Micro Lab Final Quiz
0.0(0)
Card Sorting
1/193
Last updated 8:36 PM on 4/28/23
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
194 Terms
1
New cards
What are the true pathogens of the enterobacteria?
S. typhi and S. dysenteriae
2
New cards
What is enterobacteria
gram neg rods that are frequently found in the intestinal tract
3
New cards
There are 4 major diseases caused by enterobacteria. what are they and what causes them
1. dysentery (shigella dysenteriae)
2. typhoid (salmonella typhi)
3. cholera (vibrio cholerae)
4. travelers diarrhea (escherichia coli)
4
New cards
what is a facultative anaerobe in the context of enterobacteria
a bacterium that can grow in the anaerobic intestinal tract but also in the presence of oxygen
5
New cards
what is selective medium
medium to prevent growth of some species but permitting others to thrive
6
New cards
what is differential medium
medium that enables the investigator to distinguish one species from another. this is usually done through use of chemical reaction which causes the color of medium or colonies to change
7
New cards
what is MacConkey agar?
lactose fermenting organisms produce red colonies on this plate medium. gram pos bacteria are inhibited. ingredients include lactose, bile salts, and neutral red (pH indicator).
8
New cards
what is XLD agar? What colors would you expect to see using this dye and what do those colors indicate? What does this kind of medium contain?
abbreviation for Xylose Lysine Deoxycholate agar. organisms that ferment the constituent carbohydrates produce yellow and red colonies on this plate medium. if lysin decarboxylase is produced, colonies are red. colonies may be black if H2S is produced. the medium contains xylose, lactose, sucrose, phenol red (pH indicator), bile salts, lysin and ferric ammonium citrate (H2S detection)
9
New cards
What is TSI agar? What colors would you expect to see using this dye and what do those colors indicate? What does this kind of medium contain?
abbreviation for triple sugar iron agar; triple sugar iron agar is used in the form of a slant tube. if an organism can use lactose or sucrose, the entire tube will turn yellow from the acid produced. Gas may push the agar up the tube or form large bubbles. If only glucose is used, the butt of the agar slant tube will turn yellow but the slant itself will remain red. an organism that produces H2S will cause the formation of of a black pigment in the tube. Besides the sugars, the medium contains phenol red (pH indicator) and iron salts (H2S detection)
10
New cards
What is Simmons Citrate agar
this medium will turn blue if an inoculated organism can use citrate. the medium includes citrate and thymol blue (pH indicator) and is prepared as an agar slant
11
New cards
What is urea agar?
Organisms that can break down urea can be recognized by changing the color of this medium. Phenol red is used as an indicator
12
New cards
What is iron agar?
this medium is for the detection of H2S produced by some species
13
New cards
What is fermentation broth?
this is a test to determine if an organism can use a specific carbohydrate.
14
New cards
What is decarboxylase broth
this medium can detect the ability to produce decarboxylases by a color change of the tube
15
New cards
what is motility medium?
if growth spreads from a straight vertical stab line of inoculation, the bacterium may be motile
16
New cards
what is enterotube II?
this is a multiple test medium made by Roche Diagnostics that can assay for several qualities at once
17
New cards
What is the biolog automated redox-based system?
to identify the genus and species the system assays the ability of an organism to oxidize a panel of 95 sources in a 96 well microplate
18
New cards
How does the biolog automated redox-based system testing work?
if an organism being tested uses a specific carbon source, this is detected by the redox dye, tetrazolium violet.
19
New cards
The ___ microplate panel of carbon sources is used for gram neg _____ bacteria. These species include… (hint: 3 things)
GN, aerobic
enteric, non-fermenter, fastidious species
enteric, non-fermenter, fastidious species
20
New cards
The ____ microplate panel of carbon sources is used for gram pos ______ bacteria.
GP, aerobic
21
New cards
The data for the biolog automated redox-based system software contains ___ gram neg species/groups and over ___ gram pos species/groups.
503; 200
22
New cards
Try to describe in one or two sentences the basis behind identifying of a gram neg rod
The basis in which the gram-negative rod can be identified is based on two main criteria: what products are made by the bacteria and what substrates are needed for processes conducted within the bacteria. Bacterial species have a unique combination of products and substrates, and the wide variety of tests can be used to pinpoint exactly which species the sample is.
23
New cards
Why must the tube media be inoculated with a pure strain when identifying gram neg rods?
The sample that is used must be a pure strain. If the sample contains more than one strain of bacteria, the inaccuracy of the tests will increase, and it may lead to an incorrect conclusion. For example, some strains of Klebsiella can produce indole while others cannot. Therefore, for the indole test to be accurate, the sample must be a pure strain so the appropriate color change occurs.
24
New cards
What are diseases that E coli causes
While a lot of E. coli are found in the intestinal tracts of animals and humans, some of these bacteria can be the cause of various serious bacterial infections. Such types of E. coli are known to cause diarrhea, but others can cause UTIs, bloodstream infections, respiratory tract infections, and pneumonia.
25
New cards
What are diseases that K pneumoniae causes
Like E. coli, K. pneumoniae also lives in the human intestinal tract, but when this bacteria goes to different areas of the body it is known to cause a variety of infections, especially in a clinical setting. Pneumonia, bloodstream infections, UTIs, meningitis, and wound or surgical site infections are just some of the illnesses that are seen because of K. pneumoniae.
26
New cards
What are diseases that P vulgaris causes
Similarly, P. vulgaris is found in the human intestinal tract and is commonly known to cause infections of the bloodstream, urinary tract, respiratory tract, burns, and wounds.
27
New cards
What are diseases that P aeruginosa causes?
P. aeruginosa is commonly found in places in the surrounding environment like water, and often causes human infections in a clinical setting after surgeries are performed. Infections of the blood and lungs are some of the most common while UTIs, bone and joint infections, gastrointestinal infections, dermatitis, septicemia, and pneumonia can also arise.
28
New cards
What is a phage?
a virus that infects bacteria
29
New cards
What is a phage
a virus that infects bacteria
30
New cards
what is the purpose of phage titration
2 things: measure abundance and make more viruses
31
New cards
What is a plaque
infective center (clear area) caused by a phage on a lawn of bacteria on a plate. Contains thousands of new phage. in this area the bacteria have been killed
32
New cards
what is a plaque forming unit (PFU)
a phage particle that is capable of forming a plaque on a lawn of bacteria
33
New cards
what are methods to measure virus concentration
1. phage titration or plaque assay
2. routine test dilution (RTD)
3. electron microscopy (EM)
4. hemagglutination titration
5. dose to infect 50% of subjects (ID50)
6. dose to kill 50% of subjects (LD50)
34
New cards
Let’s say we have a tube that is going to be used in a phage titration series. What do we expect to find in that broth?
0\.2 mL of bacterial cells
0\.1 mL of phage stock or broth from another tube in the set
9\.7 mL of sterile broth
0\.1 mL of phage stock or broth from another tube in the set
9\.7 mL of sterile broth
35
New cards
We need to wait for a period of time (an hour as Graves said although the packet says incubate for 20 min so remember both) before we plate the inoculated tubes. why?
the phages need time to invade the bacteria
36
New cards
what is the procedure for plating the broth tubes in phage titration?
after incubation of the tubes, add 4 mL of melted 45 deg C agar to one tube at a time, mix and pour evenly over the top of a fresh agar plate.
37
New cards
What is the titer?
concentration of a solution determined by titration
38
New cards
We want to see how many plaques on our plates?
30-300
39
New cards
What is the equation used to determine the concentration for phage titrations?
\# plaques \* 10 \* 1/tube dilution = titer in PFU/mL
40
New cards
Every phage particle will not make a plaque. Why?
1. the bacteria could have been attacked by too many phage particles, and in such instances, a plaque does not form.
2. the phage particles simply could not have been able to find a bacteria to infect, especially because of the limited amount of bacteria available on the plate.
3. It is also possible that the particular virus used was unable to attach to the bacteria provided, E. coli.
41
New cards
1 plaque is one virus attaching to one bacterial cell every time. T or F?
False: similar to the counting inaccuracy with colony count assay, some of the bacteria could have been infected by more than one virus, but only one plaque results.
42
New cards
There are no plaques but on the zero dilution plate. why?
The zero dilution plate consisted of the highest concentration of phage particles because it was from the phage stock. The high quantity of phage led to the creation of too many plaques, causing them to overlap. Therefore when observing the zero dilution plate, you cant decipher where one plaque begins and ends because it is the edge of the bacteria growth that defines what a plaque is.
43
New cards
There are colonies on the zero dilution plate. what are they?
mutants of the E. coli bacteria. The phage infects the most evolutionarily fit bacteria because it would be more beneficial for the phage. Consequently, the less favored mutants of E. coli are actually the colonies that survived and are seen on the zero dilution plate.
44
New cards
Why do the plaques stop growing?
because the bacteria stop growing
45
New cards
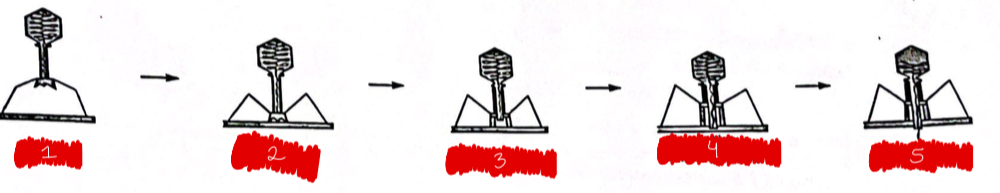
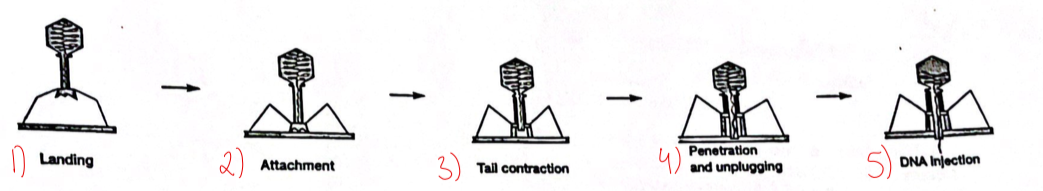
label the figure
see attached
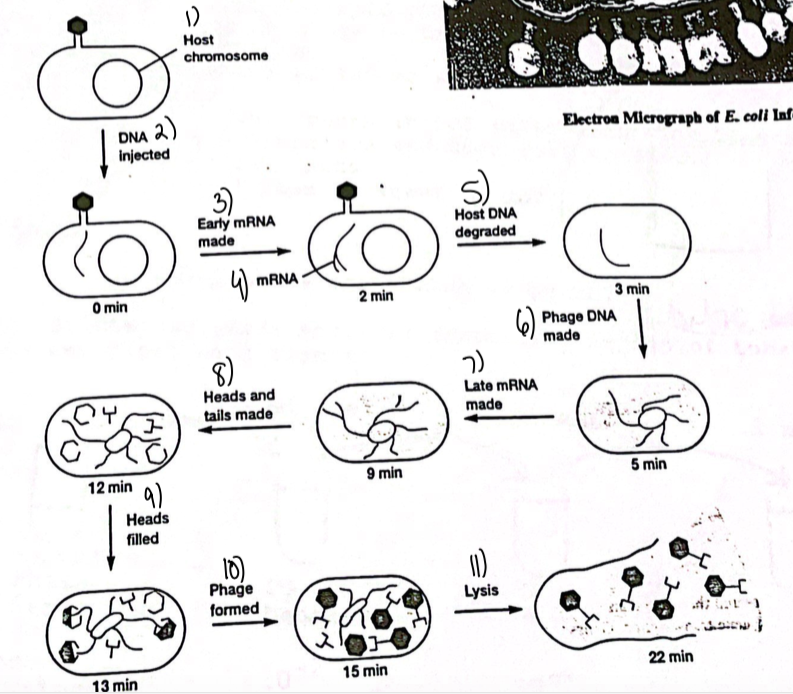
46
New cards
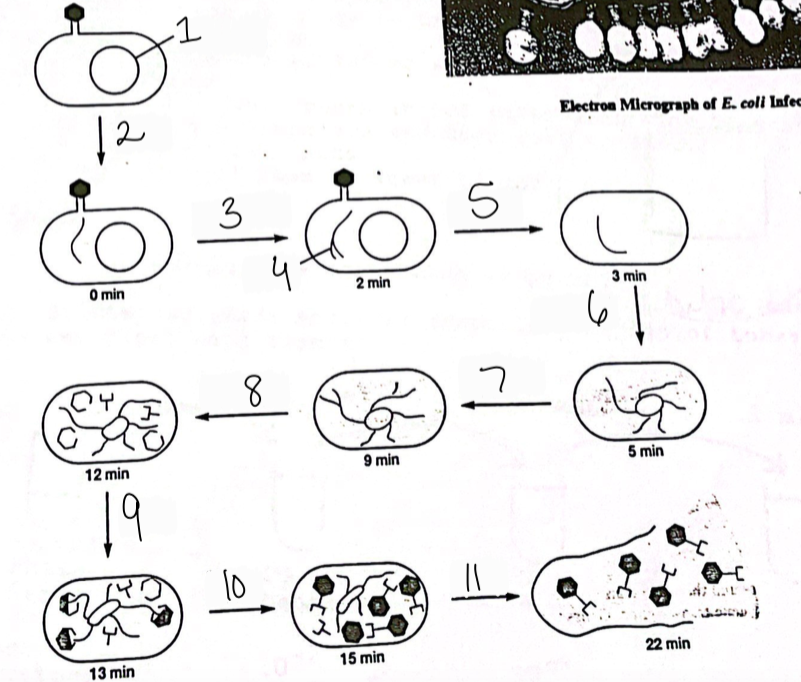
label the figure
see attached
47
New cards
What is an antibiotic?
a chemical synthesized by a microbe that will kill or inhibit other microbes
48
New cards
Name 4 producers of antibiotics
streptomyces, bacillus, penicillium, cephalosporium
49
New cards
Describe the tube dilution antibiotic sensitivity assay
a known concentration of antibiotic is diluted in a twofold tube dilution series and a drop of test organism is added to each tube to observe if good growth will occur.
50
New cards
In the tube dilution antibiotic sensitivity assay, the antibiotic conc in the highest dilution tube that shows no culture growth is called what?
minimum inhibitory concentration (MIC)
51
New cards
Who are the scientists behind the disc method of determining antibiotic sensitivity?
Kirby and Bauer
52
New cards
How do you conduct the disc method of determining antibiotic sensitivity? What type of agar is used?
paper discs containing antibiotic are used to test for inhibition of bacterial growth in the vicinity of the disc of an agar plate. For technique standardization, Mueller-Hinton agar is used for plates. To determine if an isolate is resistant or sensitive to an antibiotic, growth inhibition zone diameter is compared with values produced by reference organisms of the some species on a standard table.
53
New cards
In the disc method of determining antibiotic sensitivity, two antibiotics that produce the same inhibition zone diameter have the same equal efficacy. T or F?
False; they do not have equal efficacy because of many factors such as diffusion rates
54
New cards
Why does Graves think August von Wasserman is a bigshot?
He was physician that came up with the complement fixation test, the first definitive test for syphilis. The test was also used for other diseases.
55
New cards
in our tube dilution test for antibiotics, what was the minimum inhibitory conc (MIC)?
5 micrograms/mL
56
New cards
In our tube dilution test for antibiotics, there were 10 wasserman tubes in total. The 10th tube was a control. Why was the 10th tube a control?
there was no antibiotics
57
New cards
Would the MIC of penicillin or streptomycin be the same as that for tetracycline? Why or why not?
They would not be the same. Each of the antibiotics are tailored toward a specific pathogen, so the MIC is individualized to the antibiotic.
58
New cards
In the treatment of patients, why would it be important to know the MIC of an antibiotic used to cure an infection?
need to know the correct dosage
59
New cards
Which test is more quantitative for antibiotic sensitivity: tube dilution or disc? Why?
The tube dilution test is the more quantitative test in comparison to the antibiotic disc assay. For the antibiotic disc assay, the inhibition zones are measured. However, the inhibition zones are essentially a description of the ==effect== of the antibiotic on the bacteria. With the tube dilution test on the other hand, the ==concentration== of the antibiotic is being measured.
60
New cards
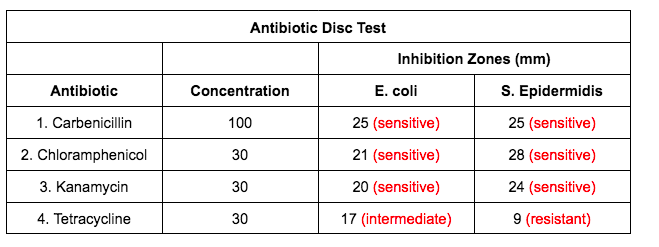
In the disc assay for antibiotic sensitivity, what 4 antibiotics were used?
1. Carbenicillin
2. Chloramphenicol
3. Kanamycin
4. Tetracycline
61
New cards
In the disc assay for antibiotic sensitivity, what measures sensitivity?
the zone of inhibition
62
New cards
Of the 4 antibiotics used in the disc assay, what was E. coli most and least sensitive to? How about S epidermidis?
Carbenicillin- most sens (E.coli)
Tetracycline - least sens (E. coli)
Chloramphenicol - most sens (SE)
Tetracycline - least sens (SE)
Tetracycline - least sens (E. coli)
Chloramphenicol - most sens (SE)
Tetracycline - least sens (SE)
63
New cards
E coli and S epidermidis did not show the same antibiotic sensitivities. why? (hint: 2 reasons)
1. the antibiotic is working against completely different types of bacteria. Therefore, the effectiveness of the antibiotic will depend on whether its antibacterial properties will be successful against the bacteria of interest.
2. E. coli is gram negative which indicates a thin peptidoglycan layer in the cell wall. On other hand, S. epidermidis is gram positive indicating a thick peptidoglycan layer in the cell wall. The ability of the different antibiotics to penetrate the structurally different cell walls will vary and thus the inhibition zone will also vary.
64
New cards
what is the difference between bactericidal and bacteriostatic antibiotics?
Bactericidal antibiotics are medications that destroy the bacteria. They differ from bacteriostatic antibiotics that suppress bacterial growth by preventing their ability to move on from the stationary growth phase in their life cycles.
65
New cards
What is pencillinase’s function?
Penicillinase is an enzyme produced by certain kinds of bacteria that provides the ability to inactivate penicillin. If a strain of bacteria can make penicillinase is exposed to the antibiotic penicillin, it will begin to produce and secrete penicillinase extracellularly which will exit the bacterial cell and begin the degradation of penicillin by the means of hydrolyzing the bonds that make up penicillin, ultimately inactivating the antibiotic.
66
New cards
How are plasmids associated with the efficacy of antibiotic therapy?
Plasmids are associated with a loss of efficacy of antibiotic therapy. If one bacterium undergoes a mutation that allows antibiotic resistance, that ability can move throughout the rest of the bacteria through horizontal gene transfer. One of the mechanisms in which asexual bacteria obtain genetic diversity is through conjugation, a gene transfer event where a piece of DNA is transferred from one bacterium to another through a tube connection. The piece of DNA is called a plasmid. This plasmid is then transcribed and translated to obtain the antibiotic resistance and can then transfer to another bacteria to do the same.
67
New cards
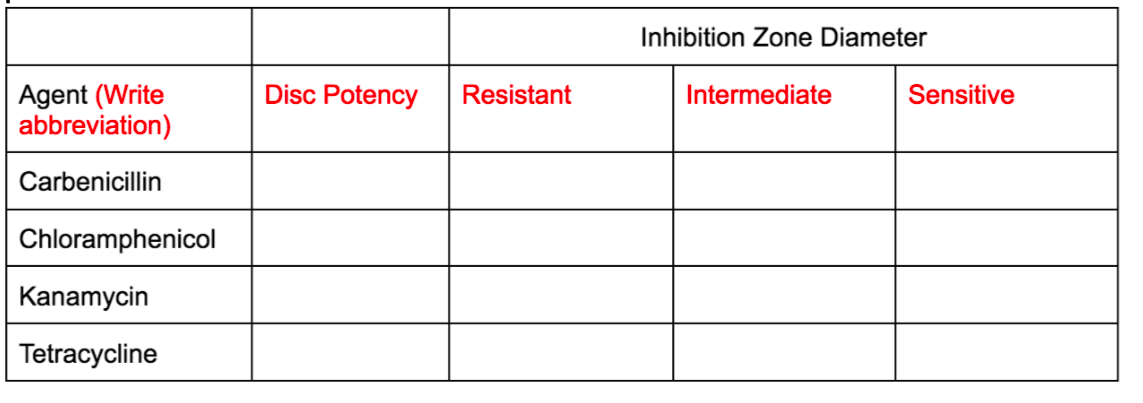
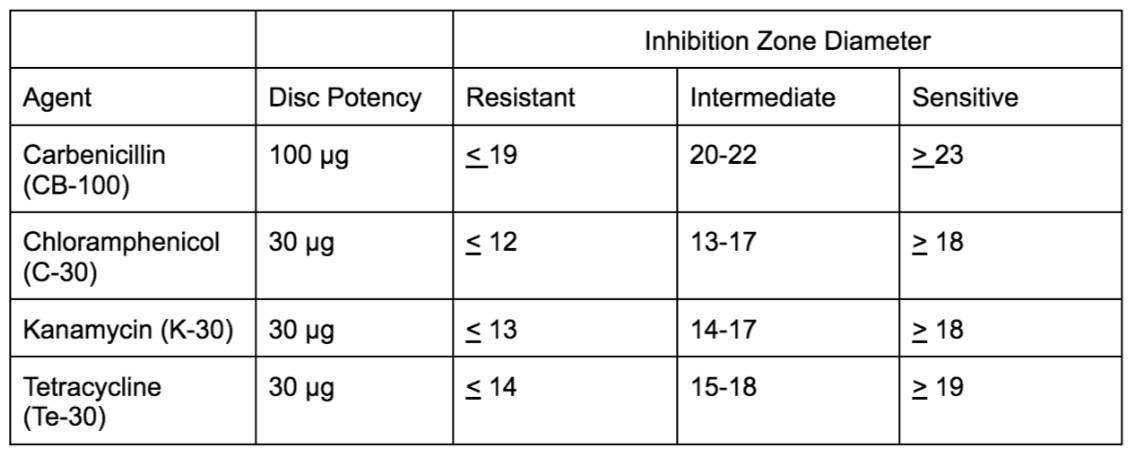
Fill in the attached chart
see attached
68
New cards
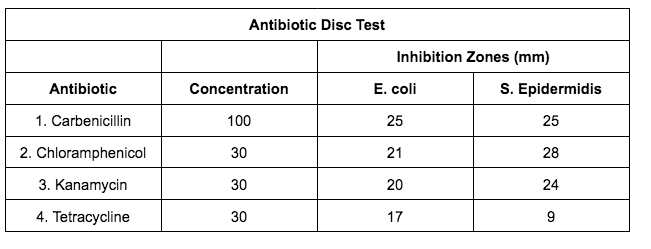
We have divided inhibition zone diameter ranges into 3 arbitrary categories: resistant, intermediate, sensitive. Let’s say we ran the exp and got the attached values. Based on the values attached and knowing the ranges for each of the 4 antibiotics, in which of the 3 categories would you place each diameter?
see attached
69
New cards
What is a bacteriophage? What is another name for it?
aka pha
70
New cards
What is a transposon
A small piece of linear DNA that contains a few genes that has the ability to replicate and jump into a different region of DNA The
71
New cards
Transposons were first discovered in what??
corn
72
New cards
What is a mutation?
a change in DNA sequence
73
New cards
What is a mutagen?
an agent that causes mutations
74
New cards
What is a mutant?
an organism that contains a mutation
75
New cards
The phage used in the transposon mutagenesis had a very important gene called what which had what ability?
Tn10, tetracycline resistance
76
New cards
Humans can make about 100 million antibodies, but we only have 30,000 genes. How is that possible?
transposons or jumping DNA creates various combinations even in a relatively small genome
77
New cards
Within the broth culture used in the transposon mutagenesis, there was E. coli and what else? What was its purpose?
MgSO4. Cells have a neg charge, and phages have a neg charge. Magnesium ion acts as mediator to allow interaction.
78
New cards
Within the BHI plate used in the transposon mutagenesis, there were 2 important substances. what are they? explain why they are important?
tetracycline - ensures that the only colonies on the plate are those that have antibiotic resistance
Tetrasodium pyrophosphate- chelator (a substance that binds to metal ions such as magnesium ions)
Tetrasodium pyrophosphate- chelator (a substance that binds to metal ions such as magnesium ions)
79
New cards
We basically had three plates in the transposon mutagenesis. Explain what was on each plate and whether each plate would have colonies or not. Also explain why there would be colony presence or absence.
1) phage plate - no colonies because although they have Tn10, they have no host bacteria and no machinery to make use of the Tn10 gene.
2) bacterial cell plate - no colonies because the E. coli are sensitive to tetracycline
3) phage + bacterial cell plate - colonies are present because Tn10 will be inserted into the host bacterial cell from the phage where the bacterial machinery will transcribe and trnal
2) bacterial cell plate - no colonies because the E. coli are sensitive to tetracycline
3) phage + bacterial cell plate - colonies are present because Tn10 will be inserted into the host bacterial cell from the phage where the bacterial machinery will transcribe and trnal
80
New cards
It is possible that the transposon can damage the gene it is jumping into. T or F?
true
81
New cards
What is transposase?
It is a enzymatic protein that facilitates the jumping of transposons
82
New cards
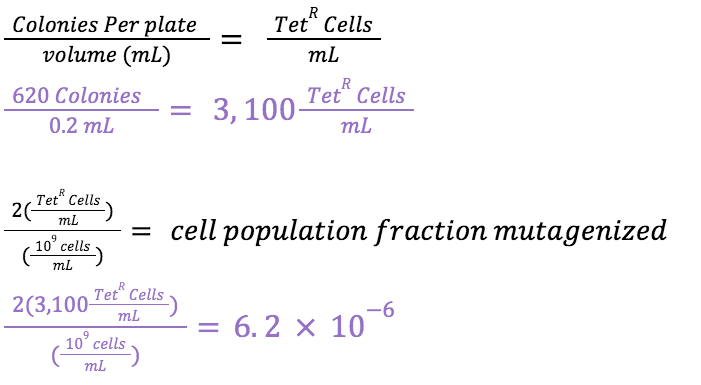
In the transposon mutagenesis lab, we assumed that there are _____ cells per mL in the original culture when calculating the fraction that were mutagenized.
10^9
83
New cards
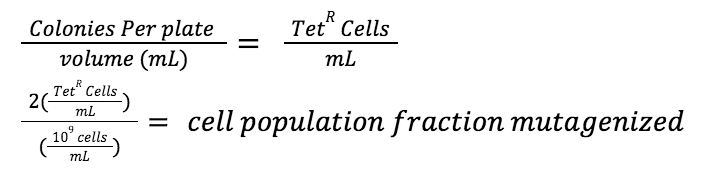
What is formula to calculate the cell population fraction mutagenized?
See attached
84
New cards
Why are we multiplying the tetR cell concentration by 2 in the ell population fraction mutagenized formula?
multiplication by 2 is performed bc cells were diluted with an equal volume of phage
85
New cards
Let’s say we conducted the transposon mutagenesis experiment, and the phage + cell plate has 620 colonies. What would the cell population fraction mutagenized be?
see attached
86
New cards
In the transposon mutagenesis experiment, why are the tetracycline resistant cells mutants?
\
The tetracycline resistant cells are mutants because they can grow on the plates which contain the tetracycline antibiotic, as opposed to no growth observed on the plate with only cells. The tetracycline resistant cells are specifically deemed to be mutants because the transposon, which carries the Tn10 gene for tetracycline resistance, makes an insertion mutation when it jumped into the cellular DNA.
The tetracycline resistant cells are mutants because they can grow on the plates which contain the tetracycline antibiotic, as opposed to no growth observed on the plate with only cells. The tetracycline resistant cells are specifically deemed to be mutants because the transposon, which carries the Tn10 gene for tetracycline resistance, makes an insertion mutation when it jumped into the cellular DNA.
87
New cards
In the transposon mutagenesis experiment, why do the tetracycline resistant cells grow if they are now mutants?
\
The tetracycline resistant cells still grow if they are mutants because the transposon contains the Tn10 gene which is the gene for tetracycline resistance, enabling the cells to now grow on the plate with tetracycline antibiotic.
The tetracycline resistant cells still grow if they are mutants because the transposon contains the Tn10 gene which is the gene for tetracycline resistance, enabling the cells to now grow on the plate with tetracycline antibiotic.
88
New cards
What is the general purpose of the phage in the transposon mutagenesis experiment?
The general purpose of the phage in this experiment is to carry the Tn10 gene into the cell.
\
\
\
\
89
New cards
What are common mutagenic mutagenic agents (Hint: 5 answers)
1) tobacco products
2) radioactive substances
3) X-rays
4) UV radiation
5) certain chemicals
2) radioactive substances
3) X-rays
4) UV radiation
5) certain chemicals
90
New cards
Definition of meta is…
after or beyond Wh
91
New cards
what is the definition of genomics?
study of the package of hereditary material inside an organismWh
92
New cards
what is the definition of metagenomics?
study of deoxyribonucleic acid (DNA) isolated from env samples. sequence of a small region of the 16 S rRNA gene is used to recognize microorganisms and place them in clustersWha
93
New cards
what is bioinformatics?
application of computer science and statistics to analyze large quantities of biological data
94
New cards
What does de novo mean?
a procedure that results in conclusions about characteristics by computation
95
New cards
What is polymerase chain reaction?
a technique used to copy a segment of DNA many fold
96
New cards
What is DNA sequencing
a method to discover the order of bases in a DNA molecule
97
New cards
What is next generation sequencing? what is another name for it?
aka high-throughput sequencing; contemporary nucleic acid sequencing that is fast and inexpensive
98
New cards
What is Alumina DNA Sequencing
a next generation sequencing technique that uses reversible dye terminators and engineered polymerases. clonal synthesis of DNA on a surface results in the formation of DNA clusters. Photographs record fluorescently labeled nucleotides in the sequence
99
New cards
What is QIIME?
Quantitative Insights Into Microbial Ecology; software for analysis of DNA sequence data (operational taxonomic units, taxonomy, and statistical figures).
100
New cards
What is OTU?
Operational taxonomic unit; closely related group of subjects. sequences of variable region four (V4) for the 16 S rRNA gene are used to evaluate similarity.