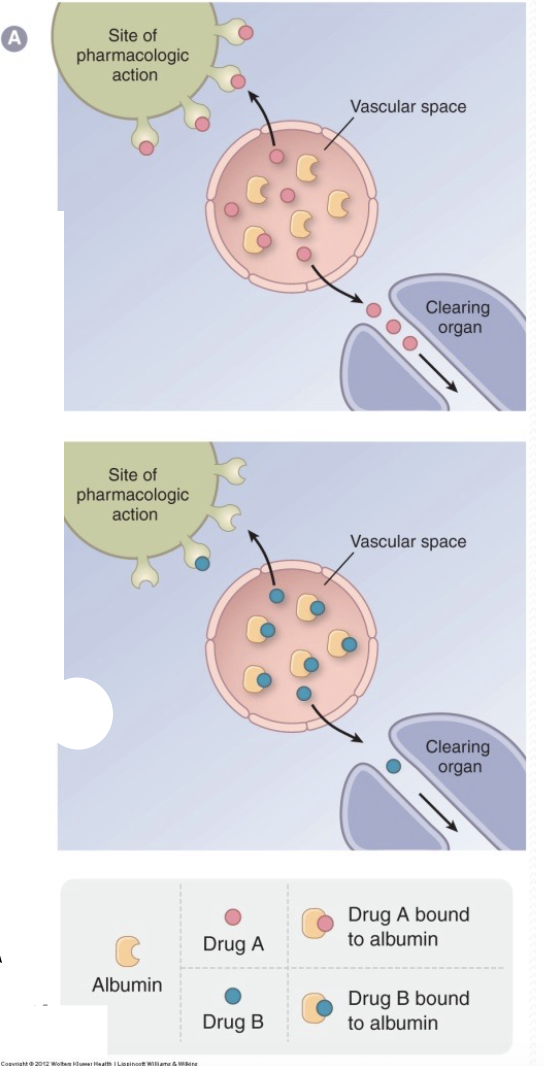
9
New cards
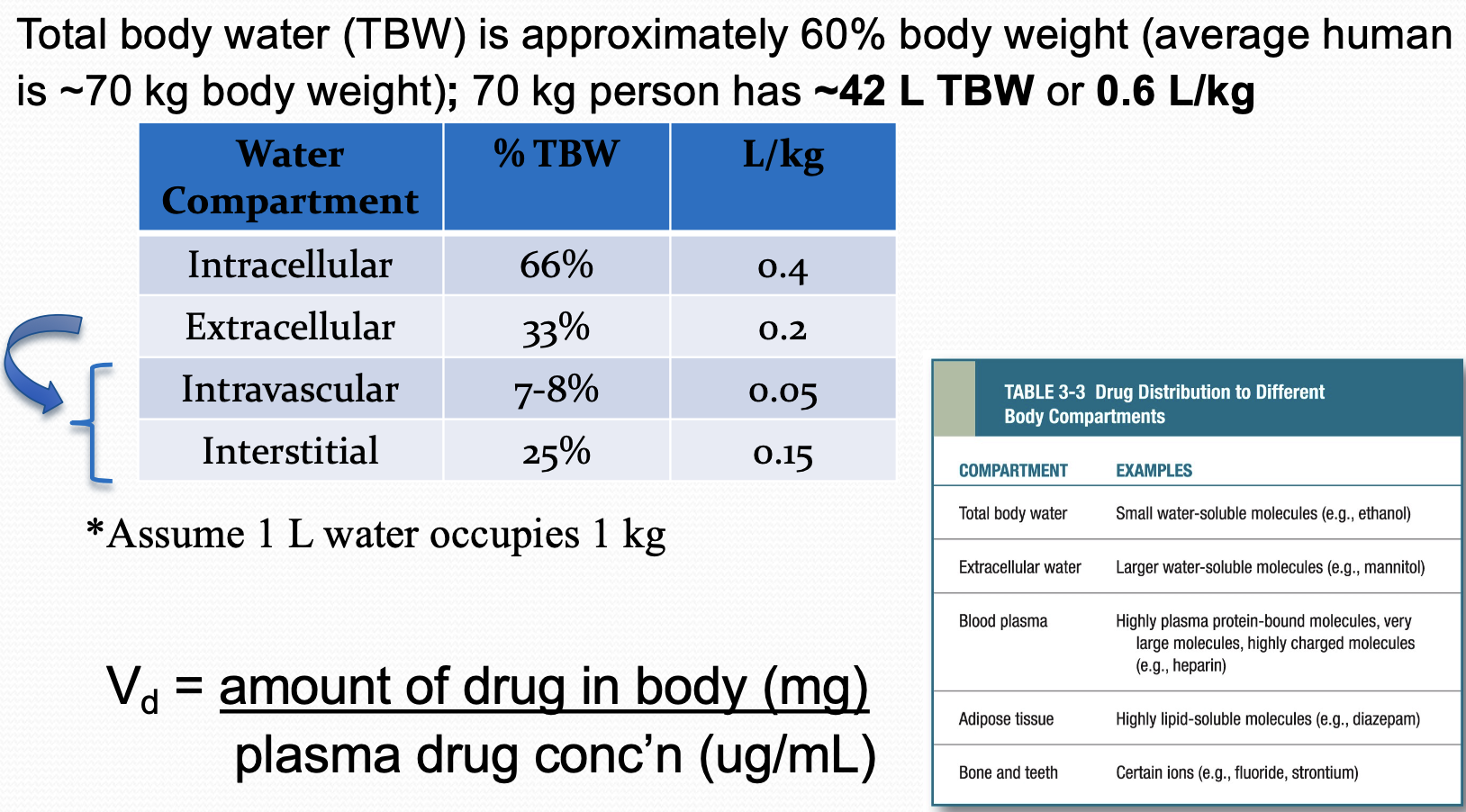
Passive transport consists of what kind of lipid
amphipathic
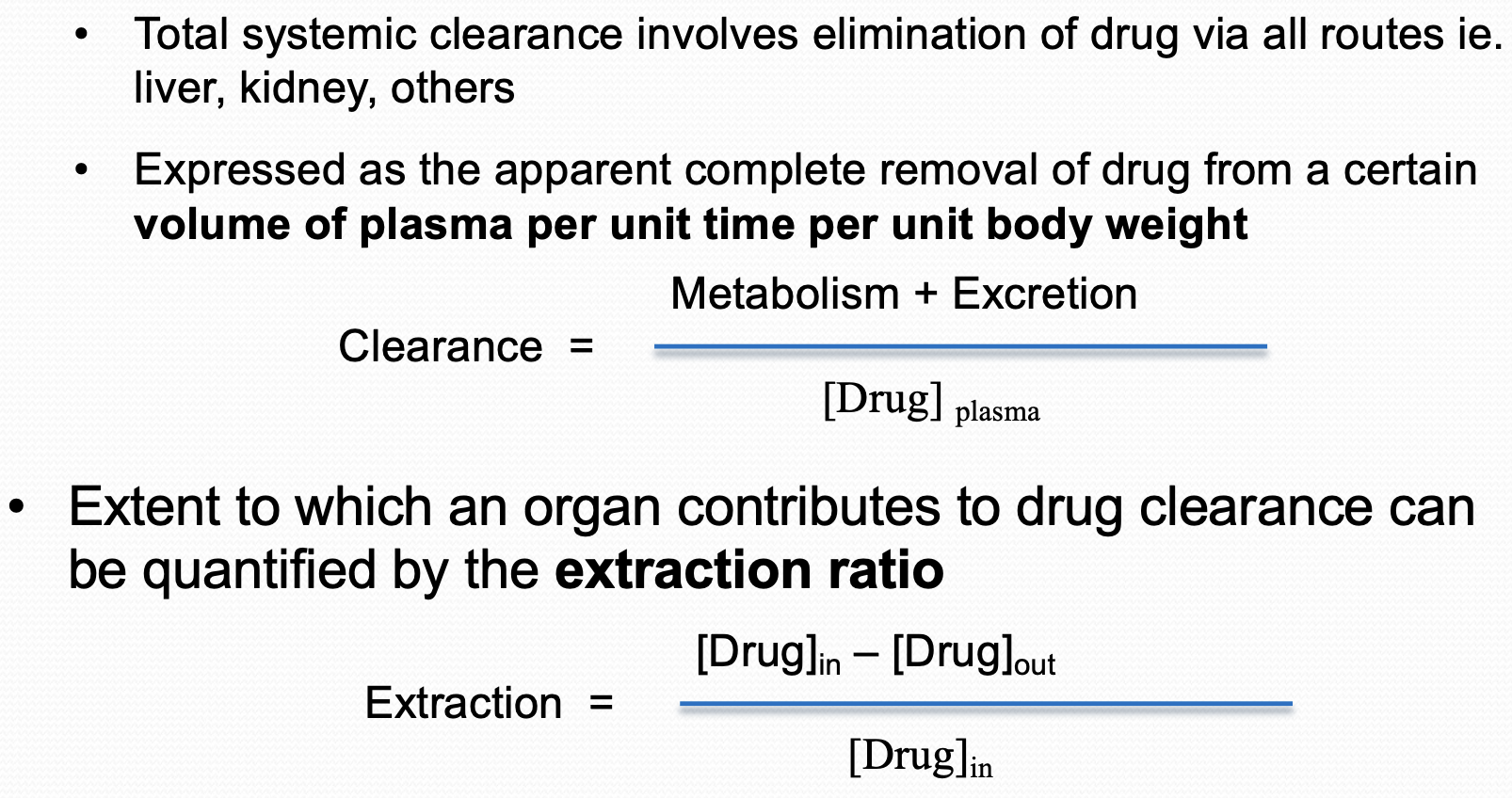
10
New cards
Are cell membranes permeable to water
yes
* bulk flow of water can carry small water soluble substances(100-200 Da)
* bulk flow of water can carry small water soluble substances(100-200 Da)
11
New cards
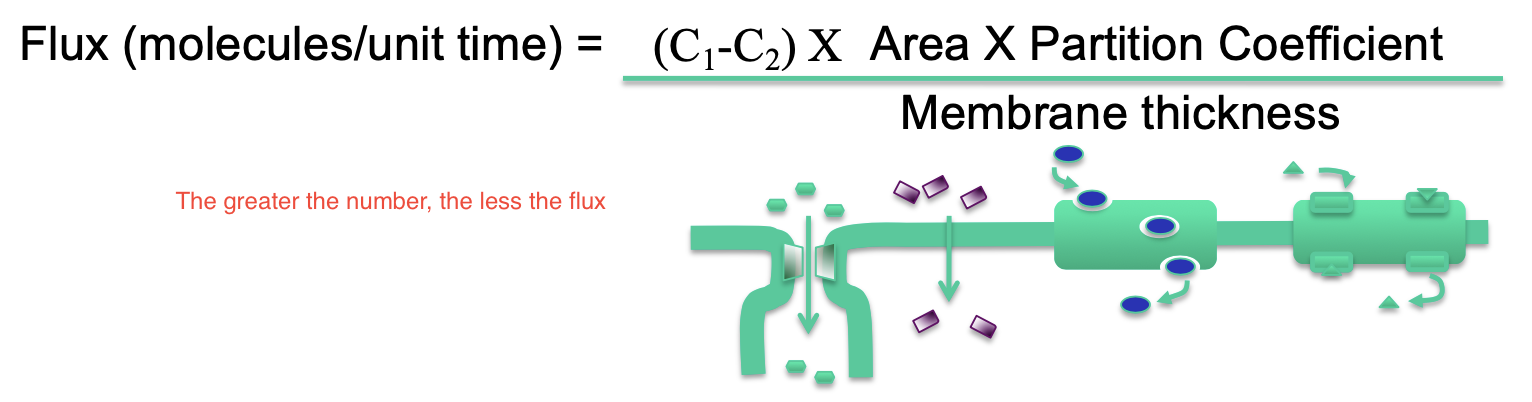
Passive flux across the membrane is driven by
* drug concentration gradient across membrane
* solubility of drug
* greater the coefficient, the faster the diffusion
* The surface area of membrane
* Membrane thickness
* solubility of drug
* greater the coefficient, the faster the diffusion
* The surface area of membrane
* Membrane thickness
12
New cards
Many drugs are ____ acids or bases present in solution as un-ionized and ionized species
weak
13
New cards
Un-ionized species ____ lipid soluble; ____ readily diffuse cell membranes
more, more
14
New cards
Ionized species are __ lipid soluble; __ able to cross thru cell membranes \n directly;
less, less
15
New cards
Transmembrane distribution of a weak electrolyte is influenced by ________ and _________
* its pKa (ionizable constant)
* the pH gradient across the cell membrane
* the pH gradient across the cell membrane
16
New cards
pKa
= pH at which 50% of drug is ionized and 50% is unionized
* pKa usually between pH 3 and pH 11
* pKa usually between pH 3 and pH 11
17
New cards
Drug accumulation of side of cell membrane where ionization is highest or lowest
* highest
* called ‘ion trapping’
* basic drugs accumulate in acidic forms and vice versa
* called ‘ion trapping’
* basic drugs accumulate in acidic forms and vice versa
18
New cards
Important to memorize about passive transport
* basic drugs accumulate in acidic fluids
* acidic drugs accumulate in basic fluid
* acidic drugs accumulate in basic fluid
19
New cards
Why is carrier-mediated transport important (for) (3)
* molecules too large for passive diffusion
* molecules not soluble in lipids for passive diffusion
* carriers are saturable, selective, and inhabitable
* molecules not soluble in lipids for passive diffusion
* carriers are saturable, selective, and inhabitable
20
New cards
What does a active transporter do
move molecules against their concentration and electrical
* requires energy in the form of ATP
* requires energy in the form of ATP
21
New cards
What do faciliated transporters do?
Move large/lipid insoluble molecules down their electrochemical gradients
* no energy input acquired
* no energy input acquired
22
New cards
Acronym for pharmacokinetics
* what the body does to the drug
M- metabolism
A - absorption
D- distribution
E- excretion
M- metabolism
A - absorption
D- distribution
E- excretion
23
New cards
Where can drugs first be absorbed into the systemic circulation?
site of administrations to get to target sites
24
New cards
Which route does not required absorption
* Intravenous, intrathecal, and other minor routes
25
New cards
Before enter circulation for solid or semi-solid dosage form what does absorption first require of an active drug
dissolution
26
New cards
What affects rate of absorption from site of adminstation?
* physiochemical drug factors
* physiologic factors
* drug formation
* physiologic factors
* drug formation
27
New cards
What are the physiological factors of absorption?
* large concentration gradient between site of drug administration and surrounding tissue drives the uptake of drug into the circulation
28
New cards
What are the drug formation of absorption?
* physical and chemical ingredients of a medication
* Includes both the active drug, and any inactive chemicals that comprise a pharmaceutical product ready for administration to the patient
* Includes both the active drug, and any inactive chemicals that comprise a pharmaceutical product ready for administration to the patient
29
New cards
Modifications of the active pharmaceutical ingredient and/or final \n formulation can be employed to....
* Slow or delay the release of the API for absorption \n • More convenient as the drug is less frequently administered \n • Usually for drugs with short elimination half-lives \n • Modifications aimed at prolonging the dissolution phase of absorption \n • “Dose-dumping or erratic absorption is a potential concern
30
New cards
What is bioavailability
a fraction of administered dose that reaches the systematic circulation unchanged
31
New cards
Bioavailability can be reduced or affected by
* Precipitation of drug at injection site
* unable to be absorbed by the G.I. tract
* physiochemical property of drug
* reverse transport protein (P-glycoprotein)
* “First Pass” elimination effect following oral administration of drugs
* Primarily due to liver metabolizing enzymes inactivating drug
* Enzymes in G.I. tract wall can also metabolize drug
* Drug can also be excreted in bile
* unable to be absorbed by the G.I. tract
* physiochemical property of drug
* reverse transport protein (P-glycoprotein)
* “First Pass” elimination effect following oral administration of drugs
* Primarily due to liver metabolizing enzymes inactivating drug
* Enzymes in G.I. tract wall can also metabolize drug
* Drug can also be excreted in bile
32
New cards
What is the most common method of drug administration
Enteral: Oral
33
New cards
What is enteral
going through the GI tract
34
New cards
What are the advantages of oral administration (5)
* most convenient for self-administration
* most economical route
* usualy safer than injection
* minimal risk of infection
* can induce vomiting to potentially remove drug
* most economical route
* usualy safer than injection
* minimal risk of infection
* can induce vomiting to potentially remove drug
35
New cards
What are the disadvantages of oral administration (6)
* Absorption may be erratic
* enteric coating protects some drugs against gastric juices/acids
* patient compliance problems
* not for unconscious patients
* emesis and GI irritation possible
* “first pass elimination
* enteric coating protects some drugs against gastric juices/acids
* patient compliance problems
* not for unconscious patients
* emesis and GI irritation possible
* “first pass elimination
36
New cards
What is first pass effect
in which a drug gets metabolized at a specific location in the body that results in a reduced concentration of the active drug upon reaching its site of action or the systemic circulation.
37
New cards
What are other eternal minor adminstration routes
* Oral transmucossal
* Rectal
* Rectal
38
New cards
What are the 2 kinds of oral transmucosal
* Sublingual
* Buccal
* Buccal
39
New cards
What is sublingual oral transmucosal? (4)
* under the tongue
* absorption from the oral mucosa
* can potentially by-pass “first pass effect” by venous drainage to superior vena cava
* usually higly lipophilic drugs, eg. nitroglycerin for angina pectoris
* absorption from the oral mucosa
* can potentially by-pass “first pass effect” by venous drainage to superior vena cava
* usually higly lipophilic drugs, eg. nitroglycerin for angina pectoris
40
New cards
What is buccal oral transmucosal
* between the cheek and gum
* absorbed from mucosa, eg. fentanyl lollipop
* absorbed from mucosa, eg. fentanyl lollipop
41
New cards
Explain rectal admission
\
* Estimated that roughly 50% of drugs administered by the rectum will by-pass “the first pass effect”
* potential for irritation
* less nausea
* used in patients with GI motility disorders, and near end-of-life car
* Estimated that roughly 50% of drugs administered by the rectum will by-pass “the first pass effect”
* potential for irritation
* less nausea
* used in patients with GI motility disorders, and near end-of-life car
42
New cards
What is parenteral
* injectable drugs are most comon form
* drug availability is usually more rapid, and predictable over oral
* by passes “first pass effect”
* drug availability is usually more rapid, and predictable over oral
* by passes “first pass effect”
43
New cards
What is subcutaneous injection
* SC or SQ
* injection is administered in the tissues lying below the skin
* injection is administered in the tissues lying below the skin
44
New cards
What are the advantages of subcutaneous injection
* suitable for solid pellets eg. contraceptives
* suitable fro insoluable suspensions
* easier to administer than IV
* suitable fro insoluable suspensions
* easier to administer than IV
45
New cards
What are the disadvantages of subcutaneous injection
* absorption is slower than IM route
- can be erratic depending on blood flow to the site
* not suitable for large volumes
* pain and/necrosis with the irritating injectable drug solution
* technical skills needed for some injections
* generally, the drug is irretrievable once injected
- can be erratic depending on blood flow to the site
* not suitable for large volumes
* pain and/necrosis with the irritating injectable drug solution
* technical skills needed for some injections
* generally, the drug is irretrievable once injected
46
New cards
What is intramuscular injection
* more painful than SQ - bigger needle, deeper
* administered into the muscle (gluteus maximus, vastus laterals of the thigh, deltoid of upper arm, etc)
* administered into the muscle (gluteus maximus, vastus laterals of the thigh, deltoid of upper arm, etc)
47
New cards
What are the advantages of intramuscular injection
* absorption is typically rapid for drugs in aqueous solutions; oily suspensions will form depot
* safe, easier than IV
* safe, easier than IV
48
New cards
What are the disadvantages of intramuscular injection
* local pain and swelling with irritating solutions
49
New cards
What is intervenous injection (IV)
administered into an accessible vein (bolus vs slow infusion)
* ex. cephalic vein, jugular vein, others
* ex. cephalic vein, jugular vein, others
50
New cards
What are the advantages of intervenous injection (IV) (5)
* route of choice for emergency administration of drugs
* large volumes can be given by this route
* Bioavailability is complete; dose delivery is controlled
* Route with most rapid onset of action
* irritating solutions given by this route
* large volumes can be given by this route
* Bioavailability is complete; dose delivery is controlled
* Route with most rapid onset of action
* irritating solutions given by this route
51
New cards
What are the disadvantages of inteerbenous injection
* most inject many solutions slowly
* not for oily suspensions
* adverse reactions can occur due to higher blood levels achieved rapidly compared to other routes
* not for oily suspensions
* adverse reactions can occur due to higher blood levels achieved rapidly compared to other routes
52
New cards
What are topical
drugs applied topically to the eye, skin, and mucus membranes
* cream etc
* cream etc
53
New cards
What are the advantages of topical?
* drug delivered locally; can achieve very high concentration
54
New cards
What are the disadvantages on topical (2)
* may be absorbed systematically
* may not remain at desired site
* may not remain at desired site
55
New cards
What is transdermal
Drugs applied to the skin and absorbed into the systemic circulation
56
New cards
What are the advantages of transdermal
* absorption enhanced by abraded, denuded or burned skin
* controlled release, eg. nicotine and fentanyl patches
- prolonged duration of action
* by passes “first pass elimination” effects
* controlled release, eg. nicotine and fentanyl patches
- prolonged duration of action
* by passes “first pass elimination” effects
57
New cards
What are the disadvantages of transdermal
theraputic blood levels are slow to achieve; delay onset of action
58
New cards
Interstitial Fluid
fluid within the organs, inbetween
59
New cards
What are the 3 distributions in the body is affected by
1. Physiochemical properties of the drugs
2. Anatomy and physiology of patient: Tissue Perfusion
3. Non-target binding of drug
60
New cards
What can a drug do once in the systemic circulation (3)
* remain in vascular (blood) space
* distribute to enter interstitial fluid
* further distribute to enter intracellular fluid
* distribute to enter interstitial fluid
* further distribute to enter intracellular fluid
61
New cards
What are the physiochemical properties of the drug
* lipid solubility
* size (molecular weight)
* degree of ionization
* size (molecular weight)
* degree of ionization
62
New cards
Initially, the vessel-rich tissues (liver, kidney, brain, heart) receive
the greatest cardiac output and thus the distribution of drug
63
New cards
Distribution of drug to less well-perfused tissues (muscle, fat, skin, most viscera) is faster or slower
is slower but accounts for most of the extravascular drug
64
New cards
What is plasma protein binding (4)
* Many drugs circulate in the blood bound to plasma \n proteins; can show low → high affinity for proteins \n • Cannot diffuse from vascular space to tissues
* Binding involves a saturable, non-linear process
* Albumin (\~ 4 g/dL) is a major carrier for drugs \n that act as weak acids eg. NSAIDs
* α1-acid glycoproteins bind drugs that are weak bases
* Binding involves a saturable, non-linear process
* Albumin (\~ 4 g/dL) is a major carrier for drugs \n that act as weak acids eg. NSAIDs
* α1-acid glycoproteins bind drugs that are weak bases
65
New cards
What is tissue binding
* Many drugs accumulate in tissues at levels higher \n than blood or interstitial fluid; can prolong drug action \n • bind cellular proteins, phospholipids, etc that are not the target sites
66
New cards
What is the volume of distribution (Vd)
describes the extent to which a drug partitions between blood and tissue compartments
67
New cards
How are drugs eliminated from the body
process of *excretion* or concerted to metabolites by *biotransformation*
68
New cards
What is clearance?
* it gives and indication of efficiency of drug from blood and therefore the body
69
New cards
What do excretory organs elminate
polar (water soluble) compounds more efficiently thsn non-polar (lipid soluble)compound
70
New cards
What is the most important excretory organ
* kidney
71
New cards
What percent of cardiac output do the kidney's receive
roughly 20%
72
New cards
What does active drug selection in proximal convoluted tubule add to the urine
drugs
73
New cards
_ is saturable, selective and inhibitable by other drugs
Active drugs secretion
74
New cards
What is metabolism or biotransformation?
change in the chemical structure of an absorbed drug within an living organism, usually by enzyme-catalyzed biochemical reactions
75
New cards
What is the main metabolizing organ
Liver
76
New cards
Why is drug metabolism important?
* we don’t want drugs to keeping doing its thing forever
* enzymes play a pivotal role in matabolism by making drugs more excretable and terminating their action(inactive)
* enzymes play a pivotal role in matabolism by making drugs more excretable and terminating their action(inactive)
77
New cards
Where are drugs metabolized
* livers the major site
* also occurs in other organs (lungs, GI tract, skin, kidneys, brain, plasma, etc)
* also occurs in other organs (lungs, GI tract, skin, kidneys, brain, plasma, etc)
78
New cards
Biotransformation reactions are catluzed by cellular enzymes that are located in hepatocytes…..
* **mainly smooth ER and cytoplasm**
* mitochonidra
* nuclear/cell mebrain
* lysosome
* mitochonidra
* nuclear/cell mebrain
* lysosome
79
New cards
How are drugs metabolized?
2 phases
1. Phase I reactions (oxidation/reduction/hydrolysis reactions)
2. Phase II reactions (conjugation reactions)
1. Phase I reactions (oxidation/reduction/hydrolysis reactions)
2. Phase II reactions (conjugation reactions)
80
New cards
What is occurs in Phase I
drugs are converted to more polar(hydrophilic) metabolites → either excreted or →undergo phase II reactions
81
New cards
What are characteristics of phase I reactions
involves 1 or more cytochrome P-450 (CYP)
(called P-450 that bc they are heme-containing proteins that absorb light at 450nm)
(called P-450 that bc they are heme-containing proteins that absorb light at 450nm)
82
New cards
Approx how many CYP450’s are know to be important for metabolism of drugs
12
* mainly the CYP2C, CYP2C, CYP3A subfamilies
* mainly the CYP2C, CYP2C, CYP3A subfamilies
83
New cards
What are the types of phase I reactions
Oxidation - most common - addition of oxygen or removal of hydrogen (loss of e-) from drug
Reduction and hydrolysis - less common
Reduction and hydrolysis - less common
84
New cards
What percent of oxicdative reactions involve CYP450
95%
85
New cards
What occurs during Phase II
reactions in which a substance from a diet is attached to a group from phase I → more polar, excretable product
86
New cards
What are the characteristics of phase II
* couple drugs with substates from diet to propuce conjugates(more polar, inacitve, readily excretable)
* conjugates required the drug to have an oxygen, nitrogen, or sulfur atoms as acceptors doe hydrophilic conjugate moiety
* eg. **Glucuronic acid, sulphate, glutathione, acetyl groups most commonly,** but also methyl, glycine, cysteine , or methionine
* conjugates required the drug to have an oxygen, nitrogen, or sulfur atoms as acceptors doe hydrophilic conjugate moiety
* eg. **Glucuronic acid, sulphate, glutathione, acetyl groups most commonly,** but also methyl, glycine, cysteine , or methionine
87
New cards
What are types of Phase II reactions?
1. **Glucuronic and acid conduction (UDP glucuronosyl transferase):**
2. **Sulphate conjugation (sulfotransferases):** phenols and alcohols conjugated to sulphates (SO4)
3. **Acytlation (N-acetyltransferases):** occurs in drugs with -NH2 group conjugated to COCH3
4. **Glutathione conjugation (glutathione S-transferase):** epoxides, arena oxides conjugated to glutathione (GSH)
88
New cards
What do the dynamic interactions among drug ADME determine
plasma concentration of drug and target site concentration
89
New cards
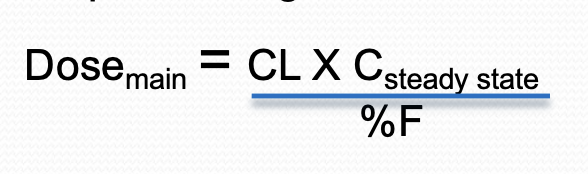
What are the 4 key parameters govern drug disposition (PK) and dosage regimen
* Bioavailability (%F)
* Volume of distribution (Vd)
* Clearance
* Elimination half-life(t1/2)
* Volume of distribution (Vd)
* Clearance
* Elimination half-life(t1/2)
90
New cards
Elimination of drug processes are usually
first-order processes
* half-life can be used to describe the rate of drug elimination (how frequently should I take that drug)
* half-life can be used to describe the rate of drug elimination (how frequently should I take that drug)
91
New cards
What is elimination half-life?
time requirednfor blood drug concentration to decrease by 50%
92
New cards
For clinical purposes, drug is considered essentially eliminated from blood after how many half-lives?
4-5
93
New cards
Therapeutic requirements often exceed …?
the duration of action following a single dose
94
New cards
Elimination half like (1/2) provides clinicians with
info about regarding frequency of drug administration needed to maintain blood drug levels in the therapeutic range
95
New cards
Elimination half life is a “___ ____” being dependant on other independent parameters
hybrid constant
96
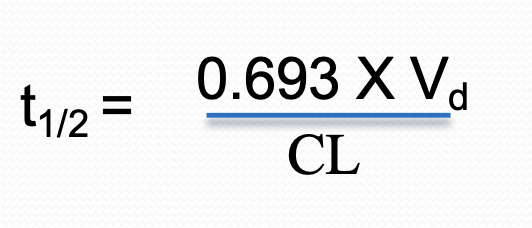
New cards
Elimination half life equation
97
New cards
Dosing regimes consist of:
* Dose(amount of drug given)
* Rotue of administration
* Frequency of administration eg. q12hrs
* Duration pf therapy ed. 3 days
* Rotue of administration
* Frequency of administration eg. q12hrs
* Duration pf therapy ed. 3 days
98
New cards
What is dosage?
amount of drugs given per body weight
99
New cards
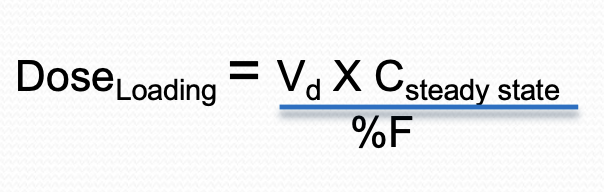
What is are loading doses?
can be used to acheive trarget therapeutic drug levels quickly
100
New cards
What are maintenance doses?
are given to maintain drug levels in the target therapeutic range