BOC: 107-154 Immune Diseases & Transplantation
1/47
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
48 Terms
Systemic lupus erythematosus patients often have which of the following test results?
a) high titers of ANA
b) decreased serum immunoglobulin levels
c) high titers of anti-smooth muscle antibodies
d) high titers of anti-mitochondrial antibody
A
Systemic lupus erythematosus patients with active disease often have which of the following test results?
a. high titers of antimicrosomal antibodies
b. high titers of anti-smooth muscle antibodies
c. marked decrease in serum CH50
d. decreased serum immunoglobulin levels
C
Which of the following is decreased in serum during the active stages of systemic lupus erythematosus?
a. anti-nuclear antibody
b. immune complexes
c. complement (C3)
d. anti-DNA
C
Which of the following is an organ-specific autoimmune disease?
a. myasthenia gravis
b. rheumatoid arthritis
c. Addison disease
d. progressive systemic sclerosis
C
In chronic active hepatitis, high titers of which of the following antibodies are seen?
a) anti-mitochondrial
b) anti-smooth muscle
c) anti-DNA
d) anti-parietal cell
B
In primary biliary cirrhosis, which of the following antibodies is seen in high titers?
a. anti-mitochondrial
b. anti-smooth muscle
c. anti-DNA
d. anti-parietal cell
A
Anti-glomerular basement membrane antibody is most often associated with this condition:
a. systemic lupus erythematosus
b. celiac disease
c. chronic active hepatitis
d. Goodpasture syndrome
D
In pernicious anemia, which of the following antibodies is characteristically detected?
a. anti-mitochondrial
b. anti-smooth muscle
c. anti-DNA
d. anti-parietal cell
D
An example of an organ specific disease with autoimmune antibodies is:
a. Wegener granulomatosus
b. rheumatoid arthritis
c. Hashimoto thyroiditis
d. systemic lupus erythematosus
C
Which of the following are true statements about selective IgA deficiency?
a. associated with a decreased incidence of allergic manifestation
b. high concentration of secretory component in the saliva
c. associated with an increased incidence of autoimmune diseases
d. found in approximately 1 out of every 50 persons
C
A monoclonal spike of IgG, Bence Jones proteinuria, and bone pain are usually associated with:
a. Burkitt lymphoma
b. Bruton disease
c. severe combined immunodeficiency disease
d. multiple myeloma
D
The hyperviscosity syndrome is most likely to be seen in monoclonal disease of which of the following immunoglobulin classes?
a. IgA
b. IgM
c. IgG
d. IgD
B
Patient suffering from Waldenstrӧm macroglobulinemia demonstrate excessively increased concentrations of which of the following?
a. IgG
b. IgA
c. IgM
d. IgD
C
Which of the following is the most common humoral immune deficiency disease?
a. Bruton agammaglobulinemia
b. IgG deficiency
c. selective IgA deficiency
d. Wiskott-Aldrich syndrome
C
Which of the following is a true statement about Bruton agammaglobulinemia?
a. it is found only in females
b. there are normal numbers of circulating B cells
c. there are decreased to absent concentrations of immunoglobulins
d. the disease presents with pyogenic infections 1 week after birth
C
Immunodeficiency with thrombocytopenia and eczema is often referred to as:
a. DiGeorge syndrome
b. Bruton agammaglobulinemia
c. ataxia telangiectasia
d. Wiskott-Aldrich syndrome
D
Hereditary angioedema is characterized by:
a) decreased activity of C3
b) decreased activity of C1 esterase inhibitor
c) increased activity of C1 esterase inhibitor
d) increased activity of C2
B
Which of the following has been associated with patients who have homozygous C3 deficiency?
a) undetectable hemolytic complement activity in the serum
b) systemic lupus erythematosus
c) no detectable disease
d) a lifelong history of life threatening infections
D
Hereditary deficiency of early complement components (C1, C4, C2) is associated with:
a) pneumococcal septicemia
b) small bowel obstruction
c) lupus erythematosus like syndrome
d) gonococcemia
C
Hereditary deficiency of late complement components (C5, C6, C7, or C8) can be associated with which of the following conditions?
a) pneumococcal septicemia
b) small bowel obstruction
c) systemic lupus erythematosus
d) a systemic Neisseria infection if exposed
D
Combined immunodeficiency disease with loss of muscle coordination is referred to as:
a. DiGeorge syndrome
b. Bruton agammaglobulinemia
c. ataxia telangiectasia
d. Wiskott-Aldrich syndrome
C
In skin tests, a wheal and flare development is indicative of:
a. immediate hypersensitivity
b. delayed hypersensitivity
c. anergy
d. Arthus reaction
A
Which immunologic mechanism is usually involved in bronchial asthma?
a) immediate hypersensitivity
b) antibody mediated cytotoxicity
c) immune complex
d) delayed hypersensitivity
A
Antihistamines like Benadryl:
a) depress IgE production
b) block antigen binding to surface IgE
c) bind histamine
d) block H1 histamine receptors
D
Incompatibility by which of the following procedures is an absolute contraindication to allotransplantation?
a. MLC (mixed lymphocyte culture)
b. HLA typing
c. Rh typing
d. ABO grouping
D
Which is a recognized theory of the origin of autoimmunity?
a. enhanced regulatory T-cell function
b. diminished helper T-cell activity
c. production of antibodies that cross-react with tissue components
d. deficient B-cell activation
C
Delayed hypersensitivity may be induced by:
a) contact sensitivity to inorganic chemicals
b) transfusion reaction
c) anaphylactic reaction
d) bacterial septicemia
A
The most rapid immediate hypersensitivity reaction is associated with:
a) transfusion
b) anaphylaxis
c) contact dermatitis
d) serum sickness
B
A marked decrease in CD4 lymphocytes and decrease in the CD4/CD8 ratio:
a) is diagnostic for bacterial septicemia
b) may be seen in MOST hereditary immunodeficiency disorder
c) is associated with a viral induced immunodeficiency
d) is only seen in patients with advanced disseminated cancer
C
Bone marrow transplant donors and their recipients must be matched for which antigen system(s)?
a. ABO-Rh
b. HLA
c. CD4/CD8
d. P1a1
B
A 28-year-old man is seen by a physician because of several months of intermittent low back pain. The patient's symptoms are suggestive of ankylosing spondylitis. Which of the following laboratory studies would support this diagnosis?
a. a decreased synovial fluid CH50 level
b. low serum CH50 level
c. positive HLA-B27 antigen test
d. rheumatoid factor in the synovial fluid
C
Cells from a patient with hairy cell leukemia have immunologic and functional features of:
a. mast cells and B lymphocytes
b. B lymphocytes and T lymphocytes
c. granulocytes and monocytes
d. B lymphocytes and monocytes
D
Which T-cell malignancy may retain "helper" activity with regard to immunoglobulin synthesis by B cells?
a. Hodgkin lymphoma
b. acute lymphocytic leukemia (ALL)
c. Sézary syndrome
d. chronic lymphocytic leukemia (CLL)
C
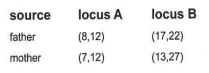
HLA typing of family yields the following results. On the basis of these genotypes, predict the possibility of ankylosing spondylitis in this percentage of their children.
a. 25% of their children
b. 50% of their children
c. 75% of their children
d. 100%
B
HLA-B8 antigen has been associated with which of the following pairs of diseases?
a. ankylosing spondylitis and myasthenia gravis
b. celiac disease and ankylosing spondylitis
c. myasthenia gravis and celiac disease
d. Reiter disease and multiple sclerosis
C
Which of the following is an important marker for the presence of immature B cells in patients with acute lymphocytic leukemia (ALL)?
a. terminal deoxynucleotidyl transferase (TdT)
b. adenosine deaminase
c. glucose-6-phosphate dehydrogenase
d. purine nucleoside phosphorylase
A
The ability of the immune system to recognize the self-antigens versus non-self antigens is an example of:
a. specific immunity
b. tolerance
c. cell-mediated immunity
d. humoral immunity
B
High titers of anti-thyroid peroxidase antibodies are most often found in:
a. Graves disease
b. systemic lupus erythematosus
c. chronic hepatitis
d. thyroid disease
D
A 2-year-old patient is suspected to have a peanut allergy because of breathing difficulties (anaphylaxis), which progressed to wheezing within a few minutes upon consumption of peanut butter. What in vitro diagnostic test (eg solid-phase enzyme immunoassay or indirect ELISA) would confirm this type of allergy?
a. total serum IgG and allergen specific IgG
b. total serum IgA and allergen specific IgA
c. total serum IgE and allergen specific IgE
d. total serum IgM and allergen specific IgM
C
A Patient underwent renal transplant, receiving a kidney from an unrelated donor. This type of transplant is termed:
a. allograft
b. syngraft
c. autograft
d. xenograft
A
Which of the following is a hyperacute reaction that is not part of chronic cell-mediated transplant rejection?
a. narrowing and occlusion of graft blood vessels
b. reaction of T and B cells to graft antigen
c. antibodies to MHC antigens on white cells
d. arteriosclerosis of the graft arterial wall
C
Graft-versus-host disease is:
a. initiated by the recipient
b. a minor concern in bone marrow transplant
c. asymptomatic in most cases
d. initiated by the donor
D
Alpha-fetoprotein, an oncofetal antigen, is least likely to be found in:
a. pregnancy
b. hepatocellular carcinoma
c. cirrhosis
d. breast carcinoma
D
Tumor-associated transplantation antigens (TAAs) are not found in:
a. fetal cells
b. tumor cells
c. bacterial cells
d. viral cells
C
Immunoediting describes the theory that our immune system prevents many cancers. Which of the following is not one of its 3 phases (called the 3 ‘e’s)?
a. efficiency
b. equilibrium
c. escape
d. elimination
A
Tissue injury in systemic rheumatic disorders such as systemic lupus erythematosus is thought to be caused by:
a. cytotoxic T cells
b. IgE activity
c. deposition of immune complexes
d. cytolytic antibodies
C
After a penicillin injection, a patient rapidly develops respiratory distress, vomiting and hives. This reaction is primarily mediated by:
a. IgG
b. IgA
c. IgM
d. IgE
D
A patient with a B-cell deficiency will most likely exhibit:
a. decreased phagocytosis
b. increased bacterial infections
c. decreased complement levels
d. increased complement levels
B