CH 8: Cardiac Pathology (mine)
1/175
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
176 Terms
Ischemic Heart Disease (IHD) is?
Group of syndromes related to myocardial ischemia
Left sided heart failure presents as?
-Decreased Ejection Fraction
-Bibasilar crackles in lung/rales
liquid accumulates in alveoli due to left heart pressure overload —> alveoli pop open during inhalation, causing rales
-S3 or S4
-exertional dyspnea, orthopnea, paroxysmal nocturnal dyspnea, or persistent coughing.
-ankle edema + abdominal fullness (ascites +hepatojugular reflex)
Describe Right-sided heart failure
-Atrial fibrillation
- JVD (don’t be confused w/JVP)—> Kussmaul breathing (PARADODIXAL INCREASE IN jvp WHEN INSPIRATION
-hepatojugular reflux
-Nutmeg liver & hepatomegaly
-Ankle edema & Ascites
Differentiate between S3 & S4
S3 = systolic failure, diastolic rumble due to excess blood volume in overload (normal in young ppl)
Increased volumes of blood move from the LA —> compliant LV ventricle resulting in a characteristic low-pitched sound as blood fills the chamber.
Systolic heart failure with decreased left ventricular contractility and increased end systolic volumes.
S4 = Diastolic failure,, systolic rumble bc of hypertrophic/thick heart
What causes S3 & S4
S3 = young, pregnant, CHF, mitral regurgitation, dilated cardiomyopathy
S4 = HCOM, Restrictive cardiomyopathy(will have Kussmaul)
What is the leading cause of death in the US?
IHD
IHD is usually due to?
Atherosclerosis of coronary arteries which decreases blood flow to the myocardium
Risk factors for IHD?
Increase in age bc it correlates with risks for atherosclerosis
Stable angina is?
Chest pain that arises with exertion or emotional stress
Stable angina is due to?
Atherosclerosis of coronary arteries with >70% stenosis.
The decreased blood flow is not able to meet the metabolic demands of the myocardium during exertion --> injury to myocardium causing chest pain
Damage to myocytes in stable angina?
Reversible injury (cellular swelling)
*No necrosis
Stable angina presents as?
Chest pain lasting <20mins that radiates to the left arm or jaw, diaphoresis, and SOB
What is diaphoresis?
Sweating, especially to an unusual degree as a symptom of disease or a side effect of a drug.
EKG on a patient with stable angina reveals?
ST segment depression due to subendocardial (between myo & endo) ischemia
What relieves stable angina?
rest
Nitroglycerin (vasodilates)
What is unstable angina?
Chest pain that occurs at REST
Unstable angina is usually due to?
Rupture of an atherosclerotic plaque with thrombosis and incomplete occlusion of a coronary artery
*So a baby bit of blood can flow through, just enough to keep myocardium alive
Keywords for stable vs unstable angina?
Stable = atherosclerosis caused stenosis (>70%)
Unstable = thrombosis due to ruptured plaque (incomplete occlusion)
Damage to myocytes in unstable angina?
Reversible injury to myocytes with no necrosis
EKG on patient with unstable angina shows?
ST segment depression due to subendocardial ischemia
What relieves unstable angina?
nitroglycerin
What does unstable angina carry a risk of?
Progression to myocardial infarction
Prinzmetal angina clinically presents as?
episodic chest pain unrelated to exertion
Prinzmetal angina is due to?
coronary artery vasospasm
Damage to myocytes in prinzmetal angina?
reversible injury with no necrosis
EKG on patient with prinzmetal angina shows?
ST segment elevation due to transmural ischemia
*not ST depression like unstable & stable
What relieves prinzmetal angina?
Balloon Angioplasty, Stents, Coronary Bypass surgery
nitroglycerin (decrease preload)
calcium channel blockers (reduce vasospasm)
What drug should you NOT give in Prinzmental angina?
Beta blockers bc they can cause more spasm
*** So only give Beta blockers in Stable & Unstable angina (can combine with NTG)
What does transmural mean?
existing or occurring across the entire wall of an organ or blood vessel- like in prinzmental angina
Myocardial Infarction(MI) is?
Usually due to?
Other causes include?
Necrosis of cardiac myocytes
Rupture of atherosclerotic plaque with thrombosis and complete occlusion of a coronary artery.
What are some causes/risk factors for MI?
coronary artery vasospasm(due to Prinzmetal angina or cocaine use),
Emboli
vasculitis(ie Kawasaki disease)
Also unstable angina can lead to it (incomplete occlusion)
Clinical features of MI?
Severe crushing chest pain lasting >20mins that radiates to left arm or jaw, diaphoresis, and dyspnea (due to pulmonary congestion & pulmonary edema).
*Symptoms are not relieved with nitroglycerin
MI usually involves what portion of the heart?
Left ventricle; RV and both atria usually spared
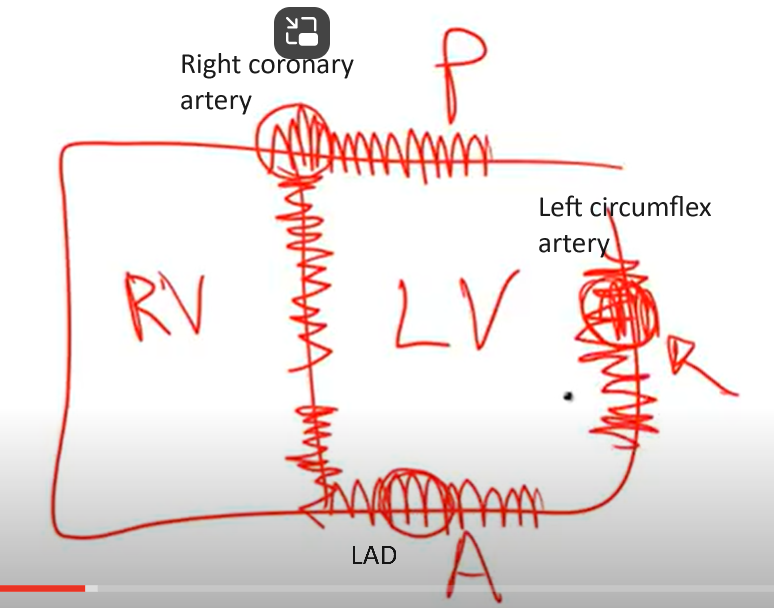
Most commonly involved artery of MI? 2nd most common?
Left anterior descending artery
Right coronary artery
Occlusion of LAD leads to infarction of?
Occlusion of RCA leads to infarction of?
Occlusion of left circumflex artery leads to infarction of?
Anterior wall and anterior septum of LV.
Posterior wall, posterior septum, and papillary muscles of LV.
Lateral wall of LV
Initial phase of MI leads to?
Continued or severe ischemia leads to?
Subendocardial necrosis involving < less than 50% of the myocardial thickness (subendocardial infarction).
Since still subendocardial, still shows ST segment depression (not yet characteristic ST elevation)
Continued MI or severe ischemia
Transmural necrosis involving most of the myocardial wall(transmural infarction) = ST elevation
Laboratory findings in MI? What are the cardiac enzymes?
EKG - ST segment depression
Troponin I - Levels rise for 2-4hrs after MI, peak at 24hrs, and return to normal in 7-10 days. This is the most sensitive and specific marker, the gold standard for MI.
Creatine Kinase - MB (CK-MB) - rise 4-6 hrs after infarction, peak at 24 hrs, and return to normal by 72 hrs
What is CK-MB useful for?
Detecting reinfarction that occurs days after initial MI
Treatment for MI includes? Include what each treatment accomplishes.
Aspirin and/or heparin - limits thrombosis
Supplemental O2 - minimizes ischemia
Nitrates - vasodilates veins and coronary arteries
ß blockers - slows heart rate, decreases O2 demand and risk for arrhythmia
ACE inhibitor - decreases LV dilation (blocks vasoconstriction of peripheral arterioles & decrease blood volume
Fibrinolysis or Angioplasty - opens blocked vessel
What does Fibrinolysis & Angioplasty essentially do?
What are the 2 bad outcomes?
Once dissolving clot it reperfuses (brings in new blood to) the irreversibly damaged cells
Contraction band necrosis & Reperfusion Injury
What occurs when you reperfuse irreversibly damaged cells after MI?
Results in calcium influx —> hypercontraction of myocytes (contraction band necrosis)
The return of oxygen and inflammatory cells —> ROS generation further damaging myocytes (reperfusion injury)
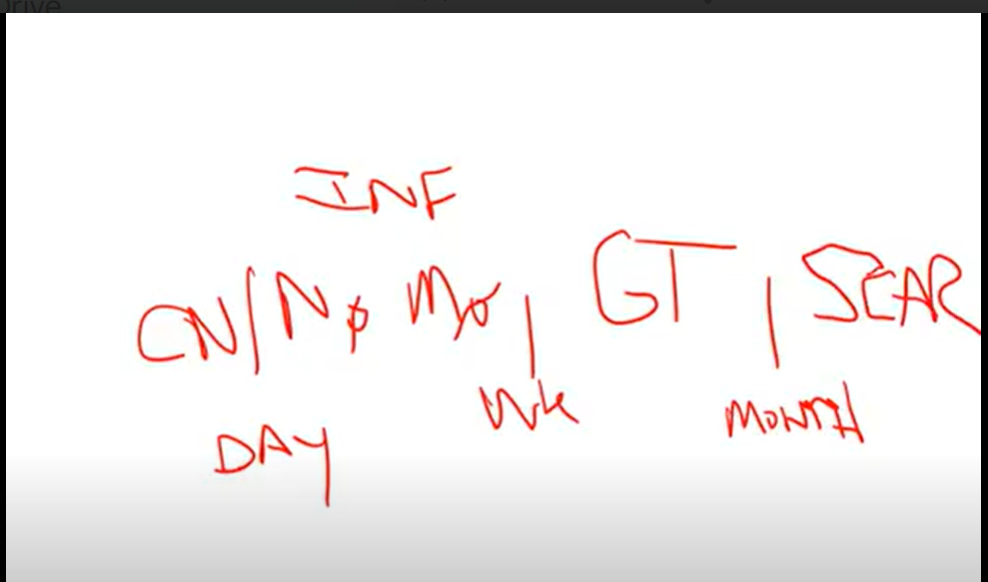
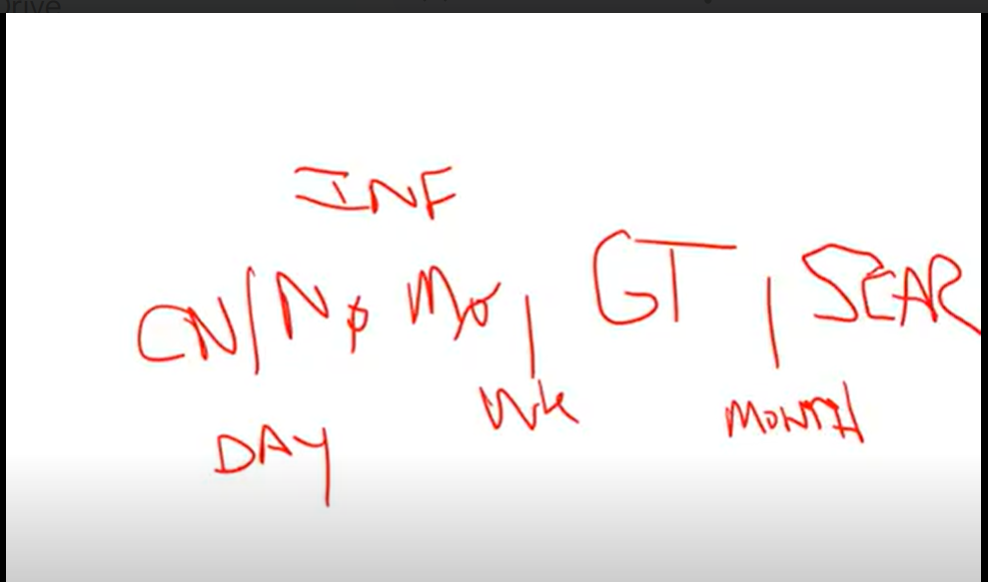
What are the gross changes, microscopic changes, and associated complications at different time points after MI?
<4hrs: no gross/microscopic changes —> cardiogenic shock(massive infarct), congestive heart failure, and arrythmia.
4-24hrs: Dark color = Coagulative necrosis (removal of nucleus due to necrosis)—> arrhythmia
1-3days: yellow pallor; Inflammation so neutrophils —> Fibrinous pericarditis
4-7 days: yellow pallor; Macrophages to clean up dead stuff —>Rupture of:
ventricular free wall (leads to cardiac tamponade)
interventricular septum (leads to shunt)
Papillary muscles (leads to mitral insufficiency)
Especially in Right coronary artery occlusion
1-3 weeks (starting to heal, softening): Red border emerges as granulation tissue enters from edge of infarct; granulation tissue with plump fibroblasts, type 1 collagen, and blood vessels —> then red —> gray
Months: White scar; Fibrosis —>
Aneurysm, mural thrombus, or Dressler Syndrome
How to remember all these stages of MI?
Fibrinous Pericarditis (like in MI)presents with?
Chest pain with friction rub- only in trasmural ischemia
What is Dressler Syndrome? When can you get it?
Autoimmune pericarditis
Months after an MI
Sudden cardiac death is _____ and usually due to?
When and how does it occurs?
Unexpected death due to cardiac disease that is usually due to fatal ventricular arrhythmia
Occurs without symptoms or
Most common etiology for sudden cardiac death?
Less common causes?
Acute ischemia
mitral valve prolapse, cardiomyopathy, and cocaine abuse
Most patients who died as a result of sudden cardiac death had?
Preexisting atherosclerosis(90% of patients)
Chronic Ischemic Heart Disease is?
Poor myocardial function due to chronic ischemic change(with or without infarction) that progresses to congestive heart failute (CHF)
CHF is?
Pump failure, can be right or left sided
Causes of left sided CHF?
Think DR. HIM
Dilated cardiomyopathy
Restrictive cardiomyopathy
HTN —> Hypertrophy
Ischemia
MI
What is dilated cardiomyopathy? What is restrictive cardiomyopathy
D: 4 chamber dilation that stretches the muscle —> can’t contract as well
R: can’t fill the heart properly —> so can’t pump it properly either
Clinical features of left sided CHF are due to?
Features include?
Pulmonary congestion & decreased forward perfusion
Pulmonary congestion= pulmonary edema w/ dyspnea, paroxysmal nocturnal dyspnea, orthopnea, and crackles (fluid)
Heart failure cells (hemosiderin laden macrophages): small congested capillaries may burst leading to intra-alveolar hemorrhage
Pleural effusions, pulmonary edema, pulmonary congestion
Decreased flow to kidneys leads to activation of RAS system (txt w/ ACE inhibitor)
*Secondary hypoperfusion —> renal + cerebral dysfunction
How does pulmonary congestion lead to paroxysmal nocturnal dyspnea?
Increased venous return while lying flat
What can exacerbate CHF?
Increased total peripheral resistance bc of Angiotensin II
Increase in Fluid retention- bc of release of aldosterone (due to Angiotensin II)
Treatment of CHF?
Mainstay is an ACE inhibitor
Right sided CHF is most commonly due to?
Other important causes include?
Left sided heart failure.
Left to right shunt and chronic lung disease (cor pulmonale = pulmonary HTN & right heart hypertrophy)
Clinical features of right sided CHF are due to?
Features include?
Congestion.
JVD,
painful hepatosplenomegaly with characteristic 'nutmeg' liver that may lead to cardiac cirrhosis, dependent pitting edema.
How does congestion in right sided CHF lead to pitting edema?
Increased hydrostatic pressure
Congenital heart defects arise during?
Seen in what % of births?
Most defects are?
Embryogenesis(usually weeks 3-8)
1% of live births
Sporadic
Congenital heart defects often result in?
Shunting between left(systemic) and right(pulmonary) circulations
Defects of left to right shunting at birth result in?
Can be relatively asymptomatic at birth but eventually shunts can reverse.
How do the L—> R shunts reverse?
Increased flow through pulmonary circulation—> Hypertrophy of pulmonary vessels and pulmonary HTN —> both leading to increased pulmonary resistance —> reverse shunt
What are the consequences of a L-R shunt reversal?
Late cyanosis(eisenmenger syndrome) with RV hypertrophy, polycythemia, and clubbing.
Defects with right to left shunting usually present as ______ after birth.
Cyanosis
What is Eisenmenger syndrome?
Late cyanosis, pulmonary hypertension, and erythrocytosis. Seen in LEFT to right shunt (not right to left)
Most common congenital heart defect?
Ventricular Septal Defect(VSD)
A VSD is?
Associated with?
Defect in septum that divides RV and LV
Fetal alcohol syndrome & Teratology of Fallot
A VSD results in?
Left to right shunt
Size of VSD defect determines?
Extent of shutting and age of presentation.
Small defects are often asymptomatic and large defects can lead to eisenmenger syndrome
Treatment of VSD?
Surgical closure, small defects may close spontaneously
Atrial Septal Defect (ASD) is?
A defect in septum that divides the atria(ostium primum and ostium secundum types)
Most common type of ASD?
Ostium secundum(90% of cases)
Ostium primum ASD is associated with?
Down syndrome
ASD results in?
Important complication of ASD?
Left to right shunt with split S2 on auscultation.
Paradoxical emboli
What causes an S2 split?
Increased blood in Right heart delays closure of pulmonary valve
Patent Ductus Arteriosus(PDA) is?
Associated with?
Failure of ductus arteriosus to close at birth
congenital rubella
PDA results in?
left to right shunt between aorta and pulmonary artery bypassing lungs
Normal function of ductus arteriosus?
During development, shunts blood from pulmonary artery to aorta to bypass lungs
Symptoms of PDA?
Asymptomatic at birth with continuous 'machine like" murmur; may lead to Eisenmenger syndrome (late cyanosis), resulting in lower extremity cyanosis
Treatment of PDA?
Indomethacin= an NSAID that decreases PGE1 (prostaglandin E1 that keeps PDA) resulting in PDA closure.
Tetralogy of Fallot is?
A right to left shunt that leads to early cyanosis
What congenital heart defect causes Left to right shunts (that can lead to late cyanosis or Eisenmenger)?
PDA
ASD (but can also be R-L in tricuspid atresia)
VSD (large, but can also be R-L in teratology of fallot)
AVSD (atrioventricular septal defect)
L—R shunt reversal due to increased pulmonary resistance
Tetralogy of Fallot is characterized by?
Think VORS
VSD
Overriding Aorta
RV hypertrophy
Stenosis of RV outflow tract
What determines that extent of shunting and cyanosis in Tetralogy of Fallot?
Degree of stenosis
What do patients learn to do with Tetralogy of Fallot that helps alleviate cyanotic spells? Why does this work?
Squatting.
Increases arterial resistance = decreases shunting and allows more blood to reach lungs
What do you find on X-Ray in tetralogy of fallot?
"boot shaped" heart
Transposition of the Great Vessels is characterized by?
Results in?
Pulmonary artery arising from LV and aorta arising from RV (the arteries are the opposite places!)
Hypertrophy of RV and atrophy of LV
Transposition of the Great Vessels is associated with?
Maternal diabetes
Transposition of the Great Vessels presents with?
Presents early with cyanosis, as pulmonary and systemic circuits do not mix (so txt will fix this)
Transposition of the Great Vessels treatment?
Creation of shunt, to allow blood to mix, after birth is necessary for survival. Surgical correction is required.
PGE can be administered to maintain a PDA until definitive surgical repair is performed
Truncus Arteriosus is characterized by?
Single large vessel arising from both ventricles due to the truncus failing to divide.
Truncus Arteriosus presents with?
Early cyanosis. Deoxygenated blood from RV mixes with oxygenated blood from LV before pulmonary and systemic circuits separate
Tricuspid Atresia is?
Often associated with ______ which results in?
Presents with?
Tricuspid valve orifice fails to develop so the RV is hypoplastic
Associated w/ ASD —> resulting in R-L shunt (early cyanosis)
Coarctation of the Aorta is?
Narrowing of the aorta; adult and infantile forms
Infantile Form of Coarctation of the Aorta is associated with?
Where does the narrowing lie?
Presents as?
PDA and also Turner Syndrome (think PDA in front of kids is bad!)
Distal to aortic arch but proximal to PDA (after arch, before PDA)
Lower extremity cyanosis in infants, often at birth
Adult form of Coarctation of the Aorta is associated with?
Where does the narrowing lie?
Presents as?
What is seen on Xray? Why?
Associated w/ Bicuspid aortic valve
Distal to aortic arch (bc adults don’t have their PDA anymore)
What does Adult Coarctation of the aorta present as? What are the symptoms?
Symptoms: HTN in upper extremities and hypotension with weak pulses in lower extremities.
Notching of ribs due to engorged arteries ( collateral circulation developing across intercostal arteries)
What are the four valves of the heart and what do they do?
Bicuspid(mitral), tricuspid, pulmonary and aortic.