1. 8.1a Fungi & Fungal Diseases
1/14
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No study sessions yet.
15 Terms
What are key features of medically important fungi?
Fungi are eukaryotic __________ (obtain nutrients from organic matter) & they lack chlorophyll
Only a few species cause most human diseases
Some produce toxic __________ or allergenic __________
They are classified as true __________ or __________
Types include __________ infections (epidermis), __________ infections (deeper skin), and __________ infections (disseminated throughout the body)
Fungi are eukaryotic saprophytes (obtain nutrients from organic matter) & they lack chlorophyll
Only a few species cause most human diseases
Some produce toxic metabolites or allergenic spores
They are classified as true pathogens or opportunists
Types include cutaneous infections (epidermis), subcutaneous infections (deeper skin), and systemic infections (disseminated throughout the body)
What are key structural features of fungal cells?
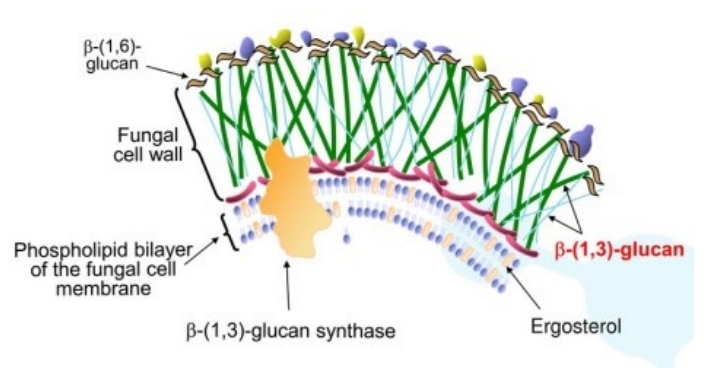
The cell membrane of fungi contains lipids, glycoproteins, and sterols, mainly __________ (differs from mammalian cells where __________ is predominant)
Fungi also have a cell wall composed of __________, __________, and __________
Nearly all fungi are strict __________
The cell membrane of fungi contains lipids, glycoproteins, and sterols, mainly ergosterol (differs from mammalian cells where cholesterol is predominant)
Fungi also have a cell wall composed of chitin, mannan, and glucan
Nearly all fungi are strict aerobes
What are the main forms of pathogenic fungi?
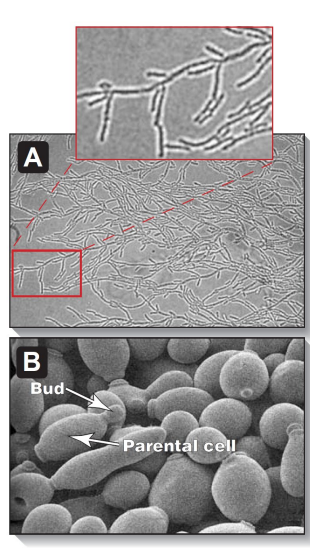
__________ – unicellular, ovoid/spherical, colonies resemble bacteria
__________ – multicellular, filamentous, form __________ (masses called __________)
Many fungi show __________ (exist as either mold or yeast)
Systemic fungal infection may exist as __________ in the environment and __________ in the body
Yeasts – unicellular, ovoid/spherical, colonies resemble bacteria
Molds – multicellular, filamentous, form hyphae (masses called mycelia)
Many fungi show dimorphism (exist as either mold or yeast)
Systemic fungal infection may exist as mold in the environment and yeast in the body
How do fungi grow and reproduce?
Fungi reproduce __________ or __________; yeasts divide by __________ forming __________, molds produce __________ on __________ asexually, and sexual reproduction forms __________ (haploid nuclei fuse and undergo meiosis to form __________)
Fungi reproduce asexually or sexually; yeasts divide by budding forming blastoconidia, molds produce conidia on conidiophores asexually, and sexual reproduction forms spores (haploid nuclei fuse and undergo meiosis to form ascospores
Where are fungi found and how is the host protected?
Fungi are part of natural human flora, mostly ________
Fungi are also in the environment, some ________ ________ , some ________ ; infection risk depends on ________ ________ and ________ ________ ________
Innate defence includes ________ , ________ ________ , and ________ ________ / ___ / ___ ________ ; ________ ________ ________ also protects
Fungi are part of natural human flora, mostly yeasts
Fungi are also in the environment, some geographically isolated , some ubiquitous ; infection risk depends on organism virulence and host immune status
Innate defence includes skin , mucosal surfaces , and skin turnover / pH / water availability ; bacterial host flora also protects
How are fungal infections diagnosed?
Diagnosis is based on ________ ________ and ________ ________
Direct examination uses ___ ________ ________ to dissolve tissue and ________ ________ to bind ________
________ ________ detect fungi in histopathology; morphology may identify species
________ can be used but may take weeks; ________ may start empirically in severe cases
________ can occur with ubiquitous fungi
________ or ________ ________ in body fluids may be detected, but antibodies are less discriminatory for opportunists
Diagnosis is based on case presentation and laboratory findings
Direct examination uses 10% potassium hydroxide to dissolve tissue and fluorescent dyes to bind chitin
Differential stains detect fungi in histopathology; morphology may identify species
Culture can be used but may take weeks; therapy may start empirically in severe cases
Contamination can occur with ubiquitous fungi
Antibodies or fungal antigens in body fluids may be detected, but antibodies are less discriminatory for opportunists
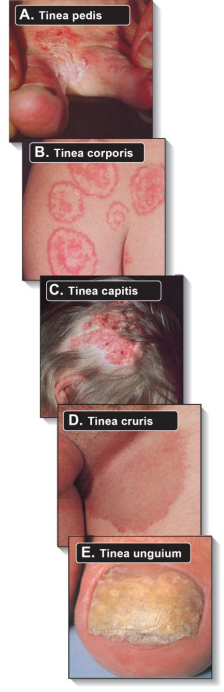
What are cutaneous fungal infections and key points? Caused by ________ (ringworm), termed ‘tinea’ by site: Tinea ________ (feet, “athlete’s foot”) , Tinea ________ (body, “ringworm”) , Tinea ________ (head) , Tinea ________ (crotch, “jock itch”) , Tinea ________ (nails, onychomycosis)
Dermatophytes not part of normal skin flora, found in ________ or ________ , survive in ________ ________
Genera include ________ , ________ , ________ ; most will not grow at ________
Caused by dermatophytes (ringworm), termed ‘tinea’ by site: Tinea pedis (feet, “athlete’s foot”) , Tinea corporis (body, “ringworm”) , Tinea capitis (head) , Tinea cruris (crotch, “jock itch”) , Tinea unguium (nails, onychomycosis)
Dermatophytes not part of normal skin flora, found in soil or animals , survive in wet locations
Genera include Microsporum , Trichophyton , Epidermophyton ; most will not grow at 37°C
How do cutaneous fungal infections develop and present?
Infection requires ________ ________ and a small ________ in the ________ – common in ________ and ________
Age/site: Tinea ________ common in children; Tinea ________ common in adults
Lesions show ________ pattern; spreads through ________ ________
Nail infection starts at ________ nail plates; hair infection may evade ________
Infection requires direct contact and a small break in the skin – common in feet and groin
Age/site: Tinea capitis common in children; Tinea pedis common in adults
Lesions show ring pattern; spreads through stratum corneum
Nail infection starts at lateral nail plates; hair infection may evade hair shaft

What are the key clinical features and treatment of cutaneous fungal infections?
Features are due to ________ response to infection
Diagnosis: skin scrapings, ________ ________ treatment, observe ________ ________ ________ under microscope; culture identifies ________
Usually treated with ________ antifungal creams/lotions (________ or )
Nail infections require ________ treatment ( or ________) for ________ months
Relapses common in Tinea ________ and Tinea ________; prompt treatment necessary
Features are due to inflammatory response to infection
Diagnosis: skin scrapings, potassium hydroxide treatment, observe branching septate hyphae under microscope; culture identifies organism
Usually treated with topical antifungal creams/lotions (allylamines or azoles)
Nail infections require systemic treatment (terbinafine or itraconazole) for 3–4 months
Relapses common in Tinea pedis and Tinea cruris; prompt treatment necessary
Key features and risk factors of Candidiasis?
Candida are _______ / _______ yeasts; may form _______
Main species: _______ _______ ; colonises __ ______ , _______ , _____
Promoted by _______-______ _______ , _______ _______ , _______ _______ _______
Candida are round / oval yeasts; may form hyphae
Main species: Candida albicans ; colonises GI tract, vagina, skin
Promoted by broad-spectrum antibiotics, immunocompromised individuals, central venous catheters
Key features of mucosal and vaginal Candidiasis?
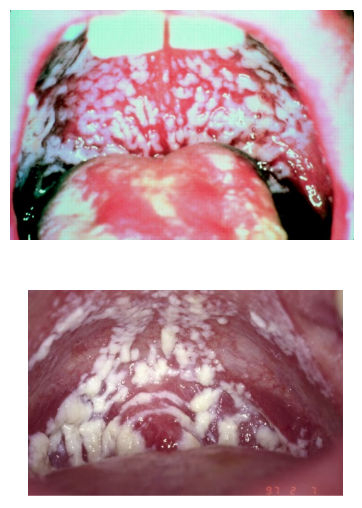
Mucosal candidiasis: _______ _______ on _______ and _______ ; called _______
Proliferates in _______ _______ areas
HIV patients: _______ _______ , may spread to _______ ; indicates ____
Diagnosis: scrapings of _______ _______ ; & organism _______
Vaginal candidiasis symptoms: _______ and _______ _______ , with _______
Mucosal candidiasis: white plaques on mouth and throat ; called thrush
Proliferates in warm moist areas
HIV patients: oral candidiasis, may spread to oesophagus ; indicates AIDS
Diagnosis: scrapings of budding yeast ; & organism cultured
Vaginal candidiasis symptoms: itching and burning pain, with discharge
What organs does candidiasis involve and how is it treated?
Systemic – GI tract, liver, kidneys, spleen; fever, sepsis, or organ dysfunction; requires tissue biopsy and culture.
Disseminated (spread through bloodstream).
Treatment: echinocandin or fluconazole; severe – amphotericin B.
Oral – miconazole; severe – fluconazole.
Vaginal – intravaginal clotrimazole or oral fluconazole; vulval symptoms – topical imidazole.
What is Aspergillosis, who is at risk, and how does it infect?
Aspergillus fumigatus and A. flavus – filamentous fungi, not normal flora.
At-risk: neutropenic, on corticosteroids, on immunosuppressants, transplant patients.
Infection: inhaled spores → hyphae invade tissues and blood vessels; invasive infection only occurs if profound immunocompromise in individuals.
What are the clinical features of aspergillosis and possible dissemination?
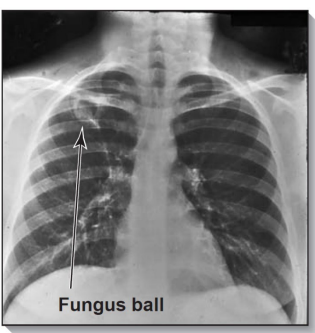
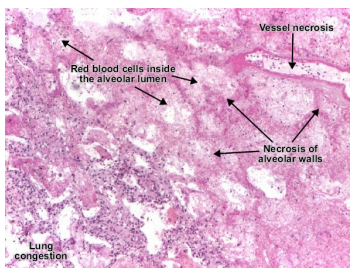
Initial – pulmonary or sinus infection; histopathology – haemorrhagic infarction (tissue death due to blocked blood vessels), necrosis, branching septate hyphae (fungal filaments with cross-walls)
Pulmonary – fever, chest pain, cough, hemoptysis (coughing up blood), shortness of breath; chest X-ray/CT – nodules, haemorrhage, cavitation.
Sinus – acute facial pain.
Dissemination (blood vessel invasion) – necrotic skin lesions, brain abscess (stroke, seizures, altered mental state).
What are the main treatments and preventive measures for aspergillosis, and who is mainly at risk?
Amphotericin B or voriconazole; itraconazole if intolerant. High-risk patients: filtered air and antifungal prophylaxis (voriconazole or posaconazole).
Transplant patients at risk, especially stem cell.