Posterior thigh
1/19
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
20 Terms
Posterior Thigh:
Is defined as the area between the gluteal fold (posteriorly) and the knee joint. (popliteal fossa)
The Hamstring Muscles
Biceps femoris
Semimembranous
Semitendinous
Biceps Femoris
Origin: Long head:Ischial tuberosity (long head & sacrotuberous ligament) Short head: femur (linea aspera and lateral supracondylar line of femur)
Insertion: Head of the fibula via a common tendon.(lateral aspect)
Action: Main function: Extends thigh and flexes leg at the knee joint (flexes the knee) Also: laterally rotates leg.
Nerve supply: Sciatic nerve (long –head= tibial division, short head = common fibular division.)
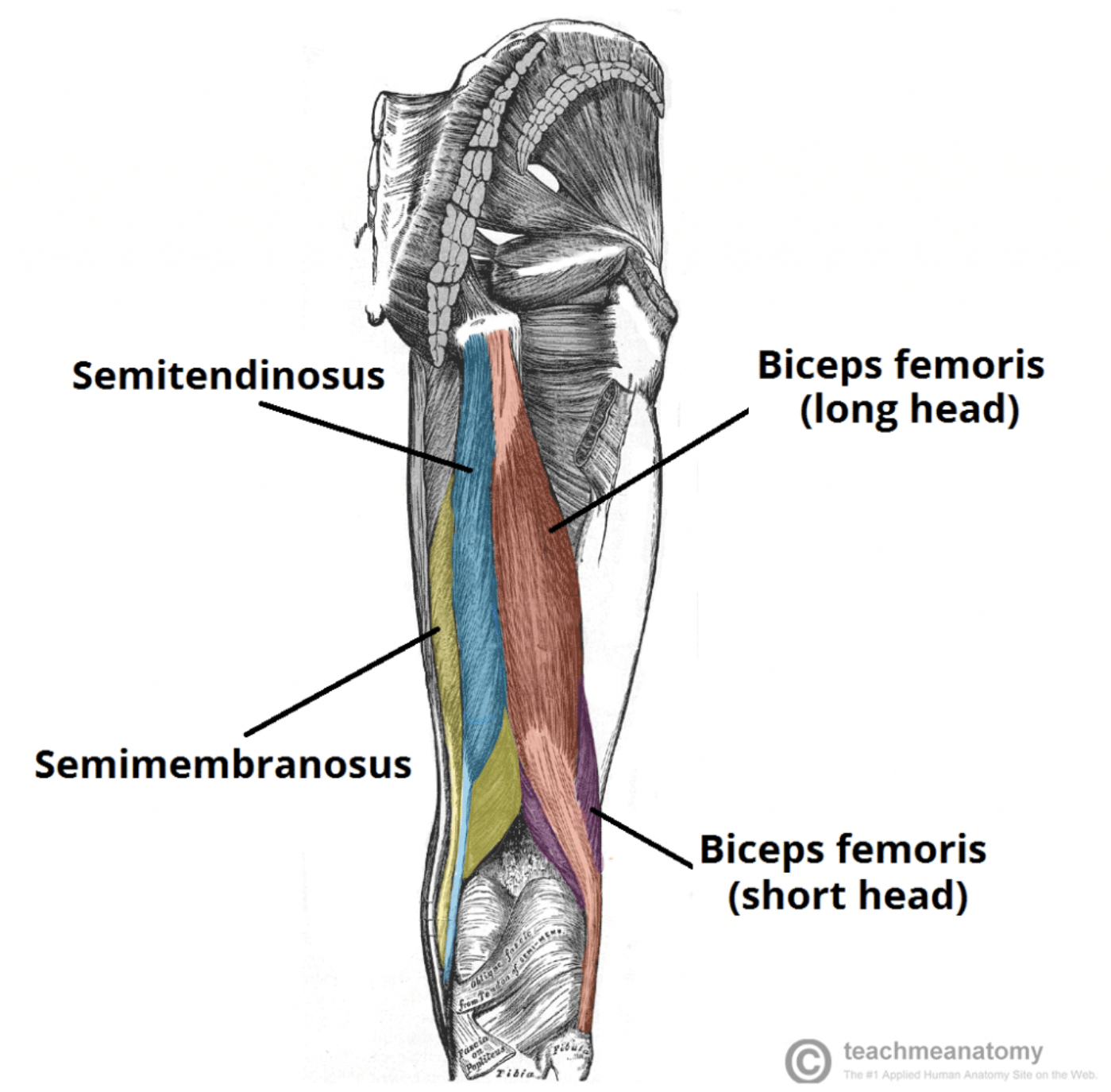
Semimembranosus
Origin: Ischial tuberosity (superior-lateral impression)
Insertion: Tibia (medial condyle).
Action: Extends thigh and flexes leg (at the knee), medially rotates leg.
Nerve supply: Sciatic nerve (tibial division)
Semitendinosus
Origin: Ischial tuberosity. (Posteromedial impression)
Insertion: Tibia (medial shaft) (proximal end of tibia below medial condyle-via pes anserinus)
Action: Extends thigh and flexes leg (at the knee), medially rotates leg.
Nerve supply: Sciatic nerve-Tibial division
Pes Anserinus
the conjoined tendons of the sartorius, gracilis & semitendinosus” muscles

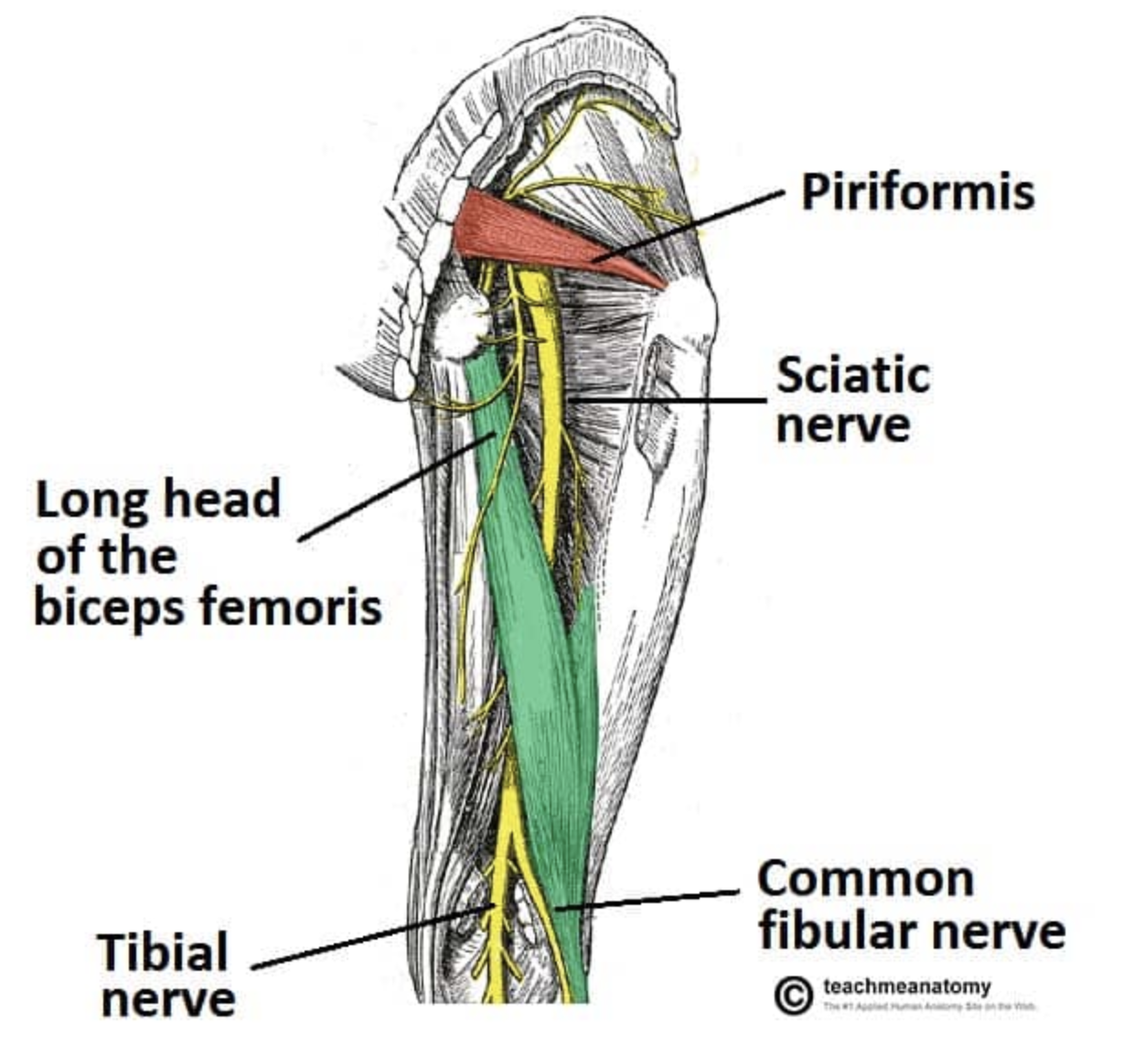
Sciatic nerve ( formation)
contains both anterior and posterior divisions of the lumbosacral plexus
The anterior divisions- run in the medial side of the nerve= later becomes= tibial nerve
The posterior division fibers run in the lateral side = later becomes= common fibular (peroneal) nerve
sciatic nerve is the largest and longest nerve in the body.
Runs from the sacral plexus where it emerges from the pelvis through the greater sciatic notch of the os coxae and runs along the posterior thigh
Just superior to the popliteal fossa the sciatic nerve splits into two nerves: a. Tibial nerve b. Common fibular nerve
Posterior Thigh-blood supply
1) Inferior gluteal artery (upper posterior compartment) (branch of anterior trunk of the internal iliac artery)
2)Perforating branches of the profunda femoris (a major collateral branch of the femoral artery and part of the anterior compartment of thigh, but helps supply the posterior thigh muscles
Lower Limb Blood Suppy- Arterial
Femoral artery becomes the popliteal artery in the popliteal fossa, and then divides into the anterior and posterior tibial arteries down the back of the leg.
The femoral artery itself crosses the adductor hiatus to enter the posterior compartment at the level of the popliteal fossa , giving branches that supply the knee
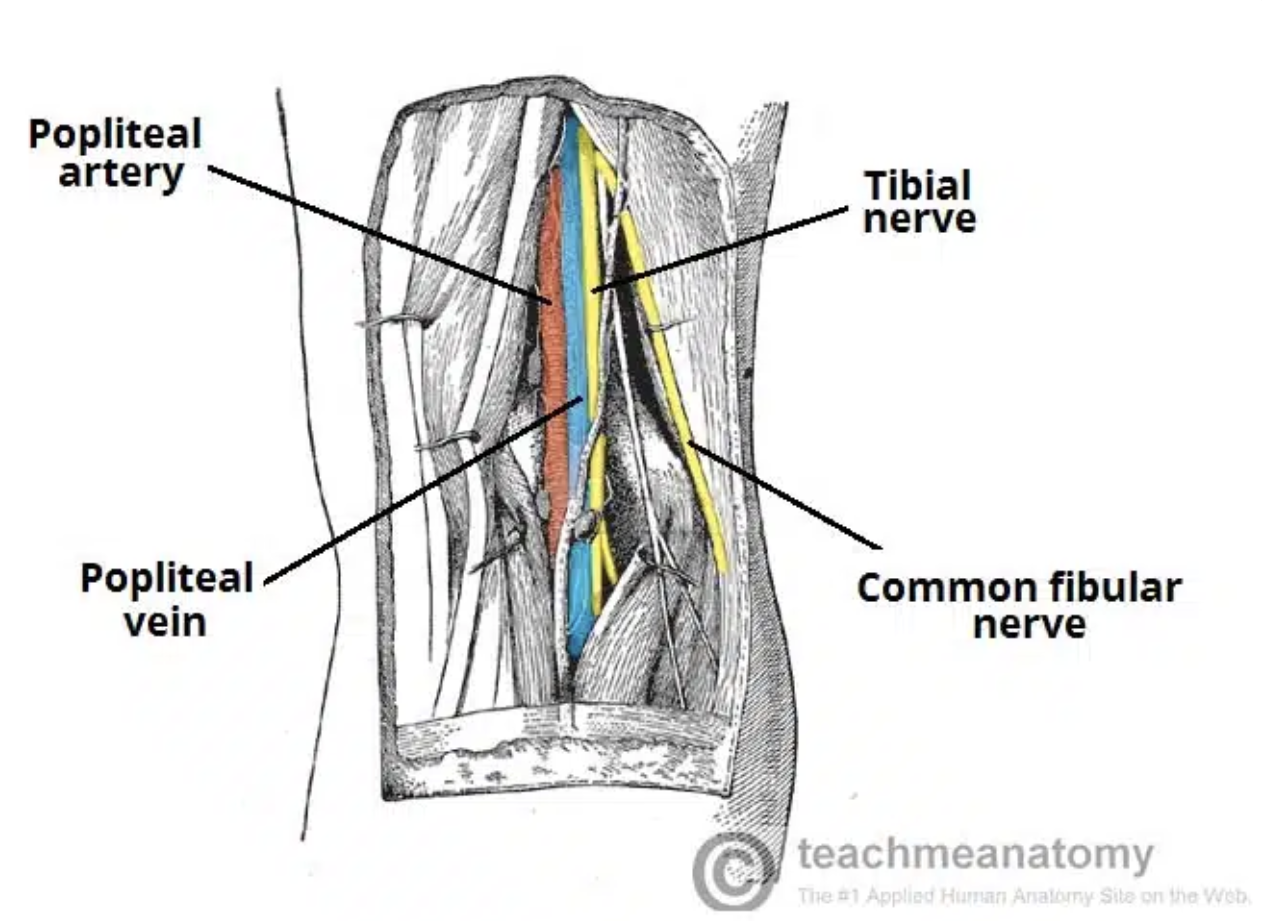
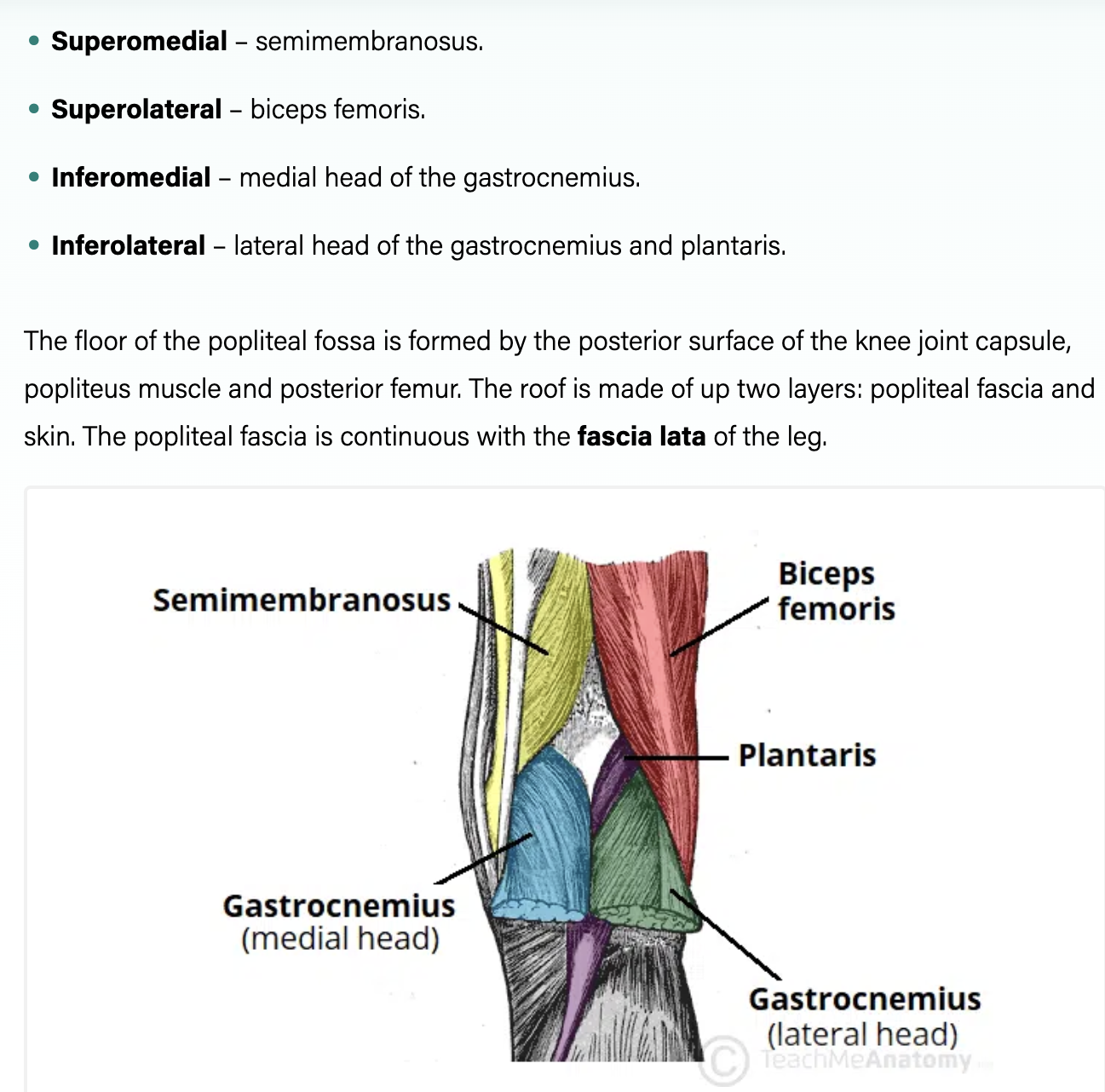
Popliteal Fossa
Boundaries:
Superior:
Medial - semitendinosus and semimebranosus
Lateral - biceps femoris
Inferior:
Medial - medial head of gastrocnemius
Lateral - plantaris and lateral head of gastrocnemius
Floor: capsule of the knee joint, femur, tibia, popliteus muscle
Roof: fascia and skin
Contents: Popliteal artery and vein, Tibial and common fibular (peroneal) nerves
Tibia and Fibula
Tibia weight bearing
Fibula non-weight bearing
Fibula stabilizes the ankle joint
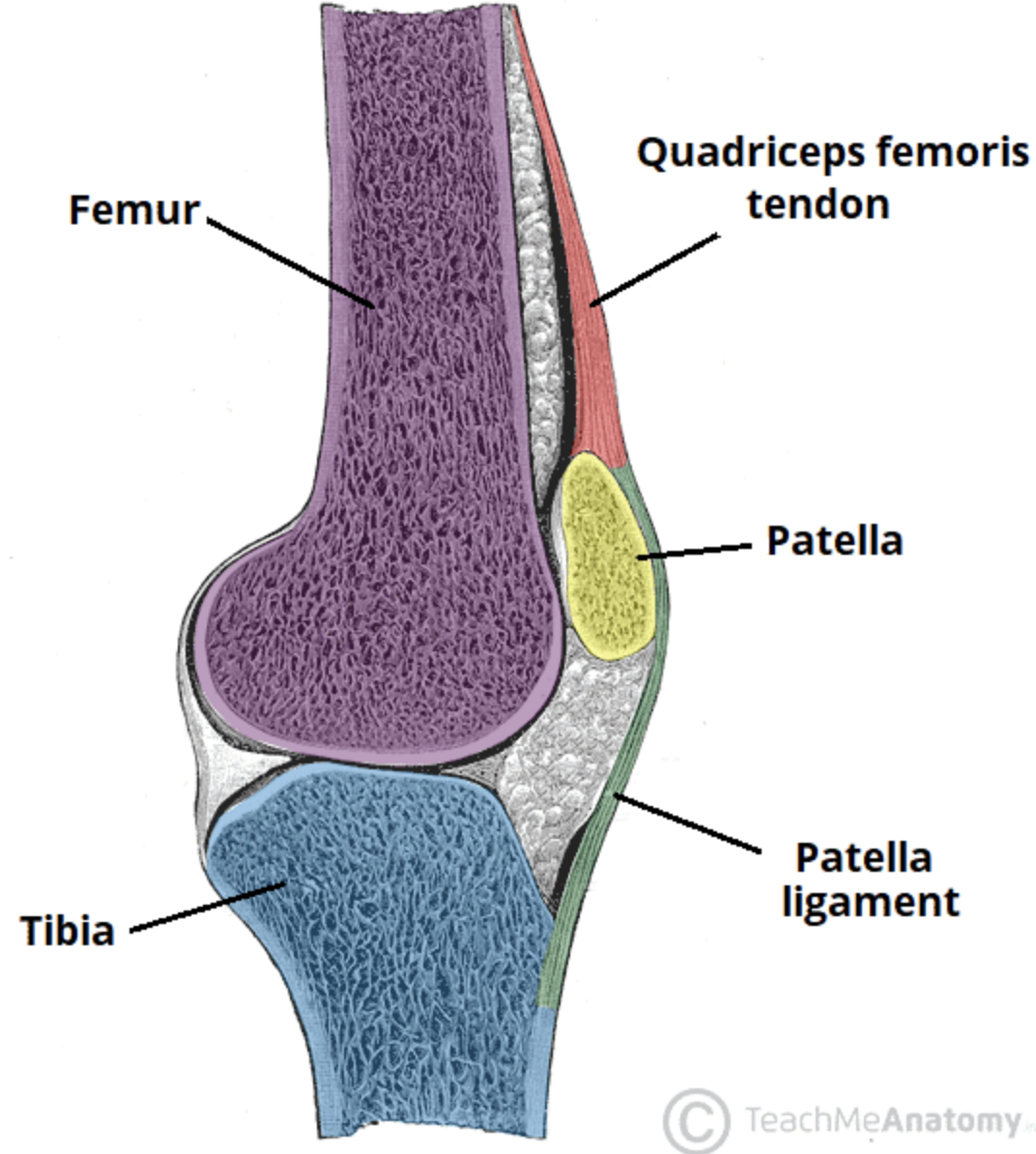
Knee Joint (Femoro-patellar koint PFJ)
Largest and most complex of the diarthrotic joints (Diarthrotic= freely movable joint)
Predominantly a hinge joint
Consists of two articulations: 1) Tibiofemoral joint 2) Patellofemoral joint
The knee joint is covered by the patella, a sesamoid bone embedded in the quadriceps (femoris) tendon superiorly
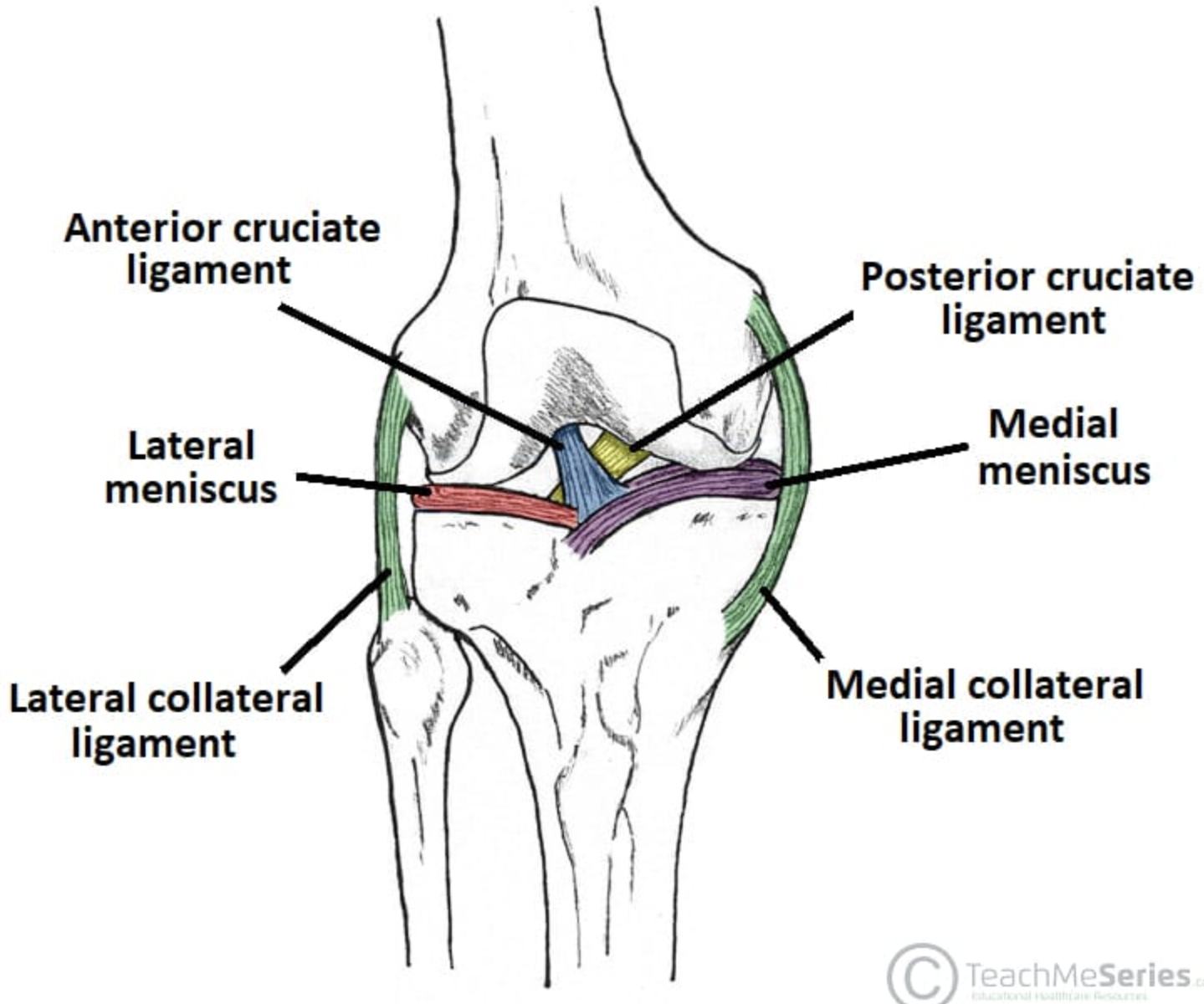
Stability of knee joint
Medial stability due predominantly to tibial (medial) collateral ligament (MCL), semitendinosus, semimembranosus, sartorius and gracilis muscles.
Lateral stability due predominantly to fibular (lateral) collateral ligament (LCL), iliotibial tract, popliteus and biceps femoris muscles.
Anterior and posterior stability enhanced by the cruciate ligaments (anterior & posterior), quadriceps tendon and ligamentum patellae
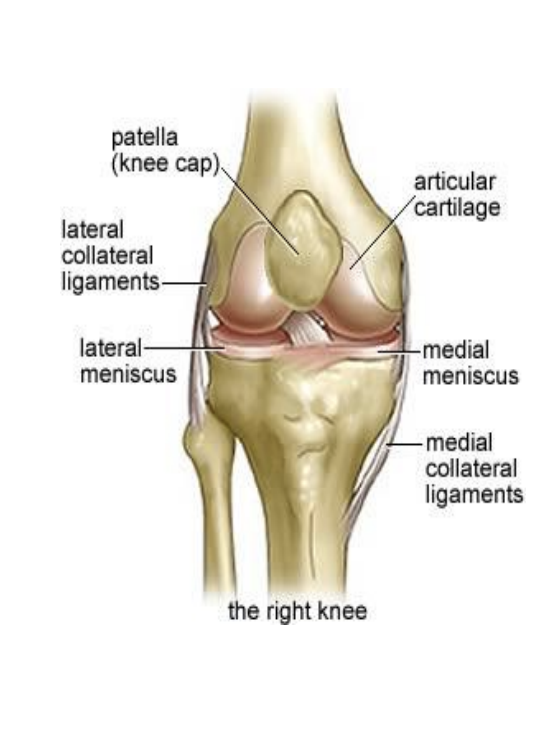
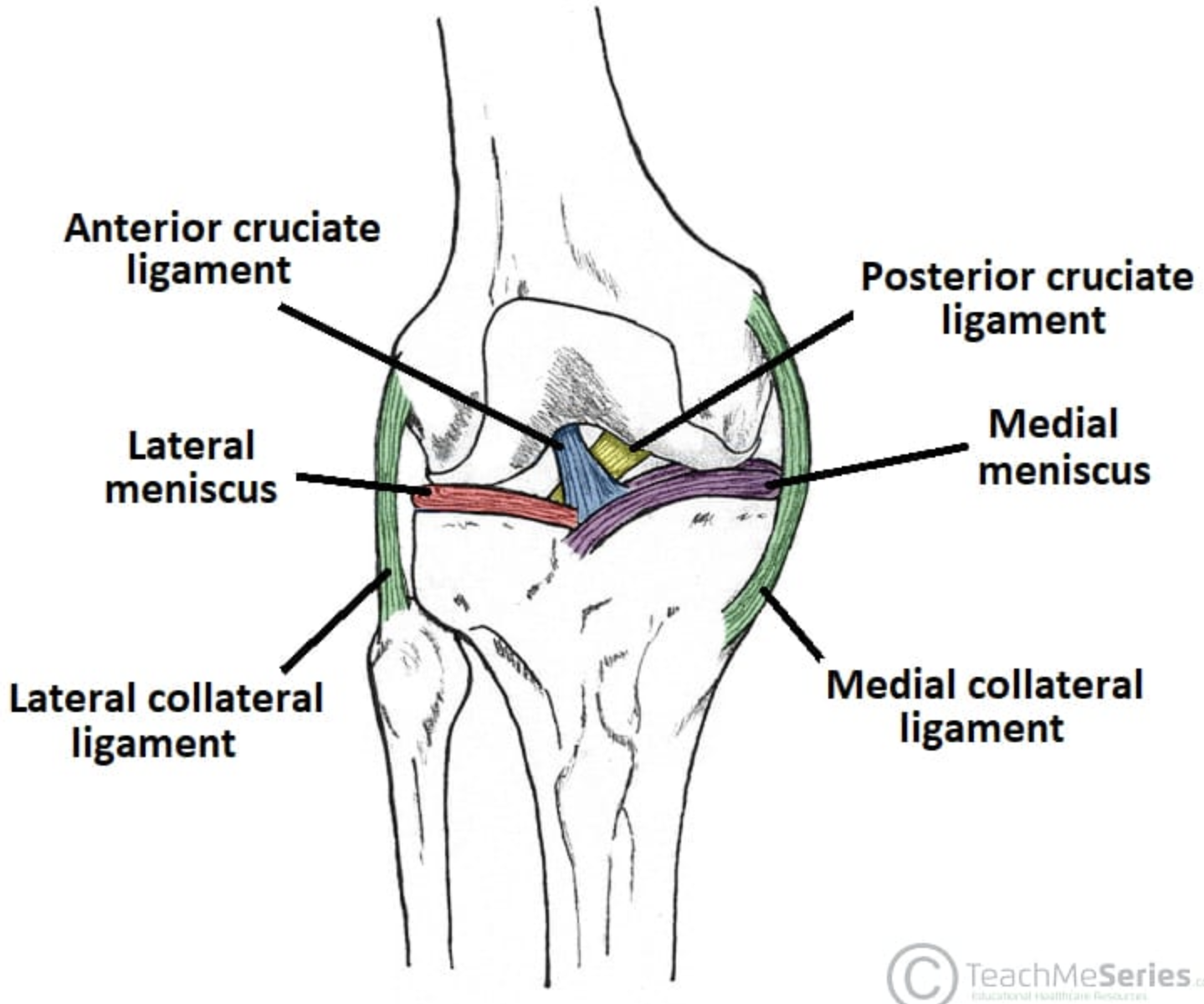
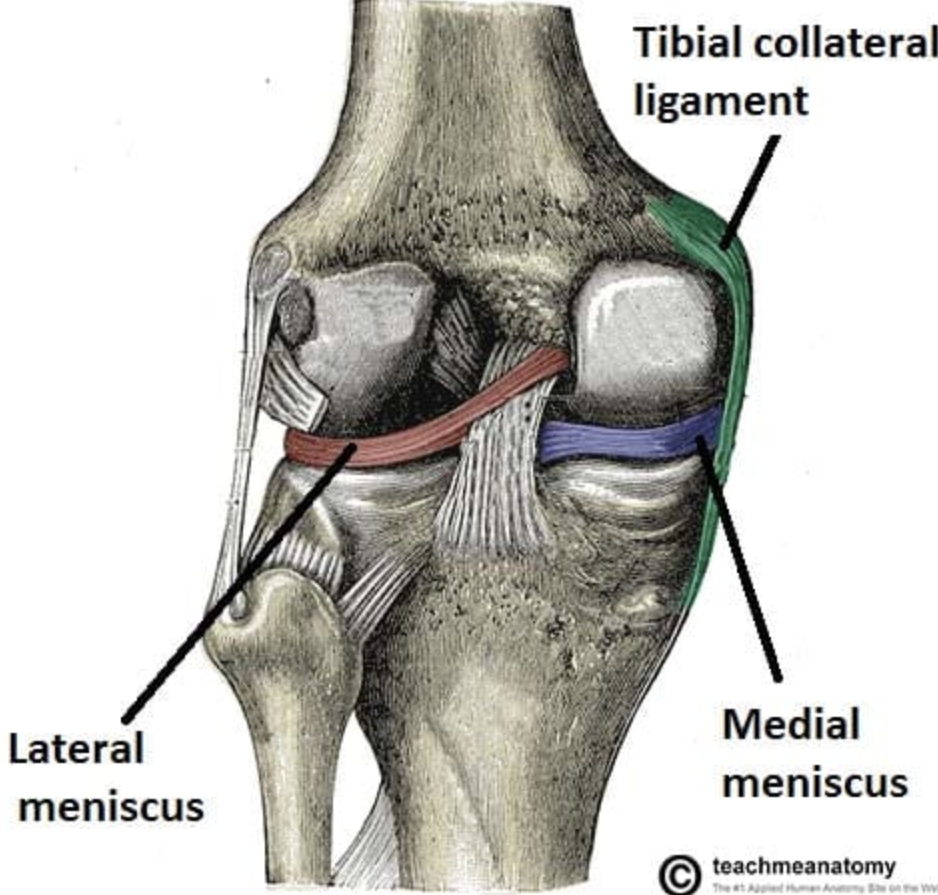
LCL and MCL
Two collateral ligaments that tighten during knee extension: a lateral (fibular) and a medial (tibial) collateral ligament
Fibular collateral (LCL) helps prevent hyper-adduction. (varus)
Tibial collateral (MCL) helps prevent hyper-abduction. (valgus)
Meniscii
Two fibrocartilage pads on the condyles of the tibia ( one medial and one lateral)
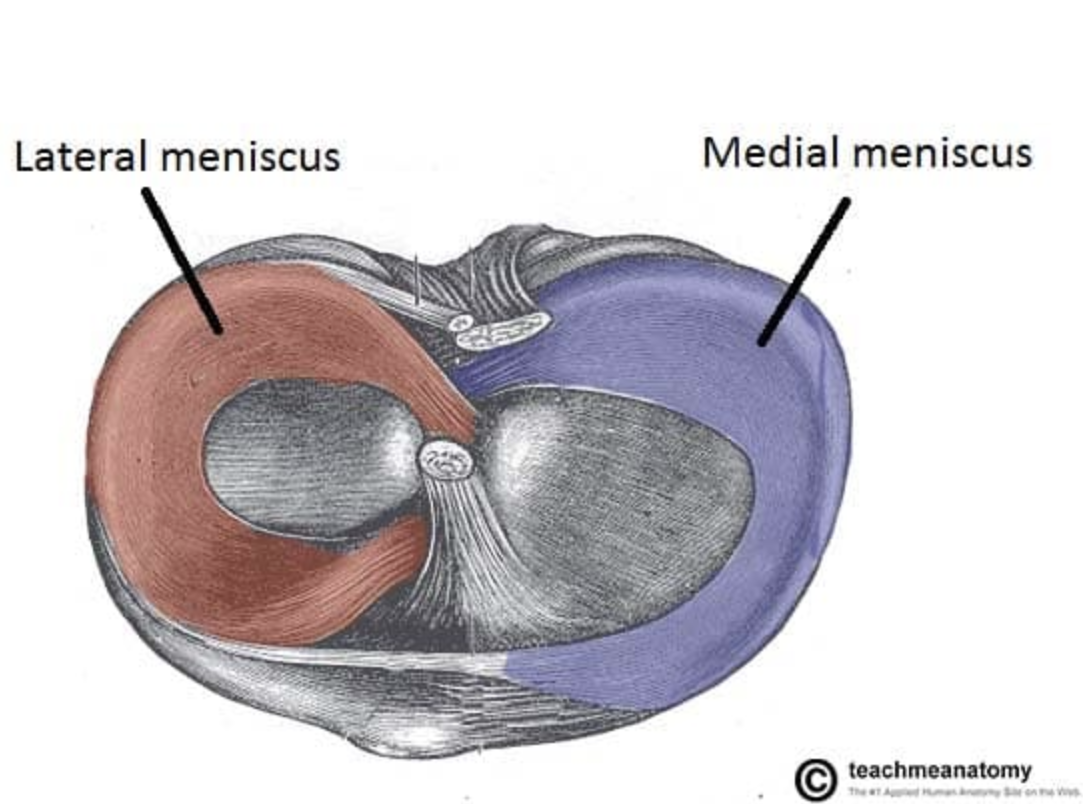
Knee Joint-meniscus
Shape= semilunar shape (Greek word meniskos means crescent)
Function= assists during tension and torsion Helps reduce friction between the femur and tibia and helps to shock absorb
Blood flow is from the periphery towards the central meniscus- but generally quite avascular structures
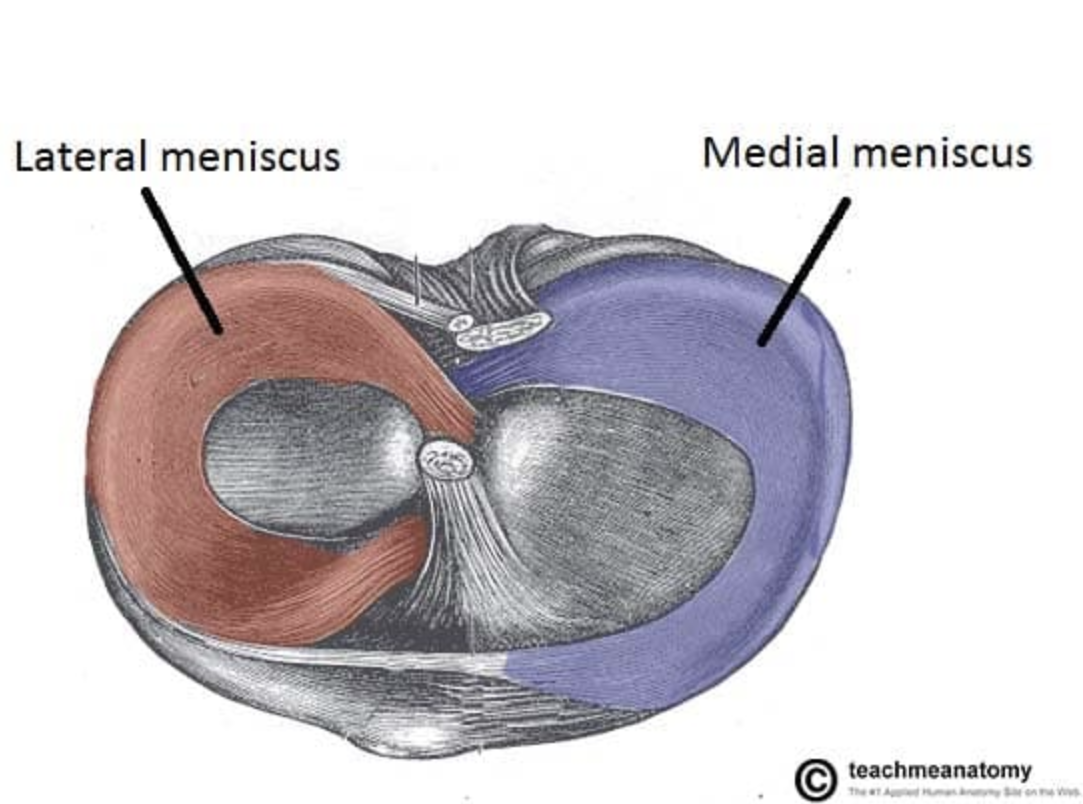
Medial Meniscus
Blood supply: inferior and superior genicular arteries Vascularity decreases with age
Nerve supply: Free nerve endings supply the vascularised portion as well as 3 different Mechanoreceptors (Ruffini corpuscles, Pacinian corpuscles, Golgi tendon)
Lateral meniscus
Grooved laterally for the popliteus tendon, which separates it from the LCL
Same blood supply as medial meniscus
As vascularity decreases with age, central portion of meniscus depends on synovial fluid diffusion for nutrition
Knee Joint Ligaments-ACL
Two cruciate ligaments limit the anterior-posterior movement of the knee joint (cruciate = “X-shaped”)
The ACL (anterior cruciate ligament) runs from the posterior femur to the anterior tibia.
The. ACL prevents hyperextension when the knee is extended
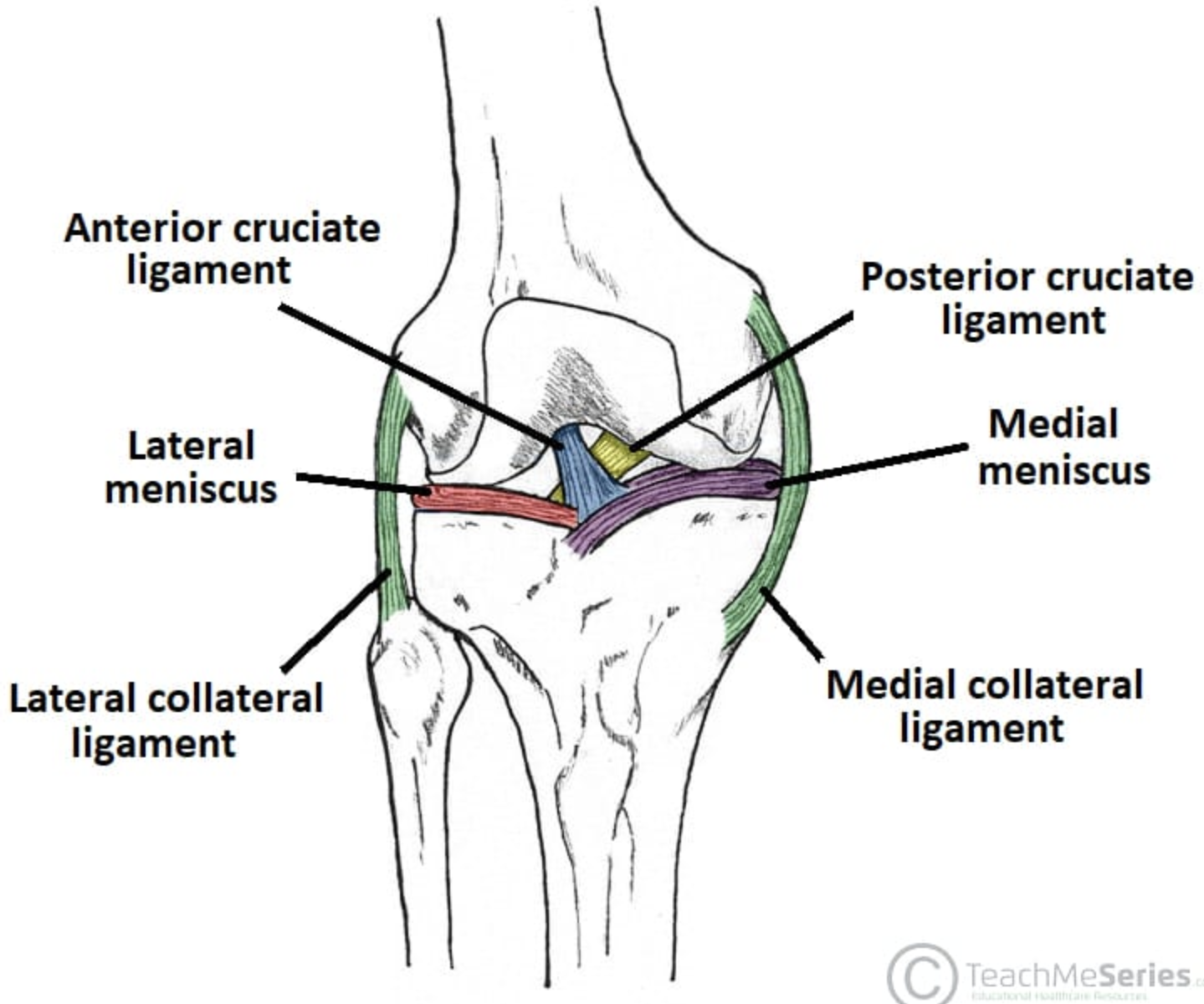
Knee Joint Ligaments- PCL
The PCL (posterior cruciate ligament) runs from the antero-inferior femur to the posterior tibia.
The PCL prevents hyperflexion of the knee (and posterior translation of the tibia in relation to the femur)