Physiology and Pain Theory
1/54
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
55 Terms
ATP-PC system
this energy system is used for ATP production during high intensity, short duration exercises (like sprinting 100 meters)
phosphocreatine decomposes and releases a large amount of energy used to contruct ATP. creates ATP almost instantaneously
can provide up to 15 seconds of muscle contraction
anaerobic glycolysis
this energy system is a major supplier of ATP during high intensity, short duration activities (like sprinting 400-800 m)
stored glycogen is split into glucose and then split again into pyruvic acid and released throughout to form ATP
can provide 30-40 seconds of muscles contraction
aerobic metabolism
used predominantly during low intensity, long duration exercise (like running a marathon). yields the most ATPs but requires several series of complex chemical reactions.
provides energy through oxidation of food and uses the combination of fatty acids, amino acids, and glucose with oxygen to form ATP
will provide energy as long as there are nutrients to utilize
If someone were to sprint 50 meters, which energy system are they predominantly using
ATP-PC system
if someone were to be running an 800 meter race, what energy system are they predominantly using
anaerobic glycolysis
if someone were to go run a marathon, what energy system are they predominantly using
aerobic metabolism
when weightlifting, how are the energy systems being used
typically
anaerobic systems (strength - anaerobic glycolysis, power - ATP-PC) work while lifting
aerobic system takes over during rest
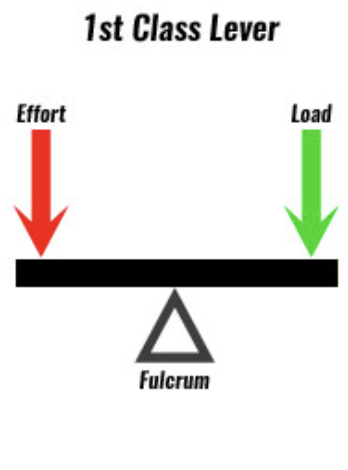
How is a class 1 lever set up
ex. seesaw
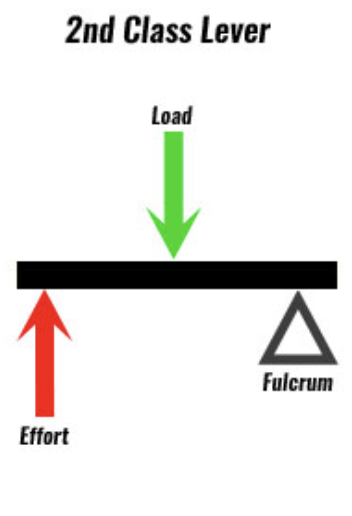
How is a class 2 lever set up
example wheelbarrow or tricep dip
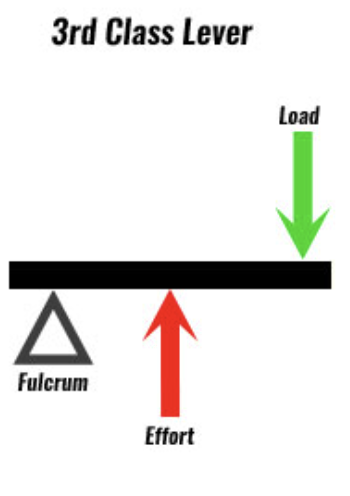
How is a class 3 lever set up
example around the world with weight
what are the different types of fibrous joints?
sutures (like the skull), syndesmosis (like between tib-fib), gomphosis (connecting tooth in its socket)
Characteristics of fibrous joints
composed of bones that are united by fibrous tissues and are nonsynovial, movement is minimal to none with amount of movement permitted at the joint dependent on the length of the fibers uniting the bones
suture
union of two bones by a ligament or membrane
immovable joint
eventual fusion is term synostosis
syndesmosis
bone connect to bone by a dense fibrous membrane or cord
very little motion
gomphosis
two bony surfaces connect as a peg in a hole
the teeth and corresponding sockets in the mandible/maxilla are the only gomphosis joints in the body
the periodontal membrane is the fibrous component of the joint
types of cartilaginous joints
synchondrosis (sternum and true ribs)
symphysis (pubic symphysis)
characteristics of cartilaginous joints
have hyaline cartilage or fibrocartilage that connect one bone to another. slightly movable joints
synchondrosis
hyaline cartilage
cartilage adjoints two ossifying centers of the bone
provides stability during growth
may ossify to a synostosis once growth is completed
slight motion
symphysis
generally located at the midline of the body
two bones covered with hyaline cartilage
two bones connected by fibrocartilage
slight motion
what are the types of synovial joints
uniaxial joint
biaxial joint
multi-axial joint
characteristics of synovial joints
provide free movement between the bones they joint. they have five distinguishing characteristics: joint cavity, articular cartilage, synovial membrane, synovial fluid, fibrous capsule
uniaxial joints
one motion around a single axis in one plane of the body
hinge and pivot joints
biaxial joints
movement occurs in the two planes and around two axes through the convex/concave surfaces
condyloid and saddle joints
multi-axial joints
movement occurs in three planes and around the tree axes
plane (gliding) joints
ball and socket joints
what are the different types of joint receptors
free nerve endings
golgi ligament endings
golgi-maxxoni corpuscles
pacinian corpuscles
ruffini endings
location, sensitivity, and primary distribution of free nerve endings
location: joint capsule, ligaments, synovium, fat pads
sensitivity: to non-noxious and noxious mechanical stress, and biochemical stimuli
primary distribution: all joints
location, sensitivity, and primary distribution of golgi ligament endings
location: ligaments, adjacent to ligaments, bony attachment
sensitivity: tension or stretch on ligaments
primary distribution: majority of joints
location, sensitivity, and primary distribution of golgi-mazzoni corpuscles
location: joint capsule
sensitivity: compression of joint capsule
primary distribution: knee joint, joint capsule
location, sensitivity, and primary distribution of pacinian corpuscles
location: fibrous layer of joint capsule
sensitivity: high frequency vibration, acceleration, high velocity changes in joint position
primary distribution: all joints
location, sensitivity, and primary distribution of ruffini endings
location: fibrous layer of joint capsule
sensitivity: stretching of joint capsule, amplitude and velocity of joint position
primary distribution: greater density in proximal joints, particularly in capsule regions
characteristics of type 1 muscle fibers
aerobic, red, tonic, slow twitch, slow-oxidative
low fatigability, high capillary density, high myoglobin content, smaller fibers, extensive blood supply, large amount of mitochondria
characteristics of type 2 muscle fibers
anaerobic, red/white, phasic, fast twitch, fast-glycotic
high fatigability, low capillary density, low myoglobin content, larger fibers, less blood supply, fewer mitochondria
what are muscle spindle’s function
to send information to the nervous system about muscle length and/or the rate of change of its length.
what are golgi tendon organs
encapsulated sensory receptors through which the muscle tendons pass immediately beyond their attachment to the muscle fibers. they provide the nervous system with instantaneous information on the degree of tension in each small muscle segment.
what are nociceptors activated by
thermal, mechanical, or chemical stimuli
nociceptors are the terminal portion of what two types of afferent neurons
A-delta and C fibers
what kind of information does A-delta fibers transmit
detailed information rapidly from peripheral cutaneous structures (skin, muscle)
what kind of information does C fibers transmit
information from deeper tissues more slowly (joints, viscera)
A-delta fibers are more likely to transmit pain signals that are (list descriptor words)
sharp, localized
C fibers are more likely to transmit pain signals that are (list descriptor words)
dull, aching, diffuse
pathway of pain
nociceptors → afferent neurons (A-delta, C) → dorsal horn of the spinal cord → spinothalamic tract → thalamus → sensory cortex
What is the gate control theory explain
explains the regulation of pain, specifically how other stimuli can help to decrease the sensation of pain.
how does the gate control theory work
A-delta and C fibers synapse with inhibitory interneurons from A-alpha and A-beta fibers.
A-alpha and A-beta fibers can stimulate inhibitory signals to prevent pain
(think massage, modalities, pressure, foam rolling)
endogenous opioids
opiopeptins (aka endorphins) can inhibit GABA which inhibits A-beta fibers
aka if GABA inhibits inhibitory fibers…endorphins can override GABA to let A-beta fibers work
What are the 5 sources of pain
cutaneous/superficial
deep somatic
visceral
neuropathic
referred
what are the 4 pain mechanisms
nociceptive
neuroplastic
nociplastic
motor and psychosocial
cutaneous/superficial pain source
superficial somatic pain - caused by structures within the skin or subcutaneous tissue. The pain tends to be well-localized and is described as stabbing or sharp, though it can be a dull ache/throb when the patient is at rest
deep somatic pain source
caused by deep somatic structures such as bone, muscle, fascia, tendons, ligaments, joint capsules, and blood vessels. the pain may be diffuse and may be referred to other areas. it is described as dull, aching, cramping, or gnawing and can be associated with muscle spasms or trigger points
visceral pain source
caused by internal organs. Pain is poorly localized and often produces referred pain to more superficial structures. visceral pain can be associated with autonomic symptoms
neuropathic pain source
caused by damage to the peripheral or central nervous system. thep ain is described as sharp, burning, shooting, tingling, or electrical and will likely follow a peripheral neurve or dermatomal pattern. symptom provocation occurs with tests that move, load, or compress neural tissues, may be evoked by stimuli that are not generally noxious (light touch)
referred pain source
pain that is felt in an area distant to the site of injury. referral of pain occurs due to the sharing of ascending pathways between visceral and somatic structures. referred pain is well-localized though it does not have sharply defined borders. localized tenderness and muscle hypertonicity are common in referred pain area.
nociceptive pain mechanism
due to injury, inflammation, or mechanical irritation to non-neural tissue in the body and results from the activation of nociceptors. Pain is proportionaly to the level of stimulus applies
neuropathic pain mechanism
due to a lesion or disease of the peripheral or central nervous system. Referred in a dermatomal or cutaneous distribution. may be associated with sensory signs such as tingling, numbness, and burning or associated with sympathetic signs such as color, temp, and trophic changes
nociplastic pain mechanism
due to abnormal pain processing withing the central nervous syems. Pain is disproportional to the level of stimulus, non-mechanical, and unpredictable. Pain and tenderness tend to be diffuse and not related to specific anatomical structures. Strongly associated with psychosocial factors. (or can be mechanical pain that has lasted longer than what is expected for normal tissue healing)
Chronic pain is defined as
pain that lasts longer than 3 months or pain that lasts longer than what would be expected for true physiological healing to occur